Abstract
Major depression, type 2 diabetes, and essential (primary) hypertension are chronic medical and psychiatric disorders that have traditionally affected primarily adults and middle-aged individuals. However, recent decades have witnessed an increasing prevalence of these conditions among children and adolescents. For diseases that typically require prolonged exposure to risk factors to emerge in childhood and adolescence, the amount of exposure to a single risk factor would have to be exceptionally high. We advance the alternative hypothesis of multiple factors acting synergistically. Biological mechanisms underlying the response to ongoing (chronic) stress are logical candidates for being a shared pathway. In the context of persistent and synergistic psychological, social, and economic pressures, unremitting stress can lead to such disease outcomes, exerting a direct influence on the emergence of chronic disorders, and it can also contribute to obesity. Depression follows the same trajectory; therefore, we should examine it as an entity whose consequences are directly reflected in behavioral outcomes, including (over-) eating. Other contributing pathways include chronic sleep deprivation, epigenetic modifications, telomere shortening, the physical environment, pathogens, and the microbiome. We introduce here the concept of the Chronic inflammation, Obesity, Insulin resistance/type 2 diabetes, and Depressive Syndromes (COIDS) noxious quartet of pro-inflammatory stress outcomes, as an increasingly common pathophysiologic state, representing a distinct presentation of type 2 allostatic overload, with direct implications for the current chronic disease epidemic. The compounded effects of a pro-inflammatory state that is fueled by four different and co-existing sources may contribute to explain the emergence of chronic diseases of adulthood and middle age in the young. PPARγ might represent a potential translational therapeutic target for those with COIDS. We propose that highly adverse environments sustain sufficient chronic stress to bring about in the young diseases that had been previously confined to adults.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Notes
BMI – Body Mass Index is the quotient of an individual’s weight in kilograms by the square root of his height in meters. Overweight and obesity are widely regarded as having BMIs above 25 and 30 kg/m2, respectively.
GDP – Gross Domestic Product is a measure of the size of a region’s economy, commonly defined as the market value of all final goods and services produced within a country in a given period of time.
NHANES – The National Health and Nutrition Examination Survey is an ongoing survey conducted by the United States Center for Disease Control and the National Centers for Health Statistics designed to assess the health and nutritional status of adults and children in the United States through interviews and direct physical examinations.
References
Phipps SA, Burton PS, Osberg LS, Lethbridge LN. Poverty and the extent of child obesity in Canada, Norway and the United States. Obes Rev. 2006;7:5–12. https://doi.org/10.1111/j.1467-789X.2006.00217.x.
Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. https://doi.org/10.1093/ajcn/79.1.6.
Ezzati M, Vander Hoorn S, Lawes CM, Leach R, James WP, Lopez AD, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2:e133. https://doi.org/10.1371/journal.pmed.0020133.
Dennison BA, Erb TA, Jenkins PL. Television viewing and television in bedroom associated with overweight risk among low-income preschool children. Pediatrics. 2002;109:1028–35. https://doi.org/10.1542/peds.109.6.1028.
Blackwell DL, Tonthat L. Summary health statistics for the U.S. population: national health interview survey, 1999. Vital Health Stat 10. 2003;211:1–94.
Hemmingsson E, Nowicka P, Ulijaszek S, Sorensen TIA. The social origins of obesity within and across generations. Obes Rev. 2023;24:e13514. https://doi.org/10.1111/obr.13514.
Schwarz PE, Reimann M, Li J, Bergmann A, Licinio J, Wong ML, et al. The metabolic syndrome - a global challenge for prevention. Horm Metab Res. 2007;39:777–80. https://doi.org/10.1055/s-2007-990312.
Ehrlich PR. The population bomb. New York: Intext; 1971.
Bornstein SR, Ehrhart-Bornstein M, Wong ML, Licinio J. Is the worldwide epidemic of obesity a communicable feature of globalization? Exp Clin Endocrinol Diabetes. 2008;116:S30–32. https://doi.org/10.1055/s-2008-1081485.
