Abstract
Brexucabtagene autoleucel (brexu-cel) is an autologous anti-CD19 CAR T-cell therapy approved in the US to treat adults aged ≥18 years (≥26 years in the EU) with relapsed/refractory (R/R) B-cell acute lymphoblastic leukemia (B-ALL). Brexu-cel showed an overall complete remission (CR)/CR with incomplete hematologic recovery (CRi) rate of 73% (CR rate 60%) and median overall survival (OS) of 25.4 months in 78 patients with R/R B-ALL after 2 years in ZUMA-3. Here, we report updated outcomes after >3 years median follow-up. As of July 23, 2022, median follow-up in all patients (N = 78) was 41.6 months. Median OS (95% CI) was 25.6 months (1.2-47.0; N = 78) and was 38.9 months (25.4–not estimable) for responders (n = 58), with 9 patients in ongoing remission without subsequent therapies. Five deaths (none deemed brexu-cel–related) occurred since prior data cut. Benefits from brexu-cel were maintained regardless of age, prior therapies, and subsequent allogeneic stem cell transplantation (alloSCT). Subsequent alloSCT was not associated with survival benefit among responders versus responders without subsequent alloSCT. No secondary T-cell malignancies were reported in ZUMA-3 with long-term follow-up.

Similar content being viewed by others
Introduction
Targeted treatments, including blinatumomab and inotuzumab ozogamicin, have improved outcomes for adults with relapsed or refractory (R/R) B-cell acute lymphoblastic leukemia (B-ALL) in recent years, with overall complete remission (CR)/CR with incomplete hematologic recovery (CRi) rates of 44% for blinatumomab and 74% for inotuzumab; however, long-term survival remains low, with a median overall survival (OS) < 8 months following these therapies (median follow-up time: 11.7 and 29.6 months for blinatumomab and inotuzumab, respectively) [1, 2]. Following salvage therapy, patients in remission may receive consolidative allogeneic hematopoietic stem cell transplant (alloSCT), which has curative potential in some patients with B-ALL [3]. However, alloSCT can result in serious toxicities such as graft-versus-host disease, limiting the number of patients who can tolerate it, and matched stem cell donors can be difficult to locate in a timely fashion [3, 4]. Given the barriers to alloSCT, less than half of patients treated with inotuzumab in the INO-VATE study or blinatumomab in the TOWER study received potentially curative alloSCT [1, 2]. Thus, other salvage therapies with curative potential are needed for patients with R/R B-ALL. More recently, CD19-directed chimeric antigen receptor (CAR) T-cell therapies have been approved for R/R B-ALL, including tisagenlecleucel (approved in the United States [US] and European Union for patients aged <26 years) and brexucabtagene autoleucel (brexu-cel; approved in the US for patients aged ≥18 years and in the EU for patients aged ≥26 years), that have improved median OS in this patient population [5, 6]. Another anti-CD19 CAR T-cell therapy, obecabtagene autoleucel, is currently being investigated in adult patients with R/R B-ALL [7].
In the multicenter, single-arm, Phase 1/2 ZUMA-3 study, patients with R/R B-ALL (N = 78) treated with brexu-cel at the pivotal dose (1 ×106 CAR T cells/kg) had a CR/CRi rate of 73% and a CR rate of 60% [6]. After 2 years of follow-up, the median OS was 25.4 months (95% confidence interval [CI]: 16.2–not estimable [NE]) in all treated patients and 47.0 months (95% CI: 23.2–NE) in responders (n = 57) [6]. Outcomes by baseline bone marrow (BM) blast percentage were largely consistent with the overall population, though patients with >75% BM blasts at baseline had numerically lower CR/CRi rates and median OS [6]. Additionally, a post hoc subgroup analysis performed after 2 years of follow-up found that patients in ZUMA-3 benefited from brexu-cel irrespective of prior therapies or subsequent alloSCT status [8]. However, survival appeared numerically higher in patients who received fewer previous lines of therapy and in patients who did not receive blinatumomab or inotuzumab as prior therapies, though unmatched baseline characteristics and small patient numbers may have contributed to these results [8].
Here, we report outcomes after 3 years of follow-up in all treated patients and those aged ≥26 years (the EU patient population) in ZUMA-3, with updated results for subgroups of patients who received blinatumomab, inotuzumab, or alloSCT as prior therapy as well as those responders who received subsequent alloSCT.
Methods
Study design and patients
Full methodology for the ZUMA-3 was previously reported [9]. Briefly, ZUMA-3 was a single-arm, multicenter, Phase 1/2 study (NCT02614066). Eligible patients were aged ≥18 years with R/R B-ALL (>5% blasts in the BM). Prior alloSCT was allowed if conducted ≥100 days before enrollment and immunosuppressive medication was discontinued ≥4 weeks before enrollment. Prior blinatumomab was permitted if patients had documented CD19 tumor expression from BM or circulating blasts following completion of prior line of therapy. If CD19 tumor expression was quantified, then ≥90% CD19-positive blasts were required for inclusion. The study protocol was approved by the institutional review board or independent ethics committee at each site, all patients provided written informed consent, and the study was conducted in accordance with the principles of the Declaration of Helsinki [9].
Procedures
Patients in ZUMA-3 underwent leukapheresis and conditioning chemotherapy (intravenous fludarabine 25 mg/m2 on days −4, −3, and −2; and intravenous cyclophosphamide 900 mg/m2 on day −2), followed by one infusion of brexu-cel at a target dose of 1 × 106 CAR T cells/kg on Day 0 [9]. Subsequent consolidative alloSCT was allowed following brexu-cel, at physician’s discretion but was not protocol-defined [9].
Outcomes
The primary endpoint for ZUMA-3 was overall CR/CRi rate per independent review. Secondary endpoints included overall CR/CRi rate per investigator review, duration of remission (DOR) and relapse-free survival (RFS; patients without CR/CRi by data cutoff were evaluated as having an RFS event at day 0) with patients undergoing subsequent anticancer therapies, including alloSCT, censored (Philadelphia chromosome-positive [Ph+] patients who achieved CR could receive maintenance tyrosine kinase inhibitor [TKI] therapy 2 months after infusion without censoring for subsequent therapy); OS; rate of alloSCT; and safety. Patients began the long-term follow-up period after the month 3 visit and were followed for survival and disease status, if applicable, every 3 months through the month 18 visit and then every 6 months through the month 60 visit. Disease assessment was performed per independent review through the month 24 visit or until disease progression. Disease assessment after the month 24 visit for patients’ whose disease had not progressed was performed per standard of care via investigator assessment. To have all disease assessments up to date in this analysis, remission rates, DOR, and RFS are reported herein by investigator review. An exploratory translational endpoint was CAR T-cell levels in the blood. Additional outcomes reported herein include outcomes of responders who proceeded to subsequent alloSCT, cumulative incidence of progressive-disease (PD) mortality and non-PD mortality, and reasons for non-PD mortality.
