Abstract
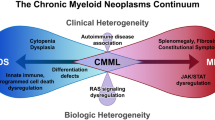
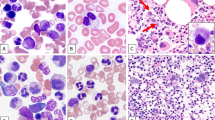
Myelodysplastic syndrome/myeloproliferative neoplasm (MDS/MPN) overlap syndromes are a rare group of biologically and clinically connected hematologic malignancies that includes chronic myelomonocytic leukemia (CMML), the most common subtype, as well as atypical chronic myeloid leukemia, MDS/MPN with SF3B1 and thrombocytosis, and MDS/MPN, not otherwise specified. Given their rarity and overlapping clinical features, accurate diagnosis and risk stratification presents a significant challenge. Therapeutic approaches are largely borrowed from either MDS or MPN and the only curative option for appropriate patients is allogeneic stem cell transplantation. Recent advances have started to uncover the pathobiologic basis for these diseases, leading to novel clinical trials for MDS/MPN overlap syndromes, in particular CMML. This review is a practical guide for the diagnosis and management of MDS/MPN overlap syndromes and presents novel therapeutics being specifically designed for these diseases to improve their historically poor outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka HM, et al. International Consensus Classification of Myeloid Neoplasms and Acute Leukemias: integrating morphologic, clinical, and genomic data. Blood. 2022;140:1200–28.
WHO Classification of Tumours Editorial Board. Haematolymphoid tumours, 5th edn, vol. 11. Lyon (France): International Agency for Research on Cancer; 2024.
Vardiman JW, Harris NL, Brunning RD. The World Health Organization (WHO) classification of the myeloid neoplasms. Blood. 2002;100:2292–302.
Palomo L, Meggendorfer M, Hutter S, Twardziok S, Adema V, Fuhrmann I, et al. Molecular landscape and clonal architecture of adult myelodysplastic/myeloproliferative neoplasms. Blood. 2020;136:1851–62.
Guru Murthy GS, Dhakal I, Mehta P. Incidence and survival outcomes of chronic myelomonocytic leukemia in the United States. Leuk Lymphoma. 2017;58:1648–54.
Mangaonkar AA, Lasho TL, Ketterling RP, Reichard KK, Gangat N, Al-Kali A, et al. Myelodysplastic/myeloproliferative neoplasms with ring sideroblasts and thrombocytosis (MDS/MPN-RS-T): Mayo-Moffitt collaborative study of 158 patients. Blood cancer J. 2022;12:26.
Vardell VA, Ose J, Rets AV, Tantravahi SK, Patel AB. Chronic Myelomonocytic Leukemia and Atypical Chronic Myeloid Leukemia: A National Analysis. Clin Lymphoma Myeloma Leukemia. 2024;24:843–51.
Wang SA, Hasserjian RP, Fox PS, Rogers HJ, Geyer JT, Chabot-Richards D, et al. Atypical chronic myeloid leukemia is clinically distinct from unclassifiable myelodysplastic/myeloproliferative neoplasms. Blood. 2014;123:2645–51.
Elena C, Galli A, Such E, Meggendorfer M, Germing U, Rizzo E, et al. Integrating clinical features and genetic lesions in the risk assessment of patients with chronic myelomonocytic leukemia. Blood. 2016;128:1408–17.
DiNardo CD, Daver N, Jain N, Pemmaraju N, Bueso-Ramos C, Yin CC, et al. Myelodysplastic/myeloproliferative neoplasms, unclassifiable (MDS/MPN, U): natural history and clinical outcome by treatment strategy. Leukemia. 2014;28:958–61.
Prakash S, Arber DA, Bueso-Ramos C, Hasserjian RP, Orazi A. Advances in myelodysplastic/myeloproliferative neoplasms. Virchows Arch. 2023;482:69–83.
Faria C, Tzankov A. Progression in Myeloid Neoplasms: Beyond the Myeloblast. Pathobiology. 2024;91:55–75.
Chen J, Kao YR, Sun D, Todorova TI, Reynolds D, Narayanagari SR, et al. Myelodysplastic syndrome progression to acute myeloid leukemia at the stem cell level. Nat Med. 2019;25:103–10.
Ok CY, Trowell KT, Parker KG, Moser K, Weinberg OK, Rogers HJ, et al. Chronic myeloid neoplasms harboring concomitant mutations in myeloproliferative neoplasm driver genes (JAK2/MPL/CALR) and SF3B1. Mod Pathol. 2021;34:20–31.