Shafrir E. Development and consequences of insulin resistance: lessons from animals with hyperinsulinaemia. Diabetes Metab. 1996;22:122–31.
Reed J, Bain S, Kanamarlapudi V. A review of current trends with type 2 diabetes epidemiology, aetiology, pathogenesis, treatments and future perspectives. Diabetes Metab Syndr Obes. 2021;14:3567–602. https://doi.org/10.2147/DMSO.S319895.
Amutha A, Mohan V. Diabetes complications in childhood and adolescent onset type 2 diabetes-a review. J Diabetes Complications. 2016;30:951–7. https://doi.org/10.1016/j.jdiacomp.2016.02.009.
Kautzky-Willer A, Harreiter J, Pacini G. Sex and gender differences in risk, pathophysiology and complications of type 2 diabetes mellitus. Endocr Rev. 2016;37:278–316. https://doi.org/10.1210/er.2015-1137.
Groves BM, Zuckerman B, Marans S, Cohen DJ. Silent victims. Children who witness violence. JAMA. 1993;269:262–4.
Agid O, Shapira B, Zislin J, Ritsner M, Hanin B, Murad H, et al. Environment and vulnerability to major psychiatric illness: a case control study of early parental loss in major depression, bipolar disorder and schizophrenia. Mol Psychiatry. 1999;4:163–72.
Evans GW. The environment of childhood poverty. Am Psychol. 2004;59:77–92. https://doi.org/10.1037/0003-066X.59.2.77.
Drake B, Pandey S. Understanding the relationship between neighborhood poverty and specific types of child maltreatment. Child Abuse Negl. 1996;20:1003–18. https://doi.org/10.1016/0145-2134(96)00091-9.
Li X, Stanton B, Feigelman S. Exposure to drug trafficking among urban, low-income African American children and adolescents. Arch Pediatr Adolesc Med. 1999;153:161–8. https://doi.org/10.1001/archpedi.153.2.161.
Hobson JM, Moody MD, Sorge RE, Goodin BR. The neurobiology of social stress resulting from Racism: implications for pain disparities among racialized minorities. Neurobiol Pain. 2022;12:100101. https://doi.org/10.1016/j.ynpai.2022.100101. PMC9449662
LLerena A, Dorado P, O’Kirwan F, Jepson R, Licinio J, Wong ML. Lower frequency of CYP2C9*2 in Mexican-Americans compared to Spaniards. Pharmacogenomics J. 2004;4:403–6. https://doi.org/10.1038/sj.tpj.6500278.
Daniel-Calveras A, Baldaqui N, Baeza I. Mental health of unaccompanied refugee minors in Europe: a systematic review. Child Abuse Negl. 2022;133:105865. https://doi.org/10.1016/j.chiabu.2022.105865.
de Kloet ER, Joels M. The cortisol switch between vulnerability and resilience. Mol Psychiatry. 2024;29:20–34. https://doi.org/10.1038/s41380-022-01934-8.
Agorastos A, Chrousos GP. The neuroendocrinology of stress: the stress-related continuum of chronic disease development. Mol Psychiatry. 2022;27:502–13. https://doi.org/10.1038/s41380-021-01224-9.
Sternberg EM, Licinio J. Overview of neuroimmune stress interactions. implications for susceptibility to inflammatory disease. Ann N Y Acad Sci. 1995;771:364–71. https://doi.org/10.1111/j.1749-6632.1995.tb44695.x.
Licinio J, Frost P. The neuroimmune-endocrine axis: pathophysiological implications for the central nervous system cytokines and hypothalamus-pituitary-adrenal hormone dynamics. Braz J Med Biol Res. 2000;33:1141–8. https://doi.org/10.1590/s0100-879x2000001000003.
Inserra A, Rogers GB, Licinio J, Wong ML. The microbiota-inflammasome hypothesis of major depression. Bioessays. 2018;40:e1800027. https://doi.org/10.1002/bies.201800027.
McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med. 1993;153:2093–101.
McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Horm Behav. 2003;43:2–15. https://doi.org/10.1016/s0018-506x(02)00024-7.
Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS, et al. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152:940.e941–948. https://doi.org/10.1016/j.ahj.2006.05.009.
Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–217. https://doi.org/10.1161/01.cir.99.16.2192.
Matthews K, Schwartz J, Cohen S, Seeman T. Diurnal cortisol decline is related to coronary calcification: CARDIA study. Psychosom Med. 2006;68:657–61. https://doi.org/10.1097/01.psy.0000244071.42939.0e.
Falkner B, Onesti G, Angelakos ET, Fernandes M, Langman C. Cardiovascular response to mental stress in normal adolescents with hypertensive parents. Hemodynamics and mental stress in adolescents. Hypertension. 1979;1:23–30. https://doi.org/10.1161/01.hyp.1.1.23.
Peyrot MF, McMurry JF Jr. Stress buffering and glycemic control. The role of coping styles. Diabetes Care. 1992;15:842–6. https://doi.org/10.2337/diacare.15.7.842.
Kai K, Morimoto I, Morita E, Okada Y, Yamamoto S, Kanda K, et al. Environmental stress modifies glycemic control and diabetes onset in type 2 diabetes prone otsuka long evans tokushima fatty (OLETF) rats. Physiol Behav. 2000;68:445–52. https://doi.org/10.1016/s0031-9384(99)00187-0.
Kessler RC, Walters EE. Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the national comorbidity survey. Depress Anxiety. 1998;7:3–14.
Wong ML, Dong C, Andreev V, Arcos-Burgos M, Licinio J. Prediction of susceptibility to major depression by a model of interactions of multiple functional genetic variants and environmental factors. Mol Psychiatry. 2012;17:624–33. https://doi.org/10.1038/mp.2012.13.
Thapar A, Eyre O, Patel V, Brent D. Depression in young people. Lancet. 2022;400:617–31. https://doi.org/10.1016/S0140-6736(22)01012-1.
Lavori PW, Klerman GL, Keller MB, Reich T, Rice J, Endicott J. Age-period-cohort analysis of secular trends in onset of major depression: findings in siblings of patients with major affective disorder. J Psychiatr Res. 1987;21:23–35. https://doi.org/10.1016/0022-3956(87)90006-9.
Torrey EF, Miller J. The invisible plague: the rise of mental illness from 1750 to the present. xiv. New Brunswick, NJ: Rutgers University Press; 2001. p. 416 p.
Young LR, Nestle M. The contribution of expanding portion sizes to the US obesity epidemic. Am J Public Health. 2002;92:246–9. https://doi.org/10.2105/ajph.92.2.246.
Epel E, Jimenez S, Brownell K, Stroud L, Stoney C, Niaura R. Are stress eaters at risk for the metabolic syndrome? Ann N Y Acad Sci. 2004;1032:208–10. https://doi.org/10.1196/annals.1314.022.
