Abstract
Background
Unplanned extubation (UE) is the fourth most common adverse event in neonatal intensive care units (NICUs) and remains a significant global challenge. Standardizing endotracheal tube (ETT) maintenance could reduce UE rates to 0.5–1.0 events per 100 non-tracheostomy ventilation days. This quality improvement (QI) project aimed to reduce the UE rate to below 1.0 event per 100 non-tracheostomy ventilation days within 12 months.
Methods
Using a QI methodology, we conducted four Plan–Do–Study–Act (PDSA) cycles, including frequent ETT securement evaluations, ETT stabilization during procedures, audits of chest radiographs, and the use of a silk tie for ETT reinforcement. Statistical process control charts monitored progress.
Results
Baseline UE rate was 1.73 events per 100 non-tracheostomy ventilation days. The first three PDSA cycles (January 2019–May 2020) produced a non-significant signal for reduced UE to 0.88. After introducing the silk suture tie in PDSA cycle 4, the rate significantly declined to 0.58 and was sustained from October 2020 to December 2021. A further special cause variation occurred from February to December 2022 with UE reduction to 0.06.
Conclusions
A multidisciplinary approach and silk suture tie intervention significantly reduced and sustained one of the lowest reported UE rates, enhancing ETT securement and patient safety.
Impact
-
Unplanned extubation (UE) events are not uncommon in the neonatal intensive care unit.
-
This project demonstrates that the lowest reported UE rates in neonatal ICUs are possible without incurring additional costs or requiring new securement devices.
-
The success of this project underscores the importance of standardizing care, reducing variability, and fostering a multidisciplinary, collaborative approach.
-
The silk tie enhancement for ETT stabilization offers a practical, scalable solution to prevent UEs and improve neonatal care.
Similar content being viewed by others
Introduction
Problem description
Infants admitted to neonatal intensive care units (NICUs) often require ventilator support as a life-saving intervention. However, unplanned extubation (UE), necessitating reintubation, is the fourth most common adverse event (AE) among NICU patients.1
Available knowledge
The literature offers various definitions of UE, leading to inconsistencies in its characterization and challenges in comparing and generalizing interventions across institutions.2,3,4,5 Epidemiologic studies have identified multiple risk factors for UE, including an infant’s chronological age, procedural and transport activities, and the type of securement device used.6 For example, anatomical and developmental factors, such as the small size of the neonatal trachea (2–6 cm), increase the risk of endotracheal tube (ETT) dislodgment during routine care or procedures.7 Additionally, the use of short, uncuffed ETTs exacerbates instability compared to longer, cuffed ETTs.
UE is associated with serious complications, including severe cardiorespiratory events, increased oxygen requirements, post-reintubation sepsis, prolonged NICU stays, higher healthcare costs, and even death prior to discharge.8,9,10 As a result, UE has been nationally recognized as a preventable hospital-acquired condition. In recent years, standardized bundles and validated practices have enabled a few institutions to achieve UE rates below 1.0 per 100 non-tracheostomy ventilation days.11,12,13,14
Specific aims
This quality improvement (QI) project aimed to reduce UE events as part of the institutional “zero harm” patient safety initiative. The multidisciplinary Neonatal Quality Council (NQC) was tasked with reducing the baseline UE rate of 1.7 per 100 non-tracheostomy ventilation days to below 1.0 event per 100 non-tracheostomy ventilation days within 12 months.
Methods
Context
Cleveland Clinic Children’s NICU provides services across three locations, comprising two Level III units and one Level IV unit, with a total capacity of 87 beds. The Obstetrics department facilitates over 10,000 deliveries annually, resulting in approximately 1300 NICU admissions, including an average of 140 very-low-birth-weight infants (<1500 g) each year. All infants are inborn with <10% transport rate between NICUs within the system. Care across all three NICUs is delivered by the same team of caregivers, following standardized guidelines. Importantly, the guidelines for intubation, mechanical ventilation, and extubation remained unchanged throughout the duration of this project.
Definitions
At our institution, UE is defined as the unintentional dislodgement of an ETT from the trachea. This definition aligns with the operational criteria established by the Children’s Hospitals’ Solutions for Patient Safety (SPS) network.15
Data collection
Data on non-tracheostomy ventilation days, UE events, and reintubations were extracted from electronic medical records by respiratory team supervisors and stored in a secure institutional drive using Excel spreadsheets.
