Abstract
Background
Exposure to heat may increase the risk of intussusception through various mechanisms, including alterations in dietary intake. However, no nationwide studies have examined the association between daily heat exposure and intussusception in children. This study aims to examine the association between higher daily ambient temperatures and intussusception in children.
Methods
The daily number of intussusception hospitalizations among children up to 5 years old from 2011 to 2022 was extracted from Japan’s nationwide administrative claims database. Daily mean temperature data were obtained from the Japan Meteorological Agency. Since the focus is on heat exposure, the analysis examines hospitalizations that occurred during the five warmest months (May to September). A time-stratified case-crossover design with conditional quasi-Poisson regression analysis was applied to estimate the relative risk of heat exposure on intussusception with a lag of 0–4 days.
Results
There were 13,083 cases of intussusception hospitalizations. Higher daily mean temperatures were associated with an elevated risk of intussusception hospitalizations. Specifically, exposure to extremely high daily mean temperatures at the 99th percentile was associated with a 39% increase in hospitalization risk (95% CI: 1.05, 1.83).
Conclusion
The study found the association between higher daily mean temperatures and an increased risk of hospitalization for intussusception. Future research should clarify the mechanisms of the association between higher daily mean temperatures and the increased risk of intussusception hospitalizations.
Impact
-
While exposure to heat may increase the risk of intussusception through mechanisms such as alterations in dietary intake and intestinal motility, no nationwide studies have investigated the association between daily heat exposure and intussusception in children.
-
The study found the association between higher daily mean temperatures and an increased risk of hospitalization for intussusception.
-
Both caregivers and healthcare providers should be aware of a potential increase in pediatric intussusception cases during warmer days, which may become even more critical as climate change results in more frequent and severe heat events.
Similar content being viewed by others
Introduction
Intussusception is one of the most common causes of pediatric abdominal emergencies, affecting both infants and children.1,2 This condition occurs when part of the intestinal tract is pulled into the adjacent segment towards the anal side, leading to obstruction, bowel necrosis, or, in severe cases, death if not treated promptly.2 Most cases of intussusception are primary (i.e., idiopathic), with secondary cases, caused by pathological lead points such as Meckel’s diverticulum and duplication cysts, account for only 1–4% of all cases in children under 5 years of age.2,3 A delay in the diagnosis and treatment of intussusception can have serious consequences,2 emphasizing the importance of understanding the risk factors involved in this condition.
Previous studies have explored various risk factors for intussusception, with several focusing on seasonal patterns. For example, research conducted in northeastern China, Taiwan, Korea, and India has shown a higher incidence during the warmer months.4,5,6,7 However, these findings remain inconclusive, as other studies from Switzerland,8 multiple Latin American countries,9 and Japan10 finding no clear seasonal trend.
Interestingly, some studies from China and India have further investigated the association between ambient temperature and intussusception, reporting associations between higher temperatures and an increased risk of intussusception in children.1,4,5,11 Possible mechanisms underlying this association include alterations in dietary intake and intestinal motility during warmer temperatures.12,13,14,15 Given that climate change is expected to further increase the frequency and severity of extreme weather events,16 research into the effects of heat on health outcomes, particularly for vulnerable populations such as children, is crucial for understanding the potential impacts of a warmer future. However, existing studies on the association between ambient temperature and intussusception have primarily relied on the analysis of monthly or weekly incidence in relation to average temperatures, often without accounting for potential confounders such as long-term trends and seasonality. Furthermore, no large nationwide studies have examined the association between higher daily ambient temperatures and intussusception in children to date.
Building on the methodology from our previous studies,17,18,19,20 this research employs a time-stratified case-crossover design to investigate the association between higher daily ambient temperatures and intussusception in children in Japan. The use of the time-stratified case-crossover with daily ambient temperature and hospitalization data allows for the control of potential confounders by stratifying time by month and day of the week.21,22 Utilizing a comprehensive dataset from Japan’s administrative claims database, which includes 13,083 pediatric intussusception patients, this study seeks to provide new insights into the role of temperature, particularly extreme heat exposure, as a risk factor for pediatric intussusception.