Steenblock C, Schwarz PEH, Ludwig B, Linkermann A, Zimmet P, Kulebyakin K, et al. COVID-19 and metabolic disease: mechanisms and clinical management. Lancet Diabetes Endocrinol. 2021;9:786–98. https://doi.org/10.1016/S2213-8587(21)00244-8. receiving grants for investigator-initiated studies for AstraZeneca, Novartis, Novo Nordisk, Sanofi-Aventis, Lilly and Merck Sharp & Dohme, Boehringer Ingelheim, Bayer, Berlin-Chemie AG-Menarini Group, Janssen, and Napp. JSS reports personal fees as a consultant or advisor for Abvance, Adocia, Astra-Zeneca, Avotres, Bayer, Biozeus, Boehringer-Ingelheim, Dalcor, Dance Biopharm-Aerami Therapeutics, Diavacs, Duologics, Elcelyx, Eli Lilly, Enthera, Esperion, Geneuro, Ideal Life, Imcyse, Immunomolecular Therapeutics, Intarcia, Kamada, Kriya, Moerae Matrix, Novo-Nordisk, Oramed, Orgenesis, Pila Pharma, Precigen ActoBiotics, Preziba/Signos, Provention Bio, Sanofi, Tolerion, Valeritas, Viacyte, Viela Bio, vTv Therapeutics, and Zafgen. JHDV reports personal fees as consultant or advisor for Adocia, Novo Nordisk, and Zealand. ER reports personal fees as consultant or advisor for Abbott, Air Liquide, AstraZeneca, Boehringer-Ingelheim, Cellnovo, Dexcom, Eli Lilly, Insulet, Johnson & Johnson (Animas, LifeScan), Medirio, Medtronic, Novo Nordisk, Roche Diagnostics, Sanofi-Aventis, and Tandem; and research grant or material support from Abbott, Dexcom, Insulet, Roche Diagnostics, and Tandem. BG reports personal fees as consultant or advisor for Novo Nordisk, Pfizer, Merck Sharp & Dohme, Astra Zeneca, and Takeda. FR reports personal fees as a consultant or advisor for Ethicon, Medtronic, and Novo Nordisk. All other authors declare no competing interests
Steenblock C, Schwarz PEH, Perakakis N, Brajshori N, Beqiri P, Bornstein SR. The interface of COVID-19, diabetes, and depression. Discov Ment Health. 2022;2:5. https://doi.org/10.1007/s44192-44022-00007-44190.
Steenblock C, Toepfner N, Kok YP, Mavberg P, Bruckmoser H, Breu A, et al. A multimodal approach for treating post-acute infectious syndrome. Brain Medicine. 2024:1-7. https://doi.org/10.61373/bm024p.0064.
Siddiq S, Ahmed S, Akram I. Clinical outcomes following COVID-19 infection in ethnic minority groups in the UK: a systematic review and meta-analysis. Public Health. 2023;222:205–14. https://doi.org/10.1016/j.puhe.2022.05.019.
Lee FC, Adams L, Graves SJ, Massetti GM, Calanan RM, Penman-Aguilar A, et al. Counties with High COVID-19 incidence and relatively large racial and ethnic minority populations - United States, April 1-December 22, 2020. MMWR Morb Mortal Wkly Rep. 2021;70:483–9. https://doi.org/10.15585/mmwr.mm7013e1. PMC8022874 Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed
Fabiano N, Luu B, Puder D Human microplastic removal: what does the evidence tell us? Brain Medicine. 2025:1-2. https://doi.org/10.61373/bm025c.0020.
Nihart AJ, Garcia MA, El Hayek E, Liu R, Olewine M, Kingston JD, et al. Bioaccumulation of microplastics in decedent human brains. Nature medicine. 2025. https://doi.org/10.1038/s41591-024-03453-1.
Estadella D, da Penha Oller do Nascimento CM, Oyama LM, Ribeiro EB, Damaso AR, de Piano A. Lipotoxicity: effects of dietary saturated and transfatty acids. Mediators Inflamm. 2013;2013:137579. https://doi.org/10.1155/2013/137579.
Sick E, Brehin S, Andre P, Coupin G, Landry Y, Takeda K, et al. Advanced glycation end products (AGEs) activate mast cells. Br J Pharmacol. 2010;161:442–55. https://doi.org/10.1111/j.1476-5381.2010.00905.x.
Tristan Asensi M, Napoletano A, Sofi F, Dinu M. Low-grade inflammation and ultra-processed foods consumption: a review. Nutrients. 2023;15:1546. https://doi.org/10.3390/nu15061546.
Gold PW, Wong ML, Goldstein DS, Gold HK, Ronsaville DS, Esler M, et al. Cardiac implications of increased arterial entry and reversible 24-h central and peripheral norepinephrine levels in melancholia. Proc Natl Acad Sci USA. 2005;102:8303–8. https://doi.org/10.1073/pnas.0503069102.