Zhang H, Wilmot B, Bottomly D, Dao KT, Stevens E, Eide CA, et al. Genomic landscape of neutrophilic leukemias of ambiguous diagnosis. Blood. 2019;134:867–79.
Baumgartner F, Baer C, Bamopoulos S, Ayoub E, Truger M, Meggendorfer M, et al. Comparing malignant monocytosis across the updated WHO and ICC classifications of 2022. Blood. 2024;143:1139–56.
Selimoglu-Buet D, Wagner-Ballon O, Saada V, Bardet V, Itzykson R, Bencheikh L, et al. Characteristic repartition of monocyte subsets as a diagnostic signature of chronic myelomonocytic leukemia. Blood. 2015;125:3618–26.
Xu Y, McKenna RW, Karandikar NJ, Pildain AJ, Kroft SH. Flow cytometric analysis of monocytes as a tool for distinguishing chronic myelomonocytic leukemia from reactive monocytosis. Am J Clin Pathol. 2005;124:799–806.
Goasguen JE, Bennett JM, Bain BJ, Vallespi T, Brunning R, Mufti GJ, et al. Morphological evaluation of monocytes and their precursors. Haematologica. 2009;94:994–7.
Foucar K, Hsi ED, Wang SA, Rogers HJ, Hasserjian RP, Bagg A, et al. Concordance among hematopathologists in classifying blasts plus promonocytes: A bone marrow pathology group study. Int J Lab Hematol. 2020;42:418–22.
Bernard E, Hasserjian RP, Greenberg PL, Arango Ossa JE, Creignou M, Tuechler H, et al. Molecular taxonomy of myelodysplastic syndromes and its clinical implications. Blood. 2024;144:1617–32.
Garcia-Gisbert N, Arenillas L, Roman-Bravo D, Rodriguez-Sevilla JJ, Fernandez-Rodriguez C, Garcia-Avila S, et al. Multi-hit TET2 mutations as a differential molecular signature of oligomonocytic and overt chronic myelomonocytic leukemia. Leukemia. 2022;36:2922–6.
Komrokji RS, Komrokji Z, Al Ali NH, Xie Z, Chan O, Kuykendall AT, et al. CMML Is in the Eye of the Be_Who_ Lder: Interrogating the Newly Proposed Entity of Oligomonocytic Chronic Myelomonocytic Leukemia (O-CMML): MDS or CMML? Blood. 2024;144:1004–1004.
Chapman J, Geyer JT, Khanlari M, Moul A, Casas C, Connor ST, et al. Myeloid neoplasms with features intermediate between primary myelofibrosis and chronic myelomonocytic leukemia. Mod Pathol. 2018;31:429–41.
Hu Z, Ramos CEB, Medeiros LJ, Zhao C, Yin CC, Li S, et al. Utility of JAK2 V617F allelic burden in distinguishing chronic myelomonocytic Leukemia from Primary myelofibrosis with monocytosis. Hum Pathol. 2019;85:290–8.
Vitte F, Fabiani B, Benet C, Dalac S, Balme B, Delattre C, et al. Specific skin lesions in chronic myelomonocytic leukemia: a spectrum of myelomonocytic and dendritic cell proliferations: a study of 42 cases. Am J Surg Pathol. 2012;36:1302–16.
Mathew RA, Bennett JM, Liu JJ, Komrokji RS, Lancet JE, Naghashpour M, et al. Cutaneous manifestations in CMML: Indication of disease acceleration or transformation to AML and review of the literature. Leuk Res. 2012;36:72–80.
Qiao Y, Jian J, Deng L, Tian H, Liu B. Leukaemia cutis as a specific skin involvement in chronic myelomonocytic leukaemia and review of the literature: Acknowledgments. Transl Cancer Res. 2020;9:4988–98.
Martin de Fremont G, Hirsch P, Gimenez de Mestral S, Moguelet P, Ditchi Y, Emile JF, et al. Myeloid Clonal Infiltrate Identified With Next-Generation Sequencing in Skin Lesions Associated With Myelodysplastic Syndromes and Chronic Myelomonocytic Leukemia: A Case Series. Front Immunol. 2021;12:715053.
