Abstract
Head and neck squamous cell carcinoma (HNSCC) remains a prevalent and challenging cancer to treat due to its genetic heterogeneity. Cisplatin resistance is one of important causes in treatment failure of locally advanced HNSCC. ONC201, a selective dopamine receptor D2 antagonist and mitochondrial ClpP agonist, has emerged as a potential antitumor agent in various malignancies. This study explores the therapeutic potential of ONC201, alone and in combination with cisplatin, in both cisplatin-sensitive and -resistant HNSCC cells, with an emphasis on endoplasmic reticulum (ER) stress-mediated apoptosis. A cisplatin-resistant HNSCC subline (OC2-CR1) was developed via long-term drug exposure. The treatment effectiveness of ONC201 alone and cisplatin in combination on cell viability, DNA damage, reactive oxygen species (ROS) production, and stress response markers were evaluated. ONC201 exhibited potent cytotoxicity in both cisplatin-sensitive and -resistant HNSCC cells, retaining efficacy in OC2-CR1 cells. Combined treatment with ONC201 and cisplatin demonstrated synergistic inhibition of proliferation and migration, with enhanced induction of apoptosis. Mechanistically, ONC201 induced ER stress-mediated cell death via ATF4/CHOP signaling in cisplatin-sensitive cells, while ATF3/CHOP predominated in resistant cells. In vivo, combination therapy significantly suppressed tumor growth in xenograft models, including cisplatin-resistant tumors, without inducing toxicity. Immunohistochemical analysis confirmed activation of CHOP in tumor tissues. Furthermore, clinical correlation revealed that low CHOP expression in OSCC patients was associated with increased recurrence risk and inferior recurrence-free survival significantly. This study provides compelling evidence that ONC201 enhances cisplatin efficacy through distinct, stress-mediated apoptotic pathways in HNSCC. The ability of ONC201 to overcome cisplatin resistance and its synergistic antitumor effects highlight its promise as a candidate for combination therapy. These findings support the translational potential of targeting the ATF3/ATF4/CHOP axis to improve outcomes in patients with cisplatin resistant HNSCC.
Similar content being viewed by others
Introduction
Head and neck squamous cell carcinoma (HNSCC) is one of the most prevalent cancers globally, often associated with risk factors such as tobacco use, betel quid chewing, alcohol consumption, and human papillomavirus (HPV) infection [1,2,3,4]. HNSCC primarily originates from the mucosal epithelium of the upper aerodigestive tract, including the oral cavity, larynx, oropharynx, and hypopharynx. Due to the lack of enhanced public awareness about the hazards from these substances, many patients are still diagnosed at an advanced stage. Current treatment strategies include surgery, radiotherapy, chemotherapy, target therapy, immunotherapy or combination. Despite of the multidisciplinary approach in the care of patients with HNSCC, there are still many patients who would experience the treatment failure. This is largely due to the remarkable heterogeneity of HNSCC, characterized by various genetic mutations and aberrant gene expressions [5, 6]. Consequently, there is a need to develop a novel therapeutic agent that is able to provide more effective in the treatment outcomes. One of the current types of research focuses on advancing targeted therapy that exploit specific molecular pathways critical to cancer growth and survival.
Cisplatin, a platinum-based agent is widely used as the first-line chemotherapy agent for HNSCC because of its potent anticancer activity. The mechanisms of cisplatin in treating HNSCC involve the formation of platinum-DNA adducts, which induce G2/S cell cycle arrest and subsequent cell death by causing DNA damage in rapidly dividing cancer cells [7, 8]. Additionally, cisplatin can trigger cellular stress responses through the activation of ATF3 and ATF4, leading to the inhibition of MCL1 expression and inducing the apoptosis in HNSCC cells [9, 10].
ONC201, a small molecule which has been shown to have anti-tumor efficacy by using a monotherapy or in combination with other treatments [11, 12] in phase II clinical trials for various solid tumors and hematological malignancies. ONC201 which would activate the integrated stress response (ISR), inhibition of AKT/ERK signaling, and induction of ATF3, ATF4, and CHOP is a DRD2 antagonist and ClpP agonist. These pathways converge to activate TRAIL (TNF-related apoptosis-inducing ligand)-mediated apoptosis, particularly in tumor cells that are resistant to conventional therapies.
In HNSCC, ATF3 has been identified as a tumor suppressor that promotes apoptosis and inhibits cell growth, regulating various cellular processes in response to stressors such as DNA damage [13]. ATF4, another stress-responsive transcription factor, plays a role in programmed cell death by regulating downstream targets, including MCL1 [14]. CHOP, also known as GADD153, is a multifunctional transcription factor that is upregulated in response to various stresses, such as DNA damage, ER stress, and mitochondrial dysfunction. CHOP mediates apoptosis by downregulating anti-apoptotic proteins like BCL2, BCL-XL, and MCL-1, and upregulating pro-apoptotic proteins like BIM, BAK, and BAX [15]. It plays a crucial role in coordinating cellular responses to stress, mediating cell fate decisions, including cell survival or programmed cell death [16]. The role of MCL1 in regulating apoptosis makes it a critical factor in determining cancer cell survival and resistance to therapy in HNSCC [17].
Cisplatin is the major backbone of chemotherapy agent for treatment of HNSCC [18] but the genetic heterogeneity and aberrant mutations could lead to primary cisplatin resistance, causing the treatment failure in locally advanced tumor or recurrent ones [19]. The ONC201 is able to induce mitochondria-mediated apoptosis by downregulating MCL1 and this phenomenon suggests its potential as an effective agent to overcome cisplatin resistance. In this study, we explore the synergistic effects of ONC201 and cisplatin in HNSCC models. Our aim is to elucidate the underlying molecular mechanisms and evaluate the therapeutic potential of this combination in overcoming treatment resistance and improving outcomes in HNSCC.
Results
Generation and characterization of cisplatin-resistant HNSCC cells
Cisplatin-resistant HNSCC cells were generated from the OC2 cell line through a progressive selection process involving increasing concentrations of cisplatin (Sigma-Aldrich, UK) over a 6-month period. The selection began with low doses and culminated in continuous exposure to 1 μM cisplatin, resulting into the stable resistant phenotype designated as OC2-CR1 (Fig. 1A). To assess cisplatin sensitivity, OC2 and OC2-CR1 cells were treated with a range of cisplatin concentrations for 24 and 48 h, and cell viability was evaluated by using the WST1 assay (Fig. 1B). OC2 cells displayed sensitivity to cisplatin, while OC2-CR1 cells exhibited marked resistance. At 48 h, the IC50 values were 2 μM for OC2 cells and 9 μM for OC2-CR1 cells, confirming the significant resistance of OC2-CR1 cells compared to the parental OC2 cells.
A Schematic timeline illustrating the establishment of cisplatin-resistant HNSCC cell line OC2-CR1. B Cell viability of OC2 and OC2-CR1 cells treated with cisplatin at concentrations ranging from 1 to 20 μM for 24 h or 48 h, determined by WST-1 assay. Data represent the mean ± SD from six independent experiments. C Western blot analysis of γH2AX and cleaved PARP levels in OC2 and OC2-CR1 cells following cisplatin treatment for 4, 24, 36, and 48 h. Densitometric analysis results are shown as histograms. β-actin was used as a loading control. Quantitative data are presented as the mean ± SEM of three independent experiments. *p < 0.05.
