Abstract
Background
Hypertensive disorders of pregnancy (HDP) are associated with dysfunctional placentation and are a major cause of maternal and neonatal morbidity and mortality. Twin pregnancies have a larger placental mass and are a risk factor for HDP. The effect of HDP on neonatal outcomes in twin pregnancies is unknown.
Methods
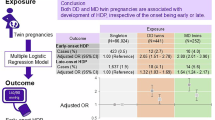
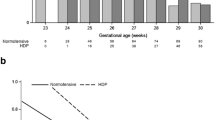
Retrospective cohort study using the Canadian Neonatal Network database from 2010–2018 of twin infants <29 weeks gestation born to mothers with HDP and normotensive pregnancies. Using multivariable models, we determined adjusted odds ratios (AORs) and 95% confidence intervals (CI) for mortality, bronchopulmonary dysplasia, severe neurologic injury, severe retinopathy of prematurity (ROP), necrotizing enterocolitis, and nosocomial infection in twin infants of mothers with HDP compared to twin infants of normotensive mothers.
Results
Of the 2414 eligible twin infants <29 weeks gestational age, 164 (6.8%) were born to mothers with HDP and had higher odds of severe ROP (AOR 2.48, 95% CI 1.34–4.59). Preterm twin infants born to mothers with HDP also had higher odds of mortality (AOR 2.02, 95% CI 1.23–3.32). There was no difference in other outcomes.
Conclusion
Preterm twin infants <29 weeks gestation of HDP mothers have higher odds of severe ROP and mortality.
Impact
Hypertensive disorders of pregnancy, associated with placental dysfunction, are a major cause of maternal and neonatal morbidity and mortality.
Twin pregnancy, associated with a larger placental mass, is a risk factor for hypertensive disorders of pregnancy.
The effect of hypertensive disorders of pregnancy on outcomes of preterm twins is unknown.
Preterm twins of mothers with hypertensive disorders of pregnancy are at higher risk of severe retinopathy of prematurity and mortality.
Our data can be used to counsel parents and identify infants at higher risk of severe retinopathy of prematurity and mortality.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Vest, A. R. & Cho, L. S. Hypertension in pregnancy. Curr. Atheroscler. Rep. 16, 395 (2014).
Hutcheon, J. A., Lisonkova, S. & Joseph, K. S. Epidemiology of pre-eclampsia and the other hypertensive disorders of pregnancy. Best. Pr. Res Clin. Obstet. Gynaecol. 25, 391–403 (2011).
Sava, R. I., March, K. L. & Pepine, C. J. Hypertension in pregnancy: taking cues from pathophysiology for clinical practice. Clin. Cardiol. 41, 220–227 (2018).
Davies, E. L., Bell, J. S. & Bhattacharya, S. Preeclampsia and preterm delivery: a population-based case–control study. Hypertens. Pregnancy 35, 510–519 (2016).
Matić, M., Inati, V., Abdel-Latif, M. E. & Kent, A. L. Maternal hypertensive disorders are associated with increased use of respiratory support but not chronic lung disease or poorer neurodevelopmental outcomes in preterm neonates at <29 weeks of gestation. J. Paediatrics Child Health 53, 391–398 (2017).
Gagliardi, L., Rusconi, F., Bellu, R. & Zanini, R. Association of maternal hypertension and chorioamnionitis with preterm outcomes. Pediatrics 134, e154–e161 (2014).
Razak, A. et al. Pregnancy-induced hypertension and neonatal outcomes: a systematic review and meta-analysis. J. Perinatol. 38, 46–53 (2018).
Gemmell, L. et al. Hypertensive disorders of pregnancy and outcomes of preterm infants of 24 to 28 weeks’ gestation. J. Perinatol. 36, 1067–1072 (2016).
Alshaikh, B., Salman, O., Soliman, N., Ells, A. & Yusuf, K. Pre-Eclampsia and the risk of retinopathy of prematurity in preterm infants with birth weight <1500 G and/or <31 weeks’ gestation. BMJ Open Ophthalmol. 1, e000049 (2017).
Huang, H.-C. et al. Preeclampsia and retinopathy of prematurity in very-low-birth-weight infants: a population-based study. PLOS ONE 10, e0143248 (2015).
Chan, P. Y. L. et al. Association of gestational hypertensive disorders with retinopathy of prematurity: a systematic review and meta-analysis. Sci. Rep. 6, 30732 (2016).
Chen, X., Wen, S., Smith, G., Yang, Q. & Walker, M. Pregnancy-induced hypertension and infant mortality: roles of birthweight centiles and gestational age. BJOG: Int. J. Obstet. Gynaecol. 114, 24–31 (2006).
Chen, X., Wen, S., Smith, G., Yang, Q. & Walker, M. General obstetrics: pregnancy-induced hypertension is associated with lower infant mortality in preterm singletons. BJOG: Int. J. Obstet. Gynaecol. 113, 544–551 (2006).
