Abstract
Preclinical evidence points to disturbances in neural networks in psychosis involving interrelations between dopaminergic-, GABAergic- and glutamatergic neurotransmitter systems. In support, we have previously shown that aberrant interrelations between these neurotransmitters, in contrast to individual transmitter systems, can separate antipsychotic-naïve first-episode psychotic patients (AN-FEP) from healthy controls (HC). Here, we characterized neurotransmitter interrelations, examined their association with treatment response, and explored the effect of treatment on the interrelations. Sixty participants (29 AN-FEP and 31 HC) underwent dynamic [18F]-DOPA PET with arterial blood sampling to measure dopamine synthesis (DS) (k3) in nucleus accumbens (NAcc) and magnetic resonance spectroscopy (MRS) to estimate levels of glutamate (Glu) in anterior cingulate cortex (ACC) and thalamus, and gamma-aminobutyric-acid (GABA) in ACC. A subgroup of the patients was re-scanned after six weeks antipsychotic monotherapy with aripiprazole (PET: 10 AN-FEP; MRS: 27 AN-FEP; 30 HC). Psychopathology was assessed at both visits. Multiple linear regression models and linear mixed models were used to analyze data. We found a negative association between k3 (dependent variable) and GABA in HC (β = −0.15, p = 0.03) and a positive association in patients (β = 0.15, p = 0.04). The aberrant relationship between k3 and GABA was driven by the group-GABA interaction (p = 0.002) and related to treatment response (p = 0.02). No significant group interactions were found for the interrelations between k3 and Glu, but a positive association was found between k3 and Glu in thalamus (p = 0.04) in both groups and the association decreased after treatment in AN-FEP (p = 0.01). The data show that DS in NAcc and GABA levels in ACC are inversely interrelated in AN-FEP, and that the degree of abnormality predicts treatment effect. Moreover, antipsychotic treatment alters the relationship between dopaminergic activity in NAcc and Glu levels in thalamus. The findings suggest that combined instead of single neurotransmitter disturbances should be considered when novel therapeutics are developed for schizophrenia. Clinical trial registration: The Pan European Collaboration on Antipsychotic Naïve Schizophrenia II (PECANSII) study, ClinicalTrials.gov Identifier: NCT02339844. https://www.clinicaltrials.gov/study/NCT02339844.
Similar content being viewed by others
Introduction
Aberrations in the interactions and connections (hereafter interrelations) between dopaminergic-, gamma-aminobutyric acid (GABA)- and glutamatergic neurotransmitter systems in the cortico-striato-thalamo-cortical macro-circuits have for decades been suggested to be involved in the development of psychosis as well as the effect of treatment [1,2,3,4,5,6]. While these interrelations are well described in preclinical literature [7,8,9,10], they are sparsely studied in clinical studies that primarily have reported on abnormalities of single neurotransmitters [5, 6]. Overall, the findings do not support altered post- or presynaptic dopamine activities in antipsychotic-naïve first-episode psychotic patients (AN-FEP) [11,12,13,14,15], whereas increased activity is seen in medicated or chronic patients [16,17,18,19]. For GABA levels in anterior cingulate cortex and nearby areas (ACC hereinafter), levels appear decreased at illness onset but seem to normalize in the chronic stage [20,21,22,23]. Glutamate (Glu) levels in ACC seem to be decreased in first-episode patients, whereas subcortical Glu levels in striatum and thalamus appear to be increased [6, 21,22,23,24,25,26]. Combined, these results suggest an abnormal relationship between neurotransmitters in the cortico-striato-thalamo-cortical macro-circuits in patients with psychosis, presumably due to decreased prefrontal glutamatergic and GABAergic regulation of striatal and thalamic activity. Still, clinical studies of combined neurotransmitter disturbances are needed before conclusions can be drawn. So far, only two studies investigated the combined relationships between striatal activity and ACC Glu levels in FEP [15] and healthy control subjects (HC) [27], respectively. The first study reported a negative association between ACC Glu levels and striatal dopamine synthesis capacity (DSC) in first-episode patients that was not present in HC [15], whereas the other study found a negative association between prefrontal Glu levels and striatal DSC in HC [27]. To date, only one study has reported on ACC GABA levels in first-episode psychosis patients and striatal perfusion as a proxy-measure of dopaminergic activity [20]. In that study, we found that higher levels of the inhibitory neurotransmitter GABA were related to lower striatal perfusion in both AN-FEP and HC [20]. However, more direct measures are needed to reveal abnormalities between prefrontal GABA levels and striatal dopaminergic activity in AN-FEP, and to our knowledge, such studies have not been published this far.
To address the impact of multiple neurotransmitter measures on the schizophrenia pathology, we recently tested if the combination of presynaptic striatal dopamine activity, levels of Glu and GABA in ACC, and levels of Glu in left thalamus could separate AN-FEP from matched HC [28]. In line with the literature, patient status could not be predicted based on individual neurotransmitters, whereas a combination of dopamine activity in nucleus accumbens (NAcc), ACC GABA levels, and thalamic Glu levels separated AN-FEP from HC with an accuracy of 83.7% where, especially, the interaction between striatal dopaminergic activity and prefrontal GABA levels contributed to patient identification [28]. Adding thalamic Glu levels increased the accuracy, although thalamic Glu levels in itself did not predict patient status [28]. These findings support that combined measures of dopaminergic activity in striatum, GABA levels in ACC, and Glu levels in thalamus are crucial to the schizophrenia pathophysiology, but it still needs to be investigated how the relationship between dopaminergic activity in NAcc and prefrontal GABA and thalamic Glu levels differs between AN-FEP and HC.