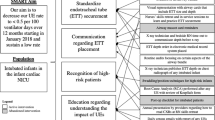
Interventions
The NQC conducted a cause-effect analysis to identify key drivers of UE and developed a UE preventive strategy (Fig. 1). Plan–Do–Study–Act (PDSA) cycles were utilized to implement interventions, with each subsequent cycle informed by the data and findings of the previous cycle.
-
PDSA Cycle 1—January 2019: Focused on evaluating ETT tape position and securement during shift changes. Respiratory therapists emphasized precautions during ETT retaping, requiring the presence of two licensed caregivers: one to stabilize the infant’s head and maintain swaddling and the other to handle the ETT securement.
-
PDSA Cycle 2—August 2019: Targeted high-risk situations such as bedside imaging, invasive procedures, kangaroo care transfers, weighing, and bed changes. These activities required the presence of two licensed caregivers.
-
PDSA Cycle 3—May 2020: Introduced random chest radiograph (CXR) audits and an apparent cause analysis (ACA) evaluation within 12 h of each UE event across all NICU sites. ACA form is provided in the Supplemental File.
-
PDSA Cycle 4—October 2020: Addressed ETT slippage through a modification of the securement method using a silk suture tie in the chevron loop to enhance ETT stability. Routine bedside care included checking tape integrity, but loose tape around the ETT, not easily visible, necessitated this intervention. Illustrations of the silk tie securement method are shown in Fig. 2. Details of this securement method is provided in the Supplemental File. Before implementation, an instructional video was created and made available to staff. All respiratory therapists were required to demonstrate proficiency in applying the silk tie on a mannequin before participating in the actual implementation. Silk tie training was also incorporated into the orientation materials for new respiratory therapists, and a refresher simulation was provided to existing therapists 1 year after implementation. Although physicians and nurses were not required to perform the silk tie procedure, they received orientation on the technique to ensure they could assist respiratory therapists when needed.
The project emphasized a “team buy-in” strategy through active engagement at all levels. To foster open communication, the NQC held staff meetings before the project launch and ahead of each PDSA cycle. Performance metrics were reviewed quarterly, and lessons from UE incidents were shared as “safety stories” during staff meetings. Regular discussions on ETT positioning during grand rounds and other educational activities further reinforced shared ownership of the project.
The QI airway team met every 2 weeks, with leadership receiving monthly updates on the UE rate. Staff were updated on UE rates and engaged in discussions at least quarterly or whenever changes were planned. NICU huddles were conducted after each event to review and address concerns. Before each PDSA cycle, staff were informed during a meeting, and any required training was provided to the involved team members.
Measures
The primary outcome measure was the UE rate, defined as the number of UE events per 100 non-tracheostomy ventilation days.15 The process measures included (a) twice-daily assessment of ETT position and securement by two bedside nurses during shift changes. Respiratory therapists independently performed their checks and corrections each shift; (b) adherence to post-UE event evaluations and completion of the ACA form; and (c) monthly audits of 10 CXRs conducted by respiratory supervisors to ensure proper ETT positioning. Suboptimal CXRs, improper ETT positioning, or missing depth annotations prompted immediate notification of the attending neonatologist for corrective action.
Balancing measures
These included self-reported difficulties during ETT tape removal, skin integrity after tape removal, and delays in emergent ETT removal due to the use of silk suture ties.
ACA process
The ACA form, aligned with the SPS reporting format, was implemented in 2020.16 It documented AEs related to UE, including arrhythmias, blood pressure changes requiring intervention, increased respiratory support, bradycardia (heart rate <60 bpm), chest compressions, administration of code medications, and delays in ETT removal due to the silk suture tie. Following each UE event, a post-event huddle was conducted within 12 h, during which the ACA form was completed and submitted to the respiratory supervisor. The supervisor presented a summary of findings, contributing factors, and proposed action plans to the NQC-NICU Airway Management Committee. These forms were securely stored, and a Pareto analysis of all UE events in 2020 informed subsequent interventions (Fig. 3).
The details of tube securement are provided in the Supplemental File.
Analysis
The Continuous Improvement Institute at the enterprise dedicated an expert staff (D.K.) who performed all analyses. Analyses were performed using Excel with QI Macros add-on (QI Macros for Excel. Version 2025.01. KDT Enterprises, Inc., 2025; https://www.qimacros.com) (Fig. 4). Special cause variations were identified using Nelson’s rules and used to assess process stability. The U-chart, plotted monthly, provided insights into variability, with favorable special cause variations indicating process improvement.
The X axis denotes the dates during this QI project, scaled monthly. The Y axis represents unplanned extubation events per 100 non-tracheostomy ventilation days. The green dashed line represents the center line (CL), and the red fine dotted line represents the upper control limit (UCL), whereas the green solid line represents the target goal for the QI project (<1 event per 100 ventilation days). UE unplanned extubation, PDSA plan, do, study, act.