Statistical analyses
Updated ZUMA-3 endpoints are reported in Phase 2-treated patients aged ≥18 years and in pooled Phase 1 and 2 patients (including patients aged ≥26 years) treated with the pivotal dose, 1 × 106 CAR T cells/kg. Analyses of OS are also reported in all enrolled patients. Exploratory post hoc subgroup efficacy and safety assessments were performed for patients who did and did not receive prior blinatumomab, inotuzumab, and/or alloSCT [8]. Post hoc subgroup analyses by receipt of subsequent alloSCT were also performed [8]. Subgroup analyses were conducted retrospectively, with inherent differences in sample sizes and baseline characteristics; no hypotheses were tested and only descriptive statistics are reported. Time-to-event endpoints were analyzed using the Kaplan–Meier method.
Results
Patients
Manufacturing details in Phase 1 and Phase 2 were previously reported [9, 10]. Notably, the median time from leukapheresis to brexu-cel manufacturing release for Phase 2 US patients was 13 days (interquartile range [IQR], 11–14), and the median time from leukapheresis to brexu-cel delivery to study site for Phase 1 US patients was 15 days (IQR, 14–16) [9, 10]. As of July 23, 2022, the median follow-up time for all treated patients was 41.6 months (range, 32.7–70.3; N = 78), for Phase 1 and 2 patients aged ≥26 years it was 41.6 months (range, 32.7–70.3; N = 63); and for all Phase 2 patients it was 38.8 months (range, 32.7–44.6; N = 55). Baseline characteristics were previously reported and were largely consistent across these three patient populations [8, 9, 11]. Briefly, for all treated patients, the median age was 42.5 years (range, 18–84), the median number of prior therapies was 2 (range, 1–8), the proportion of patients with >25% BM blasts at baseline was 72%, 22% were Ph+, and the proportion of patients with Eastern Cooperative Oncology Group performance status (ECOG PS) 1 was 72% (Supplementary Table S1) [8]. The median age for Phase 1 and 2 patients aged ≥26 years was 47 years (range, 26–84), the median number of prior therapies was 2 (range, 1–8), the proportion of patients with >25% BM blasts at baseline was 67%, 25% were Ph+, and the proportion of patients with ECOG PS 1 was 71% [11]. The median age for Phase 2 treated patients was 40 years (range, 19-84; N = 55), the median number of prior therapies was 2 (range, 1–8), the proportion of patients with >25% BM blasts at baseline was 73%, 26% were Ph+, and the proportion of patients with ECOG PS 1 was 71% [9].
As previously reported, most Phase 1 patients (96%) and Phase 2 treated patients (93%) received bridging chemotherapy prior to brexu-cel infusion, with the most common chemotherapy (>20%) being dexamethasone (49%), non-liposomal vincristine (37%), cytarabine (28%), and liposomal vincristine (21%; patients could have received more than one type of bridging chemotherapy) [9, 10]. A total of 38 patients (49%) aged ≥18 years had prior blinatumomab exposure, 17 (22%) had prior inotuzumab exposure, and 29 (37%) had prior alloSCT [8]. Additionally, 15 patients (19%) aged ≥18 years proceeded to subsequent alloSCT while in response following brexu-cel, of which 14 patients had CR/CRi and 1 had partial remission [8].
Baseline patient characteristics for prior treatment subgroups were previously reported in patients aged ≥18 years [8]. Briefly, patients with prior blinatumomab had a median of 3 prior therapies, whereas patients without prior blinatumomab had a median of 2 prior therapies (Supplementary Table S1) [8]. Additionally, patients with prior blinatumomab had a numerically higher BM blast percentage at baseline (70%) versus patients without prior blinatumomab (54%; Supplementary Table S1) [8]. Patients with prior inotuzumab also had a higher median number of prior therapies (3 vs 2) and BM blast percentage at baseline (76% vs 52%) than patients without prior inotuzumab (Supplementary Table S1) [8]. Patients with prior alloSCT had a higher median number of prior therapies versus patients without prior alloSCT (3 vs 2), but both groups had similar baseline BM blast percentages (Supplementary Table S1) [8].
Baseline patient characteristics for responders aged ≥18 years who did or did not proceed to subsequent alloSCT were also previously reported [8]. Responders who proceeded to subsequent alloSCT had fewer median prior therapies (2 vs 3) and lower baseline BM blast percentage than responders who did not (Supplementary Table S2) [8]. Additionally, responders who proceeded to subsequent alloSCT were more likely to be primary refractory (43% vs 28%) and were less likely to have been R/R after prior alloSCT (7% vs 51%; Supplementary Table S2) [8].
