Abstract
Some patients with acquired pure red cell aplasia (aPRCA) have no response or are intolerant to cyclosporine A. From April 2017 to August 2020, patients diagnosed with aPRCA at Peking Union Medical College Hospital who were refractory/recurrent/intolerant to at least 6 months of full-dose cyclosporin A (CsA) with/without steroids were recruited and treated with sirolimus for at least 6 months. Finally, a total of 64 patients were enrolled. The overall response rate and complete response rate after 3, 6 and 12 months of sirolimus were 60.9%, 84.4%, and 73.5% and 50.0%, 65.6%, and 66.0%, respectively. At a median of 14.5 (6–47) months of follow-up, 14.8% (8/54) of the patients relapsed. Apart from haemoglobin improvement, patients had decreased creatine levels and serum ferritin levels at the end of the follow-up compared with the baseline (169.3 μmol/L vs. 146.4 μmol/L, p = 0.041; 2121.5 ng/mL vs. 1018.3 ng/mL, p = 0.013). Adverse events were recorded in 19 patients, including infections and increase of creatine. Secondary aPRCA with stable underlying diseases had similar results as those with primary aPRCA. In summary, sirolimus is effective for patients with refractory/recurrent/intolerant aRPCA with a low recurrence rate and toxicities.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Means RT Jr. Pure red cell aplasia. Blood. 2016;128:2504–9.
Gurnari C, Maciejewski JP. How I manage acquired pure red cell aplasia in adults. Blood. 2021;137:2001–9.
Sawada K, Fujishima N, Hirokawa M. Acquired pure red cell aplasia: updated review of treatment. Br J Haematol. 2008;142:505–14.
Sawada K, Hirokawa M, Fujishima N, Teramura M, Bessho M, Dan K, et al. Long-term outcome of patients with acquired primary idiopathic pure red cell aplasia receiving cyclosporine A. A nationwide cohort study in Japan for the PRCA Collaborative Study Group. Haematologica. 2007;92:1021–8.
Balasubramanian SK, Sadaps M, Thota S, Aly M, Przychodzen BP, Hirsch CM, et al. Rational management approach to pure red cell aplasia. Haematologica. 2018;103:221–30.
Mamiya S, Itoh T, Miura AB. Acquired pure red cell aplasia in Japan. Eur J Haematol. 1997;59:199–205.
Halkes C, de Wreede LC, Knol C, Simand C, Aljurf M, Tbakhi A, et al. Allogeneic stem cell transplantation for acquired pure red cell aplasia. Am J Hematol. 2019;94:E294–6.
Hashimoto K, Harada M, Kamijo Y. Pure red cell aplasia induced by anti-erythropoietin antibodies, well-controlled with tacrolimus. Int J Hematol. 2016;104:502–5.
Comont T, Bournet B, Casadevall N, Chauveau D, Faguer S. Rituximab in pure red-cell aplasia secondary to anti-erythropoietin antibodies. Kidney Int. 2014;86:210–1.
Sehgal SN. Sirolimus: its discovery, biological properties, and mechanism of action. Transpl Proc. 2003;35:7S–14S.
Benjamin D, Colombi M, Moroni C, Hall MN. Rapamycin passes the torch: a new generation of mTOR inhibitors. Nat Rev Drug Disco. 2011;10:868–80.
Li J, Kim SG, Blenis J. Rapamycin: one drug, many effects. Cell Metab. 2014;19:373–9.
Cejka D, Hayer S, Niederreiter B, Sieghart W, Fuereder T, Zwerina J, et al. Mammalian target of rapamycin signaling is crucial for joint destruction in experimental arthritis and is activated in osteoclasts from patients with rheumatoid arthritis. Arthritis Rheum-Us. 2010;62:2294–302.
Bride KL, Vincent T, Smith-Whitley K, Lambert MP, Bleesing JJ, Seif AE, et al. Sirolimus is effective in relapsed/refractory autoimmune cytopenias: results of a prospective multi-institutional trial. Blood. 2016;127:17–28.
Ji L, Xie W, Zhang Z. Efficacy and safety of sirolimus in patients with systemic lupus erythematosus: a systematic review and meta-analysis. Semin Arthritis Rheum. 2020;50:1073–80.
Niu HQ, Li ZH, Zhao WP, Zhao XC, Zhang C, Luo J, et al. Sirolimus selectively increases circulating Treg cell numbers and restores the Th17/Treg balance in rheumatoid arthritis patients with low disease activity or in DAS28 remission who previously received conventional disease-modifying anti-rheumatic drugs. Clin Exp Rheumatol. 2020;38:58–66.
Long Z, Yu F, Du Y, Li H, Chen M, Zhuang J, et al. Successful treatment of refractory/relapsed acquired pure red cell aplasia with sirolimus. Ann Hematol. 2018;97:2047–54.
Teachey DT, Greiner R, Seif A, Attiyeh E, Bleesing J, Choi J, et al. Treatment with sirolimus results in complete responses in patients with autoimmune lymphoproliferative syndrome. Br J Haematol. 2009;145:101–6.
