Abstract
Background
To analyse the associations between daily steps, cardiorespiratory fitness (CRF), and remnant cholesterol in schoolchildren and to investigate whether the association between daily steps and remnant cholesterol is mediated by CRF.
Methods
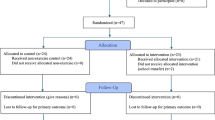
This cross-sectional study involved 394 schoolchildren (aged 9–12 years, 53.0% girls) from Cuenca, Spain. Daily steps were measured using the Xiaomi MI Band 3, CRF was assessed using the 20-m shuttle run test, and remnant cholesterol was calculated from total cholesterol, high-density lipoprotein cholesterol and low-density lipoprotein cholesterol. Mean differences in CRF and remnant cholesterol by daily steps and CRF categories were tested using analysis of covariance. Mediation analysis models examined whether CRF mediates the association between daily steps and remnant cholesterol.
Results
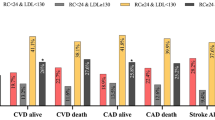
Children taking 12,000 and 9000 steps/day had higher CRF (p < 0.001) and lower remnant cholesterol (p = 0.034), respectively. Those with CRF > 47.59 kg/ml/min had lower remnant cholesterol (p = 0.009). CRF mediated the association between 1000 steps/day and remnant cholesterol (indirect effect = –0.027 (–0.055,–0.007)).
Conclusions
Both daily steps and CRF are associated with remnant cholesterol. Promoting an increase in daily steps may be a practical and promising strategy to increase CRF and, given its mediating role, to improve remnant cholesterol to prevent cardiometabolic risk in schoolchildren.
Impact
-
What’s known: Remnant cholesterol is a critical indicator of cardiovascular disease risk in the early atherosclerosis.
-
What’s new: In schoolchildren, increased daily physical activity is significantly associated with higher cardiorespiratory fitness and lower remnant cholesterol, especially walking >9000 steps/day and >12,000 steps/day, respectively.
-
What’s relevant: Encouraging schoolchildren to take more daily steps may be a promising strategy to increase cardiorespiratory fitness and, given its mediating role, to improve remnant cholesterol to prevent cardiometabolic risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 14 print issues and online access
$259.00 per year
only $18.50 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets used and/or analysed in this study are available from the corresponding author upon reasonable request.
References
Roeters Van Lennep, J. E. et al. Women, lipids, and atherosclerotic cardiovascular disease: a call to action from the European Atherosclerosis Society. Eur. Heart J. 44, 4157–4173 (2023).
Hong, Y. M. Atherosclerotic cardiovascular disease beginning in childhood. Korean Circ. J. 40, 1–9 (2010).
Napoli, C. et al. Fatty streak formation occurs in human fetal aortas and is greatly enhanced by maternal hypercholesterolemia. Intimal accumulation of low density lipoprotein and its oxidation precede monocyte recruitment into early atherosclerotic lesions. J. Clin. Invest 100, 2680–2690 (1997).
Napoli, C. et al. Influence of maternal hypercholesterolaemia during pregnancy on progression of early atherosclerotic lesions in childhood: fate of Early Lesions in Children (FELIC) study. Lancet 354, 1234–1241 (1999).
Pool, L. R. et al. Childhood risk factors and adulthood cardiovascular disease: a systematic review. J. Pediatr. 232, 118–126.e23 (2021).
Jacobs, D. R. et al. Childhood cardiovascular risk factors and adult cardiovascular events. N. Engl. J. Med. 386, 1877–1888 (2022).
Twisk, J. W. R., Kemper, H. C. G. & Van Mechelen, W. Tracking of activity and fitness and the relationship with cardiovascular disease risk factors. Med. Sci. Sports Exerc. 32, 1455–1461 (2000).
Martínez-Vizcaíno, V. & Sánchez-López, M. Relationship between physical activity and physical fitness in children and adolescents. Rev. Esp. Cardiol. 61, 108–111 (2008).
Nagata, J. M. et al. Physical activity from young adulthood to middle age and premature cardiovascular disease events: a 30-year population-based cohort study. Int. J. Behav. Nutr. Phys. Act. 19, 123 (2022).
Michos, E. D., McEvoy, J. W. & Blumenthal, R. S. Lipid management for the prevention of atherosclerotic cardiovascular disease. N. Engl. J. Med. 381, 1557–1567 (2019).
Kraus, W. E. et al. Physical activity, all-cause and cardiovascular mortality, and cardiovascular disease. Med. Sci. Sports Exerc. 51, 1270–1281 (2019).