Method
Hospital admission data
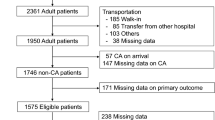
Data on hospital admissions was obtained from the Diagnosis Procedure Combination (DPC).23 The DPC had been adopted by 1764 facilities by 2022, covering 483,425 beds, which accounts for over half of all acute-care hospital beds in Japan.24 The International Classification of Diseases, Tenth Revision (ICD-10) codes are used to classify disease diagnoses. Children aged 5 years and under who were hospitalized for intussusception between 2011 and 2022 were identified using the corresponding ICD-10 code (K561). Since the exposure of interest was heat, we focused on hospitalizations occurring during the five warmest months (May to September).25 In the DPC database, 26,445 cases of hospitalization due to intussusception were recorded among children aged 5 years or younger between 2011 and 2022. After excluding 13,362 cases hospitalized from January to April and October to December, the remaining 13,083 cases were included in the analysis for this study. There were no missing values for age, gender, or prefectural information in the DPC data provided for analysis (Fig. 1). This study was approved by the Medical Research Ethics Committee at Tokyo Medical and Dental University (Institute of Science Tokyo).
Meteorological data
Temperature data from May to September for the years 2011–2022 were collected from the Japan Meteorological Agency (JMA) website, using measurements from observatories closest to the capitals of each prefecture.26 The daily mean temperature was calculated by taking the average of the hourly measurements from 1:00 a.m. to midnight.27 There were no missing values for the mean temperature. These daily weather data were subsequently linked to daily hospitalization records for each prefecture.
Study design
A time-stratified case-crossover design was used to investigate the association between daily mean temperature and pediatric intussusception hospitalizations in each prefecture. Case days were matched to control days that occurred on the same day of the week, within the same month, year, and prefecture.21 For each case day, 3 to 4 control days (occurring either before or after the case day within the same month) were selected. The relative risk was estimated by comparing the temperature on the case day (day X) to the temperatures from other days within the same stratum (e.g., X-14 days, X-7 days, X + 7 days, and X + 14 days). This design adjusted for the effects of the day of the week, seasonality, and long-term trends by stratifying time by month and day of the week.22 Additionally, this method inherently adjusts for individual characteristics within each prefecture’s population, such as genetic factors, which are unlikely to vary within short periods and could otherwise confound the association between temperature and pediatric intussusception hospitalizations.28
Statistical analysis
A conditional quasi-Poisson regression model was employed to estimate the relative risk of pediatric intussusception hospitalizations associated with daily mean temperature, allowing for flexible parameter estimation and adjusting for overdispersion. In addition, a distributed lag nonlinear model (DLNM) was used to assess the association between daily mean temperature and pediatric intussusception hospitalizations, while accounting for lagged effects. A natural cubic spline was applied to model the association between exposure and the response, with a single knot placed at the 50th percentile of the temperature distribution across the 47 prefectures. Similarly, a natural cubic spline with one knot, equally spaced on a logarithmic scale of lag days, was used to model the association between lag and response. The number of knots tested ranged from 1 to 2 for both temperature and lag, and the optimal number was determined by the lowest quasi-Akaike’s Information Criterion (QAIC) value, summed across all prefectures.29 In this study, one knot for temperature and one knot for lag provided the best model fit. A lag period of 0–4 days was used to capture the lagged effects of exposure. For the meta-analysis, prefecture-specific exposure-outcome associations cumulated over this lag period were first derived. Subsequently, a multivariate random-effects meta-analysis was performed to pool the cumulative exposure-outcome associations across all 47 prefectures.30 The temperature associated with the lowest risk was used as the reference point.31 Residual heterogeneity was evaluated using Cochran’s Q test and the I² statistic.
Sensitivity analyses were performed by adjusting the number of knots for temperature from one at the 50th percentile to two at the 33rd and 67th percentiles, with lag periods of 0–3 days and 0–5 days. An additional sensitivity analysis was conducted, focusing on data from 2013 onwards. The reason for conducting a sensitivity analysis using data from 2013 onwards was that intussusception is well known to be associated with the rotavirus vaccine.32 Since Rotarix® (RV1) became available for voluntary vaccination in November 2011 and RotaTeq® (RV5) in July 2012, we also wanted to evaluate the robustness of the results by focusing on data from 2013 onwards,32 when the transition phase for the introduction of these vaccines was completed.