Li JM, Wang ZY, Dai L, Cao LJ, Su J, Zhu MQ, et al. Effects of rapamycin combined with low dose prednisone in patients with chronic immune thrombocytopenia. Clin Dev Immunol. 2013;2013:548085.
Klemann C, Esquivel M, Magerus-Chatinet A, Lorenz MR, Fuchs I, Neveux N, et al. Evolution of disease activity and biomarkers on and off rapamycin in 28 patients with autoimmune lymphoproliferative syndrome. Haematologica. 2017;102:e52–6.
Feng YM, Xiao YS, Yan HJ, Wang P, Zhu W, Cassady K, et al. Sirolimus as rescue therapy for refractory/relapsed immune thrombocytopenia: results of a single-center, prospective, single-arm study. Front Med-Lausanne. 2020;7:110.
Li HM, Ji J, Du YL, Huang YZ, Gu H, Chen M, et al. Sirolimus is effective for primary relapsed/refractory autoimmune cytopenia: a multicenter study. Exp Hematol. 2020;89:87–95.
Masuda M, Teramura M, Matsuda A, Bessho M, Shimamoto T, Ohyashiki K, et al. Clonal T cells of pure red-cell aplasia. Am J Hematol. 2005;79:332–3.
Miano M, Poggi V, Banov L, Fioredda F, Micalizzi C, Svahn J, et al. Sirolimus as maintenance treatment in an infant with life-threatening multiresistant pure red cell anemia/autoimmune hemolytic anemia. J Pediatr Hematol/Oncol. 2014;36:e145–8.
Miano M, Calvillo M, Palmisani E, Fioredda F, Micalizzi C, Svahn J, et al. Sirolimus for the treatment of multi-resistant autoimmune haemolytic anaemia in children. Br J Haematol. 2014;167:571–4.
Jiang H, Zhang H, Wang Y, Qi W, Cao Q, Xing L, et al. Sirolimus for the treatment of multi-resistant pure red cell aplasia. Br J Haematol. 2019;184:1055–8.
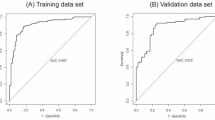
Chen S, Chen S, Lian G, Li Y, Ye X, Zou J, et al. Development and validation of a novel nomogram for pretreatment prediction of liver metastasis in pancreatic cancer. Cancer Med. 2020;9:2971–80.
Huang Y, Jiang X, Han B. Effective treatment of refractory acquired pure red blood cell aplasia with eltrombopag and sirolimus: a case report. Ther Adv Hematol. 2020;11:2040620720940144.
Feng XM, Lin ZH, Sun WL, Hollinger MK, Desierto MJ, Keyvanfar K, et al. Rapamycin is highly effective in murine models of immune-mediated bone marrow failure. Haematologica. 2017;102:1691–703.
Ghosh P, Buchholz MA, Yano S, Taub D, Longo DL. Effect of rapamycin on the cyclosporin A-resistant CD28-mediated costimulatory pathway. Blood. 2002;99:4517–24.
Chen ZS, Chen M, Yang C, Han B. Immunosuppression therapy is effective for both acquired tumor-associated and primary pure red cell aplasia: a match pair case-control study. Ann Hematol. 2020;99:1485–91.
Kawakami T, Sekiguchi N, Kobayashi J, Imi T, Matsuda K, Yamane T, et al. Frequent STAT3 mutations in CD8(+) T cells from patients with pure red cell aplasia. Blood Adv. 2018;2:2704–12.
Fu R, Zhang T, Liu B, Song J, Wang G, Li L, et al. The clinical characteristics and therapy response of patients with acquired pure red cell aplasia. Hematology. 2018;23:639–45.
Cazzola M, Della Porta MG, Malcovati L. Clinical relevance of anemia and transfusion iron overload in myelodysplastic syndromes. Hematology Am Soc Hematol Educ Program. 2008;1:166–75.
Funding
This study was supported by grants from CAMS Innovation Fund for Medical Sciences (CIFMS 2021-I2M-1-003), National Natural Science Foundation of China (NSFC 81970106).
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This prospective study was approved by the Ethics Committee of PUMCH and registered at clinicaltrial.gov (NCT03364764). All eligible patients were fully informed of this study and signed written informed consent to agree to their participation.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, Y., Chen, M., Yang, C. et al. Sirolimus is effective for refractory/relapsed/intolerant acquired pure red cell aplasia: results of a prospective single-institutional trial. Leukemia 36, 1351–1360 (2022). https://doi.org/10.1038/s41375-022-01532-1
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-022-01532-1
This article is cited by
-
Sirolimus modulates the erythroid differentiation of K562 cells by upregulating SHP1
Annals of Hematology (2025)
-
Refractory pure red cell aplasia associated with T-cell large granular lymphocyte leukemia treated by ruxolitinib
Annals of Hematology (2024)
-
A nomogram model for predicting the efficacy of cyclosporine in patients with pure red cell aplasia
Annals of Hematology (2024)
-
Sirolimus versus cyclosporine A in patients with primary acquired pure red cell aplasia: a prospective cohort study
Blood Cancer Journal (2023)