Abstract
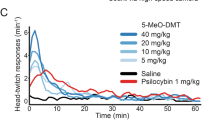
This Phase I clinical trial is the first to rigorously evaluate the safety, tolerability, and pharmacokinetics of a novel sublingual formulation of 5-MeO-DMT, administered at sub-psychedelic doses to adults with moderate to high levels of anxiety and/or depression, without formal psychiatric diagnosis or ongoing treatment. Using a double-blind, placebo-controlled design, participants received a single weekly sublingual dose of 5-MeO-DMT (6 mg, 9 mg, or 12 mg) or placebo over four weeks. The compound was well tolerated across all groups, with no significant adverse events or signs of organ toxicity; mild side effects such as nausea and headache were transient and self-resolving. Pharmacokinetic analyses showed rapid absorption, with peak plasma concentrations occurring within a median of 20 min and no evidence of drug accumulation. Neurophysiological assessments revealed dose-dependent modulation of brain activity without eliciting full psychedelic effects, supporting the feasibility of repeated sub-psychedelic dosing. Participants remained cognitively and behaviorally stable, maintaining their usual daily activities and social interactions. This study marks a pivotal advancement in the clinical exploration of psychedelic compounds, highlighting the potential of 5-MeO-DMT as a safe, fast-acting compound with favorable tolerability and emerging as a promising candidate for future therapeutic applications. These findings provide critical groundwork for future trials targeting psychiatric populations, positioning 5-MeO-DMT as a novel, fast-acting therapeutic strategy with broad clinical relevance.
Trial Registration
ClinicalTrials.gov: NCT06816667
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 13 print issues and online access
$259.00 per year
only $19.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Data will be made available upon request.
References
Nichols DE. Psychedelics. Pharm Rev. 2016;68:264–355.
O’Brien CP Drug use disorders and addiction. In: Hardman JG, Limbird LE, editors. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics. 10th ed. New York: McGraw-Hill; 2001. p. 574–639.
Chi T, Gold JA. A review of emerging therapeutic potential of psychedelic drugs in the treatment of psychiatric illnesses. J Neurol Sci. 2020;411:116715.
Carhart-Harris R, Giribaldi B, Watts R, Baker-Jones M, Murphy-Beiner A, Murphy R, et al. Trial of psilocybin versus escitalopram for depression. N. Engl J Med. 2021;384:1402–11.
Davis AK, So S, Lancelotta R, Barsuglia JP, Griffiths RR. 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) used in a naturalistic group setting is associated with unintended improvements in depression and anxiety. Am J Drug Alcohol Abus. 2019;45:161–9.
Reckweg J, Mason NL, van Leeuwen C, Toennes SW, Terwey TH, Ramaekers JG. a phase 1, dose-ranging study to assess safety and psychoactive effects of a vaporized 5-methoxy-N, N-dimethyltryptamine formulation (GH001) in healthy volunteers. Front Pharm. 2021;12:760671.
Reckweg JT, Uthaug MV, Szabo A, Davis AK, Lancelotta R, Mason NL, et al. The clinical pharmacology and potential therapeutic applications of 5‐methoxy‐N,N‐dimethyltryptamine (5‐MeO‐DMT). J Neurochem. 2022;162:128–46.
Reckweg JT, van Leeuwen CJ, Henquet C, van Amelsvoort T, Theunissen EL, Mason NL, et al. A phase 1/2 trial to assess safety and efficacy of a vaporized 5-methoxy-N,N-dimethyltryptamine formulation (GH001) in patients with treatment-resistant depression. Front Psychiatry. 2023;14:1133414.
Griffiths RR, Johnson MW, Richards WA, Richards BD, McCann U, Jesse R. Psilocybin occasioned mystical-type experiences: Immediate and persisting dose-related effects. Psychopharmacol (Berl). 2011;218:649–65.
Polito V, Stevenson RJ. A systematic study of microdosing psychedelics. PLoS One. 2019;14:e0211023.
Fadiman J, Korb S. Might microdosing psychedelics be safe and beneficial? an initial exploration. J Psychoact Drugs. 2019;51:118–22.