Carroll BJ, Curtis GC, Davies BM, Mendels J, Sugarman AA. Urinary free cortisol excretion in depression. Psychol Med. 1976;6:43–50.
Bornstein SR, Schuppenies A, Wong ML, Licinio J. Approaching the shared biology of obesity and depression: the stress axis as the locus of gene-environment interactions. Mol Psychiatry. 2006;11:892–902. https://doi.org/10.1038/sj.mp.4001873.
Steenblock C, Todorov V, Kanczkowski W, Eisenhofer G, Schedl A, Wong ML, et al. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the neuroendocrine stress axis. Mol Psychiatry. 2020;25:1611–7. https://doi.org/10.1038/s41380-020-0758-9.
Joseph JJ, Golden SH. Cortisol dysregulation: the bidirectional link between stress, depression, and type 2 diabetes mellitus. Ann N Y Acad Sci. 2017;1391:20–34. https://doi.org/10.1111/nyas.13217.
Bornstein SR, Voit-Bak K, Donate T, Rodionov RN, Gainetdinov RR, Tselmin S, et al. Chronic post-COVID-19 syndrome and chronic fatigue syndrome: Is there a role for extracorporeal apheresis? Mol Psychiatry. 2022;27:34–7. https://doi.org/10.1038/s41380-021-01148-4.
Licinio J, Wong ML. The role of inflammatory mediators in the biology of major depression: central nervous system cytokines modulate the biological substrate of depressive symptoms, regulate stress-responsive systems, and contribute to neurotoxicity and neuroprotection. Mol Psychiatry. 1999;4:317–27. https://doi.org/10.1038/sj.mp.4000586.
Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care. 2004;27:813–23. https://doi.org/10.2337/diacare.27.3.813.
Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H, et al. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw. 2006;17:4–12.
Yin M, Marrone L, Peace CG, O’Neill LAJ. NLRP3, the inflammasome and COVID-19 infection. QJM. 2023;116:502–7. https://doi.org/10.1093/qjmed/hcad011.
Wong ML, Inserra A, Lewis MD, Mastronardi CA, Leong L, Choo J, et al. Inflammasome signaling affects anxiety- and depressive-like behavior and gut microbiome composition. Mol Psychiatry. 2016;21:797–805. https://doi.org/10.1038/mp.2016.46.
Rheinheimer J, de Souza BM, Cardoso NS, Bauer AC, Crispim D. Current role of the NLRP3 inflammasome on obesity and insulin resistance: a systematic review. Metabolism. 2017;74:1–9. https://doi.org/10.1016/j.metabol.2017.06.002.
Wada J, Makino H. Innate immunity in diabetes and diabetic nephropathy. Nat Rev Nephrol. 2016;12:13–26. https://doi.org/10.1038/nrneph.2015.175.
Wang D, Wang H, Gao H, Zhang H, Zhang H, Wang Q, et al. P2X7 receptor mediates NLRP3 inflammasome activation in depression and diabetes. Cell Biosci. 2020;10:28. https://doi.org/10.1186/s13578-020-00388-1.
Alesci S, Martinez PE, Kelkar S, Ilias I, Ronsaville DS, Listwak SJ, et al. Major depression is associated with significant diurnal elevations in plasma interleukin-6 levels, a shift of its circadian rhythm, and loss of physiological complexity in its secretion: clinical implications. J Clin Endocrinol Metab. 2005;90:2522–30. https://doi.org/10.1210/jc.2004-1667.
Kreiner FF, Kraaijenhof JM, von Herrath M, Hovingh GKK, von Scholten BJ. Interleukin 6 in diabetes, chronic kidney disease, and cardiovascular disease: mechanisms and therapeutic perspectives. Expert Rev Clin Immunol. 2022;18:377–89. https://doi.org/10.1080/1744666X.2022.2045952.