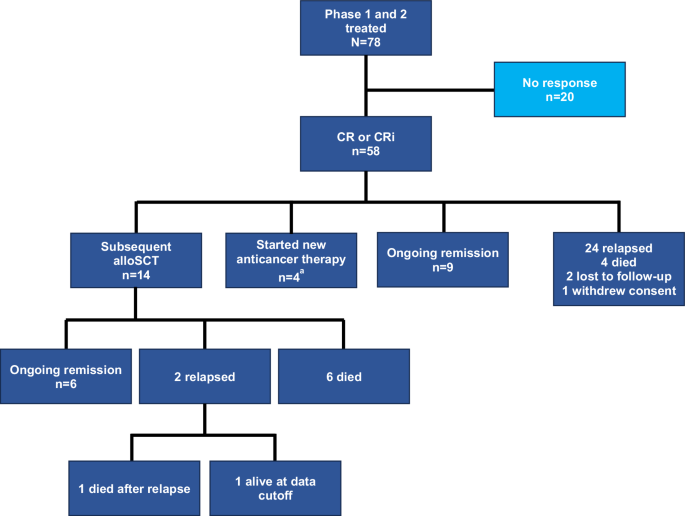
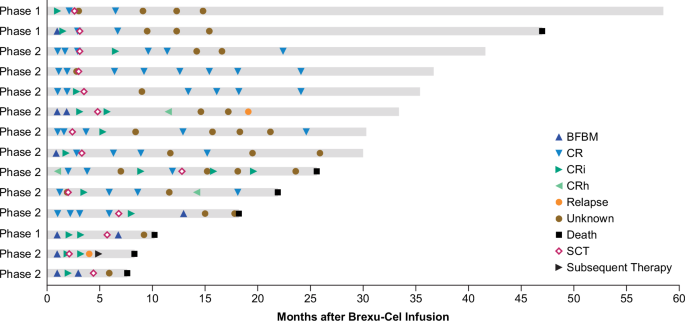
Efficacy update
Consistent with the primary analysis, the overall CR/CRi and CR rates per investigator review of all treated patients (N = 78) in this analysis were 74% and 63%, respectively (Table 1) [9]. The median DOR with censoring at subsequent therapy including alloSCT (maintenance TKI therapy was not considered subsequent therapy) was 14.6 months (n = 58; 95% CI, 9.4–23.6; Supplementary Fig. S1A). Of the 58 CR/CRi, 24 relapsed; 14 proceeded to subsequent alloSCT, 9 were in ongoing remission without additional therapy; 4 started new anticancer therapy in remission (reasons for starting subsequent therapy: 2 patients were minimal residual disease (MRD)-positive; 1 patient withdrew partial study consent then relapsed per bone marrow biopsy carried out by investigator prior to starting new anticancer therapy; and 1 started new anticancer therapy prior to formal relapse owing to a measurement of rising MRD by clonoSEQ®); 4 died (n = 1 each of progressive disease, graft versus host disease, COVID-19, and missing cause of death); 2 were lost to follow-up; and 1 had withdrawn consent as of the data cutoff date (Fig. 1). Of the 58 patients with CR/CRi per investigator review, 14 were Ph+ at baseline, of whom, 4 patients (29%) started TKI therapy without being censored as permitted by study protocol. One of these patients subsequently died without relapse; 1 patient subsequently relapsed and died; one patient had subsequent alloSCT shortly after TKI start and was censored at last disease assessment per study protocol, prior to TKI start; and 1 patient remained in ongoing remission without additional therapy as of data cutoff. Among responders aged ≥26 years (n = 47), the median DOR, with censoring at subsequent therapy including alloSCT, was 13.7 months (95% CI: 9.4–24.1; Supplementary Table S3; Supplementary Fig. S1B). The median DOR was 13.7 months (95% CI: 8.7–23.6; Supplementary Fig. S1C) among responders in Phase 2 (n = 40). Similar to previously reported results for Phase 2 patients, the best overall MRD-negative rate at any visit among all treated patients was 79% (95% CI: 69–88; N = 78) and 98% among responders (95% CI: 91–100; n = 58) [9]. In Phase 1 and 2 patients aged ≥26 years, the best overall MRD-negative rate at any visit was 81% (95% CI: 69–90; n = 63) and 100% among responders (95% CI: 92–100; n = 47).
In all treated patients, the median RFS, with censoring at subsequent therapy including alloSCT, was 11.6 months (N = 78; 95% CI: 6.0–15.5; Supplementary Fig. S2A). In patients aged ≥26 years, the median RFS, with censoring at subsequent therapy including alloSCT, was 11.6 months (n = 63; 95% CI: 3.2–14.8; Supplementary Fig. S2B) and was 11.6 months in Phase 2 patients (n = 55; 95% CI: 2.8–15.5; Supplementary Fig. S2C).
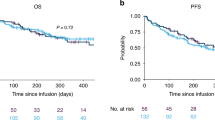
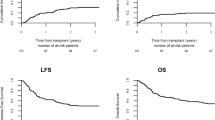
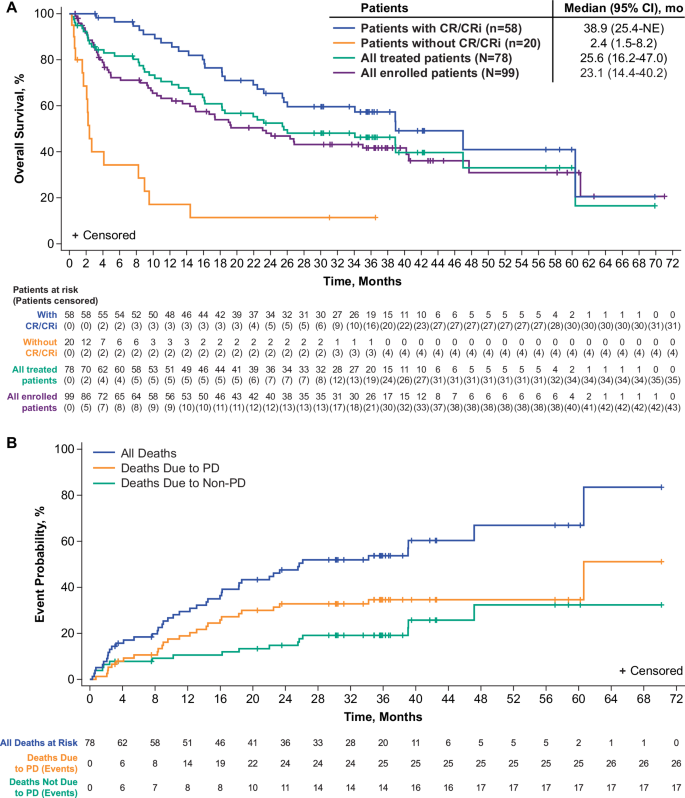
The median OS was 25.6 months (95% CI: 16.2–47.0) for all treated patients (n = 78) and 38.9 months (95% CI: 25.4–NE) for responders per investigator review (n = 58; Fig. 2A), with 28 patients (36%; 26 responders) alive on or after data cutoff. In patients aged ≥26 years, the median OS was 26.0 months (95% CI: 15.9–60.4; Supplementary Fig. S3A) for all treated patients (n = 63) and 47.0 months (95% CI: 25.4–NE) for responders per investigator review (n = 47). In all treated Phase 2 patients (n = 55), the median OS was 26.0 months (95% CI: 16.2–NE; Supplementary Fig. S3C) and 38.9 months (95% CI: 25.4–NE) in responders per investigator review (n = 40). Among all enrolled patients at the pivotal dose, median OS was 23.1 months (95% CI, 14.4–40.2; Fig. 2A) for Phase 1 and 2 patients aged ≥18 years (N = 99); 23.1 months (95% CI, 13.5–47.7; Supplementary Fig. S3B) in patients aged ≥26 years (N = 81); 23.1 months (95% CI, 10.4–40.5; Supplementary Fig. S3D) Phase 2 patients (N = 71).
