Abstract
Delirium is a common acute onset neurological syndrome characterised by transient fluctuations in cognition. It affects over 20% of medical inpatients and 50% of those critically ill. Delirium is associated with morbidity and mortality, causes distress to patients and carers, and has significant socioeconomic costs in ageing populations. Despite its clinical significance, the pathophysiology of delirium is understudied, and many underlying cellular mechanisms remain unknown. There are currently no effective pharmacological treatments which directly target underlying disease processes. Although many studies focus on neuronal dysfunction in delirium, glial cells, primarily astrocytes, microglia, and oligodendrocytes, and their associated systems, are increasingly implicated in delirium pathophysiology. In this review, we discuss current evidence which implicates glial cells in delirium, including biomarker studies, post-mortem tissue analyses and pre-clinical models. In particular, we focus on how astrocyte pathology, including aberrant brain energy metabolism and glymphatic dysfunction, reactive microglia, blood-brain barrier impairment, and white matter changes may contribute to the pathogenesis of delirium. We also outline limitations in this body of work and the unique challenges faced in identifying causative mechanisms in delirium. Finally, we discuss how established neuroimaging and single-cell techniques may provide further mechanistic insight at pre-clinical and clinical levels.
Similar content being viewed by others
Introduction
Delirium is characterised by acute onset disturbances and fluctuations in attention, awareness and cognition [1, 2]. It affects over 20% of all medical inpatients and up to 74% of patients in the intensive care unit (ICU) [3,4,5]. Key risk factors for developing delirium include patient characteristics, such as elderly age, dementia, frailty and multimorbidity, and health events, including trauma, surgery, new medications and drug withdrawal are common triggers [6]. Therefore, in the context of ageing populations in many high-income countries, delirium poses a significant challenge to healthcare systems.
Delirium develops over 24–72 h and can be classified as hypoactive, hyperactive or mixed depending on patients’ clinical presentation. The syndrome usually resolves within days but can last weeks to months. Some patients do not return to their cognitive baseline following episodes. In addition, delirium is independently associated with accelerated cognitive decline, increased hospital costs, and mortality [3, 5, 7, 8]. The healthcare consequences of delirium were recently highlighted during the SARS-CoV-2 pandemic, when one in three hospital inpatients developed delirium, which was associated with three-fold higher mortality [9]. Despite this clinical and social significance, delirium remains relatively understudied [10].
The underlying pathophysiology of the syndrome is poorly understood and there is a lack of effective pharmacological interventions [11, 12]. This is compounded by its heterogenous aetiology and clinical presentation. Therefore, there is an urgent need for an improved understanding of the neurobiology of delirium, with the aim of developing diagnostic and therapeutic strategies.
Many studies adopt a neuron-centric approach to delirium and aim to understand changes in brain network and neurotransmitter activity or to identify biomarkers of neuronal damage, such as neuron-specific enolase and phosphorylated neurofilament heavy subunit [13,14,15,16]. However, these approaches do not consider the complex neuro-glial interactions which may be disrupted in delirium, and notably, accumulating experimental data suggests a role for glial cells, including astrocytes, microglia and oligodendrocytes, in delirium pathogenesis [17, 18]. In this review, we evaluate current evidence which supports a role for glial cells and systems in the pathogenesis of delirium and outline directions for future research.
Studying the pathophysiology of delirium
As a fluctuating cognitive syndrome with a heterogenous aetiology, the underlying pathophysiology of delirium can be challenging to study [19]. Post-mortem studies only capture the end-stage of the disorder and methods typically used to assess delirium in humans, such as cognitive testing, are difficult to adapt to animal models. Neuroimaging approaches often lack the resolution required to form conclusions on the cellular and molecular pathology underlying delirium and biofluidic analyses often focus on single metabolites and proteins. In addition, the pathological effects of episodes of delirium can be challenging to isolate in patients with a high number of comorbidities. However, epidemiological evidence consistently shows that there is a significant role for patient susceptibility, such as ageing or a diagnosis of a neurodegenerative disorder, in delirium [6, 8].
Therefore, animal models frequently use aged rodents or those that model neurodegenerative disorders and subject them to “secondary insults”, such as central or systemic inflammation (e.g. lipopolysaccharide [LPS] injection) or post-operative conditions (e.g. laparotomy). Naturally, these models vary in their precise cellular and molecular pathology since they are based on different aetiologies but nevertheless often implicate common pathways. Rodent models have replicated delirium-like behaviour and display neuroimmune signatures which are mediated by astrocytes and microglia [20, 21]. This is in line with evidence of increased astrocytic and microglial reactivity with age and in neurodegeneration and suggests that delirium may exacerbate this phenotype [22,23,24]. Together, animal models suggest that cellular priming, defined as enhanced cellular reactivity on the background of pre-existing pathology, plays an important part in the pathogenesis of delirium. In the following sections, we discuss pre-clinical and clinical studies which provide evidence to suggest that glial cell types and systems contribute to the pathophysiology of delirium (Fig. 1).
Glial dysfunction has been described in delirium, but the underlying pathophysiological mechanisms are not fully understood. Key risk factors for and triggers of delirium include older age, pre-existing neurodegeneration, systemic inflammation, surgery, new medications and drug withdrawal. Reactive astrocytes with increased inflammasome activity, altered metabolism and impaired glymphatic activity have been reported in patients and models with delirium. Similarly, microglia display elevated cytokine production and C1q-tagged signalling. Impaired blood-brain barrier function and white matter changes have also been noted. Exploiting existing technologies including single-cell transcriptomics, neuroimaging, liquid biomarkers and optogenetics would provide deeper mechanistic insight into the roles of dysregulated glia in delirium. The effects of these mechanisms on neuronal function should also be interrogated. GFAP: glial fibrillary acidic protein; CXCL10: C-X-C motif chemokine ligand 10; IL-6/1β: interleukin-6/1β; TNFα: tumour necrosis factor α; C1q: complement component 1q; CD68: cluster of differentiation 68; TLR2: toll-like receptor 2.
Role of astrocytes in delirium
Astrocytes have diverse physiological functions which include regulating neuronal energy supply, modulating synaptic activity, contributing to neurogenesis, supporting the blood-brain barrier (BBB) and maintaining ion and neurotransmitter homeostasis. Many of these processes are impaired in delirium, but whether they are direct contributors remains unclear. Challenges also arise when studying astrocytic reactivity in this disorder since it can have both protective and pathological phenotypes [25]. In this section, we discuss the evidence for structural astrocyte pathology, aberrant brain energy metabolism and abnormalities in the glymphatic system in delirium.
Astrocytic inflammatory signatures in delirium
Astrogliosis is frequently observed in models of delirium and has been noted in patients with delirium. A post-mortem study identified raised astrocytic glial fibrillary acid protein (GFAP) immunoreactivity in patients with a history of delirium compared to age-matched controls, primarily in the dentate gyrus [26]. In addition, raised levels of S100B, a protein primarily expressed by astrocytes, is frequently associated with an increased risk of developing delirium following hospital admission [27].
Pre-clinical studies have provided further insight into this inflammatory signature. In an aged mouse model of post-operative delirium, astrocytes were noted to have a reactive morphology with an atrophied cell soma and shorter, deramified processes [28]. When the amyloid precursor protein/presenilin 1 mouse model of Alzheimer’s disease (AD) was subjected to a secondary inflammatory challenge with interleukin-1β (IL-1β), primed astrocytes developed exaggerated chemokine responses [21]. Similar results were observed in a model of tauopathy injected with LPS, which displayed astrogliosis, acute sickness behaviour and accelerated tau pathology [24]. In a model of post-operative delirium, reactive astrocytes showed aberrant NOD-like receptor protein 3 inflammasome activation and γ-aminobutyric acid (GABA) synthesis [29].