Enescu CD, Patel A, Friedman BJ. Unique Recognizable Histopathologic Variant of Palisaded Neutrophilic and Granulomatous Dermatitis that Is Associated With SRSF2-Mutated Chronic Myelomonocytic Leukemia: Case Report and Review of the Literature. Am J Dermatopathol. 2022;44:e33–e36.
Loghavi S, Sui D, Wei P, Garcia-Manero G, Pierce S, Routbort MJ, et al. Validation of the 2017 revision of the WHO chronic myelomonocytic leukemia categories. Blood Adv. 2018;2:1807–16.
Carreno-Tarragona G, Alvarez-Larran A, Harrison C, Martinez-Avila JC, Hernandez-Boluda JC, Ferrer-Marin F, et al. CNL and aCML should be considered as a single entity based on molecular profiles and outcomes. Blood Adv. 2023;7:1672–81.
Szuber N, Orazi A, Tefferi A. Chronic neutrophilic leukemia and atypical chronic myeloid leukemia: 2024 update on diagnosis, genetics, risk stratification, and management. Am J Hematol. 2024;99:1360–87.
Kanagal-Shamanna R, Orazi A, Hasserjian RP, Arber DA, Reichard K, Hsi ED, et al. Correction to: Myelodysplastic/myeloproliferative neoplasms-unclassifiable with isolated isochromosome 17q represents a distinct clinico-biologic subset: a multi-institutional collaborative study from the Bone Marrow Pathology Group. Mod Pathol. 2022;35:705.
Awada H, Nagata Y, Goyal A, Asad MF, Patel B, Hirsch CM, et al. Invariant phenotype and molecular association of biallelic TET2 mutant myeloid neoplasia. Blood Adv. 2019;3:339–49.
Gambacorti-Passerini CB, Donadoni C, Parmiani A, Pirola A, Redaelli S, Signore G, et al. Recurrent ETNK1 mutations in atypical chronic myeloid leukemia. Blood. 2015;125:499–503.
Fontana D, Ramazzotti D, Aroldi A, Redaelli S, Magistroni V, Pirola A, et al. Integrated Genomic, Functional, and Prognostic Characterization of Atypical Chronic Myeloid Leukemia. Hemasphere. 2020;4:e497.
Itzykson R, Kosmider O, Renneville A, Morabito M, Preudhomme C, Berthon C, et al. Clonal architecture of chronic myelomonocytic leukemias. Blood. 2013;121:2186–98.
Hercus TR, Thomas D, Guthridge MA, Ekert PG, King-Scott J, Parker MW, et al. The granulocyte-macrophage colony-stimulating factor receptor: linking its structure to cell signaling and its role in disease. Blood. 2009;114:1289–98.
Parganas E, Wang D, Stravopodis D, Topham DJ, Marine JC, Teglund S, et al. Jak2 is essential for signaling through a variety of cytokine receptors. Cell. 1998;93:385–95.
Padron E, Painter JS, Kunigal S, Mailloux AW, McGraw K, McDaniel JM, et al. GM-CSF-dependent pSTAT5 sensitivity is a feature with therapeutic potential in chronic myelomonocytic leukemia. Blood. 2013;121:5068–77.
Elbaek MV, Sorensen AL, Hasselbalch HC. Chronic inflammation and autoimmunity as risk factors for the development of chronic myelomonocytic leukemia? Leuk Lymphoma. 2016;57:1793–9.
Niyongere S, Lucas N, Zhou JM, Sansil S, Pomicter AD, Balasis ME, et al. Heterogeneous expression of cytokines accounts for clinical diversity and refines prognostication in CMML. Leukemia. 2019;33:205–16.
Franzini A, Pomicter AD, Yan D, Khorashad JS, Tantravahi SK, Than H, et al. The transcriptome of CMML monocytes is highly inflammatory and reflects leukemia-specific and age-related alterations. Blood Adv. 2019;3:2949–61.
Hoversten K, Vallapureddy R, Lasho T, Finke C, Ketterling R, Hanson C, et al. Nonhepatosplenic extramedullary manifestations of chronic myelomonocytic leukemia: clinical, molecular and prognostic correlates. Leuk lymphoma. 2018;59:2998–3001.