To further compare cisplatin and ONC201 sensitivity, IC50 values for FaDu, Detroit 562, and CAL 27 were determined alongside OC2 and OC2-CR1 cells (Fig. S1). Among these, CAL 27 (CRL-2095™) cells also demonstrated inherent resistance to cisplatin. WST-1 assay results showed IC50 values of 4 μM, 8.7 μM, and 5.1 μM,for FaDu, Detroit 562, and CAL 27, respectively. In comparison, OC2 and OC2-CR1 exhibited IC50 values of 2 μM and 13.1 μM, respectively, reinforcing the cisplatin-sensitive versus-resistant profiles of these two lines.
During ONC201 testing, it was noted that the compound interfered with the WST-1 assay, leading to overestimation of viability and discrepancies with actual cell counts. To overcome this, ONC201 IC50 values were determined using viability and cytotoxicity assays based on automated cell counting. After 72 h of treatment, IC50 values were 4.4 μM (OC2), 4.3 μM (OC2-CR1), and 4.0 μM, (CAL 27), while FaDu and Detroit 562 cells showed markedly reduced sensitivity, with IC50 values of 19 μM and > 20 μM, respectively.
Interestingly, ONC201 retained its cytotoxic efficacy in cisplatin-resistant cells, suggesting that resistance to cisplatin did not confer cross-resistance to ONC201. Notably, a combinatorial effect was observed in OC2 and OC2-CR1 cells when treated with both ONC201 and cisplatin, suggesting a potential synergistic interaction.
To further investigate the molecular response to cisplatin, Western blot analysis was performed to assess DNA damage and apoptosis markers, including γH2AX and cleaved Poly (ADP-ribose) polymerase (PARP) (Fig. 1C). In OC2 cells, cisplatin induced a dose-dependent increase in both γH2AX and cleaved PARP, indicating enhanced DNA damage and apoptotic activity. Conversely, OC2-CR1 cells exhibited only modest increases in these markers, reflecting an impaired response to cisplatin-induced cytotoxicity.
ONC201 and cisplatin induced mtROS production in HNSCC cells
Excess cellular levels of reactive oxygen species (ROS) cause damage to intracellular lipids, proteins, nucleic acids and organelles, leading to cell death and damaged biological molecules via the endoplasmic reticulum (ER) stress-mediated pathway [20, 21]. To investigate the role of oxidative stress in the anti-tumor effects of cisplatin and ONC201, mitochondrial ROS levels were assessed using confocal microscopy and flow cytometry. Cells were treated with ONC201, cisplatin, or their combination for 24 and 48 h, followed by staining with MitoSOX™ Red to detect mitochondrial ROS. Fluorescence intensity was quantified to evaluate ROS levels (Fig. 2A). Flow cytometric analysis was further performed using MitoSOX Red and dihydroethidium (DHE) probes to measure mitochondrial and intracellular ROS, respectively, at 24-, 48-, and 72- h post-treatment (Figs. 2B, 2C, and Fig. S2).
A Mitochondrial ROS levels in OC2 and OC2-CR1 cells after 24 h and 48 h treatment with ONC201, cisplatin, or their combination, determined by confocal microscopy. Cells were stained with MitoSOX™ Red (5 μM) for 30 min at 37 °C. Images were acquired at ×400 magnification. Quantitative analysis of fluorescence intensity is presented as histograms. Data are shown as the mean ± SEM from three independent experiments. *p < 0.05. Flow cytometry analysis of ROS levels: B mitochondrial ROS and C intracellular ROS after treatment with ONC201, cisplatin, or their combination for 24 h, 48 h, and 72 h. Cells were stained with 5 μM MitoSOX™ Red (mitochondrial ROS) or 5 μM DHE (intracellular ROS) for 15 min at 37 °C. Histogram data represent the mean ± SEM of six independent experiments. *p < 0.05.
The results revealed that treatment with ONC201 or cisplatin alone, as well as their combination, led to increased mitochondrial ROS generation in OC2 cells at all time points (24, 48, and 72 h). In OC2-CR1 cells, mitochondrial ROS levels were elevated at 48 and 72 h, but not at 24 h, suggesting a delayed oxidative response in the cisplatin-resistant subline. The DHE assay showed a significant increase in intracellular ROS in both OC2 and OC2-CR1 cells following cisplatin treatment for 48 h. Notably, combined treatment with high doses of cisplatin and ONC201 resulted in a marked elevation of intracellular ROS levels in OC2-CR1 cells, but not in OC2 cells, indicating a potentially synergistic oxidative stress response in the resistant phenotype.
Effects of ONC201 and cisplatin on ER stress-mediated cell death in HNSCC cells
Cisplatin and the ERK inhibitor ONC201 are known to induce an ATF-mediated integrated stress response (ISR) that inhibits the growth of various solid tumors. These agents promote cell death by inducing ISR and ER stress-mediated pathways. However, in resistant cancer cells, altered ISR and ER stress can diminish the efficacy of these drugs [22]. To elucidate the mechanisms underlying ER stress-mediated cell death, we examined the expression profiles of ER stress-related markers in parental OC2 and cisplatin-resistant OC2-CR1 cells following treatment with ONC201, cisplatin, or their combination (Fig. 3). Western blot analysis demonstrated that ONC201 markedly upregulated ATF4 and CHOP expression at 24 h in OC2 cells, with a subsequent decline observed at 72 h. Interestingly, ATF3 expression remained low at 24 and 48 h but increased substantially at 72 h post-treatment. In contrast, cisplatin treatment failed to induce ATF4 expression at any time point (24, 48, or 72 h), but robustly upregulated both ATF3 and CHOP expression (Fig. 3A).
Representative Western blot analysis of (A) ATF3, ATF4, CHOP, and (B) γH2AX, cleaved PARP (cPARP), and MCL1 expression levels in OC2 and OC2-CR1 cells after 24 h, 48 h, and 72 h of treatment with ONC201, cisplatin, or their combination. β-actin was used as a loading control. Densitometric analysis results are presented as histograms. Data are expressed as the mean ± SEM from three independent experiments. *p < 0.05.
A similar expression pattern was observed in FaDu cells. ONC201 induced transient ATF4 and CHOP expression, whereas cisplatin selectively induced ATF3 and CHOP, without affecting ATF4 levels (Fig. S3). Notably, CHOP levels remained elevated at all time points (24, 48, and 72 h) compared to control. Combination treatment in both OC2 and FaDu cells resulted in a sustained elevation of ATF3, with CHOP expression peaking at 24 and 48 h and subsequently declining at 72 h. This response appears to be, at least in part, ATF4-dependent. In cisplatin-resistant OC2-CR1 cells, both ONC201 and cisplatin similarly induced ATF3 and CHOP expression at 24 and 48 h, with a notable reduction at 72 h. A comparable pattern was also observed in Detriot 562 cells, indicating a consistent response in cisplatin-resistant cell lines. Collectively, these findings suggest that CHOP expression is regulated through distinct pathways in cisplatin-sensitive and -resistant cells. In OC2 and FaDu cells, CHOP induction appears to occur via both ATF3 and ATF4 pathways, whereas in OC2-CR1 and Detriot 562 cells, CHOP upregulation is predominantly mediated by ATF3 (Fig. 3A, S3).