Several molecules with immunomodulatory properties have shown therapeutic effects in rodent models via astrocytic mechanisms. Dexmedetomidine, an a2-adrenoceptor agonist, displayed neuroprotective effects following LPS challenges by reducing astrocytic pyroptosis and inflammasome activation [30]. Minocycline, an anti-inflammatory drug, reduced inflammatory signatures in astrocytes and long-term cognitive impairment in a model of post-operative delirium [31]. Targeting β-arrestin1, which interacts with dynamin-related protein 1 to regulate mitochondrial fusion/fission and has reduced expression in reactive astrocytes, has also shown promising pre-clinical results [32]. These approaches warrant further pre-clinical and translational investigation.
Aberrant brain energy metabolism in delirium
Astrocytes play key roles in brain energy metabolism, including via the astrocyte-neuron lactate shuttle. Patients with clinical risk factors for developing delirium, particularly a diagnosis of AD, often have pre-existing deficits in brain energy metabolism. The expression of GLUT1, a glucose transporter, is reduced in AD and patients display impaired glucose utilisation and insulin sensitivity [33,34,35]. Animal studies show that mice with pre-existing neurodegeneration are vulnerable to hypoglycaemia, which is associated with delirium in both clinical and experimental settings [36,37,38]. A 2-18F-fluoro-2-deoxyglucose positron emission tomography (PET) study identified reduced brain-wide glucose metabolism in patients with delirium [39]. In an animal model of septic encephalopathy, glucose uptake was preferentially reduced in the neocortex, which was associated with decreased cerebral blood flow (CBF) and alpha activity on electroencephalography [40]. Although definitive cellular resolution is not yet possible with this technique, rodent work suggests that this mechanism is likely driven by glutamate uptake by astrocytes [41]. Additionally, in one rodent model of post-operative delirium, when glial metabolism was inhibited with fluorocitrate for three days following surgery, GFAP expression was reduced and there were improvements in cognitive function [42].
A recent study showed that patients who developed delirium following a hip fracture had increased concentrations of ketone bodies in their cerebrospinal fluid (CSF) compared to those who did not develop delirium but that there was no difference in CSF or serum glucose concentrations [43]. Astrocytes are known to regulate the concentration of ketones in the brain via fatty acid oxidation [44]. Several studies have also identified raised CSF lactate levels in patients who developed delirium following a significant fracture, but this relationship may be mediated by patients’ age and comorbidities [36, 43]. Patients with delirium lasting more than five days have been found to have higher CSF lactate levels than outpatients diagnosed with dementia [45]. In addition, metabolic conditions, such as hepatic encephalopathy, in which hyperammonaemia induces osmotic dysregulation in astrocytes via the glutamate-glutamine cycle, mimic some clinical features of delirium [46,47,48,49,50,51]. In a rodent model of hepatic encephalopathy, astrocytes were found to be enlarged and displayed increased GFAP, tumour necrosis factor α (TNFα) and aquaporin-4 (AQP4) expression and reduced Kir 4.1 immunoreactivity [52]. Together, these findings are suggestive of altered brain glucose utilisation in patients with delirium, which may be mediated by astrocytes.
There is limited evidence on whether modulating these metabolic signatures in astrocytes would be clinically feasible or effective. For example, valproic acid (VPA), a medication currently used for bipolar disorder and epilepsy, is believed to act via GABA signalling and may also modulate excitatory/inhibitory imbalances via astrocytes [53, 54]. In addition, VPA has been shown to ameliorate pro-inflammatory signatures in astrocytes, including reducing GFAP levels [55, 56]. There are several reports of VPA being used in antipsychotic-resistant cases of delirium, but these are largely uncontrolled studies and robust evidence on this question is lacking [57]. Further studies on the potential role of VPA in the management of delirium may provide insight into the mechanisms of astrocytic dysfunction in the syndrome.
Abnormalities in the glymphatic system
The glymphatic system is comprised of a network of perivascular channels formed by astrocytes, with AQP4 channels located on astrocyte endfeet being an important component of the system [58]. In vivo models of neurodegenerative diseases, such as AD, have identified impairments in the glymphatic system [59]. It has been suggested that glymphatic impairment also occurs in the post-operative period, which could contribute to cognitive disturbances, but this remains largely unexplored [60].
Anaesthetic agents are known to affect glymphatic function and astrocytic reactivity, which may contribute to post-operative delirium [61,62,63]. Sevoflurane, an inhaled anaesthetic, disrupts calcium currents in astrocytes, which may be important in regulating glymphatic flow [64]. Sevoflurane is also associated with raised cerebral glucose and lactate levels, which correlate with post-operative delirium scores in children [65]. Other anaesthetic agents, such as dexmedetomidine and propofol, appear to promote glymphatic activity [61, 66, 67]. Dexmedetomidine also reduces the expression of monocyte chemoattractant protein-1, a pro-inflammatory cytokine, in LPS-induced astrocytes, ameliorates excessive GABA receptor expression, and is associated with a lower incidence of post-operative delirium than other anaesthetic agents [68,69,70]. The glymphatic system represents a possible therapeutic target for delirium, especially post-operatively, but further studies are needed. In particular, the use of aged aqp4 knockout mice subjected to surgery or systemic inflammation could provide further insight. However, assessing glymphatic function in pre-clinical models remains challenging as methods are highly invasive and animals need to be anaesthetised for imaging. In addition, certain aspects of the glymphatic system are not yet well-established in humans and can be difficult to assess in clinical studies [71].
Role of microglia in delirium
Microglia are the resident immune cells of the brain and remove apoptotic neurons, release inflammatory mediators, respond to local tissue factors and fine tune neural circuitry during post-natal development [72,73,74]. Dysregulation of pro-inflammatory and pro-reparative signals from microglia, for example during neurodegeneration, result in neuronal dysfunction, cell death and synapse loss [75]. In this section, we discuss evidence for microglial reactivity and dysregulated homeostasis in delirium.
Microglial reactivity and dysregulated microglial homeostasis in delirium
Post-mortem studies have identified raised expression of the myeloid lineage markers human leukocyte antigen-DR and cluster of differentiation 68 in the brain tissue of patients with a history of delirium, independent of a co-existing infection or diagnosis of dementia [26]. Brain tissue of patients with a history of sepsis or sepsis-associated encephalopathy displayed a similar phenotype, including complement component 1q (C1q) activation in hippocampal regions [76, 77]. Proteomic studies of CSF samples from patients with delirium have also identified several inflammatory markers which are associated with microglia. For example, fractalkine levels are raised in the CSF of patients with infectious delirium and AD when compared to healthy controls [78]. Fractalkine is a chemokine ligand which binds to CX3C chemokine receptor 1 (CX3CR1) on microglia and regulates microglial reactivity [79]. In contrast, both CD200 receptor 1 (CD200R1) and caspase 8 (CASP8) are downregulated in patients with infectious delirium and AD. CD200 is expressed by neurons and binds to CD200 receptors expressed on microglia to maintain a microglial resting state by regulating cytokine production [80, 81]. CASP8 is a ligand involved in cell apoptosis and inhibits pro-inflammatory microglial activity [82]. Soluble triggering receptor expressed on myeloid cells 2 (TREM2), a receptor found on microglia, is also found at higher levels in the CSF of patients with delirium in the absence of pre-existing dementia, which highlights the importance of stratifying delirium patients by their dementia status [83].