Mangaonkar AA, Swoboda DM, Coltro G, Lasho TL, Novotny PJ, Pophali P, et al. Clinicopathologic characteristics, prognostication and treatment outcomes for myelodysplastic/myeloproliferative neoplasm, unclassifiable (MDS/MPN-U): Mayo Clinic-Moffitt Cancer Center study of 135 consecutive patients. Leukemia. 2020;34:656–61.
Patel AB, Miles RR, Deininger MW. Lysozyme nephropathy in chronic myelomonocytic leukemia. Clin Case Rep. 2019;7:1263–4.
Hunter AM, Al Ali N, Mai A, Shah S, Swoboda DM, Kuykendall A, et al. Leukocytosis is associated with end organ damage and mortality in chronic myelomonocytic leukemia and can be mitigated by cytoreductive therapy. Leuk Res. 2021;109:106640.
Patnaik MM, Pophali PA, Lasho TL, Finke CM, Horna P, Ketterling RP, et al. Clinical correlates, prognostic impact and survival outcomes in chronic myelomonocytic leukemia patients with the JAK2V617F mutation. Haematologica. 2019;104:e236–e239.
Patnaik MM, Itzykson R, Lasho TL, Kosmider O, Finke CM, Hanson CA, et al. ASXL1 and SETBP1 mutations and their prognostic contribution in chronic myelomonocytic leukemia: a two-center study of 466 patients. Leukemia. 2014;28:2206–12.
Itzykson R, Kosmider O, Renneville A, Gelsi-Boyer V, Meggendorfer M, Morabito M, et al. Prognostic score including gene mutations in chronic myelomonocytic leukemia. J Clin Oncol Off J Am Soc Clin Oncol. 2013;31:2428–36.
Gurney M, Mangaonkar AA, Lasho T, Finke C, Al-Kali A, Gangat N, et al. Somatic TP53 single nucleotide variants, indels and copy number alterations in chronic myelomonocytic leukemia (CMML). Leukemia. 2023;37:1753–6.
Castano-Diez S, Lopez-Guerra M, Zugasti I, Calvo X, Schulz FI, Avendano A, et al. AML typical mutations (CEBPA, FLT3, and NPM1) identify a high-risk CMML independent of CPSS-Mol classification. Blood Adv. 2024:9:39–53.
Patnaik MM, Vallapureddy R, Lasho TL, Hoversten KP, Finke CM, Ketterling R, et al. EZH2 mutations in chronic myelomonocytic leukemia cluster with ASXL1 mutations and their co-occurrence is prognostically detrimental. Blood Cancer J. 2018;8:12.
Patnaik MM, Barraco D, Lasho TL, Finke CM, Reichard K, Hoversten KP, et al. Targeted next generation sequencing and identification of risk factors in World Health Organization defined atypical chronic myeloid leukemia. Am J Hematol. 2017;92:542–8.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Sole F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Li F, Qin T, Li B, Qu S, Pan L, Zhang P, et al. Predicting survival in patients with myelodysplastic/myeloproliferative neoplasms with SF3B1 mutation and thrombocytosis. Leukemia. 2024;38:1334–41.
Cheson BD, Greenberg PL, Bennett JM, Lowenberg B, Wijermans PW, Nimer SD, et al. Clinical application and proposal for modification of the International Working Group (IWG) response criteria in myelodysplasia. Blood. 2006;108:419–25.
Savona MR, Malcovati L, Komrokji R, Tiu RV, Mughal TI, Orazi A, et al. An international consortium proposal of uniform response criteria for myelodysplastic/myeloproliferative neoplasms (MDS/MPN) in adults. Blood. 2015;125:1857–65.
Duchmann M, Braun T, Micol JB, Platzbecker U, Park S, Pilorge S, et al. Validation of response assessment according to international consortium for MDS/MPN criteria in chronic myelomonocytic leukemia treated with hypomethylating agents. Blood Cancer J. 2017;7:e562.
Padron E, Fan W, Tinsley-Vance SM, DeZern AE, Carraway HE, Luskin MR, et al. Reduction in MPN-Total Symptom Score (TSS) Is Associated with Overall Survival (OS) in Chronic Myelomonocytic Leukemia (CMML). Blood. 2024;144:6750.
Merlevede J, Droin N, Qin T, Meldi K, Yoshida K, Morabito M, et al. Mutation allele burden remains unchanged in chronic myelomonocytic leukaemia responding to hypomethylating agents. Nat Commun. 2016;7:10767.