Cumulative incidence of cause-specific mortality
The 36-month rate of non-PD mortality for all treated patients was 19% (n = 15) and the 36-month rate of PD mortality was 35% (n = 27; Fig. 2B). At data cutoff, there were 17 patients with non-PD mortality; 1 death was determined to be brexu-cel–related (brain herniation on Day 8), 1 death was determined to be related to both brexu-cel and lymphodepleting chemotherapy (septic shock on Day 18), and 15 deaths were deemed unrelated to brexu-cel. The most common causes of non-PD mortality included graft versus host disease (n = 3; Days 554, 773 and 1429), sepsis (n = 2; Days 50 and 72), and pneumonia (n = 2; Days 15 and 46), with 6 deaths having occurred in patients who received subsequent alloSCT (Supplementary Table S4).
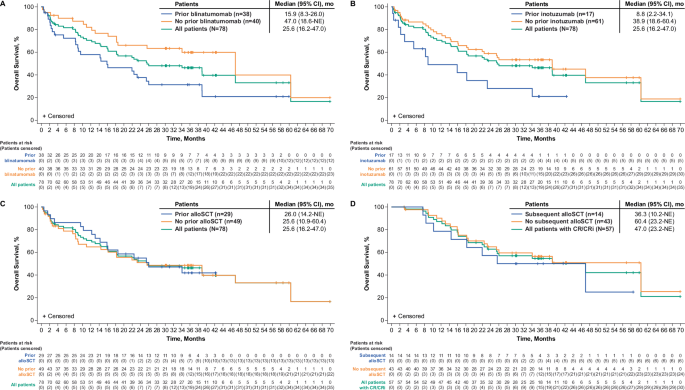
Survival update in key subgroups
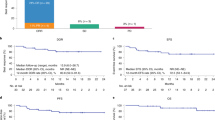
Consistent with previous reports, the median OS for all treated patients with prior blinatumomab exposure (n = 38) was 15.9 months (95% CI: 8.3–26.0), and was 47.0 months (95% CI: 18.6–NE) for patients without prior blinatumomab exposure (n = 40) (Fig. 3A); however, differences in median number of prior therapies and other baseline characteristics may have confounded these results [8]. Trends for median OS also remained consistent with prior reports for all treated patients with prior inotuzumab exposure (n = 17) at 8.8 months (95% CI: 2.2–34.1) and 38.9 months (95% CI: 18.6–60.4) for those without prior inotuzumab exposure (n = 61; Fig. 3B) [8]. With longer follow-up, the median OS estimates for patients with and without prior alloSCT were similar at 26.0 months (n = 29; 95% CI, 14.2–NE) and 25.6 months (n = 49; 95% CI: 10.9–60.4), respectively (Fig. 3C), whereas estimated medians for patients without prior alloSCT appeared higher in a previous report [8].
Kaplan-Meier estimates of overall survival by (A) prior blinatumomab exposure, (B) prior inotuzumab exposure, (C) prior alloSCT exposure, and (D) subsequent alloSCT exposure. alloSCT allogeneic stem cell transplant, CI confidence interval, CR complete remission, CRi complete remission with incomplete hematologic recovery, NE not estimable.
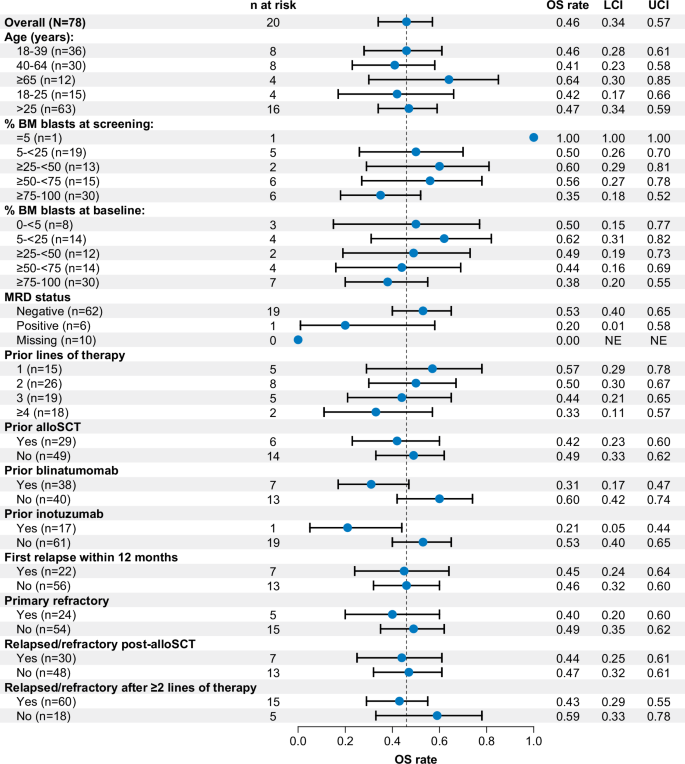
OS rates at 36 months for most key subgroups were largely similar to the overall population (46%; 95% CI: 34–57). Notably, the 36-month OS rates by bone marrow blast percentage at baseline and age categories were similar to that of all patients, but was lower for patients who received blinatumomab (31%; 95% CI, 17–47) or inotuzumab (21%; 95% CI, 5–44) as prior therapy, and was lower among patients who had ≥4 prior therapies (33%; 95% CI, 11–57; Fig. 4). Rates of OS at 36 months among patients aged ≥26 years and Phase 2 patients were similar to those for all treated patients (Supplementary Figs. S4 and S5).