All analyses were conducted using R version 4.4.1 (R Development Core Team, Vienna, Austria, 2014). The ‘dlnm’ package was used for DLNM, ‘gnm’ for conditional quasi-Poisson regression, and ‘mixmeta’ for multivariate meta-analysis.
Results
Table 1 presents the descriptive statistics of intussusception hospitalizations across the prefectures. During the study period, a total of 13,083 hospitalizations were recorded, with male patients accounting for 65.1% of the cases. Overall, 64.4% of the patients were aged ≤1 year, and the average age was 1.3 years (SD = 1.3). Supplementary Table 1 shows descriptive statistics of the daily mean temperature for each prefecture. The median temperature across all prefectures during the study period was 24.0 °C.
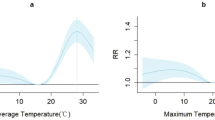
Figure 2a shows the association between daily mean temperature and intussusception hospitalizations, based on the cumulative relative risk over a lag period of 0–4 days, as derived from the meta-analysis. There was no significant heterogeneity detected among the prefectures (Q = 101.1, p = 0.241; I2 = 9.0%). Higher mean temperatures were associated with an elevated risk of hospitalization. Table 2 shows relative risk associated with each daily mean temperature percentile derived from the meta-analysis. Specifically, extremely high daily mean temperatures (at the 90th and 99th percentiles) were associated with a 46% increased risk of hospitalization (95% confidence interval [CI]: 1.11, 1.92) and a 39% increase (95% CI: 1.05, 1.83), respectively. Figure 2b shows the lag-response curve, which indicate that the increased risk of hospitalization associated with exposure to high temperatures occurs approximately 0–3 days post-exposure. Supplementary Table 2 shows the associations between each percentile of daily mean temperatures and hospitalization for intussusception in children up to 5 years of age in each prefecture prior to the meta-analysis.
Table 3 presents the results of the sensitivity analyses, showing that our findings remained consistent even after adjusting the number of temperature knots from one at the 50th percentile to two at the 33rd and 67th percentiles, as well as with lag periods of 0–3 days and 0–5 days. For example, in the analysis where the number of temperature knots was adjusted from one to two, extremely high daily mean temperatures at the 99th percentile were associated with a 56% increased risk of hospitalization (95% CI: 1.09, 2.24). The results also remained consistent in an additional sensitivity analysis focusing on data from 2013 onwards. In addition, the small number of cases in Yamanashi Prefecture may have resulted in an unstable estimation of relative risk for this prefecture. To address this, we conducted an additional sensitivity analysis excluding cases from Yamanashi during the meta-analysis. Nonetheless, the results remained consistent. Specifically, extremely high daily mean temperatures at the 99th percentile were associated with a 36% increased risk of hospitalization (95% CI: 1.04, 1.80). Supplementary Fig. 1a–e illustrates the corresponding association between daily mean temperature and intussusception hospitalizations. All figures consistently demonstrate that, even with sensitivity analyses, higher daily mean temperatures were associated with an increased risk of hospitalization.
Discussion
The study found that higher daily mean temperatures were associated with an increased risk of hospitalization for intussusception in children. With climate change expected to intensify the severity and frequency of extreme weather events, such as heatwaves,16 these findings are critical for understanding the potential health impacts of heat exposure within the context of climate change.
Previous studies from China and India have identified associations between higher temperatures and an increased risk of intussusception in children.1,4,5,11 For example, research conducted in Shenyang4 and Suzhou, China,11 as well as a study using data from 20 hospitals in India,5 found that higher monthly mean temperatures were associated with an increase in monthly intussusception cases in children. A single-center study from Hangzhou, China, used Spearman correlation and Poisson regression analyses to show that weekly mean temperatures were linked to intussusception hospitalizations in children.1 These studies were pioneering; however, they neither used daily data nor employed the time-stratified case-crossover design, both of which are essential for effectively controlling for long-term trends and seasonality.21,22 To our knowledge, this is the first large nationwide study to use daily data and the time-stratified case-crossover design to demonstrate this association.