To further validate these findings, we performed quantitative reverse transcription PCR (RT-qPCR). In OC2 cells, ONC201 significantly increased ATF4 and CHOP transcript levels at 24 h, while cisplatin primarily upregulated ATF3 and CHOP, with only modest effects on ATF4. Combination treatment significantly elevated all three transcripts (ATF3, ATF4, and CHOP). In OC2-CR1 cells, ONC201 significantly induced ATF3, ATF4, and CHOP at 48 h, whereas cisplatin predominantly increased ATF3 and CHOP at 24 and 48 h. Combination treatment further augmented expression of all three markers at both time points. Overall, transcriptional and protein expression patterns were generally consistent, although some time-dependent discrepancies between mRNA and protein levels were observed. Notably, ONC201 induced ATF4 protein only in OC2, not in OC2-CR1 cells (Fig. S4).
We next examined whether these stress responses were linked to cell death. Western blot analysis showed that ONC201 did not induce γH2AX, a marker of DNA damage, but upregulated MCL1 expression at 24 h, followed by decreased MCL1 and cleaved-PARP levels at 48 and 72 h in both cell lines. Cisplatin treatment, in contrast, markedly increased γH2AX and cleaved-PARP levels in a dose-dependent manner while downregulating MCL1 in OC2 cells. A similar trend was observed in OC2-CR1 cells, although the extent of DNA damage and apoptosis was attenuated compared to the parental line. Combined treatment recapitulated the effects of cisplatin at 24 and 48 h, but significantly suppressed MCL1 and cleaved-PARP levels by 72 h (Fig. 3B). These findings suggest that ONC201 and cisplatin induce ER stress–mediated apoptosis through distinct regulatory pathways: via ATF4/CHOP in OC2 cells and via ATF3/CHOP in OC2-CR1 cells, both converging on MCL1 downregulation as a critical determinant of cell death.
ONC201 and cisplatin inhibit cell viability and migration and induce apoptosis in HNSCC cells
To investigate the therapeutic potential of ONC201 and cisplatin in HNSCC, we assessed their short-term effects on cell proliferation, apoptosis, necrosis, and migration across multiple HNSCC cell lines. These in vitro studies aimed to elucidate the cytotoxic mechanisms of each agent and optimize conditions for potential in vivo application [23, 24]. Cell viability assays revealed that both ONC201 and cisplatin independently reduced cell viability in a time- and dose-dependent manner in OC2 cells. Similar inhibitory effects were observed in FaDu, Detroit 562, and CAL27 cells. In the cisplatin-resistant OC2-CR1 cells, cytotoxicity was delayed but became evident after 48 h of treatment. Notably, combination treatment with ONC201 and cisplatin produced a synergistic reduction in viability in all five HNSCC cell lines, with the most pronounced effect observed at 72 h (Fig. 4A and S5).
A Cell viability was assessed by consecutive cell counting over three days. Treatment with ONC201, cisplatin, or their combination significantly reduced cell viability compared to the control group (*p < 0.05 vs. control, #p < 0.05 vs. ONC201 alone, \(\dagger\)p < 0.05 vs. cisplatin alone). B Colony formation assays of OC2 and OC2-CR1 cells treated with various concentrations of cisplatin, ONC201, or their combination for 10 days, stained with crystal violet, and quantified using ImageJ software. Data are presented as the mean ± SEM (n = 6). *p < 0.05 versus control. C Representative images and quantification of cell migration assays. OC2 and OC2-CR1 cells were treated with various concentrations of cisplatin, ONC201, or their combination and assessed using the Oris™ Cell Migration Assay. Real-time migration curves were generated, and data are expressed as the mean ± SEM (n = 6). *p < 0.05. D Apoptosis was analyzed by flow cytometry in OC2 and OC2-CR1 cells treated with ONC201, cisplatin, or the combination for 24, 48, and 72 h. Experiments were performed in triplicate, and data are shown as mean ± SEM. *p < 0.05 vs. control, #p < 0.05 vs. ONC201 alone, \(\dagger\)p < 0.05 vs. cisplatin alone (Student’s t-test).
To evaluate long-term proliferative capacity, colony formation assays were performed in OC2 and OC2-CR1 cells. Both ONC201 and cisplatin significantly suppressed colony formation in a dose-dependent manner over a 9-day period. The combination of 1 µM cisplatin with increasing concentrations of ONC201 (0.25–1 µM) further enhanced this suppressive effect, particularly in OC2 cells, which were more sensitive than the resistant OC2-CR1 cells (Fig. 4B).
Cell migration was assessed using a 2D Oris™ Cell Migration Assay. Treatment with ONC201 (1 µM), cisplatin (10 or 20 µM), or their combination significantly impaired motility in both OC2 and OC2-CR1 cells after 48 h. Combination treatment exerted the strongest inhibitory effect on migration. Interestingly, this suppression was more pronounced in OC2-CR1 cells, indicating a heightened sensitivity of resistant cells to the anti-migratory effects of the drug combination (Fig. 4C).
Apoptosis and necrosis were evaluated using Annexin V/PI staining. Cisplatin induced dose- and time-dependent apoptosis in all cell lines tested. ONC201 primarily induced necrosis in OC2 cells but triggered classic apoptotic features in FaDu, Detroit 562, and CAL27 cells at 72 h. Combination treatment significantly increased apoptotic cell death in OC2, FaDu, Detroit 562, and CAL27 cells, suggesting a synergistic effect. However, in the cisplatin-resistant OC2-CR1 cells, the combination failed to enhance apoptosis beyond the levels induced by individual treatments, indicating an altered cell death response in the resistant phenotype (Fig. 4D and S6).
Together, these findings demonstrate that ONC201 and cisplatin synergistically inhibit cell viability and migration, while promoting apoptosis in HNSCC cells. Although cisplatin-resistant cells retain partial sensitivity to combination treatment with respect to proliferation and migration, they exhibit reduced apoptotic responses, suggesting the involvement of distinct cell death mechanisms in drug resistance. These short-term cellular responses provide critical mechanistic insights into drug action and inform the design of future in vivo efficacy studies.
Significant anti-proliferative effects of cisplatin and ONC201 in an orthotopic graft model of HNSCC
To investigate the long-term antitumor efficacy of cisplatin and ONC201, we employed an in vivo xenograft model using both parental OC2 and cisplatin-resistant OC2-CR1 HNSCC cells. While the direct translation of short-term in vitro responses to long-term in vivo outcomes remains complex due to the influence of pharmacokinetics, tumor microenvironment, and immune modulation [23], it is well established that early cellular stress responses such as apoptotic activation and ER stress can culminate in durable tumor suppression over time. Prior to efficacy studies, the maximum tolerated doses (MTDs) of ONC201 and cisplatin were established in NU/NU and BALB/c mice based on weight monitoring and clinical scoring (activity, appearance, general condition). Intraperitoneal administration of ONC201 (50 mg/kg) and cisplatin (3 mg/kg), twice weekly for four weeks, did not elicit significant toxicity compared to vehicle-treated controls. Hematoxylin and eosin (H&E) staining of liver and kidney tissues revealed no overt histopathological alterations, further supporting the tolerability of the dosing regimen (Fig. S7).