Treatment response to antipsychotics may also depend on combined neurotransmitter disturbances, but up till now, studies have only investigated associations with single neurotransmitter levels. Antipsychotics dampen dopamine activity via dopamine D2 receptors [29]. We have previously in two different AN-FEP cohorts found that treatment effect is related to the availability of frontal and striatal D2 receptors [12, 14, 30], and Jauhar et al reported an association with presynaptic striatal dopamine activity in FEP as well [31]. Recently, in the largest longitudinal positron emission tomography (PET) study of AN-FEP to date, we used arterial blood sampling and a four-parameter (4 P) model to study striatal dopamine synthesis (DS: the decarboxylation rate of [18F]-DOPA to [18F]-dopamine = k3) and DSC (Ki4p) in a novel cohort, and, for comparison, we also assessed Kicer values with the commonly used tissue reference (TR) method [11]. Using the 4 P model, we found highly significant associations between k3 estimates in nucleus accumbens (NAcc) and psychotic symptoms at baseline as well as between k3 and the effect of six weeks of treatment with the partial D2 receptor agonist aripiprazole, whereas no associations were found with the TR-method [11]. This points to k3 estimates as key markers of psychopathology as well as treatment response in psychosis. In an overlapping group of AN-FEP subjects we likewise showed that increased levels of Glu in thalamus and decreased levels of GABA in ACC were related to treatment response with aripiprazole [23]. Other studies reported glutamatergic abnormalities in ACC in first-episode patients with poor treatment response to amisulpride or naturalistic treatment [32, 33], supporting a link between glutamatergic abnormalities and treatment effect of first-line treatment, although the affected region and direction of abnormality differs. However, it has never been possible to separate AN-FEP from HC subjects based on single transmitters, but only by using combined measures of dopaminergic activity in striatum, GABA levels in ACC, and Glu levels in thalamus, where especially the interactions between dopaminergic activity in NAcc and GABA levels in ACC was important [28]. An aberrant interrelation between striatal dopaminergic activity and prefrontal GABA levels may therefore be relevant for treatment response as well. Further, a recent study has suggested that antipsychotic treatment alters the neurotransmitter relationship between striatal DSC and Glu levels in ACC [34]. However, no previous study has investigated whether treatment alters the interrelations between presynaptic striatal dopamine activity and GABA levels in ACC or Glu levels in thalamus.
Our primary aim was to study how the interrelations between striatal DS and cortical GABA levels differ between strict AN-FEP and matched HC. We further explored if combined measures of GABA and Glu levels in ACC and Glu levels in thalamus characterized striatal DS in AN-FEP more accurately than GABA levels alone. Our secondary aim was to investigate if an abnormal relationship between striatal DS and GABA levels in ACC has an impact on treatment effect with a partial dopamine agonist aripiprazole. In explorative analyses we additionally investigated if the interrelations between striatal DS and GABA as well as glutamate levels change after treatment.
We hypothesized inverse interrelations between DS (k3) in NAcc and GABA levels in ACC at baseline associated with the subsequent effect of treatment on psychotic symptoms. In previous studies of individual neurotransmitter levels, neither dopamine activity in NAcc [11] nor Glu levels in ACC [23] changed following treatment with aripiprazole whereas this was the case for thalamic Glu levels [23]; accordingly, we also expect changes in the relation between k3 and thalamic Glu following treatment.
Methods and materials
Participants
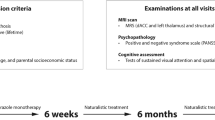
Participants were part of a large multimodal cohort study (PECANS II) approved by the National Committee on Biomedical Research Ethics (H-3-2013-149) previously described [11, 23] and conducted in accordance with the Declaration of Helsinki. Patients were referred from Mental Health Centers in the Capital Region of Denmark and all participants provided written informed content prior to inclusion. Inclusion criteria were: lifetime antipsychotic-naïve; lifetime naïve to central nervous system stimulants, 18-45 years, legally competent, and fulfilling the diagnostic criteria for schizophrenia, schizoaffective disorder, or non-organic psychosis according to the International Classification of Diseases, 10th revision (ICD-10) evaluated by ‘Schedules for Clinical Assessment in Neuropsychiatry’ [35]. We assessed psychopathology with the Positive and Negative Syndrome Scale (PANSS) [36] at baseline and after six weeks of treatment with flexible doses of a partial D2 agonist (aripiprazole). Treatment effect was estimated as change of PANSS positive scores, denoted ∆PANSS, from baseline to six weeks’ follow-up (PANSS positive follow-up - PANSS positive baseline) as previously defined [11]. Hence, a negative ∆PANSS indicates an improvement of positive symptom severity. Medication compliance was assessed by serum concentrations.
We recruited HC matched on age, sex, and parental educational level through online advertisement (www.forsøgsperson.dk).
Exclusion criteria are described previously [11, 23] and in the Supplementary Methods.
Prescribed benzodiazepines were tolerated in patients before initiation of antipsychotic treatment after examinations, although not 12 h before magnetic resonance imaging (MRI) or PET-imaging. Substance use was assessed through self-report and a urine drug test (Rapid Response, Jepsen HealthCare, Tune, Denmark).
[18F]-DOPA PET
DS was assessed with [18F]-DOPA PET imaging with integrated PET-CT (Siemens Biograph m CT64 from 2013). We administered carbidopa 150 mg and entacapone 400 mg orally one hour before PET to minimize [18F]-DOPA metabolic degradation before passage through the blood brain barrier. A low-dose CT-scan was performed before each PET-session to enable attenuation correction. A detailed description of the methodology is provided elsewhere [11].
Magnetic resonance imaging and magnetic resonance spectroscopy
Proton magnetic resonance spectroscopy (1H-MRS) and T1 weighted structural MRI were performed on a 3.0 Tesla scanner (Achieva, Philips Healthcare, Eindhoven, NL) with a 32-channel head coil (Invivo, Orlando, Lorida, USA) as previously described [37]. A T1 weighted structural scan (TR: 10 ms; TE: 4.6 ms; flip angle: 8°; voxel size: 0.79*0.79*0.80mm3) was obtained for co-registration and anatomical reference of the PET images, and segmentation of gray- and white matter in the spectroscopic voxels. We used FreeSurfer [13, 14] version 5.3.0 [38, 39] for individual segmentation in the PET analyses, where nucleus accumbens (NAcc) was the primary region of interest (ROI) based on a significant association between positive symptoms and both k3 and Ki4P in NAcc as well as between k3 in NAcc at baseline and reduction of positive symptoms after six weeks aripiprazole previously found in an overlapping cohort [11].
Point-resolved spectroscopy (PRESS) was used to estimate levels of Glu (TR 3000 ms, TE 30 ms, 128 averages with MOIST water-suppression, 7 min pr. Scan). Spectra were obtained in a 2.0 × 2.0 × 2.0 cm3 voxel in dorsal ACC and a 2.0 × 1.5 × 2.0 cm3 voxel in left thalamus (Supplementary Figure S1B and C) simultaneously with an inbuilt unsuppressed water reference scan. Glu levels were estimated by fitting spectra in the range of 0.2-4.0ppm using LCModel version 6.3-1 L (s-provencher.com/lcmodel.shtml) [40].