Pleyer L, Germing U, Sperr WR, Linkesch W, Burgstaller S, Stauder R, et al. Azacitidine in CMML: matched-pair analyses of daily-life patients reveal modest effects on clinical course and survival. Leuk Res. 2014;38:475–83.
Robin M, de Wreede LC, Padron E, Bakunina K, Fenaux P, Koster L, et al. Role of allogeneic transplantation in chronic myelomonocytic leukemia: an international collaborative analysis. Blood. 2022;140:1408–18.
Gagelmann N, Badbaran A, Beelen DW, Salit RB, Stolzel F, Rautenberg C, et al. A prognostic score including mutation profile and clinical features for patients with CMML undergoing stem cell transplantation. Blood Adv. 2021;5:1760–9.
Symeonidis A, van Biezen A, de Wreede L, Piciocchi A, Finke J, Beelen D, et al. Achievement of complete remission predicts outcome of allogeneic haematopoietic stem cell transplantation in patients with chronic myelomonocytic leukaemia. A study of the Chronic Malignancies Working Party of the European Group for Blood and Marrow Transplantation. Br J Haematol. 2015;171:239–46.
Onida F, Gagelmann N, Chalandon Y, Kobbe G, Robin M, Symeonidis A, et al. Management of adult patients with CMML undergoing allo-HCT: recommendations from the EBMT PH&G Committee. Blood. 2024;143:2227–44.
Onida F, de Wreede LC, van Biezen A, Eikema DJ, Byrne JL, Iori AP, et al. Allogeneic stem cell transplantation in patients with atypical chronic myeloid leukaemia: a retrospective study from the Chronic Malignancies Working Party of the European Society for Blood and Marrow Transplantation. Br J Haematol. 2017;177:759–65.
Sharma P, Shinde SS, Damlaj M, Hefazi Rorghabeh M, Hashmi SK, Litzow MR, et al. Allogeneic hematopoietic stem cell transplant in adult patients with myelodysplastic syndrome/myeloproliferative neoplasm (MDS/MPN) overlap syndromes. Leuk lymphoma. 2017;58:872–81.
Kurosawa S, Shimomura Y, Tachibana T, Ishiyama K, Ota S, Kobayashi T, et al. Outcome of Allogeneic Hematopoietic Stem Cell Transplantation in Patients with Myelodysplastic/Myeloproliferative Neoplasms-Unclassifiable: A Retrospective Nationwide Study of the Japan Society for Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant. 2020;26:1607–11.
Xicoy B, Germing U, Jimenez MJ, Garcia O, Garcia R, Schemenau J, et al. Response to erythropoietic-stimulating agents in patients with chronic myelomonocytic leukemia. Eur J Haematol. 2016;97:33–8.
Ramadan H, Duong VH, Al Ali N, Padron E, Zhang L, Lancet JE, et al. Eltrombopag Use in Patients With Chronic Myelomonocytic Leukemia (CMML): A Cautionary Tale. Clin Lymphoma Myeloma Leuk. 2016;16:S64–S66.
Rabian F, Chevret S, Gruson B, Thepot S, Walter-Petrich A, Braun T, et al. Eltrombopag in chronic myelomonocytic leukemia with severe thrombocytopenia. A Groupe Francophone des Myelodysplasies (GFM) study. Leukemia. 2024;38:2510–3.
Silverman LR, Demakos EP, Peterson BL, Kornblith AB, Holland JC, Odchimar-Reissig R, et al. Randomized controlled trial of azacitidine in patients with the myelodysplastic syndrome: a study of the cancer and leukemia group B. J Clin Oncol Off J Am Soc Clin Oncol. 2002;20:2429–40.
Kantarjian H, Issa JP, Rosenfeld CS, Bennett JM, Albitar M, DiPersio J, et al. Decitabine improves patient outcomes in myelodysplastic syndromes: results of a phase III randomized study. Cancer. 2006;106:1794–803.
Santini V, Allione B, Zini G, Gioia D, Lunghi M, Poloni A, et al. A phase II, multicentre trial of decitabine in higher-risk chronic myelomonocytic leukemia. Leukemia. 2018;32:413–8.
Itzykson R, Santini V, Thepot S, Ades L, Chaffaut C, Giagounidis A, et al. Decitabine Versus Hydroxyurea for Advanced Proliferative Chronic Myelomonocytic Leukemia: Results of a Randomized Phase III Trial Within the EMSCO Network. J Clin Oncol. 2023;41:1888–97.