To evaluate therapeutic efficacy, tumor-bearing NU/NU mice were treated with cisplatin (3 mg/kg), ONC201 (50 mg/kg), or a combination of both agents, beginning on day 14 post-inoculation and continuing for 4 weeks (Fig. 5A). In the OC2 xenograft model, both monotherapies significantly suppressed tumor growth compared to vehicle control. Importantly, combination treatment achieved the greatest tumor inhibition without affecting overall body weight, indicating a favorable safety profile (Fig. 5B, C). In contrast, in the OC2-CR1 xenografts, neither cisplatin nor ONC201 alone significantly inhibited tumor growth. Strikingly, only the combination treatment led to a significant reduction in tumor burden in this resistant model, highlighting the potential of ONC201 to overcome cisplatin resistance in vivo.
OC2 or cisplatin-resistant OC2-CR1 cells were subcutaneously implanted into the dorsal flank of athymic nude mice. After 14 days of tumor establishment, mice were randomly assigned to four treatment groups (n ≥ 6 per group): vehicle control, cisplatin (3 mg/kg), ONC201 (50 mg/kg), or the combination of both agents. Treatments were administered intraperitoneally twice weekly for 4 weeks. A Schematic representation of the in vivo treatment schedule (B.I.W. = twice a week). B Body weights of mice in each treatment group over time, shown as mean ± SEM at pre-specified time points. C Tumor photographs and volumes at the study endpoint for each treatment group, presented as mean ± SEM. *p < 0.05. D Immunohistochemical analysis of ATF3, ATF4, and CHOP expression in xenograft tumor tissues harvested from each treatment group. Scale bars = 100 μm (original magnification, ×100). Data are presented as mean ± SEM and analyzed using Student’s t test. *p < 0.05.
To elucidate the underlying mechanisms, immunohistochemical (IHC) analysis was conducted to assess expression of ER stress markers ATF3, ATF4, and CHOP in tumor tissues from each treatment group (Fig. 5D). In OC2-derived tumors, cisplatin and ONC201 both elevated ATF3 expression. However, in OC2-CR1 tumors, ATF3 expression remained low regardless of treatment. ATF4 levels were consistently higher in OC2 tumors compared to OC2-CR1, with minimal treatment-related changes. CHOP expression was significantly upregulated by all treatments cisplatin, ONC201, and the combination in both OC2 and OC2-CR1 tumors relative to untreated controls.
Taken together, these results demonstrate that the combination of ONC201 and cisplatin exerts synergistic antitumor effects in vivo, particularly in cisplatin-resistant HNSCC models. The efficacy appears to be associated with differential modulation of ER stress signaling pathways, supporting the translational relevance of the short-term in vitro findings.
Validation the in vitro and xenograft results from the real-world evidence and survival analyses
To further validate the in vitro and xenograft results, we retrospectively analyzed clinical data from patients diagnosed with first primary oral squamous cell carcinoma (OSCC) who underwent curative surgery followed by cisplatin-based adjuvant concurrent chemoradiotherapy (CCRT) at Kaohsiung Chang Gung Memorial Hospital, Taiwan, between January 2011 and December 2016. The clinicopathological parameters of the entire OSCC cohort who underwent radical surgery followed by adjuvant CCRT are summarized in Table 1. Among the 45 patients included in the study, high expression of ATF3 was observed in 30 patients (66.7%), high expression of ATF4 in 23 patients (51.1%), and high expression of CHOP in 37 patients (82.2%) (Fig. 6).
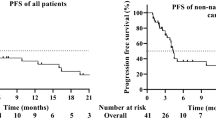
A Representative immunohistochemical images showing low and high expression of ATF3, ATF4, and CHOP in OSCC tissues. Scoring criteria: ATF3 (Low: weak, 5%, IRS < 2; High: strong, 90%, IRS ≥ 2), ATF4 (Low: weak, 5%, IRS < 9; High: strong, 90%, IRS ≥ 9), and CHOP (Low: weak, 5%, IRS < 2; High: strong, 90%, IRS ≥ 2). Scale bar = 100 μm (original magnification ×100). B Correlations between ATF3, ATF4, and CHOP expression levels and recurrence status in OSCC patients. C Kaplan–Meier analysis of 5-year recurrence-free survival based on differential expression of ATF3, ATF4, and CHOP.
Patients were followed for a median of 53.7 months (range: 4.5–106.4 months), during which tumor recurrence occurred in 22 patients (48.9%). Tumor with low CHOP expression were associated with significantly higher odds of recurrence compared to those with high CHOP expression (odds ratio [OR]: 10.267, 95% confidence interval [CI]: 1.143–92.256, p = 0.022). However, this trend was not statistically significant for ATF3 and ATF4 expression levels (ATF3: OR: 1.306, 95% CI: 0.377–4.524, p = 0.673; ATF4: OR: 0.764, 95% CI: 0.237–2.466, p = 0.652). No significant correlations were observed between the expression levels of ATF3, ATF4, or CHOP and other clinicopathological parameters in the cohort. However, a marginally significant association between high CHOP expression and ATF3 expression was observed (p = 0.095) (Table 2).
The 5-year recurrence-free survival (RFS) rate for the entire cohort was 50.9%. To explore the relationship between clinicopathological factors particularly the expression levels of ATF3, ATF4, and CHOP and their potential impact on survival, we performed univariate analysis. The results showed that ATF3, ATF4, and CHOP expression were not significantly associated with 5-year RFS. Survival curves were generated based on varying expression levels of ATF3, ATF4, and CHOP, but no individual factor reached statistical significance in the univariate analysis. Consequently, we included all variables in the multivariate regression analysis. This analysis identified low CHOP expression as an independent negative prognostic factor for RFS (hazard ratio [HR]: 4.922, 95% CI: 1.415–17.123, p = 0.012) (Table 2).
Discussion
The present study provides significant insights into the therapeutic potential of combining ONC201 with cisplatin to overcome the issue of resistance in HNSCC. ONC201, a well-characterized activator of the integrated stress response (ISR), has been shown to upregulate ATF4 and CHOP through ER stress-related kinases, including PERK and GCN2. Additionally, ONC201 promotes apoptosis by activating the TRAIL pathway via upregulation of death receptor 5 (DR5), implicating the involvement of extrinsic apoptotic signaling [25] distinct from cisplatin, which primarily triggers intrinsic apoptosis through mitochondrial damage and DNA lesions. Through comprehensive in vitro and in vivo analyses, we demonstrated that ONC201, a first-in-class imipridone known to activate the ISR can potentially overcome cisplatin resistance by modulating stress-related transcriptional programs, particularly those involving the ATF3/ATF4/CHOP signaling axis (Fig. 7).