Last, Mescher–Garwood point-resolved spectroscopy sequence (MEGAPRESS) was used for acquisitions of GABA levels (TE = 68 ms; TR = 2000ms, 14 ms editing pulses applied at 1.9 and 7.5ppm, 320 averages, MOIST water suppression, and interleaved unsuppressed water reference) [41] in a 3.0 × 3.0 × 3.0 cm3 voxel placed in dorsal ACC (Supplementary Figure S1A). Gannet version 3.1 was used to fit GABA levels quantified as water-scaled values in the spectral range between 2.79 and 3.55ppm [42].
All metabolite levels were calculated in institutional units by correcting for partial volume cerebrospinal fluid as previously described [22]. Minimum reporting standards for MRS [43] including quality data are provided in Supplementary Tables S1, S2, S3, and S4. In ACC, there were small but significant differences in FWHM for PRESS acquisitions, and fit error as well as FWHM for MEGAPRESS acquisitions at baseline (Supplementary Table S3 and S4) but no other significant group differences in data quality parameters.
Statistical analysis
Multiple linear regression using Ordinary Least Squares and linear mixed effects model analyses were performed in Python version 3.12 as implemented in the statsmodels library version 0.14.1. Independent variables were standardized by subtracting the mean and dividing by the standard deviation prior to the analyses to minimize collinearity. Group differences in demographic data were analyzed using Mann-Whitney U test, Fischer´s exact test, and Chi-square tests as appropriate in SAS version 8.4.
No outliers were detected. Adjustment for age in the statistical models described below did not alter findings.
Group differences in neurotransmitter interrelations
Separate multiple linear regression analyses were applied to test the primary hypothesis that the interrelations between DS in NAcc (k3) and ACC GABA levels differed in AN-FEP and matched HC. First, the relationship between k3 in NAcc as dependent variable (y) and GABA in ACC, sex, and GABA*group was tested (Eq. 1).
where \({{{\rm{\beta }}}}_{0}\) is the intercept, \({{{\rm{x}}}}_{1}\) is GABA in ACC, and \({{{\rm{\beta }}}}_{1}-{{{\rm{\beta }}}}_{4}\) are the coefficients of the independent variables. In case of a significant GABA*group interaction, post hoc tests were performed for AN-FEP and HC separately using general linear models.
Second, we examined the additive effect of combinations of neurotransmitters by fitting models including the independent variables group, GABA in ACC, group-GABA interaction, and either Glu in ACC or Glu in thalamus in the same model (Eq. 2).
where \({{{\rm{x}}}}_{1}\) is GABA in ACC and \({{{\rm{x}}}}_{2}\) are either Glu in ACC, or Glu in thalamus.
In exploratory analyses, we tested the relationship between k3 in NAcc and either Glu in thalamus or Glu in ACC in a similar model as Eq. 1.
The relation between treatment response and neurotransmitter interrelations
Separate multiple linear regression analyses tested the second hypothesis that an abnormal relationship between striatal DS and GABA levels in ACC was associated with treatment response. First, the relationship between ∆PANSS positive as the dependent variable (y), and k3, GABA levels, and the k3*GABA interaction as independent variables (\({x}_{1}\) and \({x}_{2}\), and \({x}_{1}* {x}_{2}\)) was examined with adjustment for the covariate sex that previously has been shown to influence the load of positive symptoms [13] (Eq. 3).
where \({{{\rm{\beta }}}}_{0}\) is the intercept, and \({{{\rm{\beta }}}}_{1}-{{{\rm{\beta }}}}_{4}\) are the coefficients of the independent variables. In explorative analyses, similar models were tested by exchanging GABA levels (\({x}_{2}\)) with Glu levels in either thalamus or ACC.
Changes in neurotransmitter interrelations after treatment
In explorative analyses in the patient group, separate linear mixed effects analyses were performed to examine the effects of treatment on the neurotransmitters and the relationship between them. First, we explored whether the association between k3 and either GABA in ACC, Glu in thalamus, or Glu in ACC changed after treatment. In these analyses, k3 was the dependent variable (y). The neurotransmitter of interest (x1), visit (baseline vs follow-up), and the neurotransmitter*visit interaction were included as fixed effects, with a random participant-level effect (Eq. 4). The baseline visit was used as the reference.
where \({{{\rm{\beta }}}}_{0}\) is the intercept, and \({{{\rm{\beta }}}}_{1}-{{{\rm{\beta }}}}_{3}\) are the coefficients of the independent variables. Further, the effect of treatment on each neurotransmitter individually was explored. In these models the neurotransmitter of interest was the dependent variable, visit was a fixed effect, with a random participant-level effect (i.e., x1 = 0 in Eq. 4).
Results
A total of 62 participants (31 patients and 31 HCs) were included. Two patients were excluded due to positive screening for benzodiazepines on neuroimaging days, leaving a study population of 29 patients and 31 HCs as shown in Fig. 1 together with a study flow-chart illustrating usable PET and MRS data.
Table 1 displays demographic and clinical characteristics. As expected, patients were less educated than HCs, and patients were more frequently smokers. Mean doses and plasma concentrations of aripiprazole are listed. Patients were moderately ill, with baseline PANSS total scores on 78. Patients improved on all PANSS items after treatment (Table 1).
Differences in neurotransmitter interrelations between patients and HC at baseline
The results of the multiple linear regression analyses testing the interrelations between DS in NAcc and GABA levels in ACC, as well as Glu levels in ACC or thalamus are provided in Table 2 and described below.
The interrelation between DS in NAcc and GABA levels in ACC
DS was modelled by treating k3 in NAcc as the dependent variable and group, GABA levels, and the group-GABA interaction as independent variables (Table 2, Model 1). This model was significant and driven by the group-GABA interaction (p = 0.002) indicating an inverse relationship between GABA levels and k3 in AN-FEP compared to HC, as hypothesized. Post hoc analyses revealed a positive association between GABA in ACC and dopamine activity in NAcc in patients (p = 0.04, β = 0.15) and a negative association in HC (p = 0.03, β = −0.15) (Fig. 2A).
A An inverse relationship was observed between decarboxylation rate (k3) in nucleus accumbens (NAcc) and GABA levels in anterior cingulate cortex (ACC) in antipsychotic-naïve patients with first-episode psychosis (AN-FEP) (red circles) compared to healthy controls (HC) (blue triangles) (p = 0.002, Table 2, Model 1) due to a positive association in AN-FEP (p = 0.04, β = 0.15) but a negative in HC (p = 0.03, β = −0.15). B A positive association was found between k3 in NAcc and glutamate levels in thalamus in both AN-FEP and HC (p = 0.04, b = 0.04). DS dopamine synthesis, NAcc nucleus accumbens, ACC anterior cingulate cortex, AN-FEP antipsychotic-naïve patients with first-episode psychosis, HC healthy controls, IU Institutional units.