Luo, Y. & Peng, D. Residual atherosclerotic cardiovascular disease risk: focus on non-high-density lipoprotein cholesterol. J. Cardiovasc. Pharmacol. Ther. 28, https://doi.org/10.1177/10742484231189597 (2023)
Crea, F. High-density lipoproteins, lipoprotein(a), and remnant cholesterol: new opportunities for reducing residual cardiovascular risk. Eur. Heart J. 44, 1379–1382 (2023).
Varbo, A. & Nordestgaard, B. G. Remnant cholesterol and triglyceride-rich lipoproteins in atherosclerosis progression and cardiovascular disease. Arterioscler. Thromb. Vasc. Biol. 36, 2133–2135 (2016).
Baratta, F. et al. Cholesterol remnants, triglyceride-rich lipoproteins and cardiovascular risk. Int. J. Mol. Sci. 24, 4268 (2023).
Delialis, D. et al. Remnant cholesterol and atherosclerotic disease in high cardiovascular risk patients. Beyond LDL cholesterol and hypolipidemic treatment. Hellenic J. Cardiol. 66, 26–31 (2022).
Kondamudi, N., Mehta, A., Thangada, N. D. & Pandey, A. Physical activity and cardiorespiratory fitness: vital signs for cardiovascular risk assessment. Curr. Cardiol. Rep. 23, 172 (2021).
Mozaffarian, D. et al. Heart Disease and Stroke Statistics-2016 Update: a report from the American Heart Association. Circulation 133, e38–e48 (2016).
WHO. Global status report on physical activity 2022: executive summary (2022).
Casado-Robles, C., Viciana, J., Guijarro-Romero, S. & Mayorga-Vega D. Effects of consumer-wearable activity tracker-based programs on objectively measured daily physical activity and sedentary behavior among school-aged children: a systematic review and meta-analysis. Sports Med. Open 8, 18 (2022).
Pozuelo-Carrascosa, D. P., García-Hermoso, A., Álvarez-Bueno, C., Sánchez-López, M. & Martinez-Vizcaino, V. Effectiveness of school-based physical activity programmes on cardiorespiratory fitness in children: a meta-analysis of randomised controlled trials. Br. J. Sports Med. 52, 1234–1240 (2018).
Mayorga-Vega, D., Casado-Robles, C., López-Fernández, I. & Viciana, J. A comparison of the utility of different step-indices to translate the physical activity recommendation in adolescents. J. Sports Sci. 39, 469–479 (2021).
Ross, R. et al. Precision exercise medicine: understanding exercise response variability. Br. J. Sports Med. 53, 1141–1153 (2019).
Rodríguez-Gutiérrez, E. et al. Steps per day and health-related quality of life in schoolchildren: the mediator role of cardiorespiratory fitness. Eur. J. Pediatr. 183, 739–748 (2024).
Paluch, A. E. et al. Prospective association of daily steps with cardiovascular disease: a harmonized meta-analysis. Circulation 147, 122–131 (2023).
Banach, M. et al. The association between daily step count and all-cause and cardiovascular mortality: a meta-analysis. Eur. J. Prev. Cardiol. 18, 1975–1985 (2023).
Stens, N. A. et al. Relationship of daily step counts to all-cause mortality and cardiovascular events. J. Am. Coll. Cardiol. 15, 1483–1494 (2023).
Sheng, M. et al. The relationships between step count and all-cause mortality and cardiovascular events: a dose-response meta-analysis. J. Sport Health Sci. 10, 620–628 (2021).
Rodríguez-Gutiérrez, E. et al. Daily steps and all-cause mortality: an umbrella review and meta-analysis. Prev. Med. 185, 108047 (2024).
Ramírez-Vélez, R. et al. Cardiorespiratory fitness, adiposity, and cardiometabolic risk factors in schoolchildren: the FUPRECOL study. West. J. Nurs. Res. 39, 1311–1329 (2017).
Sequí-Domínguez, I. et al. Association of daily steps on lipid and glycaemic profiles in children: the mediator role of cardiorespiratory fitness. Acta Paediatr. 113, 296–302 (2024).
Reyes-Ferrada, W. et al. Cardiorespiratory fitness, physical activity, sedentary time and its association with the atherogenic index of plasma in Chilean adults: influence of the waist circumference to height ratio. Nutrients 12, 1250 (2020).
Muscella, A., Stefàno, E. & Marsigliante, S. The effects of exercise training on lipid metabolism and coronary heart disease. Am. J. Physiol. Heart Circ. Physiol. 319, H76–H88 (2020).
Packard, C. J. Remnants, LDL, and the quantification of lipoprotein-associated risk in atherosclerotic cardiovascular disease. Curr. Atheroscler. Rep. 24, 133–142 (2022).