Tremblay D, Csizmar C, DiNardo CD, Ball S, Rippel N, Hammond D, et al. Venetoclax in combination with hypomethylating agents in chronic myelomonocytic leukemia: a propensity score matched multicenter cohort study. Leukemia. 2024:39:257–60.
Pleyer L, Leisch M, Kourakli A, Padron E, Maciejewski JP, Xicoy Cirici B, et al. Outcomes of patients with chronic myelomonocytic leukaemia treated with non-curative therapies: a retrospective cohort study. Lancet Haematol. 2021;8:e135–e148.
Hunter AM, Newman H, DeZern AE, Steensma DP, Niyongere S, Roboz GJ, et al. Integrated Human and Murine Clinical Study Establishes Clinical Efficacy of Ruxolitinib in Chronic Myelomonocytic Leukemia. Clin Cancer Res. 2021;27:6095–105.
Verstovsek S, Mesa RA, Gotlib J, Levy RS, Gupta V, DiPersio JF, et al. A double-blind, placebo-controlled trial of ruxolitinib for myelofibrosis. N Engl J Med. 2012;366:799–807.
Padron E, Tinsley-Vance SM, DeZern AE, Carraway HE, Luskin MR, Roboz GJ, et al. Efficacy and safety of ruxolitinib for treatment of symptomatic chronic myelomonocytic leukemia (CMML): results of a multicenter phase II clinical trial. Blood. 2022;140:1101–3.
Assi R, Kantarjian HM, Garcia-Manero G, Cortes JE, Pemmaraju N, Wang X, et al. A phase II trial of ruxolitinib in combination with azacytidine in myelodysplastic syndrome/myeloproliferative neoplasms. Am J Hematol. 2018;93:277–85.
Arora S, Senapati J, Pemmaraju N, Bose P, Masarova L, Montalban-Bravo G, et al. Five-Year Follow up Results of Phase II Clinical Trial Evaluating Ruxolitinib (RUX) and Azacitidine (AZA) Combination Therapy in Patients (pts) with Myelodysplastic Syndrome/Myeloproliferative Neoplasms (MDS/MPNs). Blood. 2023;142:1861.
Tharakan S, Feld J, Van Hyfte G, Mascarenhas J, Tremblay D. Impact of Facility Type on Survival in Chronic Myelomonocytic Leukemia: A Propensity Score Matched, National Cancer Database Analysis. Clin Lymphoma Myeloma Leuk. 2024;24:e385–e391 e381.
Costello R, Lafage M, Toiron Y, Brunel V, Sainty D, Arnoulet C, et al. Philadelphia chromosome-negative chronic myeloid leukaemia: a report of 14 new cases. Br J Haematol. 1995;90:346–52.
Sun Y, Wang Q, Zhang X, Zhang Z, Wang Q, Cen J, et al. Molecular genetics and management of world health organization defined atypical chronic myeloid leukemia. Ann Hematol. 2023;102:777–85.
Maxson JE, Luty SB, MacManiman JD, Abel ML, Druker BJ, Tyner JW. Ligand independence of the T618I mutation in the colony-stimulating factor 3 receptor (CSF3R) protein results from loss of O-linked glycosylation and increased receptor dimerization. J Biol Chem. 2014;289:5820–7.
Dao KH, Solti MB, Maxson JE, Winton EF, Press RD, Druker BJ, et al. Significant clinical response to JAK1/2 inhibition in a patient with CSF3R-T618I-positive atypical chronic myeloid leukemia. Leuk Res Rep. 2014;3:67–69.
Dao KT, Gotlib J, Deininger MMN, Oh ST, Cortes JE, Collins RH Jr, et al. Efficacy of Ruxolitinib in Patients With Chronic Neutrophilic Leukemia and Atypical Chronic Myeloid Leukemia. J Clin Oncol Off J Am Soc Clin Oncol. 2020;38:1006–18.
Broseus J, Florensa L, Zipperer E, Schnittger S, Malcovati L, Richebourg S, et al. Clinical features and course of refractory anemia with ring sideroblasts associated with marked thrombocytosis. Haematologica. 2012;97:1036–41.