Anderson T, Petranker R, Rosenbaum D, Weissman CR, Dinh-Williams LA, Hui K, et al. Microdosing psychedelics: personality, mental health, and creativity differences in microdosers. Psychopharmacol (Berl). 2019;236:731–40.
Sherwood AM, Claveau R, Lancelotta R, Kaylo KW, Lenoch K. Synthesis and characterization of 5-MeO-DMT succinate for clinical use. ACS Omega. 2020;5:32067–75.
Shen HW, Jiang XL, C. Winter J, Yu AM. Psychedelic 5-methoxy-N,N-dimethyltryptamine: metabolism, pharmacokinetics, drug interactions, and pharmacological actions. Curr Drug Metab. 2011;11:659–66.
Uthaug MV, Lancelotta R, Ortiz Bernal AM, Davis AK, Ramaekers JG. A comparison of reactivation experiences following vaporization and intramuscular injection (IM) of synthetic 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting. J Psychedelic Stud. 2020;4:104–13.
Uthaug MV, Lancelotta R, van Oorsouw K, Kuypers KPC, Mason N, Rak J, et al. A single inhalation of vapor from dried toad secretion containing 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting is related to sustained enhancement of satisfaction with life, mindfulness-related capacities, and a decrement of psyc. Psychopharmacol (Berl). 2019;236:2653–66.
Yoon J, Sharma V, Harada A. Safety, tolerability, and pharmacokinetics of oral BI 1358894 in Healthy Japanese Male Volunteers. Clin Drug Investig. 2024;44:319–28.
Straumann I, Ley L, Holze F, Becker AM, Klaiber A, Wey K, et al. Acute effects of MDMA and LSD co-administration in a double-blind placebo-controlled study in healthy participants. Neuropsychopharmacology. 2023;48:1840–8.
Saeger HN, Olson DE. Psychedelic-inspired approaches for treating neurodegenerative disorders. J Neurochem. 2022;162:109–27.
Mastinu A, Anyanwu M, Carone M, Abate G, Bonini SA, Peron G, et al. The bright side of psychedelics: latest advances and challenges in neuropharmacology. Int J Mol Sci. 2023;24:1329.
Cavanna, Muller F, de la Fuente LA S, Zamberlan F, Palmucci M, Janeckova L, et al. Microdosing with psilocybin mushrooms: a double-blind placebo-controlled study. Transl Psychiatry. 2022;12:1–11.
Aaronson ST, Van Der Vaart A, Miller T, Lapratt J, Swartz K, Shoultz A, et al. Single-dose synthetic psilocybin with psychotherapy for treatment-resistant bipolar type II major depressive episodes: a nonrandomized controlled trial. JAMA Psychiatry. 2024;21204:1–8.
Ley L, Holze F, Arikci D, Becker AM, Straumann I, Klaiber A, et al. Comparative acute effects of mescaline, lysergic acid diethylamide, and psilocybin in a randomized, double-blind, placebo-controlled cross-over study in healthy participants. Neuropsychopharmacology. 2023;48:1659–67.
James E, Erritzoe D, Benway T, Joel Z, Timmermann C, Good M, et al. Safety, tolerability, pharmacodynamic and wellbeing effects of SPL026 (dimethyltryptamine fumarate) in healthy participants: a randomized, placebo-controlled phase 1 trial. Front Psychiatry. 2023;14:1–14.
Lancelotta RL, Davis AK. Use of Benefit Enhancement Strategies among 5-Methoxy-N,N-Dimethyltryptamine (5-MeO-DMT) Users: Associations with Mystical, Challenging, and Enduring Effects. J Psychoact Drugs. 2020;52:273–81.
Holze F, Singh N, Liechti ME, D’Souza DC. Serotonergic Psychedelics: A Comparative Review of Efficacy, Safety, Pharmacokinetics, and Binding Profile. Vol. 9, Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. Elsevier Inc.; 2024. p. 472–89.
Holze F, Caluori T, Vizeli P, Liechti M. Safety pharmacology of acute LSD administration in healthy subjects. Psychopharmacology. 2022;239:1893–905.