When examining combinations of the independent variables GABA in ACC, Glu in ACC, and Glu in thalamus we found that a combination of GABA in ACC and Glu in thalamus was significantly related to k3 (Table 2, Model 2). The association was driven by the group*GABA interaction (p = 0.007) and not GABA in ACC or Glu in thalamus. Similarly, a combination of GABA in ACC and Glu in ACC revealed a significant association between k3 and the group*GABA interaction (p = 0.003) whereas GABA in ACC and Glu in ACC were insignificant (Table 2, model 3).
The interrelation between DS in NAcc and Glu in either thalamus or ACC
Explorative analyses of the association between k3 and levels of either Glu in thalamus or Glu in ACC revealed a significant positive association between k3 and thalamic glutamate levels that did not differ between AN-FEP and HC (Table 2, model 4 and Fig. 2B), whereas there were no significant associations between k3 and ACC glutamate levels (Table 2, Model 5, Supplementary Figure S2). Sex was included as a covariate but did not contribute to any of the models.
The relation between neurotransmitter interrelations and improvement in positive symptoms
Multiple linear regression models examining the relation between improvement in positive symptoms after six weeks of treatment and striatal DS as well as glutamate and GABA levels are described below and summarized in Supplementary Table S5.
First, we tested the second hypothesis that an abnormal relationship between striatal DS and GABA levels in ACC had an impact on treatment response. Improvement in positive psychotic symptoms was associated with k3 (p = 0.021) and the GABA-k3 interaction (p = 0.023). The GABA-k3 interaction indicated that having either high or low values of both k3 and GABA at baseline were associated with a better treatment response (i.e., negative value of ∆PANSS positive), whereas low GABA and high k3 values, or the opposite, were associated with poor treatment response (Fig. 3A and Supplementary Table S5, Model 6).
The effect of k3 (NAcc) and either GABA levels in ACC (A) or Glu levels in thalamus (B) and their interaction on the treatment response (change in PANSS positive). The colorbars indicate the change in PANSS positive score after treatment, where a positive change indicates worsening symptoms, and a negative change indicates improvement. The white dots illustrate the individual patients. The neurotransmitters are standardized to zero mean and unit variance. A) Illustrates the significant interaction between k3 and GABA in ACC. If both k3 and GABA are either low or high, the patient improves during the six weeks of treatment (dark blue). In contrast, if GABA is high and k3 is low or opposite, the patient has more symptoms after treatment (yellow). B) Illustrates a significant effect of k3 on the treatment response, but no interaction effect between k3 and Glu in thalamus: the treatment response only depends on the value of k3, i.e., the color only changes along the x-axis and not along the y-axis.
When GABA levels were exchanged with Glu levels in thalamus (Supplementary Table S5, Model 7), the overall model was significant, but this was driven by a significant relation between treatment response and k3 (p = 0.008) as well as sex (p = 0.015) (due to better treatment response in male patients), whereas the relation between treatment response and the k3*Glu in thalamus interaction was insignificant, suggesting that Glu in thalamus was not related to treatment response. Similar findings were observed when GABA levels were exchanged with Glu levels in ACC (Supplementary Table S5, Model 8), where the overall model was significant driven by a significant relation between treatment response and k3 (p = 0.015) but not Glu in ACC or the k3*Glu in ACC interaction.
Changes in neurotransmitter interrelations after treatment
At baseline, there was a significant positive association between k3 and Glu in thalamus in the patients (p = 0.002) (as also previously illustrated in Fig. 2B) that decreased over time (p = 0.013) (Fig. 4).
We did not observe significant changes after treatment in the interrelation between k3 and GABA (p = 0.31) or in the interrelation between k3 and Glu levels in ACC (p = 0.73) in the patients (Supplementary Figures S3 and S4).
Discussion
To our knowledge, the present study is the first to characterize the interrelations between DS in NAcc, cortical GABA levels, and cortical and thalamic Glu levels in AN-FEP compared with matched HC and to relate these interrelations to treatment response in the patients. The data confirmed our main hypotheses, i.e., that GABA levels in ACC and DS in NAcc are inversely interrelated in AN-FEP and HC, and that the degree of abnormality is associated with treatment response. In addition, we found a significant positive relationship between Glu levels in thalamus and k3 in both patients and HC. The relationship between Glu levels in thalamus and k3 changed in the patients after treatment but was not associated with treatment response. We found no significant group differences in the interrelations between k3 and Glu levels in ACC nor any changes in the relationship in the patients after treatment.
The finding of an inverse interrelation between striatal dopaminergic and cortical GABAergic activity in AN-FEP and HC support previous data showing that this interrelation is pivotal in the separation of patients from HC [28], and extend these findings by revealing that the abnormality in patients is a positive instead of negative association between ACC GABA levels and striatal dopaminergic activity. Interestingly, dysfunction of cortical GABAergic interneurons has long been hypothesized to be implicated in the development of psychosis [44, 45]. Development of prefrontal cortex in adolescence is assumed to be initiated by maturation of inhibitory GABAergic function [46,47,48,49,50,51] and the meso-cortical dopaminergic system [52, 53]. For schizophrenia, it is suggested that abnormalities in this neurodevelopmental period may contribute to development of psychopathology [52]. In support, preclinical models of schizophrenia report reduced prefrontal GABAergic inhibition of hippocampus, causing hippocampal hyperactivity and increased stimulation of NAcc [54]. In line with this, the present findings show an abnormal relationship between striatal dopaminergic activity and prefrontal GABAergic levels at illness onset in AN-FEP.
The mechanisms underlying the abnormal DS (k3)-GABA interrelation remains to be clarified, but preclinical studies have shown that GABAergic interneurons control the output of glutamatergic pyramidal cells believed to have a downstream effect on among others striatal dopaminergic activity via the direct cortico-striato-thalamo-cortical pathway – or the accelerator pathway – and the indirect so-called brake pathway [2, 55, 56]. According to this model, both increased and decreased cortical glutamatergic activity can increase subcortical dopaminergic activity via the direct, respectively the indirect pathway, and normal information-processing depends on a balance between the two pathways. In line with this, the present data show a negative relationship between GABA levels in ACC and DS in NAcc in HC, supporting the notion that striatal DS is dampened by increased cortical GABA activity in normal conditions, whereas the relationship is abnormal in the AN-FEP.