Outcomes after subsequent alloSCT
As previously reported, 14 patients with CR/CRi proceeded to subsequent alloSCT while in remission following brexu-cel [8]. Of these patients, 10 had CR as best response and 4 had CRi, with a total median time from brexu-cel infusion of 114 days (range, 78–175) for Phase 1 patients and 101 days (range, 60–390) for Phase 2 patients. As expected and consistent with the 2-year data cut, responders who received subsequent alloSCT (n = 14) and responders who did not receive subsequent alloSCT (n = 43) experienced a numerically longer median OS compared with the overall patient population. However, responders with subsequent alloSCT appeared to experience less benefit with a median OS reached at 36.3 months (95% CI: 10.2–NE; n = 14), whereas responders without subsequent alloSCT had a median OS of 60.4 months (95% CI: 23.2–NE; n = 43 Fig. 3D) [8]. Of the 14 responders who proceeded to subsequent alloSCT, 6 were in ongoing remission at data cutoff, 2 relapsed (1 patient died after relapse), and 6 died without relapse (Fig. 5; n = 1 each of hypoxia on Day 778; hemorrhagic shock due to gastrointestinal bleed on Day 231; herpes simplex viremia on Day 309; multi-organ failure due to infection and graft versus host disease on Day 554; cardiopulmonary arrest on Day 667; and pulmonary graft versus host disease on Day 1429). Median OS results were largely consistent across all subgroups examined among Phase 1 and 2 patients aged ≥26 years and Phase 2 patients (prior blinatumomab: Supplementary Figs. S6A and S7A; prior inotuzumab: Supplementary Figs. S6B and S7B; prior alloSCT: Supplementary Figs. S6C and S7C; subsequent alloSCT: Supplementary Figs. S6D and S7D, respectively).
alloSCT allogeneic stem cell transplant, BFBM blast-free hypoplastic or aplastic bone marrow, brexu-cel brexucabtagene autoleucel, CR complete remission, CRh complete remission with partial hematological recovery, CRi complete remission with incomplete hematological recovery, SCT stem cell transplantation.
Safety update
Safety outcomes for patients in ZUMA-3 after 3 years of follow-up remained largely consistent with previous reports [6]. Brexu-cel–related treatment-emergent adverse events (TEAEs) remained unchanged, and no Grade 5 adverse events occurred since the prior data cut in Phase 1 and 2 patients (N = 78). No new incidence of cytokine release syndrome (CRS), neurologic events, infections, or hypogammaglobulinemia of any grade were reported since the prior data cut. As previously reported, one patient had a secondary malignancy of ongoing Grade 4 myelodysplastic syndrome at data cutoff [9]. Two additional events among 1 patient (Grade 1 and 2 leukemic retinopathy, both resolved with treatment) were previously reported as secondary malignancies but were subsequently recategorized as leukemic retinopathy as a manifestation of the underlying B-ALL (or leukemia) diagnosis [9]. None of these events were T-cell malignancies or deemed related to brexu-cel per investigator assessment [9].
Brexu-cel–related TEAEs, CRS, and neurologic events were largely consistent across prior therapy subgroups. However, patients without prior blinatumomab experienced Grade ≥3 CRS at a numerically lower rate and Grade ≥3 neurologic events at a numerically higher rate than patients with prior blinatumomab. Patients without prior inotuzumab and patients with prior alloSCT experienced Grade ≥3 CRS at lower rates than their respective counterparts (Table 2). Of the 43 patients treated in Phase 1 and 2 who died, 5 deaths occurred since the prior data cutoff due to the following causes, none of which were determined to be brexu-cel–related: progressive disease (n = 2; Day 1036 and Day 1837), hypoxia with acute respiratory distress syndrome and accompanying hypotension (n = 1; Day 778), intracranial hemorrhage deemed related to relapsed ALL with thrombocytopenia and possible central nervous system involvement (n = 1; Day 1183), missing cause of death (n = 1; Day 1184) [12].
Pharmacokinetics update
Consistent with previous ZUMA-3 analyses, median peak and area under the curve from Day 0 to Day 28 (AUC0‑28) anti‑CD19 CAR T‑cell levels were higher in evaluable pooled Phase 1 and 2 patients with ongoing remission (n = 7; median peak, 62.97 cells/μL [range, 21.89–83.99]; median AUC0-28, 698.13 cells/μL×days [range, 185.75–1122.59]) compared with patients who relapsed or died after achieving remission (n = 19; median peak, 23.26 cells/μL [range, 2.18–322.24]; median AUC0-28, 263.13 cells/μL×days [range, 15.29–2624.52]) and non-responders (n = 18; median peak, 2.45 cells/μL [range, 0.00–183.50]; median AUC0-28, 32.08 cells/μL×days [range, 0.00–642.25]; Table 3) [8, 12]. Patients who had alloSCT, started new anticancer therapy, withdrew consent, or were lost to follow-up at data cutoff were not included in this analysis. Similar to results previously reported for Phase 2 patients, of the 9 Phase 1 and 2 patients with ongoing remission, 8 were evaluable for B cell recovery. At 6 months post-infusion, 7 of 8 patients had full B cell recovery, and all 8 evaluable patients had full B cell recovery by Year 1, with no detectable anti-CD19 CAR T cells [12].
Discussion
After 3.5 years of median follow-up in ZUMA-3, patients continued to benefit from brexu-cel therapy, with a median OS of almost 4 years in 58 responders, including 9 patients who were still in ongoing remission without subsequent therapy or alloSCT at data cutoff. Additionally, consistent with prior reports, overall MRD negativity rate was high among responders (98%), which has previously been shown to be associated with longer OS across many studies of adult patients with B-ALL [9, 10, 13]. OS rates at 36 months and median OS across key subgroups were generally similar although patients who received prior blinatumomab or inotuzumab had numerically lower 36-month OS rates and medians relative to the overall population. However, as discussed in a previous analysis, these results may be confounded by differences in baseline characteristics such as number of prior therapies and small sample sizes. For example, patients with prior blinatumomab had a higher disease burden at baseline (70% vs 54% BM blasts) and more prior therapies (median 3 vs 2) versus patients with no prior blinatumomab [8]. Similarly, patients with prior inotuzumab treatment had a higher disease burden and more prior therapies than patients without prior inotuzumab, along with a small sample size of patients treated with prior inotuzumab (n = 17) [8]. Recent reports of patients treated with brexu-cel with and without prior blinatumomab treatment in real-world settings have shown high CR/CRi rates and OS rates at 6 months or 1 year regardless of prior treatment status [14, 15]. Interestingly, in one real-world study, patients who did not respond to prior blinatumomab treatment had a lower 1-year OS rate following brexu-cel therapy versus patients with response to prior blinatumomab treatment or blinatumomab-naive patients [14]. However, we previously reported that responses to brexu-cel in ZUMA-3 were observed regardless of best response to prior blinatumomab therapy. As such, more studies are needed to determine the impact prior blinatumomab and response to prior blinatumomab on efficacy of brexu-cel, but there were patients with prior blinatumomab treatment in both ZUMA-3 and in the real-world analysis who experienced significant benefit from subsequent brexu-cel therapy [16].