Nakamura, N. et al. Mortality and neurological outcomes in extremely and very preterm infants born to mothers with hypertensive disorders of pregnancy. Scientific Reports 11, 1729 (2021).
McBride, C. A., Bernstein, I. M., Badger, G. J., Horbar, J. D. & Soll, R. F. The effect of maternal hypertension on mortality in infants 22, 29 weeks gestation. Pregnancy Hypertension: Int. J. Women’s Cardiovascular Health 5, 362–366 (2015).
Roberts, C. L., Ford, J. B., Henderson‐Smart, D. J., Algert, C. S. & Morris, J. M. Hypertensive disorders in pregnancy: a population‐based study. Med. J. Aust. 182, 332–335 (2005).
Staff, A. C. The two-stage placental model of preeclampsia: an update. J. Reprod. Immunol. 134–135, 1–10 (2019).
Sparks, T. N., Nakagawa, S. & Gonzalez, J. M. Hypertension in Dichorionic Twin Gestations: How Is Birthweight Affected?* J Maternal-Fetal Neonatal Med. 30, 380–385 (2017).
Laine, K. et al. Prevalence and risk of pre-eclampsia and gestational hypertension in twin pregnancies: a population-based register study. BMJ Open 9, e029908 (2019).
Bdolah, Y. et al. Twin pregnancy and the risk of preeclampsia: bigger placenta or relative ischemia? Am. J. Obstet. Gynecol. 198, 428.e421–426 (2008).
Bartnik, P. et al. Twin chorionicity and the risk of hypertensive disorders: gestational hypertension and pre-eclampsia. Twin Res. Hum. Genet. 19, 377–382 (2016).
Geisler, M. E., O’Mahony, A., Meaney, S., Waterstone, J. J. & O’Donoghue, K. Obstetric and perinatal outcomes of twin pregnancies conceived following Ivf/Icsi treatment compared with spontaneously conceived twin pregnancies. Eur. J. Obstet. Gynecol. Reprod. Biol. 181, 78–83 (2014).
Elsayed, E. et al. Outcomes of singleton small for gestational age preterm infants exposed to maternal hypertension: a retrospective cohort study. Pediatr. Res. 86, 269–275 (2019).
Collins, J. Global epidemiology of multiple birth. Reprod. Biomed. Online 15(Suppl 3), 45–52 (2007).
Lee, S. K. et al. Variations in practice and outcomes in the Canadian Nicu Network: 1996–1997. Pediatrics 106, 1070–1079 (2000).
Shah, P. S. et al. Internal audit of the Canadian Neonatal network data collection system. Am. J. Perinatol. 34, 1241–1249 (2017).
Network, T. C. N. Cnn Abstractor’s Manual V.3.4.4. (The Canadian Neonatal Network, Toronto, Canada) (2020).
Morse, S., Groer, M., Shelton, M. M., Maguire, D. & Ashmeade, T. A systematic review. J. Perinat. Neonatal. Nurs. 29, 315–344 (2015).
Shennan, A. T., Dunn, M. S., Ohlsson, A., Lennox, K. & Hoskins, E. M. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics 82, 527–532 (1988).
Papile, L. A., Munsick-Bruno, G. & Schaefer, A. Relationship of cerebral intraventricular hemorrhage and early childhood neurologic handicaps. J. Pediatr. 103, 273–277 (1983).
Ronnback, M., Lampinen, K., Groop, P. H. & Kaaja, R. Pulse wave reflection in currently and previously preeclamptic women. Hypertens. Pregnancy 24, 171–180 (2005).
Bell, M. J. et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann. Surg. 187, 1–7 (1978).
Breathnach, F. M. & Malone, F. D. Fetal growth disorders in twin gestations. Semin Perinatol. 36, 175–181 (2012).
Hehir, M. P. et al. Gestational hypertensive disease in twin pregnancy: influence on outcomes in a large national prospective cohort. Aust. N.Z. J. Obstet. Gynaecol. 56, 466–470 (2016).
Zayed, M. A., Uppal, A. & Hartnett, M. E. New-onset maternal gestational hypertension and risk of retinopathy of prematurity. Investig. Opthalmol. Vis. Sci. 51, 4983 (2010).
Rivera, J. C. et al. Ischemic retinopathies: oxidative stress and inflammation. Oxid. Med. Cell. Longev. 2017, 1–16 (2017).
Holmström, G., Thomassen, P. & Broberger, U. Maternal risk factors for retinopathy of prematurity – a population-based study. Acta Obstetricia et. Gynecologica Scandinavica 75, 628–635 (1996).
Yu, X. D., Branch, D. W., Karumanchi, S. A. & Zhang, J. Preeclampsia and retinopathy of prematurity in preterm births. Pediatrics 130, e101–e107 (2012).
Kalay, S. et al. The role of Vegf and its soluble receptor Vegfr-1 in preterm newborns of preeclamptic mothers with Rds. J. Matern.-Fetal Neonatal. Med. 26, 978–983 (2013).