Pre-clinical studies have provided some additional mechanistic detail. Microglia isolated from aged mice subjected to LPS challenges display increased expression of IL-1β, MHC class II molecules, toll-like receptor 2 (TLR2) and IL-10 [84]. Cytokine challenges with TNFα or IL-1β and polyinosinic:polycytidylic acid injections, which mimic systemic viral infection, also result in microglial priming in mouse models of neurodegeneration [85, 86]. Microglial reactivity, measured by increased IBA1 expression, has been observed in the hippocampi of mice subjected to LPS and was associated with an imbalance between pro- and anti-inflammatory cytokines [87]. The authors suggested that this effect may be mediated by TLR4, a LPS receptor, as blocking TLR4 signalling with viral inhibitory peptide for TLR4 (VIPER) attenuated LPS-induced neuroinflammation. Additionally, in rodents, depleting microglia by inhibiting the colony-stimulating factor 1 receptor (CSF1R) protects against post-operative cognitive decline via an anti-inflammatory mechanism [88, 89]. CSF1R inhibition has also been shown to reduce C1q complement activation and protect neurons from microglial engulfment, which is associated with cognitive improvements in mice [77].
Several studies have used minocycline, an established anti-inflammatory drug which targets NF-κB, to reduce microglial reactivity in models of delirium [90, 91]. One study demonstrated that minocycline reduces post-operative microglial reactivity and decreases the expression of IL-1β and TNFα in rat hippocampi [92]. A similar effect has been shown for astrocytes [31]. Another group showed a reduction in cytokine expression and microglial reactivity in the hippocampus following administration of minocycline and an IL-1 receptor antagonist [93]. This signature was also observed when minocycline was administered following an LPS insult, which resulted in reduced cytokine and microglial TLR2 surface expression [94]. Similarly, artemisinin, an anti-malarial drug with anti-inflammatory properties, has been shown to reduce LPS-induced cognitive impairment, likely by activating AMPKα1 signalling in microglia and suppressing pro-inflammatory cytokine production [95].
However, many of these anti-inflammatory drugs are generic immunomodulators which act on many cell types and these studies do not show whether decreased microglial reactivity was a direct result of the drug or a subsequent reduction in LPS- or surgery-mediated damage. Recent clinical trials of prophylactic minocycline administration in at-risk patients undergoing major surgery have showed contrasting effects on post-operative cognitive impairment [96, 97]. Several other molecules with anti-inflammatory properties have displayed improvements in microglial reactivity, inflammatory signatures and cognitive impairment in rodent models of delirium and warrant further translational studies [98,99,100,101,102].
Blood-brain barrier impairment in delirium
The BBB is a multicellular structure comprised of astrocytes, pericytes, neurons, microglia, endothelial cells and the basement membrane. The BBB has several important functions, including delivering nutrients, removing waste and regulating immune functions, all of which are impaired in delirium [103]. The precise contribution of BBB impairment to delirium remains unclear and assessment of BBB integrity can provide widely varying results depending on the methodology used [104].
BBB permeability, measured by the CSF:plasma albumin ratio, correlates with post-operative delirium incidence, severity, and delayed recovery [105, 106]. Notably, these studies showed that short-term increases in BBB permeability from before surgery to 24 hours after surgery are more significant in patients who develop post-operative delirium compared to those who do not, even when accounting for other clinical factors. Patients with elevated levels of plasma markers of endothelial cell activation and BBB injury, such as E-selectin and plasminogen activator inhibitor-1, are at increased risk of experiencing prolonged episodes of delirium [107]. Critically ill patients with a lower reactive hyperaemia index, an indicator of poorer systemic endothelial cell function, also experience prolonged periods of acute brain dysfunction [108].
BBB impairment is well-characterised in ageing and can drive excessive transforming growth factor-β signalling in astrocytes, which leads to neuronal dysfunction in humans and rodent models [109]. Astrocytes mediate signalling between neurons and the vasculature and increase CBF in response to neuronal activity. A significant reduction in whole-brain and regional CBF has been demonstrated in patients experiencing delirium, which resolved when symptoms improved [110]. This reduction in CBF has also been identified in a rat model of septic encephalopathy and was associated with reduced cerebral glucose uptake [40]. In addition, transcranial ultrasound studies have described abnormal cerebral autoregulation in patients experiencing delirium [111]. These mechanisms are likely associated with previously discussed findings of abnormal glucose utilisation in the brain during delirium and may represent a link between astrocytic reactivity, metabolic dysfunction and BBB impairment.
Pre-clinical studies have also identified structural BBB pathology, particularly changes in tight junction proteins and the basal lamina, in models of delirium [28]. In an LPS-induced mouse model of septic encephalopathy, pericytes detached from the basal lamina, which was associated with increased cerebrovascular permeability [112]. In vitro, cultured mouse cerebrovascular endothelial cells challenged with blood plasma from septic mice displayed a dissociation of occludin from the cytoskeleton and increased permeability [113]. An AD-related model of post-operative delirium demonstrated changes in AQP4 and GFAP expression in astrocytes following surgery and increased extravasation of fibrinogen and dextran across the BBB [114]. Proximity labelling techniques, such as TurboID, would allow for protein interactions, for example with astrocytic endfeet or endothelial cells, at the BBB to be studied, providing greater mechanistic detail.
Further research is also needed to determine whether therapies targeted toward the BBB can reduce delirium risk and improve prognosis. Explorative studies indicate that statins, which can modify the endothelium and reduce inflammation, may be protective. Evidence from a prospective cohort study suggests that statin use amongst critically ill patients is associated with a lower incidence of delirium [115, 116]. Controlled trials and long-term cognitive outcome studies would be needed to support this. Preventing the recruitment of inflammatory monocytes across the BBB could be an attractive therapeutic target for delirium and a pre-clinical model showed that this was associated with reduced neuroinflammation and cognitive impairment [117]. While administration of neuroprotectin D1, a docosahexaenoic acid-derived lipid mediator, has also been shown to ameliorate BBB pathology and was associated with improvements glial function and memory [28]. Additionally, microfluidic and multicellular organoid models of the BBB have the potential to provide further insight into possible prophylactic and treatment options by enabling high-throughput screening of candidate molecules [118]. Interestingly, therapies targeting the BBB could also be non-pharmacological and a small study showed that early physical therapy may improve endothelial function and reduce delirium duration in patients admitted to an ICU [119].
White matter dysfunction in delirium
Oligodendrocytes are glial cells which produce and maintain myelin in the central nervous system and provide metabolic support to surrounding neurons. Overall, there is mixed evidence on the role of white matter abnormalities, including hyperintensities, fractional anisotropy and altered diffusivity, in acute cognitive impairment. In particular, the extent to which white matter changes predispose patients to developing delirium, are involved in the syndrome itself, or are simply incidental findings is unclear.
White matter hyperintensities have been identified in up to 75% of patients with delirium but are also common in healthy aged individuals [120]. In the Oxford Vascular Study, patients with a history of stroke or transient ischaemic attack who also had white matter changes on magnetic resonance imaging (MRI) were more likely to develop delirium up to five years following their cerebrovascular incident [121]. This study also showed that white matter changes were associated with future delirium risk, independent of pre-admission cognitive status. In addition, in a cohort of patients undergoing cardiac surgery, those who displayed reduced pre-operative fractional anisotropy, a readout of white matter impairment, were at increased risk of developing post-operative delirium [122]. In a recent pre-clinical study, aged mice which were cognitively vulnerable to a systemic inflammatory challenge displayed increased microglial reactivity in white matter regions and the degree of their cognitive dysfunction correlated with the extent of myelin pathology around the hippocampal formation [123]. Conversely, a study of patients admitted within 48 hours of the onset of stroke symptoms identified comparable white matter changes in most brain regions between patients who developed delirium and those who did not [124]. Other studies have described no relationship between white matter lesions and post-operative delirium [125,126,127].
Some studies have considered the potential contribution of white matter changes to clinical outcomes and long-term sequalae. Specifically, white matter abnormalities identified on MRI have been shown to correlate with clinical outcomes in patients with sepsis and delirium [128]. A diffusion tensor imaging study described reduced fractional anisotropy in ICU patients with prolonged episodes of delirium [129]. These imaging features were present three months following discharge and were associated with worse cognitive outcomes up to one year later. A recent study of patients admitted with SARS-CoV-2 infection and associated neurological symptoms, including delirium, identified volume shifts indicative of vasogenic oedema affecting white matter tracts and correlated the magnitude of these findings with cognitive impairment [130].