The inverse relationship between ACC GABA levels and striatal DS is not in line with earlier findings of a negative association between cortical GABAergic levels and striatal perfusion in HC and AN-FEP [20]. However, perfusion reflects activity of other neurotransmitters than dopaminergic [57].
Next, we explored if combined measures of GABA levels in ACC and Glu in thalamus and ACC could characterize the variation in striatal DS in AN-FEP more accurately than GABA levels alone. We found that a combination of GABA in ACC, Glu in thalamus and group*GABA improved accuracy of explaining variation in striatal DS (Table 2, model 2) although it was only the group*GABA interaction that was significantly associated with k3. This extends our previous findings in an overlapping sample showing that AN-FEP could be separated from HC with higher precision when combining measures of striatal DS, GABA in ACC, Glu in thalamus and the GABA*striatal DS interaction, but that only the GABA*striatal DS interaction was a significant predictor of patients status [28]. The findings commonly suggest that the abnormal GABA*striatal DS interaction is central to the schizophrenia pathophysiology.
Although Glu in thalamus did not significantly explain the variance in striatal DS, we found a significant positive association between DS in striatum and thalamic Glu levels that did not differ between AN-FEP and HC (Fig. 2B). This corresponds to a previous study showing a positive association between subcortical DS and Glu levels in HC [27]. The data suggest that subcortical DS and Glu are related, but not disturbed in AN-FEP.
Notably, we did not find a significant negative association between presynaptic striatal dopamine activity and Glu levels in ACC in the antipsychotic-naïve patients with first-episode psychosis (Supplementary Figure S2), nor changes in this relationship after treatment (Supplementary Figure S3 and Table S5, Model 8). This seemingly contrasts earlier findings [15, 34], but the present data do in many ways differ from the data from Jauhar et al. First, all patients in the present study were strictly antipsychotic-naïve and within the schizophrenia spectrum and both medication status and diagnosis might influence neurotransmitter activity. Second, in the present study the patients received six weeks of antipsychotic monotherapy with the partial D2 receptor agonist aripiprazole compared with naturalistic treatment [34]. Third, we placed our ACC voxel more rostral where Glu levels are lower compared to ventral ACC in preclinical and HC studies [32, 58,59,60]. Next, we used arterial blood sampling and a 4 P PET model allowing us to measure the striatal decarboxylation rate of [18F]-DOPA to [18F]-dopamine (k3) in contrast to Jauhar et al. who used the traditional TR method to assess DSC (Ki). We chose k3 as our dependent variable since we have previously found it to be superior to Ki assessed with both the TR and the 4 P method [11]. Finally, we investigated NAcc and not associate striatum [15, 34]. Last, only 21% of the patients in Jauhar et al. [15] were female in contrast to 66% in the present study and ethnic differences were present as well.
In line with our second hypothesis, both the GABA-DS interrelation and DS were predictors for treatment response (Fig. 3 and Supplementary Table S5, Model 6). Regarding the GABA-DS interrelation, the data suggest that the effect on psychotic symptoms is related to either low or high values of both GABA and k3, i.e., the more the interrelation in the patients differ from that seen in HC, the better the response to treatment with the partial D2 receptor agonist, aripiprazole. This may reflect the use of aripiprazole that primarily exert partial agonism when dopamine concentrations are low and dopaminergic antagonism when dopamine activity is high [61]. Furthermore, the findings may reflect that GABA levels assessed with MRS capture overall GABAergic interneuron cell-type function [62] but mainly parvalbumin-expressing interneurons are believed to underlie schizophrenia [54, 63].
We did not, however, see a significant change in the association between k3 and GABA after treatment, but Supplementary Fig. S4 could suggest that this might be due to loss of patients to follow-up. Preclinical studies indicate several regulatory mechanisms between the dopaminergic and GABAergic neurotransmitter systems. For example, dopamine D1 and D2 as well as D4 receptors are present on cortical GABAergic interneurons, and timing, strengths of synaptic input, and firing state of the dopaminergic neurons likewise modulate GABAergic interneurons [3, 4, 64,65,66]. Future research should aim at unravelling these mechanisms further, as this may pave the way for development of novel treatment targeting a disturbed GABA-DS interrelation [67].
In extension of our own earlier findings in an overlapping sample of patients [11], and in line with a previous study [31], we also found that higher DS was associated with greater symptom improvement. We did not, however, find that combined measures of Glu in thalamus and DS or Glu in ACC and DS were associated with treatment response after six weeks (Supplementary Table S5, Model 7 and 8) although previous studies of single neurotransmitters (studied separately) in overlapping cohorts have shown an association between Glu in thalamus in AN-FEP and short-term response as well as between decreased GABA levels in ACC at illness onset and outcome after both short and longer term treatment [20, 23]. These discrepancies in findings may reflect a power issue as the current study-sample was smaller than in the previous studies since DS in striatum is technically more challenging to measure.
Last, we explored if treatment changed the interrelations between striatal DS, GABA and glutamate levels. We found that the interrelation between k3 and thalamic Glu changed after six weeks of treatment with aripiprazole, but the change was not related to treatment response. A change was expected given that we have earlier found that Glu levels in thalamus changes after treatment [23], whereas k3 in NAcc did not [11]. We did not observe significant changes in neither the interrelation between k3 and GABA nor between k3 and Glu in ACC after treatment, which is in line with previous studies of individual neurotransmitter where we neither observed changes in k3, nor in GABA levels in ACC, or Glu in ACC after six weeks treatment [11, 23]. As afore mentioned, loss to follow-up of k3 measures might also explain why no significant changes in the interrelation between k3 in NAcc and GABA levels in ACC were found despite a visual interpretation of a change after treatment (Supplementary Figure S4), whereas this does not seem to be the case for the negative findings regarding changes in the interrelation between k3 in NAcc and Glu levels in ACC (Supplementary Figure S3). The findings may suggest that short-term treatment primarily affect glutamate in subcortical regions, whereas cortical regions may be more affected after longer-term treatment [20].
Three major strengths of the current study are inclusion of strictly antipsychotic-naïve patients, measures of striatal DS using an arterial input function thereby allowing us to measure the decarboxylation rate of [18F]-DOPA to [18F]-dopamine (k3), and the combined measures of both striatal DS, GABA as well as glutamate levels. Moreover, AN-FEP were free from substance abuse and acute effects of benzodiazepines, carefully matched to HC, and studied in a longitudinal design. However, limitations should also be addressed. First, MRS measures of Glu and GABA cannot differentiate between extracellular and intracellular GABA and Glu concentrations. Moreover, the sample size for k3 at follow-up is limited given the technical challenges with striatal DS measures.