Introductory Guide for Standardised MedDRA Queries (SMQs) Version 27.0. 2024.001126.
Olabarriet.a LL, Rivera D, Galarza-Del-Angel J, Garza MT, Saracho CP, Rodríguez W, et al. Verbal fluency tests: Normative data for the Latin American Spanish speaking adult population. NeuroRehabilitation. 2015;37:515–61.
Vanotti S, Eizaguirre MB, Cores EV, Yastremis C, Garcea O, Salgado P, et al. Validation of the PASAT in Argentina. Appl Neuropsychol Adult. 2016;23:379–83.
Wechsler D. WISC-V: Technical and interpretive manual. Bloomington, MN: NCS Pearson 2015.
Daly I, Williams D, Hwang F, Kirke A, Miranda ER, Nasuto SJ. Electroencephalography reflects the activity of sub-cortical brain regions during approach-withdrawal behaviour while listening to music. Sci Rep. 2019;9:9415.
Hohaia W, Saurels BW, Johnston A, Yarrow K, Arnold DH. Occipital alpha-band brain waves when the eyes are closed are shaped by ongoing visual processes. Sci Rep. 2022;12:1194.
Hutten NRPW, Mason NL, Dolder PC, Theunissen EL, Holze F, Liechti ME, et al. Low doses of LSD acutely increase BDNF blood plasma levels in healthy volunteers. ACS Pharm Transl Sci. 2021;4:461–6.
McIlhenny EH, Riba J, Barbanoj MJ, Strassman R, Barker SA. Methodology for determining major constituents of ayahuasca and their metabolites in blood. Biomed Chromatogr. 2012;26:301–13.
Good M, Joel Z, Benway T, Routledge C, Timmermann C, Erritzoe D, et al. Pharmacokinetics of N,N-dimethyltryptamine in Humans. Eur J Drug Metab Pharmacokinet. 2023;48:311–27.
Nour MM, Evans L, Nutt D, Carhart-Harris RL. Ego-dissolution and psychedelics: validation of the ego-dissolution inventory (EDI). Front Hum Neurosci. 2016;10:1–13.
Barrett FS, Johnson MW, Griffiths RR. Validation of the revised mystical experience questionnaire with psilocybin. J Psychopharmacol. 2015;29:1182–90.
Barrett FS, Matthew PB, Leoutsakos J-MS. Neuroticism is associated with challenging experiences with psilocybin mushrooms. Pers Individ Dif. 2017;117:155–60.
Rucker JJ, Roberts C, Seynaeve M, Young AH, Suttle B, Yamamoto T, et al. Phase 1, placebo-controlled, single ascending dose trial to evaluate the safety, pharmacokinetics and effect on altered states of consciousness of intranasal BPL-003 (5-methoxy-N,N-dimethyltryptamine benzoate) in healthy participants. J Psychopharmacol. 2024;38:712–23.
Acknowledgements
This work was supported by Biomind Labs Inc.
Author information
Authors and Affiliations
Contributions
MBBM and LN contributed equally to the work. Designed and performed the research; analyzed the data and wrote the manuscript. BD, VL, and MZ. Conducted the neuropsychological and psychiatric tests KD, OJ, and FG performed PK studies; OL, GMA, and DP. Analyzed EEG data; PDD served as the Chief Scientific Officer of Biomind Labs Inc. during the study; SGA was the Medical Director of the clinical trial and MAB. Designed the research; Contributed to data analysis, and reviewed the final version of the manuscript. All authors gave final approval to the manuscript.
Corresponding author
Ethics declarations
Competing interests
During the study, PD-D was the Chief Scientific Officer of Biomind Labs Inc. MB was the Clinical Advisor of Biomind Labs Inc. during the study. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bistue Millón, M.B., Noguera, L., Bruno, D. et al. Safety and tolerability of multiple sublingual microdoses of 5-MeO-DMT in adults with moderate symptoms of depression and/or anxiety: a randomized, double-blind, placebo-controlled study. Neuropsychopharmacol. 50, 1715–1723 (2025). https://doi.org/10.1038/s41386-025-02167-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41386-025-02167-3