Further neuroimaging studies are required to detect structural white matter changes which may contribute to episodes of delirium. Using data from prospective cohorts, for example the UK Biobank, would allow for thorough investigation of delirium risk factors and long-term outcomes.
Future directions
Both pre-clinical and clinical studies have identified dysregulated glial cells and systems in delirium, but in many cases, the cellular mechanisms underlying this pathology are unclear. In addition, the crosstalk between neurons and glia in delirium and how this may be disrupted is largely unexplored (Table 1).
Techniques such as fluorescence-activated cell sorting to isolate astrocytes, microglia or oligodendrocytes from animal models of delirium, followed by transcriptomic or proteomic analyses would help elucidate cell type-specific pathway dysregulation. Single-cell isolation, for example, via laser capture microscopy of post-mortem tissue or enzymatic dissociation of rodent brains, could be used to explore the role of regional heterogeneity and identify cell clusters which drive disease pathogenesis. Targeting a subset of heterogenous cell types may also improve therapeutic efficacy, since generic anti-inflammatory treatments have generally not been successful [131].
Aberrant metabolic processes in astrocytes in delirium could be explored further using existing metabolic modulators. For example, ceftriaxone, which promotes glutamate transport, a function which is likely disrupted in astrocytes during delirium, could be used in animal models to assess effects on cognition [41]. Astrocytes and microglia play important roles in modulating the neural circuitry and future work could investigate this using calcium imaging and opto- and chemogenetic tools in delirium models [132]. Therefore, applying technologies currently used to investigate glial dysfunction in other neurological disorders could help elucidate the roles of these cell types in delirium.
While there is some clinical evidence which suggests a role for white matter impairment in delirium, this has not been explored extensively in pre-clinical models. Changes in white matter could be assessed at different time points in delirium pathogenesis using MRI, along with cognitive testing as a correlative investigation. Compounds associated with protection or repair of white matter could be tested in these models to determine if this therapeutic strategy is associated with improved cognitive function.
The impaired crosstalk between glial cells in delirium also warrants further investigation. For example, it has been demonstrated that reactive microglia, by secreting IL-1α, TNFα and C1q, induce a unique phenotype in astrocytes in neurodegenerative disorders such as Alzheimer’s and Parkinson’s disease [133]. Targeting this aberrant signalling to prevent neurotoxic crosstalk between microglia and astrocytes has been shown to be protective in models of Parkinson’s disease and could offer a new therapeutic approach for delirium [134].
Several neuroimaging methods have the potential to improve our clinical understanding of the roles of glial cells in delirium aetiology and progression. Two PET tracers, 11C-BU99008, which primarily binds to I2-imidazoline-2 on the outer mitochondrial membrane in astrocytes, and 11C-DED, which primarily targets monoamine oxidase B in astrocytes, are currently in use and could provide further insight into the metabolic changes in astrocytes during episodes of delirium [135]. The utility of astrocytic and microglial plasma biomarkers, including chitinase-3-like protein 1, translocator protein (18 kDa), CX3CL1 and CSF1, which are currently being trialled for other disorders should also be explored in the context of delirium [19, 136, 137]. The development of tracers which can discriminate between different glial phenotypes would allow for investigation of these dynamic states throughout the course of the syndrome and in response to treatment. Finally, additional studies using dynamic contrast-enhanced MRI and PET, for example targeting P-glycoprotein-mediated efflux at the BBB, are needed to elucidate the temporal contribution of BBB impairment to delirium.
Conclusion
Delirium remains an understudied condition, especially given its high prevalence of approximately one in five medical inpatients. The pathophysiology of delirium is poorly understood and no effective pharmacological treatments which target its pathogenesis have been identified. Emerging evidence has described dysfunctional glial cells and systems in delirium. This includes the loss of astrocytic functions in brain energy metabolism and the glymphatic system, aberrant microglial reactivity, impairment of the blood-brain barrier, and white matter dysfunction. However, mechanistic detail in these areas is still lacking. We propose that exploiting existing technologies, such as high-resolution neuroimaging and single-cell approaches, would provide insight into the spatiotemporal involvement of glia in delirium and identify dysregulated pathways which could be targeted. Establishing glial biomarkers is also important for improving our understanding of the roles of these cells in delirium risk, prognosis and management. A better understanding of the role of glia in delirium across multiple pre-clinical and clinical models will help advance the development of effective therapeutic strategies.
References
Wilson JE, Mart MF, Cunningham C, Shehabi Y, Girard TD, MacLullich AMJ, et al. Delirium. Nat Rev Dis Primers. 2020;6:90.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed., text rev. edn, 2022.
Pendlebury ST, Lovett NG, Smith SC, Dutta N, Bendon C, Lloyd-Lavery A, et al. Observational, longitudinal study of delirium in consecutive unselected acute medical admissions: age-specific rates and associated factors, mortality and re-admission. BMJ Open. 2015;5:e007808.
Roberts B, Rickard CM, Rajbhandari D, Turner G, Clarke J, Hill D, et al. Multicentre study of delirium in ICU patients using a simple screening tool. Aust Crit Care. 2005;18:6. 8-9, 11-14 passim
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369:1306–16.
Mattison MLP. Delirium. Ann Intern Med. 2020;173:Itc49–itc64.
Kinchin I, Mitchell E, Agar M, Trépel D. The economic cost of delirium: A systematic review and quality assessment. Alzheimers Dement. 2021;17:1026–41.
Davis DH, Muniz-Terrera G, Keage HA, Stephan BC, Fleming J, Ince PG, et al. Association of delirium with cognitive decline in late life: a neuropathologic study of 3 population-based cohort studies. JAMA Psychiatry. 2017;74:244–51.
Shao SC, Lai CC, Chen YH, Chen YC, Hung MJ, Liao SC. Prevalence, incidence and mortality of delirium in patients with COVID-19: a systematic review and meta-analysis. Age Ageing. 2021;50:1445–53.
Teodorczuk A, MacLullich A. New waves of delirium understanding. Int J Geriatr Psychiatry. 2018;33:1417–9.
Scottish Intercollegiate Guidelines Network. Risk reduction and management of delirium. 2019.
Reay H, Arulkumaran N, Brett SJ. Priorities for future intensive care research in the UK: Results of a James Lind Alliance Priority Setting Partnership. Journal of the Intensive Care Society. 2014;15:288–96.
Mietani K, Hasegawa-Moriyama M, Inoue R, Ogata T, Shimojo N, Kurano M, et al. Elevated neuron-specific enolase level is associated with postoperative delirium and detection of phosphorylated neurofilament heavy subunit: A prospective observational study. PLoS One. 2021;16:e0259217.
Gunther ML, Morandi A, Ely EW. Pathophysiology of delirium in the intensive care unit. Crit Care Clin. 2008;24:45–65.
Sanders RD. Hypothesis for the pathophysiology of delirium: role of baseline brain network connectivity and changes in inhibitory tone. Med Hypotheses. 2011;77:140–3.
Mietani K, Sumitani M, Ogata T, Shimojo N, Inoue R, Abe H, et al. Dysfunction of the blood-brain barrier in postoperative delirium patients, referring to the axonal damage biomarker phosphorylated neurofilament heavy subunit. PLoS One. 2019;14:e0222721.
Sfera A, Osorio C, Price AI, Gradini R, Cummings M. Delirium from the gliocentric perspective. Front Cell Neurosci. 2015;9:171.
Cerejeira J, Firmino H, Vaz-Serra A, Mukaetova-Ladinska EB. The neuroinflammatory hypothesis of delirium. Acta Neuropathol. 2010;119:737–54.
Vasunilashorn SM, Lunardi N, Newman JC, Crosby G, Acker L, Abel T, et al. Preclinical and translational models for delirium: Recommendations for future research from the NIDUS delirium network. Alzheimers Dement. 2023;19:2150–74.