Conclusion and future directions
The present study characterizes as the first aberrant interrelations between DS in NAcc and GABA levels in ACC in AN-FEP that predict the effect of subsequent antipsychotic treatment. We additionally found identical significant interrelations between DS in NAcc and Glu levels in thalamus in patients and HC. The interrelation between k3 and thalamic Glu levels changed over time in the patients but was not associated with treatment response. The pathophysiological mechanisms behind the observed, clinically relevant, abnormalities in the interrelations between cortical GABAergic and subcortical dopaminergic activity, as well as their implications for future treatment strategies, should be further studied in future longitudinal studies on AN-FEP involving additional modalities such as cognitive functions, early information processing, functional and structural connectivity and brain structure as well as other neurochemical measures, e.g. neuromelanin MRS and/or PET including serotonin 2 A and/or dopamine D2/3 receptor ligands or new radioligands for glutamate and GABA receptors. Moreover, future longitudinal studies on AN-FEP followed up after several years could clarify if the abnormal GABA-DS interrelation at illness onset also impact long-term and not only short-term outcome.
Data availability
Analyzes of the data in the present paper are ongoing as part of other projects, and data are therefore not shared public yet. However, the data may be shared in collaborative project on reasonable request to the corresponding author: Kirsten.borup.bojesen@regionh.dk.
References
Carlsson A. The current status of the dopamine hypothesis of schizophrenia. Neuropsychopharmacology. 1988;1:179–86.
Carlsson A. The neurochemical circuitry of schizophrenia. Pharmacopsychiatry. 2006;39:S10–4.
Glenthoj B, Mogensen J, Laursen H, Holm S, Hemmingsen R. Electrical sensitization of the meso-limbic dopaminergic system in rats: a pathogenetic model for schizophrenia. Brain Res. 1993;619:39–54.
Glenthoj BY, Mogensen J, Laursen H, Hemmingsen R. Dopaminergic sensitization of rats with and without early prefrontal lesions: implications for the pathogenesis of schizophrenia. Int J Neuropsychopharmacol. 1999;2:271–81.
Jauhar S, Johnstone M, McKenna PJ. Schizophrenia. Lancet. 2022;399:473–86.
Howes OD, Bukala BR, Beck K. Schizophrenia: from neurochemistry to circuits, symptoms and treatments. Nat. Rev. Neurol. 2024;20:22–35.
Kiemes A, Gomes FV, Cash D, Uliana DL, Simmons C, Singh N, et al. GABA(A) and NMDA receptor density alterations and their behavioral correlates in the gestational methylazoxymethanol acetate model for schizophrenia. Neuropsychopharmacology. 2022;47:687–95.
Sesack SR, Carr DB, Omelchenko N, Pinto A. Anatomical substrates for glutamate-dopamine interactions: evidence for specificity of connections and extrasynaptic actions. Ann N Y Acad Sci. 2003;1003:36–52.
Povysheva NV, Gonzalez-Burgos G, Zaitsev AV, Kroner S, Barrionuevo G, Lewis DA, et al. Properties of excitatory synaptic responses in fast-spiking interneurons and pyramidal cells from monkey and rat prefrontal cortex. Cereb Cortex. 2006;16:541–52.
Matsumoto M, Togashi H, Kaku A, Kanno M, Tahara K, Yoshioka M. Cortical GABAergic regulation of dopaminergic responses to psychological stress in the rat dorsolateral striatum. Synapse. 2005;56:117–21.
Sigvard AK, Nielsen MO, Gjedde A, Bojesen KB, Fuglo D, Tangmose K, et al. Dopaminergic activity in antipsychotic-naive patients assessed with positron emission tomography before and after partial dopamine D(2) receptor agonist treatment: association with psychotic symptoms and treatment response. Biol Psychiatry. 2022;91:236–45.
Wulff S, Pinborg LH, Svarer C, Jensen LT, Nielsen MO, Allerup P, et al. Striatal D(2/3) binding potential values in drug-naive first-episode schizophrenia patients correlate with treatment outcome. Schizophr Bull. 2015;41:1143–52.
Glenthoj BY, Mackeprang T, Svarer C, Rasmussen H, Pinborg LH, Friberg L, et al. Frontal dopamine D(2/3) receptor binding in drug-naive first-episode schizophrenic patients correlates with positive psychotic symptoms and gender. Biol Psychiatry. 2006;60:621–9.
Wulff S, Nielsen MO, Rostrup E, Svarer C, Jensen LT, Pinborg L, et al. The relation between dopamine D(2) receptor blockade and the brain reward system: a longitudinal study of first-episode schizophrenia patients. Psychol Med. 2020;50:220–8.
Jauhar S, McCutcheon R, Borgan F, Veronese M, Nour M, Pepper F, et al. The relationship between cortical glutamate and striatal dopamine in first-episode psychosis: a cross-sectional multimodal PET and magnetic resonance spectroscopy imaging study. LanPsy. 2018;5:816–23.
Reith J, Benkelfat C, Sherwin A, Yasuhara Y, Kuwabara H, Andermann F, et al. Elevated dopa decarboxylase activity in living brain of patients with psychosis. PNAS USA. 1994;91:11651–4.
Meyer-Lindenberg A, Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M, et al. Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nat Neurosci. 2002;5:267–71.
McGowan S, Lawrence AD, Sales T, Quested D, Grasby P. Presynaptic dopaminergic dysfunction in schizophrenia: a positron emission tomographic [18F]fluorodopa study. Arch Gen Psychiatry. 2004;61:134–42.
Kumakura Y, Cumming P, Vernaleken I, Buchholz HG, Siessmeier T, Heinz A, et al. Elevated [18F] fluorodopamine turnover in brain of patients with schizophrenia: an [18F] fluorodopa/positron emission tomography study. J Neurosci. 2007;27:8080–7.
Bojesen KB, Rostrup E, Sigvard AK, Mikkelsen M, Edden RAE, Ebdrup BH, et al. The trajectory of prefrontal GABA levels in initially antipsychotic-naive patients with psychosis during two years treatment and associations with striatal cerebral blood flow and outcome. Biol Psychiatry Cogn Neurosci Neuroimaging. 2023;9:703–13.
Nakahara T, Tsugawa S, Noda Y, Ueno F, Honda S, Kinjo M, et al. Glutamatergic and GABAergic metabolite levels in schizophrenia-spectrum disorders: a meta-analysis of 1H-magnetic resonance spectroscopy studies. Mol Psychiatry. 2022;27:744–57.