Results
The characteristics of the NICU population during this period are detailed in Table 1. The baseline UE rate in the years 2017–2018—preceding the project—was 1.73 per 100 non-tracheostomy ventilator days. Following the first three PDSA cycles, the UE rate decreased to 0.88 events per 100 ventilator days; however, this reduction represented a common cause variation, as it did not fulfill the control chart criterion of 8 consecutive points below the center line, and thus did not indicate a statistically significant improvement.
Following the implementation of interventions in PDSA cycle 3 and PDSA cycle 4 (the silk tie), the UE rate further decreased to 0.58 per 100 non-tracheostomy ventilator days. This reduction was considered significant, as the rate remained consistently below the center line for 8 consecutive months.
During the sustainment phase following the four PDSA cycles, the UE rate dropped to zero for 9 consecutive months, with an overall rate of 0.06 per 100 non-tracheostomy ventilator days throughout 2022 (Fig. 4). Although no new formal intervention was introduced at the time of the second center line shift, the improvement was attributed to the cumulative impact of earlier interventions, as well as increased staff experience and proficiency with the silk tie securing method. As familiarity with the technique improved, greater consistency in ETT care likely contributed to the observed special cause variation and sustained reduction in UE rates. Following the completion of this QI project by the end of 2022, UE rate remained within range in 2023, 2024, and 2025 (year to date) with UE rates of 0.11, 0.23, and zero events per 100 non-tracheostomy ventilation days, respectively.
Notably, prior to PDSA cycle 4 in 2020, all UE events were attributed to loose tape. After implementing the silk tie intervention, only two events related to loose tape were recorded—one in 2021 and one in 2022.
Adherence to post-UE event evaluations and completion of the ACA form consistently exceeded 80%, as did compliance with obtaining optimal CXRs for ETT positioning. Importantly, there were no reported delays in ETT removal due to the silk suture tie throughout the intervention period.
Additionally, no other adverse outcomes or delays in resuscitation were attributed to the use of the silk suture tie. No changes in respiratory care unrelated to the interventions were noted or reported during this time that could have influenced the observed outcomes.
With approximately 2000 non-tracheostomy ventilation days annually, this QI initiative reduced UEs from 36 to 1 event, preventing an estimated 35 events per year.
Discussion
Summary and interpretation
This QI project achieved the lowest reported UE rates in neonates, sustained for over 2 years. Implementation of four PDSA cycles resulted in eight consecutive points below the mean UE rate, with a significant reduction from 1.725 to 0.58 per 100 ventilator days. The subsequent reduction to 0.06 in February 2022 further validated the sustainability of these interventions. Previous QI projects reported UE rates as low as 0.99 to 0.68 per 100 ventilator days,11,12,13,14 highlighting the impact of our approach in achieving even greater reductions.
Critical to the project’s success was adherence to QI principles, including fostering team buy-in and active engagement at all levels within the division. Establishing a focused task force, engaging leadership, and adopting a standardized operational definition of UE were foundational steps. Data transparency and regular feedback to frontline caregivers through electronic visual boards, division meetings, regional operational meetings, and huddles effectively motivated staff. Empowering the respiratory team to implement the silk tie intervention in the PDSA cycle 4 further enhanced engagement. Unlike previous studies that required suturing through the ETT wall for stabilization,17,18 the current method of securing the ETT with a silk tie avoided the need for needles, streamlining the intervention while maintaining effectiveness. Although a learning curve was present, ongoing education from respiratory supervisors and transparent feedback facilitated widespread adoption.
This QI initiative was well-received by staff, with progress and outcomes attributed to the project fostering enthusiasm across teams. The success of the intervention even motivated colleagues in pediatric critical care units to adopt the approach. It is important to note that the interventions in the four PDSA cycles were not presented as a bundle, as they lacked strong evidence-based literature to support such a framework. Respiratory therapists and bedside nurses were required to document the ETT position and assess securement quality during routine handoff at shift changes. These new practice guidelines were adopted by both nursing and respiratory therapy teams, with full compliance expected. This practice change played a key role in the project’s success. In recent years, standardization of care during high-risk situations and accurate ETT placement have been associated with reduced UE rates.11,12,13,14 During PDSA cycles 1–3, adopting standardized practices reduced the UE rate to less than 1 per 100 non-tracheostomy ventilation days by early 2020. This reproducible effect stemmed from minimizing variations in patient care and eliminating special cause variations, creating a highly reliable and stable system. The stability allowed for precise identification of the most significant contributors to UE, leading to the PDSA cycle 4 intervention that addressed ETT slippage through the wet chevron loop. Standardizing the definition of UE events was also critical for comparing institutional outcomes to benchmarks. At our institution, the UE definition aligned with that used for the SPS Network, ensuring consistency in reporting and data accuracy.