Cortelazzo S, Finazzi G, Ruggeri M, Vestri O, Galli M, Rodeghiero F, et al. Hydroxyurea for patients with essential thrombocythemia and a high risk of thrombosis. N Engl J Med. 1995;332:1132–6.
Mascarenhas J, Kosiorek HE, Prchal JT, Rambaldi A, Berenzon D, Yacoub A, et al. A randomized phase 3 trial of interferon-alpha vs hydroxyurea in polycythemia vera and essential thrombocythemia. Blood. 2022;139:2931–41.
Mesa RA, Kiladjian JJ, Catalano JV, Devos T, Egyed M, Hellmann A, et al. SIMPLIFY-1: A Phase III Randomized Trial of Momelotinib Versus Ruxolitinib in Janus Kinase Inhibitor-Naive Patients With Myelofibrosis. J Clin Oncol Off J Am Soc Clin Oncol. 2017;35:3844–50.
Gisslinger H, Gotic M, Holowiecki J, Penka M, Thiele J, Kvasnicka HM, et al. Anagrelide compared with hydroxyurea in WHO-classified essential thrombocythemia: the ANAHYDRET Study, a randomized controlled trial. Blood. 2013;121:1720–8.
Antelo GB, Coltro G, Mangaonkar AA, Lasho T, Finke C, Carr RM, et al. Response to Erythropoiesis Stimulating Agents in Patients with WHO-Defined Myelodysplastic Syndrome/Myeloproliferative Neoplasm with Ring Sideroblasts and Thrombocytosis (MDS/MPN-RS-T). Blood. 2019;134:4182–4182.
Komrokji RS, Platzbecker U, Fenaux P, Zeidan AM, Garcia-Manero G, Mufti GJ, et al. Luspatercept for myelodysplastic syndromes/myeloproliferative neoplasm with ring sideroblasts and thrombocytosis. Leukemia. 2022;36:1432–5.
FDA. FDA approves luspatercept‐aamt for anemia in adults with MDS. FDA; 2020. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-luspatercept-aamt-anemia-adultsmds.
Platzbecker U, Della Porta MG, Santini V, Zeidan AM, Komrokji RS, Shortt J, et al. Efficacy and safety of luspatercept versus epoetin alfa in erythropoiesis-stimulating agent-naive, transfusion-dependent, lower-risk myelodysplastic syndromes (COMMANDS): interim analysis of a phase 3, open-label, randomised controlled trial. Lancet. 2023;402:373–85.
Siddiqui MT, Kanagal-Shamanna R, Naqvi K, Sasaki K, Masarova L, Jabbour E, et al. Clinical Outcomes with Hypomethylating Agents in Patients with Myelodysplastic Syndrome/Myeloproliferative Neoplasm with Ring Sideroblasts and Thrombocytosis (MDS/MPN-RS-T); A Case Series. Blood. 2020;136:18–19.
Melody M, Al Ali N, Sallman DA, Padron E, List AF, Lancet JE, et al. Lenalidomide Is Effective Treatment Option for Patients with Refractory Anemia with Ring Sideroblasts and Thrombocytosis. Blood. 2018;132:4383.
Naqvi K, Sasaki K, Montalban-Bravo G, Teach MS, Pierce SA, Kantarjian HM, et al. Characteristics and Role of Lenalidomide Therapy in Patients with Myelodysplastic/Myeloproliferative Neoplasm with Ring Sideroblasts and Thrombocytosis. Blood. 2018;132:5513.
Rhyasen GW, Bolanos L, Fang J, Jerez A, Wunderlich M, Rigolino C, et al. Targeting IRAK1 as a therapeutic approach for myelodysplastic syndrome. Cancer Cell. 2013;24:90–104.
Oh ST, Mesa R, Harrison C, Bose P, Gerds AT, Heaney ML, et al. Pacritinib Is a Potent ACVR1 Inhibitor with Significant Anemia Benefit in Patients with Myelofibrosis. Blood. 2022;140:1518–21.
Obba S, Hizir Z, Boyer L, Selimoglu-Buet D, Pfeifer A, Michel G, et al. The PRKAA1/AMPKalpha1 pathway triggers autophagy during CSF1-induced human monocyte differentiation and is a potential target in CMML. Autophagy. 2015;11:1114–29.