The distinct cellular mechanisms of stress response between OC2 and OC2-CR1 cells are highlighted by the differential induction of ATF3, ATF4, and CHOP. In both OC2 and cisplatin-resistant OC2-CR1 cells, cisplatin treatment primarily induced CHOP expression through ATF3. In contrast, ONC201 activated the ISR mainly through early upregulation of ATF4 and CHOP in OC2 cells, followed by an increase in ATF3. However, in OC2-CR1 cells, ONC201-induced CHOP expression was predominantly mediated by ATF3. This differential regulation of CHOP, a key pro-apoptotic factor, indicates that the combination of ONC201 and cisplatin targets multiple pathways to effectively induce apoptosis and overcome the resistance mechanisms in OC2-CR1 cells. Additionally, the combination treatment led to the downregulation of MCL1, an anti-apoptotic protein, in both cell lines, further enhancing cellular sensitivity to apoptosis.
Our results reveal that ONC201 and cisplatin engage distinct but partially overlapping stress response pathways in HNSCC cells. ONC201 predominantly initiates the ISR via early upregulation of ATF4 and CHOP, followed by a delayed increase in ATF3 expression. This temporal transition from adaptive to pro-apoptotic signaling is further characterized by activation of the TRAIL/DR5 pathway and MCL1 downregulation, ultimately promoting apoptosis through both intrinsic and extrinsic pathways. In contrast, cisplatin treatment did not induce ATF4 expression but markedly increased ATF3 and CHOP, suggesting that its stress response is primarily driven by DNA damage and ATF3-mediated mechanisms rather than canonical ER stress pathways.
Although our data primarily focus on the ATF3/ATF4/CHOP signaling axis, it is important to consider the upstream regulators of this pathway. ONC201 has been shown to activate ER stress-related kinases such as PERK and GCN2, both of which can phosphorylate eIF2α and promote ATF4 translation. PERK, in particular, is a canonical ER stress sensor that responds to protein misfolding within the ER lumen, while GCN2 is activated by amino acid deprivation and other metabolic cues [26, 27]. Although we did not directly assess the activation of PERK, GCN2, or eIF2α in this study, the early induction of ATF4 and CHOP in ONC201-treated cells is consistent with activation of these kinases. Further studies exploring the specific contributions of PERK, GCN2, and potentially other ISR-related kinases, such as HRI and PKR, will help delineate the upstream regulatory network driving ONC201-mediated stress responses in HNSCC and their role in overcoming cisplatin resistance.
The development of cisplatin resistance in HNSCC is a great challenge in the treatment of locally advanced tumor or recurrent metastasis tumor and it often leads to therapeutic failure and dismal clinical outcomes [5, 28]. In this study, the cisplatin-resistant OC2-CR1 cells exhibited significantly higher IC50 values compared to the parental OC2 cells, confirming their resistant phenotype (Fig. 1). This marked difference in sensitivity highlights the difficulty in treating cisplatin-resistant HNSCC and address the importance of combination therapies to restore drug sensitivity. While cisplatin alone was able to induce DNA damage and apoptosis, its efficacy was notably reduced in the resistant OC2-CR1 cells, likely due to the upregulation of stress-responsive transcription factors like ATF3 (Fig. 3). Interestingly, in these resistant cells, both ONC201 and cisplatin induced CHOP expression primarily via ATF3, rather than ATF4, indicating a shift in stress response dependency. This aligns with previous studies which had implicated ATF3 in the promotion of cell survival and resistance to radiation therapy [29] or chemotherapy [30] through the induction of anti-apoptotic proteins such as MCL1.
ONC201, known for its role as a DRD2 antagonist and ClpP agonist, has demonstrated potent anti-tumor activity across various cancer types. In this study, ONC201 was shown to significantly sensitize OC2-CR1 cells to cisplatin, primarily by exacerbating oxidative stress and modulating ER stress pathways. The increase in mitochondrial and intracellular ROS levels following treatment with ONC201, particularly when combined with cisplatin, suggests that the generation of oxidative stress is a critical mechanism by which ONC201 enhances the cytotoxic effects of cisplatin. This increase in ROS levels was associated with heightened DNA damage and apoptosis, particularly in the cisplatin-resistant OC2-CR1 cells, thereby highlighting the potential of ONC201 to overcome chemoresistance (Fig. 2).
The differential induction of stress response markers, such as ATF3, ATF4, and CHOP, between OC2 and OC2-CR1 cells demonstrates the distinct cellular mechanisms employed by these cell lines to cope with therapeutic stress (Fig. 6). In both OC2 and cisplatin-resistant OC2-CR1 cells, cisplatin treatment primarily induced CHOP expression through ATF3. However, ONC201 induced CHOP expression primarily through ATF4 in OC2 cells, while in the resistant OC2-CR1 cells, CHOP induction was mediated predominantly by ATF3 (Fig. 3). This differential regulation of CHOP, a key pro-apoptotic factor, suggests that the combination of ONC201 and cisplatin effectively targets multiple pathways to induce apoptosis, thereby overcoming the resistance mechanisms presented in OC2-CR1 cells.
Importantly, the combination of ONC201 and cisplatin produced synergistic effects in both parental and resistant HNSCC cells. This combination led to sustained ATF3 activation, increased DNA damage, suppression of MCL1, and enhanced apoptosis, as shown by elevated cleaved PARP levels. The ability of ONC201 to exacerbate oxidative and ER stress likely amplifies cisplatin-induced cytotoxicity through multiple converging stress pathways. Furthermore, the combination significantly reduced colony formation and cell migration, particularly in OC2-CR1 cells (Fig. 4), suggesting a broader impact on tumorigenic potential and metastatic behavior.
The in vivo xenograft experiments provided strong evidence for the therapeutic potential of the ONC201 and cisplatin combination (Fig. 5). The combined treatment significantly suppressed tumor growth in both OC2 and OC2-CR1 derived xenograft models, demonstrating its efficacy in overcoming resistant mechanisms. Importantly, this treatment regimen did not result in significant weight loss in the mice, showing a less toxicity profile. These results support the therapeutic value of targeting stress response pathways, such as the ATF3/ATF4/CHOP axis, to overcome resistance mechanisms and improve treatment outcomes in HNSCC. Additionally, combination with other therapeutic agents to ONC201 such as chemotherapy agents, check point inhibitors, target therapy agents to treat HNSCC may provide other possible options to improve the clinical outcomes although more studies are necessary to prove this assumption.
In conclusion, this study elucidates the distinct stress response mechanisms activated by ONC201 and cisplatin and reveals how ONC201 enhances cisplatin sensitivity through both ISR- and ATF3-mediated pathways. The differential responses between OC2 and OC2-CR1 cells demonstrate the importance of targeting multiple pathways to effectively treat against the resistant cancer phenotypes. The therapeutic value of combining ONC201 with cisplatin shows its ability to target multiple resistant mechanisms simultaneously. By inducing oxidative stress, modulating ER stress pathways, and promoting apoptosis through different molecular routes, this combination addresses the genetic heterogeneity and adaptive responses of HNSCC cells. This multi-faceted approach is helpful and promising in coping with the complexity of cancer resistance from cisplatin and improving the clinical outcomes in HNSCC.