Bojesen KB, Broberg BV, Fagerlund B, Jessen K, Thomas MB, Sigvard A, et al. Associations between cognitive function and levels of glutamatergic metabolites and gamma-aminobutyric acid in antipsychotic-naive patients with schizophrenia or psychosis. Biol Psychiatry. 2021;89:278–87.
Bojesen KB, Ebdrup BH, Jessen K, Sigvard A, Tangmose K, Edden RAE, et al. Treatment response after 6 and 26 weeks is related to baseline glutamate and GABA levels in antipsychotic-naive patients with psychosis. Psychol Med. 2020;50:2182–93.
Smucny J, Carter CS, Maddock RJ. Medial prefrontal cortex glutamate is reduced in schizophrenia and moderated by measurement quality: a meta-analysis of proton magnetic resonance spectroscopy studies. Biol Psychiatry. 2021;90:643–51.
Merritt K, McCutcheon RA, Aleman A, Ashley S, Beck K, Block W, et al. Variability and magnitude of brain glutamate levels in schizophrenia: a meta and mega-analysis. Mol Psychiatry. 2023;28:2039–48.
Merritt K, McGuire PK, Egerton A, Investigators HMiS, Aleman A, Block W, et al. Association of age, antipsychotic medication, and symptom severity in schizophrenia with proton magnetic resonance spectroscopy brain glutamate level: a mega-analysis of individual participant-level data. JAMA Psychiatry. 2021;78:667–81.
Gleich T, Deserno L, Lorenz RC, Boehme R, Pankow A, Buchert R, et al. Prefrontal and striatal glutamate differently relate to striatal dopamine: potential regulatory mechanisms of striatal presynaptic dopamine function? J Neurosci. 2015;35:9615–21.
Sigvard AK, Bojesen KB, Ambrosen KS, Nielsen MO, Gjedde A, Tangmose K, et al. Dopamine synthesis capacity and GABA and glutamate levels separate antipsychotic-naive patients with first-episode psychosis from healthy control subjects in a multimodal prediction model. Biol Psychiatry Glob Open Sci. 2023;3:500–9.
Kapur S, Remington G. Dopamine D(2) receptors and their role in atypical antipsychotic action: still necessary and may even be sufficient. Biol Psychiatry. 2001;50:873–83.
Norbak-Emig H, Ebdrup BH, Fagerlund B, Svarer C, Rasmussen H, Friberg L, et al. Frontal D2/3 receptor availability in schizophrenia patients before and after their first antipsychotic treatment: relation to cognitive functions and psychopathology. Int J Neuropsychopharmacol. 2016;19:pyw006.
Jauhar S, Veronese M, Nour MM, Rogdaki M, Hathway P, Turkheimer FE, et al. Determinants of treatment response in first-episode psychosis: an (18)F-DOPA PET study. Mol Psychiatry. 2019;24:1502–12.
Egerton A, Brugger S, Raffin M, Barker GJ, Lythgoe DJ, McGuire PK, et al. Anterior cingulate glutamate levels related to clinical status following treatment in first-episode schizophrenia. Neuropsychopharmacology. 2012;37:2515–21.
Egerton A, Broberg BV, Van Haren N, Merritt K, Barker GJ, Lythgoe DJ, et al. Response to initial antipsychotic treatment in first episode psychosis is related to anterior cingulate glutamate levels: a multicentre (1)H-MRS study (OPTiMiSE). Mol Psychiatry. 2018;23:2145–55.
Jauhar S, McCutcheon RA, Veronese M, Borgan F, Nour M, Rogdaki M, et al. The relationship between striatal dopamine and anterior cingulate glutamate in first episode psychosis changes with antipsychotic treatment. Transl Psychiatry. 2023;13:184.
Wing JK, Babor T, Brugha T, Burke J, Cooper JE, Giel R, et al. SCAN. schedules for clinical assessment in neuropsychiatry. Arch Gen Psychiatry. 1990;47:589–93.
Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76.
Bojesen KB, Andersen KA, Rasmussen SN, Baandrup L, Madsen LM, Glenthoj BY, et al. Glutamate levels and resting cerebral blood flow in anterior cingulate cortex are associated at rest and immediately following infusion of s-ketamine in healthy volunteers. Front Psychiatry. 2018;9:22.
Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage. 1999;9:179–94.
Fischl B, Sereno MI, Dale AM. Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. Neuroimage. 1999;9:195–207.
Provencher SW. Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med. 1993;30:672–9.
Mescher M, Merkle H, Kirsch J, Garwood M, Gruetter R. Simultaneous in vivo spectral editing and water suppression. NMR Biomed. 1998;11:266–72.
Edden RA, Puts NA, Harris AD, Barker PB, Evans CJ. Gannet: a batch-processing tool for the quantitative analysis of gamma-aminobutyric acid-edited MR spectroscopy spectra. J Magn Reson Imaging. 2014;40:1445–52.
Lin A, Andronesi O, Bogner W, Choi IY, Coello E, Cudalbu C, et al. Minimum reporting standards for in vivo magnetic resonance spectroscopy (MRSinMRS): experts’ consensus recommendations. NMR Biomed. 2021;34:e4484.
Benes FM. Berretta S. GABAergic interneurons: implications for understanding schizophrenia and bipolar disorder. Neuropsychopharmacology. 2001;25:1–27.
Lewis DA, Hashimoto T, Volk DW. Cortical inhibitory neurons and schizophrenia. Nat Rev Neurosci. 2005;6:312–24.
Dorrn AL, Yuan K, Barker AJ, Schreiner CE, Froemke RC. Developmental sensory experience balances cortical excitation and inhibition. Nature. 2010;465:932–6.
Espinosa JS, Stryker MP. Development and plasticity of the primary visual cortex. Neuron. 2012;75:230–49.
Hensch TK, Fagiolini M. Excitatory-inhibitory balance and critical period plasticity in developing visual cortex. Prog Brain Res. 2005;147:115–24.
Long MA, Cruikshank SJ, Jutras MJ, Connors BW. Abrupt maturation of a spike-synchronizing mechanism in neocortex. J Neurosci. 2005;25:7309–16.
Toyoizumi T, Miyamoto H, Yazaki-Sugiyama Y, Atapour N, Hensch TK, Miller KD. A theory of the transition to critical period plasticity: inhibition selectively suppresses spontaneous activity. Neuron. 2013;80:51–63.
Zhang Z, Jiao YY, Sun QQ. Developmental maturation of excitation and inhibition balance in principal neurons across four layers of somatosensory cortex. Neuroscience. 2011;174:10–25.