UEs and subsequent reintubations are associated with AEs, including bradycardia, oxygen desaturation, airway trauma, prolonged ventilator support, and extended hospital stays. Serious events such as chest compressions, epinephrine administration, or even death have been reported.8,19 By reducing the UE rate to less than 1 per 100 ventilator days, as seen in other institutions,20,21,22 this project minimized these risks. Further reductions to an average UE rate of 0.06 in 2022 highlight the silk tie intervention as a positive special cause variation, enabling a stable and reliable system that is ripe for future improvements.
Addressing the “rising tide phenomenon” is important for interpreting results. System-wide improvements often occur once healthcare teams recognize an issue, narrowing the observed differences between control and intervention groups in prospective studies.23 Acknowledging this phenomenon is essential to accurately interpret outcomes and avoid overgeneralizing findings to other healthcare systems where such trends may not exist. In the context of this project, the improvement in the UE rate was not immediate. Significant improvement occurred after PDSA cycle 4, making the influence of the rising tide phenomenon unlikely.
Strengths and limitations
The silk tie intervention was easily adopted following a single demonstration on a mannequin in each NICU. This process change did not require additional securement devices or costs, making it feasible for low-resource settings, including low- and middle-income countries. Additional benefits included reduced exposure to unnecessary reintubations, decreased facial skin compromise from repetitive retaping, and improved caregiver and parental satisfaction, as reported anecdotally during staff meetings. The silk tie was not associated with skin breakdown, as the tie is positioned between two layers of tape without direct contact with the skin. When the decision is made to remove the tube, the silk tie does not cause delays since the entire tube, tape, and silk tie are removed together. However, if retaping the tube is required, the process can be time-consuming. In such cases, two caregivers are involved: one carefully removes the superficial layer of tape, cuts the silk tie, removes the deep layer of tape, adjusts the tube position, and then retapes the tube securely.
However, there are limitations to this initiative. Standardized data on pain scores, ETT taping-related skin breakdown, and caregiver or parental satisfaction were not collected. While the intervention was implemented in three NICUs with different respiratory therapists and nursing teams, all belonged to a single enterprise with one physicians’ group, limiting the generalizability of these findings. Additionally, the sustained reduction in UE rates to 0.06 in 2022 may partly reflect growing experience and skill with the silk tie technique, though no objective measures of this were captured. Greater involvement of parents and families in the NICU could have provided valuable feedback and enhanced the initiative.
Conclusions
This QI project demonstrates that achieving the lowest reported UE rates in neonatal ICUs is possible without incurring additional costs or requiring new securement devices. The success of this project underscores the importance of standardizing care, reducing variability, and fostering a multidisciplinary, collaborative approach. Once ETT securement procedures and UE definitions are standardized, additional interventions can be introduced to further optimize outcomes. The silk tie enhancement for ETT stabilization emerged as the most impactful intervention in reducing UEs, supported by process improvements such as CXR audits and ACA implementation. While the earlier steps contributed to optimizing care practices, sustained low UE rates have been primarily attributed to interventions introduced in PDSA cycles 3 and 4.
Data availability
The dataset generated during and/or analyzed during the current study is available from the corresponding author on reasonable request.
References
Sharek, P. J. et al. Adverse events in the neonatal intensive care unit: development, testing, and findings of an NICU-focused trigger tool to identify harm in North American NICUs. Pediatrics 118, 1332–1340 (2006).
Loughead, J. L. et al. Reducing accidental extubation in neonates. Jt. Comm. J. Qual. Patient Saf. 34, 164–170 (2008).
Kandil, S. B. et al. Reducing unplanned extubations across a children’s hospital using quality improvement methods. Pediatr. Qual. Saf. 3, e114 (2018).
Meyers, J. M., Pinheiro, J. & Nelson, M. U. Unplanned extubation in NICU patients: are we speaking the same language? J. Perinatol. 35, 676–677 (2015).
Ndakor, S. M. et al. Wide variation in unplanned extubation rates related to differences in operational definitions. J. Patient Saf. 18, e92–e96 (2020).
Hatch, L. D. et al. Effect of anatomical and developmental factors on the risk of unplanned extubation in critically ill newborns. Am. J. Perinatol. 34, 1234–1240 (2017).