Responders (n = 43) who did not proceed to subsequent alloSCT had a numerically higher median OS than responders who proceeded to subsequent alloSCT suggesting that patients who respond to brexu-cel may experience long-term survival regardless of whether they receive consolidation therapy in the form of alloSCT. As previously stated, baseline patient characteristics between subgroups were not balanced, though responders without subsequent alloSCT had a numerically higher median number of prior therapies, numerically higher median BM blasts at baseline, and were numerically more likely to have had prior alloSCT than responders who proceeded to subsequent alloSCT [8]. It is also important to note that 6 of 14 responders (43%) who proceeded to subsequent alloSCT died due to non-PD events, 2 of whom died due to graft versus host disease. Additionally, 35% of all non-PD mortality events (n = 6) occurred in patients who proceeded to subsequent alloSCT. Rates of treatment-related mortality for consolidative alloSCT after CAR T-cell therapy were high (29–35%) in 2 other studies of CAR T-cell therapy in patients with R/R B-ALL, but these also examined small sample sizes (n = 17–21) [17, 18]. Given the small patient numbers in each subgroup and the lack of balanced patient characteristics between responders who did or did not proceed to subsequent alloSCT in ZUMA-3, it is difficult to fully assess the risks and benefits of consolidative alloSCT after brexu-cel treatment. However, given responders without subsequent alloSCT had a median OS of ~5 years, it is clear that long-term remissions can be established without subsequent alloSCT. These results provide support for additional studies with more patients to assess the risks and benefits of consolidative alloSCT following CAR T-cell therapy in R/R ALL.
There were no new safety signals and no new AEs of interest among patients in ZUMA-3 since the prior data cut. This is consistent with the one-time administration of brexu-cel and has been demonstrated in long-term follow-up of other CAR T-cell therapies [5, 19]. Of the 5 deaths that occurred since the previous analysis, none were determined to be related to brexu-cel. Safety outcomes were also largely consistent across patient subgroups, although patients without prior blinatumomab or inotuzumab treatment, as well those with prior alloSCT, experienced fewer Grade ≥3 CRS events. This may be related to the lower disease burden at baseline and smaller number of prior therapies observed in these patient subgroups versus patients with prior blinatumomab or inotuzumab treatment and patients without prior alloSCT [8]. Conversely, patients without prior blinatumomab experienced higher rates of Grade ≥3 NEs for reasons that remain unclear. As noted above, differences in baseline characteristics and number of prior therapies in these subgroups limit interpretation of these results and more studies are needed to fully understand the impact prior therapies may have on adverse events experienced with subsequent brexu-cel therapy.
Given the EU’s approval of brexu-cel is limited to patients aged ≥26 years with R/R B-ALL, we assessed the efficacy and safety outcomes of patients ≥26 years (n = 63) in this follow-up analysis. This patient population benefitted from brexu-cel therapy with outcomes comparable to the overall ZUMA-3 population, suggesting that patients can benefit from brexu-cel treatment regardless of age.
Consistent with previous reports, median peak CAR T-cell levels were higher in ongoing responders versus patients who relapsed or non-responders, suggesting that these parameters may be an early indicator of long-term durability of remissions [6, 8]. As has been suggested previously, the B-cell recovery and lack of detectable CAR T cells in ongoing responders suggest that persistence of CAR T cells in blood is not necessary for maintaining remission after brexu-cel therapy [6]. A prior analysis examined median peak and area under the curve from time of infusion to Day 28 CAR T-cell levels among patients who received prior blinatumomab or inotuzumab treatment versus those who did not. No significant differences in either metric were observed between patients who did or did not receive either of these prior treatments, suggesting that prior targeted therapy did not significantly lessen anti-CD19 T-cell expansion in patients treated with brexu-cel [8].
Limitations of this study include the single-arm study design of ZUMA-3, small patient numbers in certain subgroups, limited availability of independent review of remissions after 24 months, and unmatched baseline characteristics between corresponding subgroups.
With almost 3.5 years of median follow-up in ZUMA-3, updated results demonstrate that brexu-cel continues to provide benefit for adult patients with R/R B-ALL, including responders without subsequent alloSCT. As of the data cutoff date, 9 patients were in ongoing remission per investigator review without subsequent therapies, including alloSCT, suggesting that brexu-cel therapy can produce long-lasting remissions that extend survival in patients with R/R B-ALL. Brexu-cel demonstrated durable efficacy across key subgroups, though survival appeared better in patients not previously treated with the targeted therapies blinatumomab or inotuzumab. However, unmatched baseline characteristics and small patient numbers among subgroups may have contributed to these results. No new safety signals were identified, and no cases of secondary T-cell malignancies have been reported at any time in ZUMA-3. Additional studies are needed to fully assess the impact of prior and subsequent therapies in patients with R/R B-ALL who receive brexu-cel.
Data availability
Kite, a Gilead Company, is committed to sharing clinical trial data with external medical experts and scientific researchers in the interest of advancing public health, and access can be requested by contacting medinfo@kitepharma.com.
References
Kantarjian HM, DeAngelo DJ, Stelljes M, Liedtke M, Stock W, Gokbuget N, et al. Inotuzumab ozogamicin versus standard of care in relapsed or refractory acute lymphoblastic leukemia: Final report and long-term survival follow-up from the randomized, phase 3 INO-VATE study. Cancer. 2019;125:2474–87.
Kantarjian H, Stein A, Gokbuget N, Fielding AK, Schuh AC, Ribera JM, et al. Blinatumomab versus Chemotherapy for Advanced Acute Lymphoblastic Leukemia. N Engl J Med. 2017;376:836–47.
Aldoss I, Yang D, Malki MMA, Mei M, Mokhtari S, Artz A, et al. Allogeneic Hematopoietic Cell Transplantation for Relapsed and Refractory Philadelphia Negative B Cell ALL in the Era of Novel Salvage Therapies. Transpl Cell Ther. 2021;27:255.e1–e9.
Khaled SK, Thomas SH, Forman SJ. Allogeneic hematopoietic cell transplantation for acute lymphoblastic leukemia in adults. Curr Opin Oncol. 2012;24:182–90.