Possible mechanisms linking high temperatures to intussusception include alterations in dietary intake and intestinal motility during warmer months. Previous studies suggests that changes in intestinal motility,12,13 and dietary patterns13 may contribute to the acute development of intussusception, as demonstrated in animal models. One study12 showed that mice developed intussusception six hours after the injection of a triggering agent. Furthermore, food allergies have been associated with an increased risk of intussusception;14 notably, a case report described a patient who developed anaphylaxis and intussusception simultaneously after consuming salmon roe, with the authors attributing this to intestinal contractions triggered by the food allergy.15 While not everyone experiences anaphylaxis, it is plausible that even mild allergic reactions to food could lead to the release of histamine, which may alter intestinal motility and contribute to the development of intussusception. This is supported by a basic mechanistic study showing that histamine, a major mediator of anaphylaxis,33 can alter intestinal contractility.33,34 These findings suggest that dietary changes induced by warmer temperatures could potentially lead to alterations in intestinal motility, which, over the course of several days, might contribute to the onset of intussusception. Interestingly, the lag-response curve from our analysis indicates that the increased risk of hospitalization associated with extremely high daily mean temperatures at the 99th percentile occurs approximately 0–3 days post-exposure. Future research is warranted to investigate whether alterations in dietary intake and intestinal motility may be among the potential mechanisms linking temperature and intussusception.
Our study has several limitations. First, we used daily temperature data from fixed observatories as a proxy for individual exposure, which may introduce non-differential misclassification bias. However, this bias would likely pull the results toward the null, potentially underestimating the true association. Second, there is a possibility of non-differential misclassification in the outcome. Given that this misclassification is unlikely to be related to weather conditions, it would similarly bias the results toward the null, leading to underestimation. Third, our findings may be affected by sampling bias, as not all hospitals in Japan participate in the DPC system. Nonetheless, we believe our estimates are robust, given that DPC hospitals represent more than half of all acute-care beds in the country.24 Fourth, while most cases of intussusception in children under 5 years of age are primary (i.e., idiopathic), with secondary cases accounting for only 1–4%,2,3 it is still possible that both primary and secondary cases are included among the hospitalized patients. However, the mechanisms linking high temperatures to intussusception—such as alterations in dietary intake and intestinal motility during warmer temperatures12,13,14,15—may also affect those with secondary causes by further increasing their risk of developing intussusception. Lastly, as this is an observational study, our findings do not imply causality.
Our study may have implications for public health. First, while abdominal pain, vomiting, and bloody stools are the classic triad of symptoms, not all children present with these signs and instead may exhibit nonspecific symptoms, making diagnosis challenging.2 However, if diagnosis is delayed beyond 48 h, the risk of complications and mortality rises.7 Therefore, early diagnosis and treatment are essential. Based on our findings, both caregivers and healthcare providers should be aware of a potential increase in pediatric intussusception cases during warmer days and ensure that children suspected of having intussusception receive appropriate medical attention. This need may become even more critical as climate change results in more frequent and severe heat events. Finally, the findings from this study provide additional support for climate change adaptation strategies, such as reducing heat exposure during heatwaves, which could help lower the risk of intussusception in children.
In conclusion, this study found that higher daily mean temperatures were associated with an increased risk of hospitalization for intussusception. Future research should clarify the mechanisms of the association between higher daily mean temperatures and the increased risk of hospitalization for intussusception.
Data availability
Meteorological data are available from the Japan Meteorological Agency (JMA) website.26 The hospitalization data cannot be made available due to confidentiality restrictions.
References
Feng, Y., Zhou, H., Shu, Q. & Li, H. Association of Meteorological Factors with Paediatric Intussusception in Hangzhou: An 8-Year Retrospective Cohort Study. BMJ Open 12, e064967 (2022).
Ito, Y. et al. Japanese Guidelines for the Management of Intussusception in Children, 2011. Pediatr. Int. 54, 948–958 (2012).
Takeuchi, M. et al. Intussusception among Japanese Children: An Epidemiologic Study Using an Administrative Database. BMC Pediatr. 12, 36 (2012).
Tang, X. B., Hu, D. Y., Mu, X. Q. & Bai, Y. Z. Association of Air Temperature with Pediatric Intussusception in Northeastern China: A 10-Year Retrospective Study. Am. J. Emerg. Med. 42, 211–216 (2021).