Chattu VK, Chattu SK, Spence DW, Manzar MD, Burman D, Pandi-Perumal SR. Do disparities in sleep duration among racial and ethnic minorities contribute to differences in disease prevalence? J Racial Ethn Health Disparities. 2019;6:1053–61. https://doi.org/10.1007/s40615-019-00607-7.
Chattu VK, Chattu SK, Burman D, Spence DW, Pandi-Perumal SR. The interlinked rising epidemic of insufficient sleep and diabetes mellitus. Healthcare. 2019;7:37. https://doi.org/10.3390/healthcare7010037.
Salomon RM, Delgado PL, Licinio J, Krystal JH, Heninger GR, Charney DS. Effects of sleep deprivation on serotonin function in depression. Biol Psychiatry. 1994;36:840–6.
Shoubridge AP, Choo JM, Martin AM, Keating DJ, Wong ML, Licinio J, et al. The gut microbiome and mental health: advances in research and emerging priorities. Mol Psychiatry. 2022;27:1908–19. https://doi.org/10.1038/s41380-022-01479-w.
Zheng P, Zeng B, Zhou C, Liu M, Fang Z, Xu X, et al. Gut microbiome remodeling induces depressive-like behaviors through a pathway mediated by the host’s metabolism. Mol Psychiatry. 2016;21:786–96. https://doi.org/10.1038/mp.2016.44.
Zheng P, Yang J, Li Y, Wu J, Liang W, Yin B, et al. Gut microbial signatures can discriminate unipolar from bipolar depression. Adv Sci. 2020;7:1902862. https://doi.org/10.1002/advs.201902862.
Sankararaman S, Noriega K, Velayuthan S, Sferra T, Martindale R. Gut microbiome and its impact on obesity and obesity-related disorders. Curr Gastroenterol Rep. 2023;25:31–44. https://doi.org/10.1007/s11894-022-00859-0.
Wijdeveld M, Nieuwdorp M, IJzerman R. The interaction between microbiome and host central nervous system: the gut-brain axis as a potential new therapeutic target in the treatment of obesity and cardiometabolic disease. Expert Opin Ther Targets. 2020;24:639–53. https://doi.org/10.1080/14728222.2020.1761958.
Delzenne NM, Rodriguez J, Olivares M, Neyrinck AM. Microbiome response to diet: focus on obesity and related diseases. Rev Endocr Metab Disord. 2020;21:369–80. https://doi.org/10.1007/s11154-020-09572-7.
Lim YY, Lee YS, Ooi DSQ. Engineering the gut microbiome for treatment of obesity: a review of current understanding and progress. Biotechnol J. 2020;15:e2000013. https://doi.org/10.1002/biot.202000013.
Borrello K, Lim U, Park SY, Monroe KR, Maskarinec G, Boushey CJ, et al. Dietary intake mediates ethnic differences in gut microbial composition. Nutrients. 2022;14:660. https://doi.org/10.3390/nu14030660.
Parade SH, Huffhines L, Daniels TE, Stroud LR, Nugent NR, Tyrka AR. A systematic review of childhood maltreatment and DNA methylation: candidate gene and epigenome-wide approaches. Transl Psychiatry. 2021;11:134. https://doi.org/10.1038/s41398-021-01207-y.
Radtke KM, Schauer M, Gunter HM, Ruf-Leuschner M, Sill J, Meyer A, et al. Epigenetic modifications of the glucocorticoid receptor gene are associated with the vulnerability to psychopathology in childhood maltreatment. Transl Psychiatry. 2015;5:e571. https://doi.org/10.1038/tp.2015.63.
Ramo-Fernandez L, Gumpp AM, Boeck C, Krause S, Bach AM, Waller C, et al. Associations between childhood maltreatment and DNA methylation of the oxytocin receptor gene in immune cells of mother-newborn dyads. Transl Psychiatry. 2021;11:449. https://doi.org/10.1038/s41398-021-01546-w.