Materials/subjects and methods
Induction of cisplatin resistance in OC2 cells and cell culture
Cisplatin-resistant OC2 cells (designated OC2-CR1) were established by exposing the parental OC2 cell line to progressively increasing concentrations of cisplatin (Sigma-Aldrich, UK) over a 6-month period. The selection process began with a low dose and culminated in continuous exposure to 1 μM cisplatin, resulting in the stable resistant phenotype. To validate resistance, IC50 values were determined by measuring the cells’ response to cisplatin. Both OC2 and OC2-CR1 cells were maintained in RPMI 1640 medium (Invitrogen), supplemented with 10% fetal bovine serum (FBS), 100 U/mL penicillin, 100 μg/mL streptomycin, and 250 μg/mL Amphotericin B solution (Invitrogen). Cells were seeded at a density of 5 × 106 cells per 10 cm culture dish and treated with varying concentrations of cisplatin, ONC201 (Selleckchem), or a combination of both. The cells were harvested at specific time points for subsequent in vitro analyses.
Cell viability analysis (WST-1 assay)
OC2 and OC2-CR1 cells were seeded at a density of 104 cells per well in 96-well plates and treated with varying concentrations of cisplatin, ONC201, or their combination for 24 and 48 h. Following the treatment period, 10 μL of WST-1 reagent (4-[3-(4-Iodophenyl)-2-(4-nitrophenyl)-2H-5-tetrazolio]-1, 3-benzene sulfonate) (Roche Diagnostics) was added to each well. The plates were then incubated at 37°C for an additional 1–4 h to allow the formation of formazan dye. Absorbance was measured using a microplate reader, with the test wavelength set to 450 nm and the reference wavelength at 630 nm to correct for any background signal. The absorbance values were used to quantify cell viability, reflecting the metabolic activity of the cells post-treatment.
Detection of mitochondrial and intracellular reactive oxygen species (ROS)
Mitochondrial and intracellular ROS levels in OC2 and OC2-CR1 cells were assessed using MitoSOX™ Red (Invitrogen) and Dihydroethidium (DHE, Merck/Sigma-Aldrich) fluorescent probes, respectively. Cells were first washed twice with PBS to remove any residual media. For mitochondrial ROS detection, cells were incubated with 5 μM MitoSOX™ Red, while intracellular ROS was detected by staining with 5 μM DHE. Both staining procedures were carried out for 15 min at 37 °C. Following the staining, the cells were collected and washed twice with PBS to remove excess dye. The cells were then resuspended in 1 mL of PBS and transferred into flow cytometry tubes. The fluorescence intensity, indicative of ROS levels, was measured using a BD LSRII flow cytometer (BD Biosciences).
Immunofluorescence staining of mitochondrial ROS
Cells cultured on glass slides were washed twice with PBS and then incubated with 5 μM MitoSOX™ Red (Invitrogen) for 30 min at 37 °C to detect mitochondrial ROS. After incubation, the slides were fixed using an appropriate fixative (4% paraformaldehyde) and blocked to minimize non-specific binding. The slides were then co-stained with DAPI (4′, 6-diamidino-2-phenylindole; Molecular Probes) to visualize the nuclei. Following staining, the slides were mounted using a fluorescent mounting medium (Dako Cytomation) and sealed with coverslips. Images were captured using an Olympus FluoView® confocal microscope, ensuring that exposure gains and rates were consistent across all samples to allow for accurate comparison. Fluorescence intensities were quantified separately for each color channel.
Western blot analysis
OC2 and OC2-CR1 cells were lysed in PRO-PREP protein extraction solution (iNtRON Bio) for 30 min on ice. The lysates were centrifuged at 13,000 rpm for 5 min at 4 °C, and the resulting supernatants were collected. Protein concentrations were determined using the Bio-Rad protein assay kit (Bio-Rad). Equal amounts of protein (20-50 μg) from each sample were mixed with loading buffer, boiled for 10 min, and then separated by SDS-PAGE on a 10% polyacrylamide gel. The proteins were transferred onto nitrocellulose membranes. Following transfer, the membranes were blocked in 5% non-fat milk or BSA in TBST (Tris-buffered saline with 0.1% Tween-20) for 1 h at room temperature. The membranes were then incubated overnight at 4°C with primary antibodies against ATF3 (Cell Signaling Technology, #33593), γ-H2AX (Abcam, ab11174), ATF4 (Cell Signaling Technology, #11815), CHOP (Cell Signaling Technology, #2895), c-PARP (Cell Signaling Technology, #9541), MCL1 (Cell Signaling Technology, #5453), and β-actin (Sigma-Aldrich, A5441) according to the manufacturers’ protocols. After washing, the membranes were incubated with HRP-conjugated secondary antibodies for 1 h at room temperature. Protein bands were visualized using a chemiluminescent substrate (Santa Cruz Biotechnology) and detected by exposure to X-ray film. Densitometric analysis was performed to quantify the intensity of the protein bands relative to β-actin as a loading control.
Real-time quantitative PCR (RT-qPCR)
Total RNA was isolated using the NucleoSpin RNA II kit (Macherey-Nagel, Düren, Germany) according to the manufacturer’s instructions. For cDNA synthesis, 5 μg of total RNA was reverse transcribed using the High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems, Foster City, CA, USA). RT-qPCR was conducted using SYBR Green PCR Master Mix (Applied Biosystems) on a 7500 Fast Real-Time PCR System (Applied Biosystems). All reactions were performed in triplicate. Relative mRNA expression levels of target genes were calculated using the comparative Ct method (ΔΔCt), with GAPDH serving as internal controls. Primer sequences were designed based on cDNA sequences obtained from GenBank and are listed in Fig. S4.
Cell counting
HNSCC cells (1 × 106) were seeded into each well of 6-well plates and incubated for 24 h. The cells were then treated with varying concentrations of cisplatin, ONC201, or a combination of both, and further incubated for 24–72 h. At the indicated time points, both floating and adherent cells were harvested, combined, and resuspended in 1 ml of phosphate-buffered saline (PBS). A 50 μl aliquot of the cell suspension was mixed with 0.4% trypan blue solution (Invitrogen, Carlsbad, CA, USA), and 10 μl of the mixture was loaded onto a Cell Counting Chamber Slide. Total cell number and cell viability were assessed using an automated cell counter (Countess 3 FL, Invitrogen).
Clonogenic assay
OC2 and OC2-CR1 cells were seeded at a density of 200 cells per well in 6-well plates and allowed to adhere for 48 h. The cells were then treated with various concentrations of cisplatin, ONC201, or a combination of both, and cultured for an additional 9 days under standard conditions. After the treatment period, the cells were fixed with 4% paraformaldehyde and stained with 0.5% Crystal Violet for 30 min at room temperature. Excess stain was washed away with distilled water, and the plates were air-dried. Images of the stained colonies were captured using a digital camera. The number of colonies in each plate was counted manually or using imaging software. Relative plating efficiency (RPE) was calculated using the following formula: RPE = [total colonies of three well (test) / total colonies of three well (control)] x 100%. The results were expressed as a percentage of the control, and statistical analysis was performed to compare the clonogenic survival between different treatment groups.