Murray C, Sanderson DJ, Barkus C, Deacon RM, Rawlins JN, Bannerman DM, et al. Systemic inflammation induces acute working memory deficits in the primed brain: relevance for delirium. Neurobiol Aging. 2012;33:603–616.e603.
Lopez-Rodriguez AB, Hennessy E, Murray CL, Nazmi A, Delaney HJ, Healy D, et al. Acute systemic inflammation exacerbates neuroinflammation in Alzheimer’s disease: IL-1β drives amplified responses in primed astrocytes and neuronal network dysfunction. Alzheimers Dement. 2021;17:1735–55.
Clarke LE, Liddelow SA, Chakraborty C, Münch AE, Heiman M, Barres BA. Normal aging induces A1-like astrocyte reactivity. Proc Natl Acad Sci USA. 2018;115:E1896–e1905.
Koellhoffer EC, McCullough LD, Ritzel RM. Old Maids: Aging and Its Impact on Microglia Function. Int J Mol Sci. 2017;18:769.
Torvell M, Hampton DW, Connick P, MacLullich AMJ, Cunningham C, Chandran S. A single systemic inflammatory insult causes acute motor deficits and accelerates disease progression in a mouse model of human tauopathy. Alzheimers Dement (N Y). 2019;5:579–91.
Sofroniew MV. Astrocyte reactivity: subtypes, states, and functions in CNS innate immunity. Trends Immunol. 2020;41:758–70.
Munster BC, Aronica E, Zwinderman AH, Eikelenboom P, Cunningham C, Rooij SE. Neuroinflammation in delirium: a postmortem case-control study. Rejuvenation Res. 2011;14:615–22.
Bassi T, Rohrs E, Nicholas M, Reynolds S. Meta-analysis of serological biomarkers at hospital admission for the likelihood of developing delirium during hospitalization. Front Neurol. 2023;14:1179243.
Zhou Y, Wang J, Li X, Li K, Chen L, Zhang Z, et al. Neuroprotectin D1 protects against postoperative delirium-like behavior in aged mice. Front Aging Neurosci. 2020;12:582674.
Wang LY, Wang XP, Lv JM, Shan YD, Jia SY, Yu ZF, et al. NLRP3-GABA signaling pathway contributes to the pathogenesis of impulsive-like behaviors and cognitive deficits in aged mice. J Neuroinflammation. 2023;20:162.
Sun YB, Zhao H, Mu DL, Zhang W, Cui J, Wu L, et al. Dexmedetomidine inhibits astrocyte pyroptosis and subsequently protects the brain in in vitro and in vivo models of sepsis. Cell Death Dis. 2019;10:167.
Jin WJ, Feng SW, Feng Z, Lu SM, Qi T, Qian YN. Minocycline improves postoperative cognitive impairment in aged mice by inhibiting astrocytic activation. Neuroreport. 2014;25:1–6.
Hua F, Zhu H, Yu W, Zheng Q, Zhang L, Liang W, et al. β-arrestin1 regulates astrocytic reactivity via Drp1-dependent mitochondrial fission: implications in postoperative delirium. J Neuroinflammation. 2023;20:113.
Hölscher C. Insulin Signaling Impairment in the Brain as a Risk Factor in Alzheimer’s disease. Front Aging Neurosci. 2019;11:88.
Meltzer CC, Zubieta JK, Brandt J, Tune LE, Mayberg HS, Frost JJ. Regional hypometabolism in Alzheimer’s disease as measured by positron emission tomography after correction for effects of partial volume averaging. Neurology. 1996;47:454–61.
Sweeney MD, Kisler K, Montagne A, Toga AW, Zlokovic BV. The role of brain vasculature in neurodegenerative disorders. Nat Neurosci. 2018;21:1318–31.
Kealy J, Murray C, Griffin EW, Lopez-Rodriguez AB, Healy D, Tortorelli LS, et al. Acute Inflammation Alters Brain Energy Metabolism in Mice and Humans: Role in Suppressed Spontaneous Activity, Impaired Cognition, and Delirium. J Neurosci. 2020;40:5681–96.
Shehab N, Lovegrove MC, Geller AI, Rose KO, Weidle NJ, Budnitz DS. US emergency department visits for outpatient adverse drug events, 2013–2014. JAMA. 2016;316:2115–25.
Sonneville R, de Montmollin E, Poujade J, Garrouste-Orgeas M, Souweine B, Darmon M, et al. Potentially modifiable factors contributing to sepsis-associated encephalopathy. Intensive Care Med. 2017;43:1075–84.
Haggstrom LR, Nelson JA, Wegner EA, Caplan GA. 2-(18)F-fluoro-2-deoxyglucose positron emission tomography in delirium. J Cereb Blood Flow Metab. 2017;37:3556–67.
Semmler A, Hermann S, Mormann F, Weberpals M, Paxian SA, Okulla T, et al. Sepsis causes neuroinflammation and concomitant decrease of cerebral metabolism. J Neuroinflammation. 2008;5:38.
Zimmer ER, Parent MJ, Souza DG, Leuzy A, Lecrux C, Kim HI, et al. [(18)F]FDG PET signal is driven by astroglial glutamate transport. Nat Neurosci. 2017;20:393–5.
Wang T, Xu G, Zhang X, Ren Y, Yang T, Xiao C, et al. Malfunction of astrocyte and cholinergic input is involved in postoperative impairment of hippocampal synaptic plasticity and cognitive function. Neuropharmacology. 2022;217:109191.
Titlestad I, Watne LO, Caplan GA, McCann A, Ueland PM, Neerland BE, et al. Impaired glucose utilization in the brain of patients with delirium following hip fracture. Brain. 2024;147:215–23.
Puchalska P, Crawford PA. Multi-dimensional roles of ketone bodies in fuel metabolism, signaling, and therapeutics. Cell Metab. 2017;25:262–84.
Caplan GA, Kvelde T, Lai C, Yap SL, Lin C, Hill MA. Cerebrospinal fluid in long-lasting delirium compared with Alzheimer’s dementia. J Gerontol A Biol Sci Med Sci. 2010;65:1130–6.
Dhiman RK, Chawla YK. Minimal hepatic encephalopathy: time to recognise and treat. Tropical Gastroenterology. 2009;29:6–12.
Balzano T, Dadsetan S, Forteza J, Cabrera-Pastor A, Taoro-Gonzalez L, Malaguarnera M, et al. Chronic hyperammonemia induces peripheral inflammation that leads to cognitive impairment in rats: Reversed by anti-TNF-α treatment. J Hepatol. 2020;73:582–92.
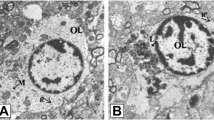
Norenberg MD. A light and electron microscopic study of experimental portal-systemic (ammonia) encephalopathy. Progression and reversal of the disorder. Lab Invest. 1977;36:618–27.
Takahashi H, Koehler RC, Brusilow SW, Traystman RJ. Inhibition of brain glutamine accumulation prevents cerebral edema in hyperammonemic rats. Am J Physiol. 1991;261:H825–829.
Willard-Mack CL, Koehler RC, Hirata T, Cork LC, Takahashi H, Traystman RJ, et al. Inhibition of glutamine synthetase reduces ammonia-induced astrocyte swelling in rat. Neuroscience. 1996;71:589–99.
Tanigami H, Rebel A, Martin LJ, Chen TY, Brusilow SW, Traystman RJ, et al. Effect of glutamine synthetase inhibition on astrocyte swelling and altered astroglial protein expression during hyperammonemia in rats. Neuroscience. 2005;131:437–49.