Das, M. K. Association of Meteorological Parameters with Intussusception in Children Aged under 2 Years: Results from a Multisite Bidirectional Surveillance over 7 Years in India. BMJ Open 11, e043687 (2021).
Chen, S. C. et al. Epidemiology of Childhood Intussusception and Determinants of Recurrence and Operation: Analysis of National Health Insurance Data between 1998 and 2007 in Taiwan. Pediatr. Neonatol. 51, 285–291 (2010).
Jo, S. et al. Characteristics of Intussusception among Children in Korea: A Nationwide Epidemiological Study. BMC Pediatr. 19, 211 (2019).
Buettcher, M., Baer, G., Bonhoeffer, J., Schaad, U. B. & Heininger, U. Three-Year Surveillance of Intussusception in Children in Switzerland. Pediatrics 120, 473–480 (2007).
Sáez-Llorens, X. et al. A Multi-Country Study of Intussusception in Children under 2 Years of Age in Latin America: Analysis of Prospective Surveillance Data. BMC Gastroenterol. 13, 95 (2013).
Nakagomi, T., Takahashi, Y., Arisawa, K. & Nakagomi, O. A High Incidence of Intussusception in Japan as Studied in a Sentinel Hospital over a 25-Year Period (1978-2002). Epidemiol. Infect. 134, 57–61 (2006).
Guo, W. L., Zhang, S. F., Li, J. E. & Wang, J. Association of Meteorological Factors with Pediatric Intussusception in Subtropical China: A 5-Year Analysis. PLoS One 9, e90521 (2014).
Nissan, A. et al. The Contribution of Inflammatory Mediators and Nitric Oxide to Lipopolysaccharide-Induced Intussusception in Mice. J. Surg. Res. 69, 205–207 (1997).
Cunnane, S. C. & Bloom, S. R. Intussusception in the Syrian Golden Hamster. Br. J. Nutr. 63, 231–237 (1990).
Aydin, E., Beşer, O. F., Ozek, E., Sazak, S. & Duras, E. Is There a Causal Relationship between Intussusception and Food Allergy? Children (Basel) 4, 89 (2017).
Takeuchi, M., Oda, Y. & Suzuki, I. Intussusception Secondary to Anaphylactic Reaction to Salmon Roe (Ikura). Pediatr. Int. 55, 649–651 (2013).
IPCC. Summary for Policymakers. In Global Warming of 1.5°C. An Ipcc Special Report on the Impacts of Global Warming of 1.5°C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty (eds Masson-Delmotte, V. et al.) 3–24 (Cambridge University Press, Cambridge, Uk and New York, NY, USA, 2018). https://doi.org/10.1017/9781009157940.001.
Terada, S., Nishimura, H., Miyasaka, N. & Fujiwara, T. Ambient Temperature and Preterm Birth: A Case-Crossover Study. Bjog 131, 632–640 (2024).
Nishimura, H., Nawa, N., Ogawa, T., Fushimi, K. & Fujiwara, T. Association of Ambient Temperature and Sun Exposure with Hip Fractures in Japan: A Time-Series Analysis Using Nationwide Inpatient Database. Sci. Total Environ. 807, 150774 (2022).
Miyamura, K., Nawa, N., Nishimura, H., Fushimi, K. & Fujiwara, T. Association between Heat Exposure and Hospitalization for Diabetic Ketoacidosis, Hyperosmolar Hyperglycemic State, and Hypoglycemia in Japan. Environ. Int. 167, 107410 (2022).
Nawa, N., Nishimura, H., Fushimi, K. & Fujiwara, T. Association between Heat Exposure and Kawasaki Disease: A Time-Stratified Case-Crossover Study. Environ. Res. 263, 120231 (2024).
Levy, D., Lumley, T., Sheppard, L., Kaufman, J. & Checkoway, H. Referent Selection in Case-Crossover Analyses of Acute Health Effects of Air Pollution. Epidemiology 12, 186–192 (2001).
Armstrong, B. G., Gasparrini, A. & Tobias, A. Conditional Poisson Models: A Flexible Alternative to Conditional Logistic Case Cross-over Analysis. BMC Med. Res. Methodol. 14, 1–6 (2014).