Cerone, J. B. & Pinheiro, J. M. B. Tracheal length measurement in intubated neonates to guide the design and use of endotracheal tube glottic depth markings. Children 9, 169 (2022).
Klugman, D. et al. Acute harm: unplanned extubations and cardiopulmonary resuscitation in children and neonates. Intensive Care Med. 39, 1333–1334 (2013).
Roddy, D. J., Spaeder, M. C., Pastor, W., Stockwell, D. C. & Klugman, D. Unplanned extubations in children: impact on hospital cost and length of stay. Pediatr. Crit. Care Med. 16, 572–575 (2015).
Kambestad, K. K. et al. The adverse impact of unplanned extubation in a cohort of critically ill neonates. Respir. Care 64, 1500–1507 (2019).
Galiote, J. P. et al. Reduction in unintended extubations in a level IV neonatal intensive care unit. Pediatrics 143, e20180897 (2019).
Morris, H. F. et al. Decreasing unplanned extubation in the neonatal ICU with a focus on endotracheal tube tip position. Respir. Care 65, 1648–1654 (2020).
Klugman, D. et al. Assessment of an unplanned extubation bundle to reduce unplanned extubations in critically ill neonates, infants, and children. JAMA Pediatr. 174, e200268 (2020).
Mahaseth, M. et al. Reducing unplanned extubations in a level IV neonatal intensive care unit: the elusive benchmark. Pediatr. Qual. Saf. 6, e337 (2020).
Children’s Hospitals’ Solutions for Patient Safety. Unplanned extubations: operational definition & bundle. https://www.solutionsforpatientsafety.org/unplannedextubations (2024).
Parikh, K. et al. Apparent cause analysis: a safety tool. Pediatrics 145, e20191819 (2020).
Gregory, G. A. Respiratory care of newborn infants. Pediatr. Clin. North Am. 19, 311–324 (1972).
Hipolito, R. B., Milstein, J. M., Sherman, J. & Sherman, M. P. Neonatal endotracheal tubes and prevention of bronchial intubation. J. Pediatr. Congenital Disord. 2, 101 (2015).
Pavlek, L. R. et al. Short-term complications and long-term morbidities associated with repeated unplanned extubations. J. Perinatol. 41, 562–570 (2021).
da Silva, P. S., Reis, M. E., Aguiar, V. E. & Fonseca, M. C. Unplanned extubation in the neonatal ICU: a systematic review, critical appraisal, and evidence-based recommendations. Respir. Care 58, 1237–1245 (2013).
Cosentino, C. et al. Unplanned extubations in intensive care unit: evidences for risk factors. A literature review. Acta Biomed. 88, 55–65 (2017).
Nair, V. & Smith, H. Phased quality improvement interventions in reducing unplanned extubation in the neonatal ICU. Respir. Care 65, 1511–1518 (2020).
Chen, Y. F., Hemming, K., Stevens, A. J. & Lilford, R. J. Secular trends and evaluation of complex interventions: the rising tide phenomenon. BMJ Qual. Saf. 25, 303–310 (2016).
Acknowledgements
The authors would like to acknowledge the cooperation of the nursing, respiratory, and medical staff in all three NICU locations as well as leadership support. The authors report no involvement in the reported QI project by any sponsor or funding organization.
Author information
Authors and Affiliations
Contributions
T.H. Nesterenko—conceptualized the manuscript, led UE prevention project; monitored, analyzed, visualized and interpreted the data; wrote original draft of the manuscript, reviewed it and edited it. F. Saker—co-authored manuscript, co-led UE prevention project, reviewed the manuscript and edited it. D. Kubiak—analyzed and interpreted the data, reviewed the manuscript. and edited it. J. Dickson, A.L. Sheppard, N. Saliba, and K.L. Fedor—conducted the QI project, reviewed the manuscript, and edited it. M.A. Mohamed—reviewed the manuscript and edited it. H. Aly—conceptualized silk suture tie technique, reviewed the manuscript, and edited it.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical considerations
The NQC holds active approval for de-identified data collection related to QI projects. In accordance with institutional guidelines, this QI initiative did not require a new institutional review board (IRB) application.
Consent statement
All parents were duly informed about the intubation process, endotracheal tube securement, and preventive measures against unplanned extubation within the standard informed consent procedure for intubation. Emergency intubation, including those in the delivery room, did not require procedure consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nesterenko, T.H., Saker, F., Kubiak, D. et al. Prevention of unplanned extubation in neonates with silk tie securement. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04168-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04168-w