Elsherbini DMA, Ghoneim FM, El-Mancy EM, Ebrahim HA, El-Sherbiny M, El-Shafey M, et al. Astrocytes profiling in acute hepatic encephalopathy: Possible enrolling of glial fibrillary acidic protein, tumor necrosis factor-alpha, inwardly rectifying potassium channel (Kir 4.1) and aquaporin-4 in rat cerebral cortex. Front Cell Neurosci. 2022;16:896172.
Wang C-C, Chen PS, Hsu C-W, Wu S-J, Lin C-T, Gean PW. Valproic acid mediates the synaptic excitatory/inhibitory balance through astrocytes — A preliminary study. Progr Neuro-Psychopharmacol Biol Psychiatry. 2012;37:111–20.
Takeda K, Watanabe T, Oyabu K, Tsukamoto S, Oba Y, Nakano T, et al. Valproic acid-exposed astrocytes impair inhibitory synapse formation and function. Sci Rep. 2021;11:23.
Tribble JR, Kastanaki E, Uslular AB, Rutigliani C, Enz TJ, Williams PA. Valproic acid reduces neuroinflammation to provide retinal ganglion cell neuroprotection in the retina axotomy model. Front Cell Dev Biol. 2022;10:903436.
Gao X, Zeb S, He Y-Y, Guo Y, Zhu Y-M, Zhou X-Y, et al. Valproic acid inhibits glial scar formation after ischemic stroke. Pharmacology. 2022;107:263–80.
Cuartas CF, Davis M. Valproic acid in the management of delirium. Am J Hosp Palliat Care. 2022;39:562–9.
Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4:147ra111.
Xu Z, Xiao N, Chen Y, Huang H, Marshall C, Gao J, et al. Deletion of aquaporin-4 in APP/PS1 mice exacerbates brain Aβ accumulation and memory deficits. Mol Neurodegener. 2015;10:58.
Ren X, Liu S, Lian C, Li H, Li K, Li L, et al. Dysfunction of the glymphatic system as a potential mechanism of perioperative neurocognitive disorders. Front Aging Neurosci. 2021;13:659457.
Gakuba C, Gaberel T, Goursaud S, Bourges J, Di Palma C, Quenault A, et al. General anesthesia inhibits the activity of the “Glymphatic System”. Theranostics. 2018;8:710–22.
Hu N, Guo D, Wang H, Xie K, Wang C, Li Y, et al. Involvement of the blood-brain barrier opening in cognitive decline in aged rats following orthopedic surgery and high concentration of sevoflurane inhalation. Brain Res. 2014;1551:13–24.
Jiwaji Z, Tiwari SS, Avilés-Reyes RX, Hooley M, Hampton D, Torvell M, et al. Reactive astrocytes acquire neuroprotective as well as deleterious signatures in response to Tau and Aß pathology. Nat Commun. 2022;13:135.
Zhou B, Chen L, Liao P, Huang L, Chen Z, Liao D, et al. Astroglial dysfunctions drive aberrant synaptogenesis and social behavioral deficits in mice with neonatal exposure to lengthy general anesthesia. PLoS Biol. 2019;17:e3000086.
Jacob Z, Li H, Makaryus R, Zhang S, Reinsel R, Lee H, et al. Metabolomic profiling of children’s brains undergoing general anesthesia with sevoflurane and propofol. Anesthesiology. 2012;117:1062–71.
Lilius TO, Blomqvist K, Hauglund NL, Liu G, Stæger FF, Bærentzen S, et al. Dexmedetomidine enhances glymphatic brain delivery of intrathecally administered drugs. J Control Release. 2019;304:29–38.
Benveniste H, Lee H, Ding F, Sun Q, Al-Bizri E, Makaryus R, et al. Anesthesia with Dexmedetomidine and Low-dose Isoflurane Increases Solute Transport via the Glymphatic Pathway in Rat Brain When Compared with High-dose Isoflurane. Anesthesiology. 2017;127:976–88.
Su X, Meng ZT, Wu XH, Cui F, Li HL, Wang DX, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet. 2016;388:1893–902.
Liu H, Davis JR, Wu ZL, Faez Abdelgawad A. Dexmedetomidine attenuates lipopolysaccharide induced MCP-1 expression in primary astrocyte. Biomed Res Int. 2017;2017:6352159.
Wang DS, Kaneshwaran K, Lei G, Mostafa F, Wang J, Lecker I, et al. Dexmedetomidine prevents excessive γ-aminobutyric acid type A receptor function after anesthesia. Anesthesiology. 2018;129:477–89.
Hladky SB, Barrand MA. The glymphatic hypothesis: the theory and the evidence. Fluids Barriers CNS. 2022;19:9.
Prinz M, Priller J. Microglia and brain macrophages in the molecular age: from origin to neuropsychiatric disease. Nat Rev Neurosci. 2014;15:300–12.
Paolicelli RC, Bolasco G, Pagani F, Maggi L, Scianni M, Panzanelli P, et al. Synaptic pruning by microglia is necessary for normal brain development. Science. 2011;333:1456–8.
Schafer DP, Lehrman EK, Kautzman AG, Koyama R, Mardinly AR, Yamasaki R, et al. Microglia sculpt postnatal neural circuits in an activity and complement-dependent manner. Neuron. 2012;74:691–705.
Manich G, Recasens M, Valente T, Almolda B, González B, Castellano B. Role of the CD200-CD200R axis during homeostasis and neuroinflammation. Neuroscience. 2019;405:118–36.
Lemstra AW, Groen in’t Woud JC, Hoozemans JJ, van Haastert ES, Rozemuller AJ, Eikelenboom P, et al. Microglia activation in sepsis: a case-control study. J Neuroinflammation. 2007;4:4.
Chung HY, Wickel J, Hahn N, Mein N, Schwarzbrunn M, Koch P, et al. Microglia mediate neurocognitive deficits by eliminating C1q-tagged synapses in sepsis-associated encephalopathy. Sci Adv. 2023;9:eabq7806.
Peters van Ton AM, Verbeek MM, Alkema W, Pickkers P, Abdo WF. Downregulation of synapse-associated protein expression and loss of homeostatic microglial control in cerebrospinal fluid of infectious patients with delirium and patients with Alzheimer’s disease. Brain Behav Immun. 2020;89:656–67.
Harrison JK, Jiang Y, Chen S, Xia Y, Maciejewski D, McNamara RK, et al. Role for neuronally derived fractalkine in mediating interactions between neurons and CX3CR1-expressing microglia. Proc Natl Acad Sci USA. 1998;95:10896–901.
Hoek RM, Ruuls SR, Murphy CA, Wright GJ, Goddard R, Zurawski SM, et al. Down-regulation of the macrophage lineage through interaction with OX2 (CD200). Science. 2000;290:1768–71.
Ragheb R, Abrahams S, Beecroft R, Hu J, Ni J, Ramakrishna V, et al. Preparation and functional properties of monoclonal antibodies to human, mouse and rat OX-2. Immunol Lett. 1999;68:311–5.
Burguillos MA, Deierborg T, Kavanagh E, Persson A, Hajji N, Garcia-Quintanilla A, et al. Caspase signalling controls microglia activation and neurotoxicity. Nature. 2011;472:319–24.
Henjum K, Quist-Paulsen E, Zetterberg H, Blennow K, Nilsson LNG, Watne LO. CSF sTREM2 in delirium-relation to Alzheimer’s disease CSF biomarkers Aβ42, t-tau and p-tau. J Neuroinflammation. 2018;15:304.
Henry CJ, Huang Y, Wynne AM, Godbout JP. Peripheral lipopolysaccharide (LPS) challenge promotes microglial hyperactivity in aged mice that is associated with exaggerated induction of both pro-inflammatory IL-1beta and anti-inflammatory IL-10 cytokines. Brain Behav Immun. 2009;23:309–17.
Field R, Campion S, Warren C, Murray C, Cunningham C. Systemic challenge with the TLR3 agonist poly I:C induces amplified IFNalpha/beta and IL-1beta responses in the diseased brain and exacerbates chronic neurodegeneration. Brain Behav Immun. 2010;24:996–1007.