Laetsch TW, Maude SL, Rives S, Hiramatsu H, Bittencourt H, Bader P, et al. Three-Year Update of Tisagenlecleucel in Pediatric and Young Adult Patients With Relapsed/Refractory Acute Lymphoblastic Leukemia in the ELIANA Trial. J Clin Oncol. 2023;41:1664–9.
Shah BD, Ghobadi A, Oluwole OO, Logan AC, Boissel N, Cassaday RD, et al. Two-year follow-up of KTE-X19 in patients with relapsed or refractory adult B-cell acute lymphoblastic leukemia in ZUMA-3 and its contextualization with SCHOLAR-3, an external historical control study. J Hematol Oncol. 2022;15:170.
Roddie C, Sandhu KS, Tholouli E, Shaughnessy P, Barba P, Guerreiro M, et al. Obecabtagene Autoleucel (obe-cel, AUTO1) for Relapsed/Refractory Adult B-cell Acute Lymphoblastic Leukemia (R/R B-ALL): Pooled Analysis of the Ongoing FELIX Phase Ib/II Study. Blood. 2023;142:222.
Shah BD, Cassaday RD, Park JH, Houot R, Oluwole OO, Logan AC, et al. Impact of prior therapies and subsequent transplantation on outcomes in adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia treated with brexucabtagene autoleucel in ZUMA-3. J Immunother Cancer. 2023;11:e007118.
Shah BD, Ghobadi A, Oluwole OO, Logan AC, Boissel N, Cassaday RD, et al. KTE-X19 for relapsed or refractory adult B-cell acute lymphoblastic leukaemia: phase 2 results of the single-arm, open-label, multicentre ZUMA-3 study. Lancet. 2021;398:491–502.
Shah BD, Bishop MR, Oluwole OO, Logan AC, Baer MR, Donnellan WB, et al. KTE-X19 anti-CD19 CAR T-cell therapy in adult relapsed/refractory acute lymphoblastic leukemia: ZUMA-3 phase 1 results. Blood. 2021;138:11–22.
Minnema MC, Xiang Y, Davi R, Keeping S, Park JE, Itani T, et al. Outcomes of patients aged ≥26 years with relapsed or refractory B-cell acute lymphoblastic leukemia in ZUMA-3 and historical trials. Leuk Lymphoma. 2024;65:1438–47.
Shah BD, Ghobadi A, Oluwole OO, Logan A, Boissel N, Cassaday RD, et al. Two-year follow-up of KTE-X19, an anti-CD19 chimeric antigen receptor (CAR) T-cell therapy, in adult patients (Pts) with relapsed/refractory B-cell acute lymphoblastic leukemia (R/R B-ALL) in ZUMA-3. J Clin Oncol. 2022;40:7010.
Berry DA, Zhou S, Higley H, Mukundan L, Fu S, Reaman GH, et al. Association of Minimal Residual Disease With Clinical Outcome in Pediatric and Adult Acute Lymphoblastic Leukemia: A Meta-analysis. JAMA Oncol. 2017;3:e170580.
Gupta VK, Roloff GW, Muffly LS, Aldoss I, Kopmar NE, Lin C, et al. Impact of Prior Response to Blinatumomab on Outcomes of Brexucabtagene Autoleucel (Brexu-cel) in Adult Patients with Relapsed or Refractory (r/r) B-Cell Acute Lymphoblastic Leukemia (B-ALL): Results from the Real-World Outcomes Collaborative of CAR-T in Adult ALL (ROCCA). Blood. 2023;142:2119.
Bezerra E, Itani T, Wudhikarn K, Perales M-A, Yang Y, Gergis U, et al. Real-World Outcomes of Brexucabtagene Autoleucel (brexu-cel) for Relapsed or Refractory (R/R) Adult B-Cell Acute Lymphoblastic Leukemia (B-cell ALL): Evidence from the CIBMTR Registry. Blood. 2023;142:1029.
Shah BD, Cassaday RD, Park JH, Houot R, Oluwole OO, Logan A, et al. Impact of age, prior therapies, and subsequent transplant on long-term outcomes of adults with relapsed or refractory B-cell acute lymphoblastic leukemia (R/R B-ALL) treated with brexucabtagene autoleucel (brexu-cel) in ZUMA-3. J Clin Oncol. 2023;41:7023.
Park JH, Rivière I, Gonen M, Wang X, Sénéchal B, Curran KJ, et al. Long-Term Follow-up of CD19 CAR Therapy in Acute Lymphoblastic Leukemia. N Engl J Med. 2018;378:449–59.
Shah NN, Lee DW, Yates B, Yuan CM, Shalabi H, Martin S, et al. Long-Term Follow-Up of CD19-CAR T-Cell Therapy in Children and Young Adults With B-ALL. J Clin Oncol : Off J Am Soc Clin Oncol. 2021;39:1650–9.
Neelapu SS, Jacobson CA, Ghobadi A, Miklos DB, Lekakis LJ, Oluwole OO, et al. 5-Year Follow-Up Supports Curative Potential of Axicabtagene Ciloleucel in Refractory Large B-Cell Lymphoma (ZUMA-1). Blood. 2023;141:2307–15.
Lee DW, Gardner R, Porter DL, Louis CU, Ahmed N, Jensen M, et al. Current concepts in the diagnosis and management of cytokine release syndrome. Blood. 2014;124:188–95.
Topp MS, Gökbuget N, Stein AS, Zugmaier G, O’Brien S, Bargou RC, et al. Safety and activity of blinatumomab for adult patients with relapsed or refractory B-precursor acute lymphoblastic leukaemia: a multicentre, single-arm, phase 2 study. Lancet Oncol. 2015;16:57–66.
Acknowledgements
We thank the patients who participated in this trial and their families, caregivers, and friends; the trial investigators, coordinators, and health care staff at each site. Medical writing support was provided by Edward Sheetz, PhD, from Nexus Global Group Science and was funded by Kite, a Gilead Company
Funding
This study was funded by Kite, a Gilead Company.
Author information
Authors and Affiliations
Contributions
Study design: BDS, TH, RDK, AG, OOO. Enrolled and treated patients and collected data: BDS, RDC, JHP, RH, ACL, NB, TL, MiRB, MST, KMO, DT, MLS, MA, MaRB, YL, GJS, MCM, WGW, DJD, PS, DJ, AG, OOO. Performed data analysis: DM, SA, LZ. All authors participated in the analysis and interpretation of data, revising the manuscript, and provided approval of the final submitted version.