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310, 2191–2194 (2013).
Casado-Robles, C., Mayorga-Vega, D., Guijarro-Romero, S. & Viciana, J. Validity of the Xiaomi Mi Band 2, 3, 4 and 5 wristbands for assessing physical activity in 12-to-18-year-old adolescents under unstructured free-living conditions. fit-person study. J. Sports Sci. Med. 22, 196 (2023).
Sajja, A. et al. Discordance between standard equations for determination of LDL cholesterol in patients with atherosclerosis. J. Am. Coll. Cardiol. 79, 530–541 (2022).
Martin, S. S. et al. Comparison of a novel method vs the Friedewald equation for estimating low-density lipoprotein cholesterol levels from the standard lipid profile. JAMA 310, 2061–2068 (2013).
Léger, L., Lambert, J., Goulet, A., Rowan, C. & Dinelle, Y. Aerobic capacity of 6 to 17-year-old Quebecois-20 meter shuttle run test with 1 min stages. Can. J. Appl. Sport Sci. 9, 64–69 (1984).
Léger, L. A., Mercier, D., Gadoury, C. & Lambert, J. The multistage 20 metre shuttle run test for aerobic fitness. J. Sports Sci. 6, 93–101 (1988).
José de Menezes, F., Correa de Jesus, Í. & Leite, N. Predictive equations of maximum oxygen consumption by shuttle run test in children and adolescents: a systematic review. Rev. Paul. de. Pediatr. 37, 241 (2019).
Textor, J., van der Zander, B., Gilthorpe, M. S., Liśkiewicz, M. & Ellison, G. T. Robust causal inference using directed acyclic graphs: the R package “dagitty. Int. J. Epidemiol. 45, 1887–1894 (2016).
Bolin, J. H. & Hayes, A. F. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: The Guilford Press. J. Educ. Meas. 51, 335–337 (2014).
Hayes A. F. Introduction to Mediation, Moderation, and Conditional Process Analysis: a Regression-based Approach. 2nd edn (New York: The Guilford Press, 2018).
Sterne, J. A. C. et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 338, 157–160 (2009).
Di Costanzo, A. et al. Elevated serum concentrations of remnant cholesterol associate with increased carotid intima-media thickness in children and adolescents. J. Pediatr. 232, 133–139.e1 (2021).
Navarese, E. P. et al. Independent causal effect of remnant cholesterol on atherosclerotic cardiovascular outcomes: a mendelian randomization study. Arterioscler. Thromb. Vasc. Biol. 43, e373–e380 (2023).
Hauser, C. et al. Cardiorespiratory fitness and development of childhood cardiovascular risk: the EXAMIN YOUTH follow-up study. Front. Physiol. 14, 1243434 (2023).
Diaz, E. C. et al. Cardiorespiratory fitness associates with blood pressure and metabolic health of children-the Arkansas active kids study. Med. Sci. Sports Exerc. 53, 2225–2232 (2021).
Isath, A. et al. Exercise and cardiovascular health: a state-of-the-art review. Prog. Cardiovasc. Dis. 79, 44–52 (2023).
Tucker, W. J. et al. Exercise for primary and secondary prevention of cardiovascular disease: JACC focus seminar 1/4. J. Am. Coll. Cardiol. 80, 1091–1106 (2022).
Bonikowske, A. R. et al. Evaluating current assessment techniques of cardiorespiratory fitness. Expert Rev. Cardiovasc. Ther. 22, 231–241 (2024).
Goodman, E., Dolan, L. M., Morrison, J. A. & Daniels, S. R. Factor analysis of clustered cardiovascular risks in adolescence: obesity is the predominant correlate of risk among youth. Circulation 111, 1970–1977 (2005).
Wei, D. et al. Lipoprotein profiles of fat distribution and its association with insulin sensitivity. Front Endocrinol. 13, 978745 (2022).
Koskinas, K. C. et al. Obesity and cardiovascular disease: an ESC clinical consensus statement. Eur. Heart J. 45, 4063–4098 (2024).
Perez-Bey, A. et al. Bidirectional associations between fitness and fatness in youth: a longitudinal study. Scand. J. Med. Sci. Sports 30, 1483–1496 (2020).
Lavie, C. J., Neeland, I. J. & Ortega, F. B. Intervention in school-aged children to prevent progression of obesity and cardiometabolic disease: a paradigm shift indeed. J. Am. Coll. Cardiol. 84, 509–511 (2024).
Santos-Beneit, G. et al. Effect of time-varying exposure to school-based health promotion on adiposity in childhood. J. Am. Coll. Cardiol. 84, 499–508 (2024).