Hennessy E, Gormley S, Lopez-Rodriguez AB, Murray C, Murray C, Cunningham C. Systemic TNF-α produces acute cognitive dysfunction and exaggerated sickness behavior when superimposed upon progressive neurodegeneration. Brain Behav Immun. 2017;59:233–44.
Zhao J, Bi W, Xiao S, Lan X, Cheng X, Zhang J, et al. Neuroinflammation induced by lipopolysaccharide causes cognitive impairment in mice. Sci Rep. 2019;9:5790.
Feng X, Valdearcos M, Uchida Y, Lutrin D, Maze M, Koliwad SK. Microglia mediate postoperative hippocampal inflammation and cognitive decline in mice. JCI Insight. 2017;2:e91229.
Mein N, von Stackelberg N, Wickel J, Geis C, Chung HY. Low-dose PLX5622 treatment prevents neuroinflammatory and neurocognitive sequelae after sepsis. J Neuroinflammation. 2023;20:289.
Nikodemova M, Watters JJ, Jackson SJ, Yang SK, Duncan ID. Minocycline down-regulates MHC II expression in microglia and macrophages through inhibition of IRF-1 and protein kinase C (PKC)alpha/betaII. J Biol Chem. 2007;282:15208–16.
Ataie-Kachoie P, Badar S, Morris DL, Pourgholami MH. Minocycline targets the NF-κB nexus through suppression of TGF-β1-TAK1-IκB signaling in ovarian cancer. Mol Cancer Res. 2013;11:1279–91.
Li W, Chai Q, Zhang H, Ma J, Xu C, Dong J, et al. High doses of minocycline may induce delayed activation of microglia in aged rats and thus cannot prevent postoperative cognitive dysfunction. J Int Med Res. 2018;46:1404–13.
Cibelli M, Fidalgo AR, Terrando N, Ma D, Monaco C, Feldmann M, et al. Role of interleukin-1beta in postoperative cognitive dysfunction. Ann Neurol. 2010;68:360–8.
Henry CJ, Huang Y, Wynne A, Hanke M, Himler J, Bailey MT, et al. Minocycline attenuates lipopolysaccharide (LPS)-induced neuroinflammation, sickness behavior, and anhedonia. J Neuroinflammation. 2008;5:15.
Lin SP, Wei JX, Hu JS, Bu JY, Zhu LD, Li Q, et al. Artemisinin improves neurocognitive deficits associated with sepsis by activating the AMPK axis in microglia. Acta Pharmacol Sin. 2021;42:1069–79.
Dal-Pizzol F, Coelho A, Simon CS, Michels M, Corneo E, Jeremias A, et al. Prophylactic Minocycline for Delirium in Critically Ill Patients: A Randomized Controlled Trial. Chest. 2024;165:1129–38.
Takazawa T, Horiuchi T, Orihara M, Nagumo K, Tomioka A, Ideno Y, et al. Prevention of postoperative cognitive dysfunction by minocycline in elderly patients after total knee arthroplasty: a randomized, double-blind, placebo-controlled clinical trial. Anesthesiology. 2023;138:172–83.
Miller-Rhodes P, Li H, Velagapudi R, Chiang W, Terrando N, Gelbard HA. URMC-099 prophylaxis prevents hippocampal vascular vulnerability and synaptic damage in an orthopedic model of delirium superimposed on dementia. FASEB J. 2022;36:e22343.
Zhang Z, Ma Q, Velagapudi R, Barclay WE, Rodriguiz RM, Wetsel WC, et al. Annexin-A1 tripeptide attenuates surgery-induced neuroinflammation and memory deficits through regulation the NLRP3 inflammasome. Front Immunol. 2022;13:856254.
Xu Y, Gao G, Sun X, Liu Q, Li C. ATPase inhibitory factor 1 is critical for regulating sevoflurane-induced microglial inflammatory responses and caspase-3 activation. Front Cell Neurosci. 2021;15:770666.
Griffin ÉW, Skelly DT, Murray CL, Cunningham C. Cyclooxygenase-1-dependent prostaglandins mediate susceptibility to systemic inflammation-induced acute cognitive dysfunction. J Neurosci. 2013;33:15248–58.
Miller-Rhodes P, Kong C, Baht GS, Saminathan P, Rodriguiz RM, Wetsel WC, et al. The broad spectrum mixed-lineage kinase 3 inhibitor URMC-099 prevents acute microgliosis and cognitive decline in a mouse model of perioperative neurocognitive disorders. J Neuroinflammation. 2019;16:193.
Abbott NJ, Patabendige AA, Dolman DE, Yusof SR, Begley DJ. Structure and function of the blood-brain barrier. Neurobiol Dis. 2010;37:13–25.
Hov KR, Berg JP, Frihagen F, Ræder J, Hall R, Wyller TB, et al. Blood-cerebrospinal fluid barrier integrity in delirium determined by Q-albumin. Dement Geriatr Cogn Disord. 2016;41:192–8.
Taylor J, Parker M, Casey CP, Tanabe S, Kunkel D, Rivera C, et al. Postoperative delirium and changes in the blood-brain barrier, neuroinflammation, and cerebrospinal fluid lactate: a prospective cohort study. Br J Anaesth. 2022;129:219–30.
Devinney MJ, Wong MK, Wright MC, Marcantonio ER, Terrando N, Browndyke JN, et al. Role of blood-brain barrier dysfunction in delirium following non-cardiac surgery in older adults. Ann Neurol. 2023;94:1024–35.
Hughes CG, Pandharipande PP, Thompson JL, Chandrasekhar R, Ware LB, Ely EW, et al. Endothelial activation and blood-brain barrier injury as risk factors for delirium in critically Ill patients. Crit Care Med. 2016;44:e809–817.
Hughes CG, Morandi A, Girard TD, Riedel B, Thompson JL, Shintani AK, et al. Association between endothelial dysfunction and acute brain dysfunction during critical illness. Anesthesiology. 2013;118:631–9.
Senatorov VV Jr, Friedman AR, Milikovsky DZ, Ofer J, Saar-Ashkenazy R, Charbash A, et al. Blood-brain barrier dysfunction in aging induces hyperactivation of TGFβ signaling and chronic yet reversible neural dysfunction. Sci Transl Med. 2019;11:eaaw8283.
Yokota H, Ogawa S, Kurokawa A, Yamamoto Y. Regional cerebral blood flow in delirium patients. Psychiatry Clin Neurosci. 2003;57:337–9.
Pfister D, Siegemund M, Dell-Kuster S, Smielewski P, Rüegg S, Strebel SP, et al. Cerebral perfusion in sepsis-associated delirium. Crit Care. 2008;12:R63.
Nishioku T, Dohgu S, Takata F, Eto T, Ishikawa N, Kodama KB, et al. Detachment of brain pericytes from the basal lamina is involved in disruption of the blood-brain barrier caused by lipopolysaccharide-induced sepsis in mice. Cell Mol Neurobiol. 2009;29:309–16.
Handa O, Stephen J, Cepinskas G. Role of endothelial nitric oxide synthase-derived nitric oxide in activation and dysfunction of cerebrovascular endothelial cells during early onsets of sepsis. Am J Physiol Heart Circ Physiol. 2008;295:H1712–1719.
Wang P, Velagapudi R, Kong C, Rodriguiz RM, Wetsel WC, Yang T, et al. Neurovascular and immune mechanisms that regulate postoperative delirium superimposed on dementia. Alzheimers Dement. 2020;16:734–49.
Morandi A, Hughes CG, Girard TD, McAuley DF, Ely EW, Pandharipande PP. Statins and brain dysfunction: a hypothesis to reduce the burden of cognitive impairment in patients who are critically ill. Chest. 2011;140:580–5.