Kuykendall A, Jain T, Singh A, Pettit K, Lovette Q, Cain J, et al. A Phase 2 study of fedratinib in patients with MDS/MPN and chronic neutrophilic leukemia. American Society of Hematology Annual Meeting, San Diego, CA; 2024.
Moyo TK, Mendler JH, Itzykson R, Kishtagari A, Solary E, Seegmiller AC, et al. The ABNL-MARRO 001 study: a phase 1-2 study of randomly allocated active myeloid target compound combinations in MDS/MPN overlap syndromes. BMC Cancer. 2022;22:1013.
Kishtagari A, Fischer MA, Seegmiller AC, Padron E, Cluzeau T, Xicoy B, et al. Preliminary Results from a Phase 1b Dose De-Escalation Stage of Abnl-Marro 001: An International MDS/MPN Working Group Study. Blood. 2023;142:1874.
Patnaik MM, Sallman DA, Mangaonkar AA, Heuer R, Hirvela J, Zblewski D, et al. Phase 1 study of lenzilumab, a recombinant anti–human GM-CSF antibody, for chronic myelomonocytic leukemia. Blood. 2020;136:909–13.
Hiwase D, Ross DM, Yeung DT, Yong AS, Lane SW, Brown A, et al. Durable Responses Observed in Chronic Myelomonocytic Leukemia Treated with Lenzilumab and Azacitidine. Blood. 2024;144:1006.
Cimmino L, Dolgalev I, Wang Y, Yoshimi A, Martin GH, Wang J, et al. Restoration of TET2 Function Blocks Aberrant Self-Renewal and Leukemia Progression. Cell. 2017;170:1079–95.e1020.
Chien KS, Class CA, Montalban-Bravo G, Wei Y, Sasaki K, Naqvi K, et al. LILRB4 expression in chronic myelomonocytic leukemia and myelodysplastic syndrome based on response to hypomethylating agents. Leuk lymphoma. 2020;61:1493–9.
Mannis GN, Aribi A, Dunavin N, Carraway HE, Saultz JN, Roboz GJ, et al. IO-202, a Novel Anti-LILRB4 Antibody, with Azacitidine for Hypomethylating Agent-Naive Chronic Myelomonocytic Leukemia: Phase 1b Expansion Cohort Results. Blood. 2024;144:1008.
Tong H, Gao S, Yang W, Li J, Yin Q, Zhao X, et al. 801MO Efficacy and safety of a phase II study: Timdarpacept (IMM01) combined with azacitidine (AZA) as the first-line treatment in adults with chronic myelomonocytic leukemia (CMML). Ann Oncol. 2024;35:S597.
Tremblay D, Csizmar CM, DiNardo CD, Ball S, Rippel N, Hammond DE, et al. Venetoclax (VEN) improves response rates but not survival in patients with chronic myelomonocytic leukemia (CMML) treated with hypomethylating agents (HMA): a multicenter, propensity score analysis. Blood. 2023;142:321.
Hunter AM, Patnaik MM, Itzykson R, Mesa R, Karanes C, Li Y, et al. Perspectives on drug development in chronic myelomonocytic leukemia: changing the paradigm. Blood. 2024;144:1987–92.
Acknowledgements
The authors would like to acknowledge Jill Gregory for the creation of Fig. 1.
Author information
Authors and Affiliations
Contributions
DT, RPH and RKR wrote the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
DT receives contracted research funding paid to his institution from Sobi, Sumitomo, Cogent Biosciences and Gilead and consulting fees from Sobi, AbbVie, Pharmaessentia, Sierra Oncology, GSK and Cogent Biosciences. RKR receives contracted research funding pain to his institution from Constellation pharmaceuticals, Ryvu, Sumitomo, Zentalis and Stemline Therapeutics and consulting fees from Incyte Corporation, Celgene/BMS, Blueprint, Abbvie, CTI, Stemline, Galecto, Pharmaessentia, Jubilant, Constellation/Morphosys, Sierra Oncology/GSK, Protagonist, Cogent, Sumitomo Dainippon, Kartos, Servier, Zentalis, Karyopharm. RPH declares no relevant conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tremblay, D., Hasserjian, R.P. & Rampal, R.K. Myelodysplastic syndrome/myeloproliferative neoplasm overlap syndromes: a practical guide to diagnosis and management. Leukemia 39, 1311–1324 (2025). https://doi.org/10.1038/s41375-025-02620-8
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41375-025-02620-8