Corresponding author
Ethics declarations
Competing interests
BDS reports consulting/advisory role for Adaptive Biotechnologies, Amgen, Autolus, BeiGene, Bristol Myers Squibb, Century Therapeutics, Deciphera, Jazz, Kite, a Gilead Company, Lilly, Novartis, Precision Biosciences, Pfizer, and Takeda; research funding from Jazz Pharmaceuticals, Kite, and Servier; and other relationship with PeproMene Bio. RDC reports employment with and stock or other ownership in Seagen (immediate family member); honoraria from Amgen, Jazz, Kite, a Gilead Company, and Pfizer; consultancy/advisory role for Amgen and Kite; research funding from Amgen, Incyte, Kite, Merck, Pfizer, Servier, and Vanda; travel support from Kite; and other relationship with Autolus (independent review committee), and PeproMene Bio (DSMB). JHP reports consulting/advisory role for AstraZeneca, Kite, a Gilead Company, and Novartis; and research funding from Amgen, Genentech, and Juno. RH reports honoraria from ADC Therapeutics, Bristol Myers Squibb, Celgene, Gilead Sciences, Janssen, Kite, a Gilead Company, MSD, and Novartis; and consulting/advisory role for Kite and Gilead Sciences. ACL reports consulting/advisory role for AbbVie, Actinium, Bristol Myers Squibb, Pfizer, and Takeda; research funding from Amgen, Astellas, Autolus, Kadmon, Kite, a Gilead Company, Pharmacyclics, and Talaris; and other relationship with DSMB: Servier. NB reports honoraria and consulting/advisory role for Amgen, Kite, a Gilead Company, and Novartis; and research funding and expert testimony for Amgen. TL reports honoraria from Amgen, Incyte, Kite, a Gilead Company, and Servier; and consulting/advisory role for Amgen, Incyte, and Servier. MiRB reports honoraria from ADC Therapeutics, Bristol Myers Squibb, Incyte, and Sanofi; consulting/advisory role for Bristol Myers Squibb, Kite, a Gilead Company, Novartis, and Sana Bio; and speakers’ bureau participation for ADC Therapeutics, Bristol Myers Squibb, Incyte, and Sanofi. MST reports consulting/advisory role for AstraZeneca, Bristol Myers Squibb, Genmab, Kite, a Gilead Company, and Roche; research funding from Kite, Regeneron, Roche, and Takeda; and travel support from Janssen and Kite. KMO has no relevant financial relationships to disclose. DT reports consulting/advisory role for and research funding from Bristol Myers Squibb. MLA reports consulting/advisory role for Kite, a Gilead Company and Syndax Pharmaceuticals, Inc.; and research funding from Kite (Institutional PI). YL reports consulting/advisory role for Janssen, Sanofi, NexImmune, Caribou, BMS, Pfizer, Regeneron; research funding from BMS and Jansen. MRB reports research funding from AbbVie, Ascentage, Kite, a Gilead Company, Kura, and Takeda. GJS reports honoraria and research funding from and speakers’ bureau participation for Kite, a Gilead Company. MS reports consulting/advisory role for Amgen, Celgene/Bristol Myers Squibb, Gilead Sciences, Janssen, and Novartis; speakers’ bureau participation for Celgene/Bristol Myers Squibb, Gilead Sciences, Janssen, and Novartis; research funding from Amgen, Gilead Sciences, Miltenyi Biotec, MorphoSys, Roche, and Seagen; and travel support from Takeda. MA reports honoraria from and consulting/advisory role for Celgene; speakers’ bureau participation for AbbVie, Bristol Myers Squibb, Celgene, and Kite, a Gilead Company. MCM reports consulting or advisory role for Bristol Myers Squibb, CDR-life, GSK, and Janssen/Cilag (institution); speakers’ bureau participation for WebMD, Siemens, and Pfizer (institution); and research funding from BeiGene (institution). WGW reports consulting/advisory role for Genzyme and Sanofi; and research funding from AbbVie, Acerta, Cyclacel, Genentech, Gilead Sciences, GSK, Janssen, Juno, Karyopharm, Loxo Oncology, miRagen, Novartis, Oncternal, Pharmacyclics, Sunesis, and Xencor. DJD reports consulting or advisory role for Agios, Amgen, Autolus, Blueprint, Forty-Seven, Gilead Sciences, Incyte, Jazz, Novartis, Pfizer, Shire, and Takeda; and research funding from AbbVie, GlycoMimetics, Novartis, and Blueprint Pharmaceuticals. PS reports honoraria from and consulting or advisory role for MorphoSys and CRISPR Therapeutics; and research funding from Amgen, Gamida Cell, Pfizer, Karyopharm, Gilead Sciences, Incyte, Seagen, and Cellectar. DJ reports research funding from Jazz Pharmaceuticals and Pfizer. DM has no relevant financial relationships to disclose. SA reports employment with and stock or other ownership in Kite, a Gilead Company. LZ reports employment with Kite, a Gilead Company; and stock or other ownership in AbbVie RSU. TH reports employment with, stock, or other ownership in Kite, a Gilead Company. RDK reports employment with, stock or other ownership in, and travel support from Kite, a Gilead Company. AG reports honoraria from Kite, a Gilead Company; consulting/advisory role for Amgen, Atara, Bristol Myers Squibb, CRISPR Therapeutics, Kite, and Wugen Inc.; research funding from Amgen, Genentech, and Kite. OOO reports honoraria from Gilead Sciences and Pfizer; consulting/advisory role for AbbVie, ADC, Cargo, Caribou Biosciences, Epizyme, Gilead Sciences, Kite, a Gilead Company, Nektar, Novartis, Pfizer, and TGR; speakers’ bureau participation for ADC; and research funding from Allogene, Daiichi Sankyo, Kite, and Pfizer.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shah, B.D., Cassaday, R.D., Park, J.H. et al. Three-year analysis of adult patients with relapsed or refractory B-cell acute lymphoblastic leukemia treated with brexucabtagene autoleucel in ZUMA-3. Leukemia 39, 1058–1068 (2025). https://doi.org/10.1038/s41375-025-02532-7
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02532-7
This article is cited by
-
CAR-T-Zell-Therapie bei der akuten lymphoblastischen Leukämie
Die Innere Medizin (2025)
-
The impact of social determinants of health on outcomes of brexucabtagene autoleucel in adults with relapsed/refractory B-cell acute lymphoblastic leukemia
Bone Marrow Transplantation (2025)