Morandi A, Hughes CG, Thompson JL, Pandharipande PP, Shintani AK, Vasilevskis EE, et al. Statins and delirium during critical illness: a multicenter, prospective cohort study. Crit Care Med. 2014;42:1899–909.
Andonegui G, Zelinski EL, Schubert CL, Knight D, Craig LA, Winston BW, et al. Targeting inflammatory monocytes in sepsis-associated encephalopathy and long-term cognitive impairment. JCI Insight. 2018;3:e99364.
Yang T, Velagapudi R, Kong C, Ko U, Kumar V, Brown P, et al. Protective effects of omega-3 fatty acids in a blood-brain barrier-on-chip model and on postoperative delirium-like behaviour in mice. Br J Anaesth. 2023;130:e370–e380.
Hughes CG, Brummel NE, Girard TD, Graves AJ, Ely EW, Pandharipande PP. Change in endothelial vascular reactivity and acute brain dysfunction during critical illness. Br J Anaesth. 2015;115:794–5.
Morandi A, Gunther ML, Vasilevskis EE, Girard TD, Hopkins RO, Jackson JC, et al. Neuroimaging in delirious intensive care unit patients: a preliminary case series report. Psychiatry (Edgmont). 2010;7:28–33.
Pendlebury ST, Thomson RJ, Welch SJV, Kuker W, Rothwell PM; Oxford Vascular Study. Utility of white matter disease and atrophy on routinely acquired brain imaging for prediction of long-term delirium risk: population-based cohort study. Age Ageing. 2022;51:afab200.
Shioiri A, Kurumaji A, Takeuchi T, Matsuda H, Arai H, Nishikawa T. White matter abnormalities as a risk factor for postoperative delirium revealed by diffusion tensor imaging. Am J Geriatr Psychiatry. 2010;18:743–53.
Healy D, Murray C, McAdams C, Power R, Hollier PL, Lambe J, et al. Susceptibility to acute cognitive dysfunction in aged mice is underpinned by reduced white matter integrity and microgliosis. Commun Biol. 2024;7:105.
Czyzycki M, Glen A, Slowik A, Chrzan R, Dziedzic T. Clinical utility of brain computed tomography in prediction of post-stroke delirium. J Neural Transm (Vienna). 2021;128:207–13.
Cavallari M, Hshieh TT, Guttmann CR, Ngo LH, Meier DS, Schmitt EM, et al. Brain atrophy and white-matter hyperintensities are not significantly associated with incidence and severity of postoperative delirium in older persons without dementia. Neurobiol Aging. 2015;36:2122–9.
Kant IMJ, de Bresser J, van Montfort SJT, Mutsaerts H, Witkamp TD, Buijsrogge M, et al. Preoperative brain MRI features and occurrence of postoperative delirium. J Psychosom Res. 2021;140:110301.
Kant IMJ, de Bresser J, van Montfort SJT, Witkamp TD, Walraad B, Spies CD, et al. Postoperative delirium is associated with grey matter brain volume loss. Brain Commun. 2023;5:fcad013.
Sharshar T, Carlier R, Bernard F, Guidoux C, Brouland JP, Nardi O, et al. Brain lesions in septic shock: a magnetic resonance imaging study. Intensive Care Med. 2007;33:798–806.
Morandi A, Rogers BP, Gunther ML, Merkle K, Pandharipande P, Girard TD, et al. The relationship between delirium duration, white matter integrity, and cognitive impairment in intensive care unit survivors as determined by diffusion tensor imaging: the VISIONS prospective cohort magnetic resonance imaging study. Crit Care Med. 2012;40:2182–9.
Rau A, Schroeter N, Blazhenets G, Dressing A, Walter LI, Kellner E, et al. Widespread white matter oedema in subacute COVID-19 patients with neurological symptoms. Brain. 2022;145:3203–13.
Masgrau R, Guaza C, Ransohoff RM, Galea E. Should we stop saying ‘Glia’ and ‘Neuroinflammation’? Trends Mol Med. 2017;23:486–500.
Lyon KA, Allen NJ. From synapses to circuits, astrocytes regulate behavior. Front Neural Circuits. 2021;15:786293.
Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541:481–7.
Yun SP, Kam TI, Panicker N, Kim S, Oh Y, Park JS, et al. Block of A1 astrocyte conversion by microglia is neuroprotective in models of Parkinson’s disease. Nat Med. 2018;24:931–8.
Harada R, Furumoto S, Kudo Y, Yanai K, Villemagne VL, Okamura N. Imaging of reactive astrogliosis by positron emission tomography. Front Neurosci. 2022;16:807435.
David-Bercholz J, Acker L, Caceres AI, Wu PY, Goenka S, Franklin NO, et al. Conserved YKL-40 changes in mice and humans after postoperative delirium. Brain Behav Immun Health. 2022;26:100555.
Vasunilashorn SM, Dillon ST, Chan NY, Fong TG, Joseph M, Tripp B, et al. Proteome-wide analysis using SOMAscan identifies and validates chitinase-3-like protein 1 as a risk and disease marker of delirium among older adults undergoing major elective surgery. J Gerontol A Biol Sci Med Sci. 2022;77:484–93.
Liu X, Chen Y, Wang H, Wei Y, Yuan Y, Zhou Q, et al. Microglia-derived IL-1β promoted neuronal apoptosis through ER stress-mediated signaling pathway PERK/eIF2α/ATF4/CHOP upon arsenic exposure. J Hazard Mater. 2021;417:125997.
Lee YB, Yune TY, Baik SY, Shin YH, Du S, Rhim H, et al. Role of tumor necrosis factor-alpha in neuronal and glial apoptosis after spinal cord injury. Exp Neurol. 2000;166:190–5.
Cunningham AJ, Murray CA, O’Neill LA, Lynch MA, O’Connor JJ. Interleukin-1 beta (IL-1 beta) and tumour necrosis factor (TNF) inhibit long-term potentiation in the rat dentate gyrus in vitro. Neurosci Lett. 1996;203:17–20.
de Vries HE, Blom-Roosemalen MC, van Oosten M, de Boer AG, van Berkel TJ, Breimer DD, et al. The influence of cytokines on the integrity of the blood-brain barrier in vitro. J Neuroimmunol. 1996;64:37–43.
Wieloch T, Engelsen B, Westerberg E, Auer R. Lesions of the glutamatergic cortico-striatal projections in the rat ameliorate hypoglycemic brain damage in the striatum. Neurosci Lett. 1985;58:25–30.
Arvanitakis Z, Fleischman DA, Arfanakis K, Leurgans SE, Barnes LL, Bennett DA. Association of white matter hyperintensities and gray matter volume with cognition in older individuals without cognitive impairment. Brain Struct Funct. 2016;221:2135–46.
Kloppenborg RP, Nederkoorn PJ, Geerlings MI, van den Berg E. Presence and progression of white matter hyperintensities and cognition: a meta-analysis. Neurology. 2014;82:2127–38.
Zhai F, Liu J, Su N, Han F, Zhou L, Ni J, et al. Disrupted white matter integrity and network connectivity are related to poor motor performance. Sci Rep. 2020;10:18369.
Acknowledgements
Figure 1 was created using BioRender.
Funding
This work is supported by the UK Dementia Research Institute (award number UK DRI-4010 and UK DRI-4003) through UK DRI Ltd, principally funded by the Medical Research Council.
Author information
Authors and Affiliations
Contributions
ÁBH and MS conceptualised the manuscript. ÁBH prepared the initial draft and designed the figure. MoS and GD participated in the preparation of the manuscript. ÁBH, MS, MoS, BTS, SC and ZJ reviewed the manuscript and prepared the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heffernan, Á.B., Steinruecke, M., Dempsey, G. et al. Role of glia in delirium: proposed mechanisms and translational implications. Mol Psychiatry 30, 1138–1147 (2025). https://doi.org/10.1038/s41380-024-02801-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-024-02801-4