Maffeis, C. Physical activity in the prevention and treatment of childhood obesity: physio-pathologic evidence and promising experiences. Int. J. Pediatr. Obes. 3, 29–32 (2008).
Aadland, E., Kvalheim, O. M., Anderssen, S. A., Resaland, G. K. & Andersen L. B. The multivariate physical activity signature associated with metabolic health in children. Int. J. Behav. Nutr. Phys. Act. 15, 106266 (2018).
Haapala, E. A. et al. Cardiorespiratory fitness, physical activity, and insulin resistance in children. Med. Sci. Sports Exerc. 52, 1144–1152 (2020).
Haapala, E. A. et al. Associations of physical activity, sedentary time, and diet quality with biomarkers of inflammation in children. Eur. J. Sport Sci. 22, 906–915 (2022).
González-Gil, E. M. et al. Improving cardiorespiratory fitness protects against inflammation in children: the IDEFICS study. Pediatr. Res. 91, 681–689 (2022).
Chung, S. T. et al. The relationship between lipoproteins and insulin sensitivity in youth with obesity and abnormal glucose tolerance. J. Clin. Endocrinol. Metab. 107, 1541–1551 (2022).
Montes-de-Oca-García, A. et al. Maximal fat oxidation capacity is associated with cardiometabolic risk factors in healthy young adults. Eur. J. Sport Sci. 21, 907–917 (2021).
Varbo, A., Benn, M., Tybjærg-Hansen, A. & Nordestgaard, B. G. Elevated remnant cholesterol causes both low-grade inflammation and ischemic heart disease, whereas elevated low-density lipoprotein cholesterol causes ischemic heart disease without inflammation. Circulation 128, 1298–1309 (2013).
Cesa, C. C. et al. Physical activity and cardiovascular risk factors in children: meta-analysis of randomized clinical trials. Prev. Med. 69, 54–62 (2014).
Nordestgaard, B. G. & Varbo, A. Triglycerides and cardiovascular disease. Lancet 384, 626–635 (2014).
Funding
This work was supported by the Ministry of Economy and Competitiveness-Carlos III Health Institute, and Health Outcomes-Oriented Cooperative Research Networks cofunded with European Union–NextGenerationEU (RD21/0016/0025) and by the Ministry of Science, Innovation and Universities-Carlos III Health Institute and FEDER funds (PI19/01126). Eva Rodríguez-Gutiérrez is supported by a grant from the University of Castilla-La Mancha (2022-UNIVERS-11373), and Bruno Bizzozero-Peroni is supported by a grant from the Universidad de Castilla‐La Mancha co-financed by the European Social Fund (2020-PREDUCLM-16746). Irene Martínez-García is supported by a grant from the Ministry of Science, Innovation and Universities (FPU21/06866). Valentina Díaz-Goñi is supported by a grant from the National Agency for Research and Innovation of Uruguay (POS_EXT_2023 _1_175630). The other authors received no additional funding.
Author information
Authors and Affiliations
Contributions
Eva Rodríguez-Gutiérrez conceptualized and designed the study, drafted the initial manuscript, and critically reviewed and revised the manuscript. Vicente Martínez-Vizcaíno designed the the data collection instruments, collected data, and critically reviewed and revised the manuscript. Bruno Bizzozero-Peroni and Valentina Díaz-Goñi carried out the initial analyses, and critically reviewed and revised the manuscript. Irene Martínez-García, Irene Sequí-Domínguez, and Sergio Núñez de Arenas-Arroyo collected data, and critically reviewed and revised the manuscript. Mairena Sánchez-López and Carlos Pascual-Morena designed the study, collected data, and critically reviewed and revised the manuscript. Ana Torres-Costoso coordinated and supervised data collection, and critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study protocol was approved by the Clinical Research Ethics Committee of the Hospital Virgen de la Luz in Cuenca (REG: 2019/PI1519). After the Board of Governors of each school approved the study, a letter was sent to the parents of all 4th, 5th and 6th graders inviting them to a meeting. At this meeting, we explained the objectives of the study and asked for written approval for their children’s participation. All procedures performed in this study were in accordance with the Declaration of Helsinki and its later amendments or comparable ethical standards for experiments involving humans.35
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rodríguez-Gutiérrez, E., Martínez-Vizcaíno, V., Bizzozero-Peroni, B. et al. Daily steps, cardiorespiratory fitness, and remnant cholesterol in schoolchildren: mediation effects for cardiovascular prevention. Pediatr Res 98, 672–679 (2025). https://doi.org/10.1038/s41390-024-03779-z
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41390-024-03779-z