Oris™ cell migration assay
The migration of OC2 and OC2-CR1 cells was assessed using the Oris™ Cell Migration Assembly Kit (Platypus Technologies) following the manufacturer’s protocol. Cells were seeded at a density of 5 × 10^4 cells per well in Oris™ 96-well plates, each equipped with stoppers that create a central cell-free detection zone. The cells were allowed to adhere and grow overnight. After incubation, the Oris™ stoppers were gently removed to initiate the migration process. Tetramethylrhodamine ethyl ester perchlorate (TMRE, Invitrogen) was added to each well to fluorescently label the cells. The plates were then incubated for an additional 48 h to allow for cell migration into the detection zones. At designated time points, the fluorescence intensity in the detection zones, which correlates with cell migration, was measured using a fluorescence plate reader. The fluorescence signals were converted to cell numbers, and the data were used to generate real-time migration curves.
Annexin V/propidium iodide (PI) apoptosis assay
HNSCC cells (1 × 106) were seeded into 6-well plates and incubated for 24 h. Cells were then treated with varying concentrations of cisplatin, ONC201, or a combination of both, and cultured for 3 days. Following treatment, both floating and adherent cells were collected, trypsinized, and washed with PBS. Cells were then stained with Annexin V and propidium iodide (PI) using the Annexin V Apoptosis Detection Kit (BioLegend, San Diego, CA, USA) for 10 min at room temperature in the dark. Stained cells were analyzed using a FACScan flow cytometer (BD LSRII BD Biosciences), and data were processed using BD FACSDiva Software v8.0.2.
Animal care and xenograft model
Male NU/NU nude mice, 6 weeks of age, were obtained from the National Laboratory Animal Center and maintained in a specific pathogen-free (SPF) facility. The mice were provided with irradiated chow and autoclaved reverse-osmosis water ad libitum. All animal procedures were conducted following protocols approved by the Institutional Animal Care and Usage Committee. For tumor inoculation, the mice were anesthetized with Zoletil (15 mg/kg body weight), and 1×10^7 OC2 or OC2-CR1 cells suspended in 0.1 mL of sterile saline were subcutaneously injected into the right flank using a 26-gauge needle. Tumor development was monitored, and visible dorsal tumors were observed approximately 14 days post-injection. Starting from day 14 post-inoculation, the mice were treated with cisplatin (3 mg/kg), ONC201 (50 mg/kg), or a combination of both, administered intraperitoneally twice a week for 4 weeks. Control groups received either saline or vehicle (10% DMSO, 40% PEG, 5% Tween 80, and 45% saline). Tumor growth was measured twice weekly using a caliper, with tumor size calculated as the product of the longest dimension and its perpendicular. Mice were monitored every other day for tumor progression and signs of weight loss. The study was concluded 7 days after the final treatment, and mice were humanely euthanized by CO2 inhalation if they lost more than 25% of their pre-injection body weight.
Hematoxylin and eosin (H&E) staining and immunohistochemistry (IHC)
For H&E staining, paraffin-embedded tissue sections (3 μm thick) were deparaffinized, rehydrated, and stained with hematoxylin to visualize nuclei, followed by eosin staining for the cytoplasm. Slides were then dehydrated through graded ethanol, cleared in xylene, and mounted with coverslips.
For IHC analysis, three cylindrical tumor cores (1.5 mm in diameter) were extracted from each donor block using a tissue microarray workstation (MTA-1; Beecher Instruments, USA). Tissue sections (3 μm thick) were mounted on poly-L-lysine-coated slides. IHC staining for ATF3, ATF4, and CHOP was performed using the immunoperoxidase method. Slides were deparaffinized, rehydrated, and subjected to antigen retrieval in 10 mmol/L citrate buffer (pH 6.0) for 15 min. Endogenous peroxidase activity was quenched with 0.3% hydrogen peroxide for 15 min. The Mouse/Rabbit PolyDetector Plus DAB HRP kit (BioSB, BSB0261) was used in accordance with the manufacturer’s protocol. Slides were incubated overnight at 4 °C with primary antibodies against ATF3 (1:100, Abcam, ab191513), ATF4 (1:100, Elabscience, E-AB-13942), or CHOP (1:100, Abcam, ab11419), followed by detection with secondary antibodies, DAB color development, and hematoxylin counterstaining. Negative controls were prepared by omitting the primary antibodies.
Staining was evaluated using a semiquantitative immunoreactive score (IRS) method, calculated by multiplying staining intensity (0 = no staining, 1 = weak, 2 = moderate, 3 = strong) by the percentage of positive cells (1 = ≤ 25%, 2 = 26–50%, 3 = 51–75%, 4 = ≥ 76%). For each patient, the mean IRS from triplicate cores was calculated and used for statistical analysis. Based on the median IRS across the cohort, patients were categorized into two groups for each marker: ATF3: Low ( < 2) vs. High ( ≥ 2); ATF4: Low ( < 9) vs. High ( ≥ 9); CHOP: Low ( < 2) vs. High ( ≥ 2).
Statistical analysis
Statistical analyses were performed using SPSS software version 25.0 (IBM Corp., Chicago, IL, USA). Data are presented as mean ± standard error of the mean (SEM) for animal studies and cell migration assays, and as mean ± standard deviation (SD) for in vitro experiments. Each experiment was independently repeated at least three times. Comparisons between two groups were conducted using an unpaired two-tailed Student’s t-test. For comparisons among more than two groups, one-way analysis of variance (ANOVA) followed by a post hoc test was used to determine statistical significance. A p value < 0.05 was considered statistically significant.
Survival analyses were conducted using the Kaplan–Meier method, and differences between survival curves were assessed using the log-rank test. Univariate and multivariate Cox proportional hazards regression analyses were performed to evaluate the association between clinical variables and survival outcomes. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated for each variable.
Data availability
All data supporting the findings of this study are included in the article and its Reporting Summary. Additional information is available from the corresponding author upon reasonable request.
References
Barsouk A, Aluru JS, Rawla P, Saginala K, Barsouk A. Epidemiology, risk factors, and prevention of head and neck squamous cell carcinoma. Med Sci (Basel). 2023;11:42.
Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29:4294–301.
Chuang HC, Tsai MH, Lin YT, Chou MH, Yang KL, Chien CY. Systemic and local effects among patients with betel quid-related oral cancer. Technol Cancer Res Treat. 2022;21:15330338221146870.
Johnson DE, Burtness B, Leemans CR, Lui VWY, Bauman JE, Grandis JR. Head and neck squamous cell carcinoma. Nat Rev Dis Prim. 2020;6:92.
Alsahafi E, Begg K, Amelio I, Raulf N, Lucarelli P, Sauter T, et al. Clinical update on head and neck cancer: molecular biology and ongoing challenges. Cell Death Dis. 2019;10:540.
Zhang J, Spath SS, Marjani SL, Zhang W, Pan X. Characterization of cancer genomic heterogeneity by next-generation sequencing advances precision medicine in cancer treatment. Precis Clin Med. 2018;1:29–48.
Papalouka C, Adamaki M, Batsaki P, Zoumpourlis P, Tsintarakis A, Goulielmaki M, et al. DNA damage response mechanisms in head and neck cancer: significant implications for therapy and survival. Int J Mol Sci. 2023;24:2760.