Fortes Filho, J. B. et al. Maternal preeclampsia protects preterm infants against severe retinopathy of prematurity. J. Pediatr. 158, 372–376 (2011).
Shah, V. A., Yeo, C. L., Ling, Y. L. & Ho, L. Y. Incidence, risk factors of retinopathy of prematurity among very low birth weight infants in Singapore. Ann. Acad. Med. Singap. 34, 169–178 (2005).
Yang, C. Y. et al. Analysis of incidence and risk factors of retinopathy of prematurity among very-low-birth-weight infants in North Taiwan. Pediatr. Neonatol. 52, 321–326 (2011).
Özkan, H., Cetinkaya, M., Koksal, N., Özmen, A. & Yıldız, M. Maternal preeclampsia is associated with an increased risk of retinopathy of prematurity. J. Perinatal Med. 39, 523–527 (2011).
Zhu, T., Zhang, L., Zhao, F., Qu, Y. & Mu, D. Association of maternal hypertensive disorders with retinopathy of prematurity: a systematic review and meta-analysis. PLOS ONE 12, e0175374 (2017).
McBride, C. A., Bernstein, I. M., Badger, G. J. & Soll, R. F. Maternal hypertension and mortality in small for gestational age 22- to 29-week infants. Reprod. Sci. 25, 276–280 (2018).
Soliman, N., Chaput, K., Alshaikh, B. & Yusuf, K. Preeclampsia and the risk of bronchopulmonary dysplasia in preterm infants less than 32 weeks’ gestation. Am. J. Perinatol. 34, 585–592 (2017).
Regev, R. H. et al. Outcome of singleton preterm small for gestational age infants born to mothers with pregnancy-induced hypertension. A population-based study. J. Matern.-Fetal Neonatal Med. 28, 666–673 (2015).
Jaskolka, D., Retnakaran, R., Zinman, B. & Kramer, C. Fetal sex and maternal risk of pre-eclampsia/eclampsia: a systematic review and meta-analysis. BJOG: Int. J. Obstet. Gynaecol. 124, 553–560 (2017).
Shapiro-Mendoza, C. K. et al. Effect of late-preterm birth and maternal medical conditions on newborn morbidity risk. Pediatrics 121, e223–e232 (2008).
Acknowledgements
The authors thank all site investigators and data abstractors of the Canadian Neonatal Network (CNN) and the Canadian Neonatal Follow-Up Network (CNFUN). Full lists of Network member investigators and their affiliations appear in Supplementary Information. We thank Heather McDonald-Kinkaid, PhD, of the Maternal-infant Care Research Centre (MiCare) at Mount Sinai Hospital in Toronto, Ontario, Canada, for editorial support in preparing this manuscript; and other MiCare staff, for organizational support. MiCare is supported by the Canadian Institutes of Health Research, the Ontario Ministry of Health and Long-Term Care, and the participating hospitals.
Funding
Although no specific funding was received for this study, organizational support for the Canadian Neonatal Network and the Canadian Neonatal Follow-Up Network was provided by the Maternal-infant Care Research Centre (M.C.) at Mount Sinai, Hospital in Toronto, Ontario, Canada. M.C. is supported by a Canadian Institutes of Health, Research (CIHR) Team Grant (CTP 87518), the Ontario Ministry of Health and Long-Term, Care, and the participating hospitals. P.S.S. holds a CIHR Applied Research Chair in Reproductive, and Child Health Services and Policy Research (APR-126340).
Author information
Authors and Affiliations
Consortia
Contributions
K.Y.: Concept and design, supervised and revised the proposal, drafting of the manuscript, revision of the manuscript. K.Y.: Wrote the proposal, interpreted data, drafting of manuscript, revision of the manuscript. B.A.: Reviewed proposal, interpreted data, revision and critical appraisal of the manuscript. S.H.: Reviewed proposal, interpreted data, revision, and critical appraisal of the manuscript. D.L.: Interpreted data, revision, and critical appraisal of the manuscript. J.E.: Interpreted data, revision, and critical appraisal of the manuscript. M.C.: Interpreted data, revision, and critical appraisal of the manuscript. M.B.: Revision and critical appraisal of the manuscript, acquisition and analysis of data. P.S.S.: Revision and critical appraisal of the manuscript, acquisition, and analysis of data. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work in ensuring that questions related to its accuracy or integrity are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
A retrospective cohort study using anonymized data form a large data base. The study was approved by the Conjoint Health Research Ethics Board University of Calgary.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yurkiw, K., Alshaikh, B., Hasan, S.U. et al. Neonatal outcomes of twins <29 weeks gestation of mothers with hypertensive disorders of pregnancy. Pediatr Res 92, 748–753 (2022). https://doi.org/10.1038/s41390-022-02044-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-022-02044-5
This article is cited by
-
The impact of hypertensive disorders of pregnancy on perinatal outcomes in twin pregnancies: a national multi-center cohort study
BMC Pregnancy and Childbirth (2025)