Perroud N, Paoloni-Giacobino A, Prada P, Olie E, Salzmann A, Nicastro R, et al. Increased methylation of glucocorticoid receptor gene (NR3C1) in adults with a history of childhood maltreatment: a link with the severity and type of trauma. Transl Psychiatry. 2011;1:e59. https://doi.org/10.1038/tp.2011.60.
Roberts AL, Gladish N, Gatev E, Jones MJ, Chen Y, MacIsaac JL, et al. Exposure to childhood abuse is associated with human sperm DNA methylation. Transl Psychiatry. 2018;8:194. https://doi.org/10.1038/s41398-018-0252-1.
Arias E, Xu J. United States life tables, 2020. Natl Vital Stat Rep. 2022;71:1–64.
Gilson E, Segal-Bendirdjian E. The telomere story or the triumph of an open-minded research. Biochimie. 2010;92:321–6. https://doi.org/10.1016/j.biochi.2009.12.014.
Shammas MA. Telomeres, lifestyle, cancer, and aging. Curr Opin Clin Nutr Metab Care. 2011;14:28–34. https://doi.org/10.1097/MCO.0b013e32834121b1.
Whittemore K, Vera E, Martinez-Nevado E, Sanpera C, Blasco MA. Telomere shortening rate predicts species life span. Proc Natl Acad Sci USA. 2019;116:15122–7. https://doi.org/10.1073/pnas.1902452116.
Heidinger BJ, Blount JD, Boner W, Griffiths K, Metcalfe NB, Monaghan P. Telomere length in early life predicts lifespan. Proc Natl Acad Sci USA. 2012;109:1743–8. https://doi.org/10.1073/pnas.1113306109.
Topiwala A, Taschler B, Ebmeier KP, Smith S, Zhou H, Levey DF, et al. Alcohol consumption and telomere length: mendelian randomization clarifies alcohol’s effects. Mol Psychiatry. 2022;27:4001–8. https://doi.org/10.1038/s41380-022-01690-9. PMC9718662 financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work
Jung J, McCartney DL, Wagner J, Rosoff DB, Schwandt M, Sun H, et al. Alcohol use disorder is associated with DNA methylation-based shortening of telomere length and regulated by TESPA1: implications for aging. Mol Psychiatry. 2022;27:3875–84. https://doi.org/10.1038/s41380-022-01624-5.
Cabeza de Baca T, Prather AA, Lin J, Sternfeld B, Adler N, Epel ES, et al. Chronic psychosocial and financial burden accelerates 5-year telomere shortening: findings from the coronary artery risk development in young adults study. Mol Psychiatry. 2020;25:1141–53. https://doi.org/10.1038/s41380-019-0482-5.
Ayora M, Fraguas D, Abregu-Crespo R, Recio S, Blasco MA, Moises A, et al. Leukocyte telomere length in patients with schizophrenia and related disorders: a meta-analysis of case-control studies. Mol Psychiatry. 2022;27:2968–75. https://doi.org/10.1038/s41380-022-01541-7.
Spano L, Etain B, Meyrel M, Hennion V, Gross G, Laplanche JL, et al. Telomere length and mitochondrial DNA copy number in bipolar disorder: identification of a subgroup of young individuals with accelerated cellular aging. Transl Psychiatry. 2022;12:135. https://doi.org/10.1038/s41398-022-01891-4. PMC8975957 symposium speaker from Sanofi-Aventis, Lundbeck, AstraZeneca, Eli Lilly, Bristol-Myers Squibb, and Servier. B. Etain has received honoraria from Sanofi-Aventis. The remaining authors declare no competing interests
Lin YF, Chen PY, Liu HC, Chen YL, Chou WH, Huang MC. Shortened leukocyte telomere length in young adults who use methamphetamine. Transl Psychiatry. 2021;11:519. https://doi.org/10.1038/s41398-021-01640-z.
Leaderer BP, Belanger K, Triche E, Holford T, Gold DR, Kim Y, et al. Dust mite, cockroach, cat, and dog allergen concentrations in homes of asthmatic children in the northeastern United States: impact of socioeconomic factors and population density. Environ Health Perspect. 2002;110:419–25. https://doi.org/10.1289/ehp.02110419.