Ranasinghe R, Mathai ML, Zulli A. Cisplatin for cancer therapy and overcoming chemoresistance. Heliyon. 2022;8:e10608.
Britt EL, Raman S, Leek K, Sheehy CH, Kim SW, Harada H. Combination of fenretinide and ABT-263 induces apoptosis through NOXA for head and neck squamous cell carcinoma treatment. PLoS One. 2019;14:e0219398.
Sharma K, Vu TT, Cook W, Naseri M, Zhan K, Nakajima W, et al. p53-independent Noxa induction by cisplatin is regulated by ATF3/ATF4 in head and neck squamous cell carcinoma cells. Mol Oncol. 2018;12:788–98.
Prabhu VV, Morrow S, Rahman Kawakibi A, Zhou L, Ralff M, Ray J, et al. ONC201 and imipridones: Anti-cancer compounds with clinical efficacy. Neoplasia. 2020;22:725–44.
Wei F, Fang R, Lyu K, Liao J, Long Y, Yang J, et al. Exosomal PD-L1 derived from head and neck squamous cell carcinoma promotes immune evasion by activating the positive feedback loop of activated regulatory T cell-M2 macrophage. Oral Oncol. 2023;145:106532.
Niknejad N, Gorn-Hondermann I, Ma L, Zahr S, Johnson-Obeseki S, Corsten M, et al. Lovastatin-induced apoptosis is mediated by activating transcription factor 3 and enhanced in combination with salubrinal. Int J Cancer. 2014;134:268–79.
Liu X, Lv Z, Zou J, Liu X, Ma J, Wang J, et al. Afatinib down-regulates MCL-1 expression through the PERK-eIF2alpha-ATF4 axis and leads to apoptosis in head and neck squamous cell carcinoma. Am J Cancer Res. 2016;6:1708–19.
Hu H, Tian M, Ding C, Yu S. The C/EBP Homologous Protein (CHOP) Transcription Factor Functions in Endoplasmic Reticulum Stress-Induced Apoptosis and Microbial Infection. Front Immunol. 2018;9:3083.
Liu K, Zhao C, Adajar RC, DeZwaan-McCabe D, Rutkowski DT. A beneficial adaptive role for CHOP in driving cell fate selection during ER stress. EMBO Rep. 2024;25:228–53.
Sancho M, Leiva D, Lucendo E, Orzaez M. Understanding MCL1: from cellular function and regulation to pharmacological inhibition. FEBS J. 2022;289:6209–34.
Brown A, Kumar S, Tchounwou PB. Cisplatin-based chemotherapy of human cancers. J Cancer Sci Ther. 2019;11:97.
Cheng Y, Li S, Gao L, Zhi K, Ren W. The molecular basis and therapeutic aspects of cisplatin resistance in oral squamous cell carcinoma. Front Oncol. 2021;11:761379.
Checa J, Aran JM. Reactive oxygen species: drivers of physiological and pathological processes. J Inflamm Res. 2020;13:1057–73.
Su LJ, Zhang JH, Gomez H, Murugan R, Hong X, Xu D, et al. Reactive oxygen species-induced lipid peroxidation in apoptosis, autophagy, and ferroptosis. Oxid Med Cell Longev. 2019;2019:5080843.
Tian X, Zhang S, Zhou L, Seyhan AA, Hernandez Borrero L, Zhang Y, et al. Targeting the integrated stress response in cancer therapy. Front Pharm. 2021;12:747837.
Iannelli F, Zotti AI, Roca MS, Grumetti L, Lombardi R, Moccia T, et al. Valproic acid synergizes with cisplatin and cetuximab in vitro and in vivo in head and neck cancer by targeting the mechanisms of resistance. Front Cell Dev Biol. 2020;8:732.
Seliger B, Al-Samadi A, Yang B, Salo T, Wickenhauser C. In vitro models as tools for screening treatment options of head and neck cancer. Front Med (Lausanne). 2022;9:971726.
Tian X, Srinivasan PR, Tajiknia V, Sanchez Sevilla Uruchurtu AF, Seyhan AA, Carneiro BA et al. Targeting apoptotic pathways for cancer therapy. J Clin Invest. 2024;134:e179570.
Kline CL, Van den Heuvel AP, Allen JE, Prabhu VV, Dicker DT, El-Deiry WS. ONC201 kills solid tumor cells by triggering an integrated stress response dependent on ATF4 activation by specific eIF2alpha kinases. Sci Signal. 2016;9:ra18.
Nwosu GO, Powell JA, Pitson SM. Targeting the integrated stress response in hematologic malignancies. Exp Hematol Oncol. 2022;11:94.
Hu H, Li B, Wang J, Tan Y, Xu M, Xu W, et al. New advances into cisplatin resistance in head and neck squamous carcinoma: Mechanisms and therapeutic aspects. Biomed Pharmacother. 2023;163:114778.
Zhao W, Sun M, Li S, Chen Z, Geng D. Transcription factor ATF3 mediates the radioresistance of breast cancer. J Cell Mol Med. 2018;22:4664–75.
Böpple K, Oren Y, Henry WS, Dong M, Weller S, Thiel J, et al. ATF3 characterizes aggressive drug-tolerant persister cells in HGSOC. Cell Death Dis. 2024;15:290.
Acknowledgements
This study was supported by grant number CRRPG8K0081-3, CORPG8L0331, CRRPG8N0041, CORPG8P0862 from the Center for Mitochondrial Research and Medicine, Chang Gung Memorial Hospital and MOST 111-2314-B-182A-099, MOST 111-2314-B-182A-079 -MY3, MOST 108-2314-B-182A-112-MY3 and MOST 107-2314-B-182A-085 from the Ministry of Science and Technology (National Science and Technology Council). We thank Yu-Li Liu, Rui-An Lin, Shin-Yan Lee, Yu-An Li and Chih-Kuan Chao for discussions and technical assistance. We thank Research Specimen Processing Laboratory for human tissue specimens and Institute for Translational Research in Biomedicine, Kaohsiung Chang Gung Memorial Hospital for instruments.
Author information
Authors and Affiliations
Contributions
HCC was responsible for drafting the manuscript, data acquisition, and final approval of the submitted version. MHT contributed to clinical data analysis, immunohistochemical evaluation, and survival analyses. JHC performed critical revision of the manuscript and approved the final version. YTH was responsible for data analysis, interpretation, and final approval of the manuscript. MHC and CYC contributed to the study conception and design, and approved the final version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. All animal procedures were conducted following protocols approved by the Institutional Animal Care and Usage Committee of Chang Guang Memorial Hospital (approval number: 2021122318). This study was approved by the Medical Ethics and Human Clinical Trial Committees of Chang Gung Memorial Hospital (Institutional Review Board approval number: 202302023B0). The IRB granted a waiver of informed consent from the participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chuang, HC., Tsai, MH., Chuang, JH. et al. ONC201 enhances the cytotoxic effect of cisplatin through ATF3/ATF4/CHOP in head and neck squamous cell carcinoma cells. Oncogenesis 14, 20 (2025). https://doi.org/10.1038/s41389-025-00563-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41389-025-00563-4