Hayashida, K., Murakami, G., Matsuda, S. & Fushimi, K. History and Profile of Diagnosis Procedure Combination (Dpc): Development of a Real Data Collection System for Acute Inpatient Care in Japan. J. Epidemiol. 31, 1–11 (2021).
Ministry of Health, Labour and Welfare, Japan. Estimated Size of Hospitals Subject to Dpc and Hospitals Preparing for Dpc (April 1, 2023), https://www.mhlw.go.jp/content/12404000/001089926.pdf (2023).
Vaidyanathan, A. et al. Assessment of Extreme Heat and Hospitalizations to Inform Early Warning Systems. Proc. Natl Acad. Sci. USA 116, 5420–5427 (2019).
Japan Meteorological Agency. Historical Weather Data (in Japanese), https://www.data.jma.go.jp/gmd/risk/obsdl/index.php (2023).
Japan Meteorological Agency. Terms Used in Weather Forecasting, Etc. (in Japanese), https://www.jma.go.jp/jma/kishou/know/yougo_hp/kion.html (2023).
Maclure, M. The Case-Crossover Design: A Method for Studying Transient Effects on the Risk of Acute Events. Am. J. Epidemiol. 133, 144–153 (1991).
Gasparrini, A., Armstrong, B. & Kenward, M. G. Distributed Lag Non‐Linear Models. Stat. Med. 29, 2224–2234 (2010).
Gasparrini, A. & Armstrong, B. Reducing and Meta-Analysing Estimates from Distributed Lag Non-Linear Models. BMC Med. Res. Methodol. 13, 1 (2013).
Jiang, Y. et al. Non-Optimum Temperature Increases Risk and Burden of Acute Myocardial Infarction Onset: A Nationwide Case-Crossover Study at Hourly Level in 324 Chinese Cities. EClinicalMedicine 50, 101501 (2022).
Fukuda, Y. et al. Characteristics of Intussusception among Children in Hokkaido, Japan, During the Pre- and Post-Rotavirus Vaccine Eras (2007–2016). Acta Paediatr. 112, 868–875 (2023).
Nguyen, S. M. T. et al. Mechanisms Governing Anaphylaxis: Inflammatory Cells, Mediators, Endothelial Gap Junctions and Beyond. Int. J. Mol. Sci. 22, 7785 (2021).
Bertaccini, G., Morini, G. & Coruzzi, G. Different Mechanisms Are Responsible for the Contractile Effects of Histaminergic Compounds on Isolated Intestinal Smooth Muscle Cells. J. Physiol.-Paris 91, 199–202 (1997).
Acknowledgements
During the preparation of this work, the authors used ChatGPT to improve the readability and language of the manuscript. After utilizing this tool, the authors reviewed and edited the content as necessary and take full responsibility for the content of the published article.
Funding
This work was supported by Science and Technology Research Partnership for Sustainable Development (SATREPS) in collaboration between Japan Science and Technology Agency (JST, JPMJSA2402) and Japan International Cooperation Agency (JICA). The funders had no involvement in the research or the preparation of the paper, including the study design, data collection, analysis, interpretation, writing of the paper, or the decision to submit the paper for publication.
Author information
Authors and Affiliations
Contributions
N.N., H.N., and T.F. conceptualized the study. All authors contributed to data curation. N.N. performed the formal analysis, interpreted the results, and wrote the first draft of the manuscript. All authors critically reviewed and revised the first draft. All authors approved the final draft of the manuscript. Additionally, all authors had full access to all the data in the study and bear final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet the authorship criteria and that no one meeting the criteria has been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent statement
This study was approved by the Medical Research Ethics Committee at Tokyo Medical and Dental University (Institute of Science Tokyo). Patient consent was not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nawa, N., Nishimura, H., Fushimi, K. et al. Association between heat exposure and intussusception in children in Japan from 2011 to 2022. Pediatr Res 98, 871–875 (2025). https://doi.org/10.1038/s41390-025-03930-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41390-025-03930-4
This article is cited by
-
Heat exposure impacts the incidence of intussusception in children
Pediatric Research (2025)