Larsen B, Luna B. Adolescence as a neurobiological critical period for the development of higher-order cognition. Neurosci Biobehav Rev. 2018;94:179–95.
Islam KUS, Blaess S. The impact of the mesoprefrontal dopaminergic system on the maturation of interneurons in the murine prefrontal cortex. Front Neurosci. 2024;18:1403402.
Gee A, Dazzan P, Grace AA, Modinos G. Corticolimbic circuitry as a druggable target in schizophrenia spectrum disorders: a narrative review. Transl Psychiatry. 2025;15:21.
Carlsson A, Waters N, Carlsson ML. Neurotransmitter interactions in schizophrenia-therapeutic implications. Eur Arch Psychiatry Clin Neurosci. 1999;249:37–43.
Dandash O, Pantelis C, Fornito A. Dopamine, fronto-striato-thalamic circuits and risk for psychosis. Schizophr Res. 2017;180:48–57.
Attwell D, Buchan AM, Charpak S, Lauritzen M, Macvicar BA, Newman EA. Glial and neuronal control of brain blood flow. Nature. 2010;468:232–43.
Dou W, Palomero-Gallagher N, van Tol MJ, Kaufmann J, Zhong K, Bernstein HG, et al. Systematic regional variations of GABA, glutamine, and glutamate concentrations follow receptor fingerprints of human cingulate cortex. J Neurosci. 2013;33:12698–704.
Palomero-Gallagher N, Vogt BA, Schleicher A, Mayberg HS, Zilles K. Receptor architecture of human cingulate cortex: evaluation of the four-region neurobiological model. Hum Brain Mapp. 2009;30:2336–55.
Theberge J, Bartha R, Drost DJ, Menon RS, Malla A, Takhar J, et al. Glutamate and glutamine measured with 4.0 T proton MRS in never-treated patients with schizophrenia and healthy volunteers. Am J Psychiatry. 2002;159:1944–6.
de Bartolomeis A, Tomasetti C, Iasevoli F. Update on the mechanism of action of aripiprazole: translational insights into antipsychotic strategies beyond dopamine receptor antagonism. CNS Drugs. 2015;29:773–99.
Takado Y, Takuwa H, Sampei K, Urushihata T, Takahashi M, Shimojo M, et al. MRS-measured glutamate versus GABA reflects excitatory versus inhibitory neural activities in awake mice. J Cereb Blood Flow Metab. 2022;42:197–212.
Knight S, McCutcheon R, Dwir D, Grace AA, O’Daly O, McGuire P, et al. Hippocampal circuit dysfunction in psychosis. Transl Psychiatry. 2022;12:344.
Laruelle M, Kegeles LS, Abi-Dargham A. Glutamate, dopamine, and schizophrenia: from pathophysiology to treatment. Ann N Y Acad Sci. 2003;1003:138–58.
Yang CR, Seamans JK, Gorelova N. Developing a neuronal model for the pathophysiology of schizophrenia based on the nature of electrophysiological actions of dopamine in the prefrontal cortex. Neuropsychopharmacology. 1999;21:161–94.
Grace AA. Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience. 1991;41:1–24.
Uliana DL, Lisboa JRF, Gomes FV, Grace AA. The excitatory-inhibitory balance as a target for the development of novel drugs to treat schizophrenia. Biochem Pharmacol. 2024;228:116298.
Acknowledgements
This study was funded by an independent grant from the Lundbeck Foundation (R155-2013-16337) to the Lundbeck Foundation Centre of Excellence for Clinical Intervention and Neuropsychiatric Schizophrenia Research (CINS) (Glenthøj), grants from the Wørzner and Gerhard Linds Foundations and support from the Mental Health Services, Capital Region of Denmark (Glenthøj and Ebdrup). PhD grants and a post doc grant were obtained from the Mental Health Services in the Capital Region of Denmark (Sigvard), the Faculty of Health and Medical Sciences, University of Copenhagen (Bojesen), the research Fund 2022 in the Capital Region of Denmark (Bojesen), and an independent grant from the Lundbeck Foundation (R403-2022-1361). The funding sources had no role in the design or conduction of the study design, nor in the collection, analyses, and interpretation of data, or in the writing, review approval and submission of the manuscript for publication. We further wish to thank the staff at Center for Neuropsychiatric Schizophrenia Research (CNSR) and the Centre for Clinical Intervention and Neuropsychiatric Schizophrenia Research (CINS), Mental Health Centre Glostrup, University of Copenhagen; the PET Centre, Herlev Hospital, University of Copenhagen and Functional Imaging Unit, Rigshospitalet, Glostrup for help.
Funding
Open access funding provided by Copenhagen University.
Author information
Authors and Affiliations
Contributions
KBB and KSA had full access to all data in the present study population and takes responsibility for the integrity of the data and the accuracy of the data analysis. BG, KSA, KBB, ER, and AKS designed and conceptualized the study; BG, AKS, KBB, and BE obtained funding for the study; KBB and AKS acquired the data; LTJ and DF provided technical assistance with the PET scans; BG, ER, BE, MØN, AG, and YK supervised the study; KSA, ER and AKS performed the analyzes; BG, KSA, KBB, and ER interpretated the data; BG, KSA, and KBB drafted the manuscript. All authors revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
Dr. Glenthøj has been the leader of a Lundbeck Foundation Centre of Excellence for Clinical Intervention and Neuropsychiatric Schizophrenia Research (CINS) (January 2009 – December 2021), which was partially financed by an independent grant from the Lundbeck Foundation based on international review and partially financed by the Mental Health Services in the Capital Region of Denmark, the University of Copenhagen, and other foundations. All grants are the property of the Mental Health Services in the Capital Region of Denmark and administrated by them. She has no other conflicts to disclose. Dr. Bojesen received lecture fees from Lundbeck Pharma A/S. Dr. Ebdrup BE is part of the Advisory Board of Boehringer Ingelheim, Lundbeck Pharma A/S; and has received lecture fees from Boehringer Ingelheim, Otsuka Pharma Scandinavia AB, and Lundbeck Pharma A/S. The rest of the authors have no conflicts of interest to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bojesen, K.B., Ambrosen, K.S., Sigvard, A.K. et al. Interrelations between dopaminergic-, gabaergic- and glutamatergic neurotransmitters in antipsychotic-naïve psychosis patients and the association to initial treatment response. Mol Psychiatry (2025). https://doi.org/10.1038/s41380-025-03229-0
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-025-03229-0