Lanphear BP, Kahn RS, Berger O, Auinger P, Bortnick SM, Nahhas RW. Contribution of residential exposures to asthma in us children and adolescents. Pediatrics. 2001;107:E98. https://doi.org/10.1542/peds.107.6.e98.
Janani C, Ranjitha Kumari BD. PPAR gamma gene–a review. Diabetes Metab Syndr. 2015;9:46–50. https://doi.org/10.1016/j.dsx.2014.09.015.
Gold PW. The PPARg system in major depression: pathophysiologic and therapeutic implications. Int J Mol Sci. 2021;22:9248. https://doi.org/10.3390/ijms22179248.
Devchand PR, Liu T, Altman RB, FitzGerald GA, Schadt EE. The pioglitazone trek via human PPAR gamma: from discovery to a medicine at the FDA and beyond. Front Pharmacol. 2018;9:1093. https://doi.org/10.3389/fphar.2018.01093.
Rasgon N, Lin KW, Lin J, Epel E, Blackburn E. Telomere length as a predictor of response to pioglitazone in patients with unremitted depression: a preliminary study. Transl Psychiatry. 2016;6:e709. https://doi.org/10.1038/tp.2015.187. PMC5068869 role in this study. NR has been a consultant for the following companies: Shire Pharmaceuticals and Sunovion Pharmaceuticals. She has received research support from the following companies: Magceutics, ADA (American Diabetes Association) and Corcept Pharmaceuticals. None of these companies have a potential role in this study. The remaining authors declare no conflict of interest
Mahmudpour M, Vahdat K, Keshavarz M, Nabipour I. The COVID-19-diabetes mellitus molecular tetrahedron. Mol Biol Rep. 2022;49:4013–24. https://doi.org/10.1007/s11033-021-07109-y.
Inserra A, Mastronardi CA, Rogers G, Licinio J, Wong ML. Neuroimmunomodulation in major depressive disorder: focus on caspase 1, inducible nitric oxide synthase, and interferon-gamma. Mol Neurobiol. 2019;56:4288–305. https://doi.org/10.1007/s12035-018-1359-3.
Bornstein SR, Licinio J. Improving the efficacy of translational medicine by optimally integrating health care, academia and industry. Nat Med. 2011;17:1567–9. https://doi.org/10.1038/nm.2583.
Lores T, Musker M, Collins K, Burke A, Perry SW, Wong ML, et al. Pilot trial of a group cognitive behavioural therapy program for comorbid depression and obesity. BMC Psychol. 2020;8:34. https://doi.org/10.1186/s40359-020-00400-w.
Funding
Grants R01MH127423, R21MH128726, R21MH126405, National Institute of Mental Health, National Institutes of Health, USA awarded to JL and MLW.
Author information
Authors and Affiliations
Contributions
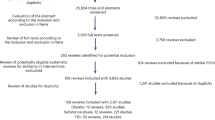
JL: contributed the manuscript writing, original draft, revision, and created and prepared Fig. 1; AWL: contributed the manuscript writing and original draft, JVB: contributed the manuscript writing and original draft; LR: contributed the manuscript writing and original draft; PWG: contributed the manuscript writing and original draft; SRB: contributed the manuscript writing and original draft, and Ma-Li Wong: contributed the manuscript writing, original draft, and revision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Licinio, J., Licinio, A.W., Busnello, J.V. et al. The emergence of chronic diseases of adulthood and middle age in the young: the COIDS (chronic inflammation, obesity, insulin resistance/type 2 diabetes, and depressive syndromes) noxious quartet of pro-inflammatory stress outcomes. Mol Psychiatry 30, 3348–3356 (2025). https://doi.org/10.1038/s41380-025-03034-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41380-025-03034-9
This article is cited by
-
Anxiety and sleep hygiene among college students, a moderated mediating model
BMC Public Health (2025)