Abstract
Background
Explore longer-term psychosocial adaptation to congenital heart disease among families of children with dextro-Transposition of the Great Arteries (d-TGA).
Methods
In this qualitative study, semi-structured interviews were conducted for 16 families (16 mothers, 12 fathers, 9 siblings) and analyzed using an inductive thematic approach.
Results
Key qualitative themes included parents reflecting “back then” when 1) navigating hospital and healthcare experiences, 2) challenges to psychosocial wellbeing and family functioning, and 3) coping and support needs were greatest. Parents described 4) key transitions and defining moments, and 5) feeling “lucky” and grateful for contemporary cardiac care and when compared to families of children with univentricular conditions and valuing a “normal” life. Furthermore, 6) the surgical scar served as a constant reminder of past experiences and 7) uncertainty about the role of the cardiac condition in their child’s development persisted for some parents. Key themes among siblings included 1) having a “normal” family life, 2) positive and negative aspects of the sibling relationship, and 3) limitations in understanding their sibling’s cardiac condition.
Conclusion
Families of children with d-TGA value “normal” family lives years after surgical intervention. To improve care and support, a focus on positive psychosocial adaptation, including individual and family resilience, parental perceptions of surgical scars, and self-reported sibling experiences, is required.
Impact
-
Families of children with complex congenital heart disease are at risk for psychosocial and family functioning difficulties. Research has focused on early experiences of diagnosis and hospitalization, with limited evidence of longer-term experiences.
-
Using qualitative methodology, we explored the lived experiences of families of children with dextro-Transposition of the Great Arteries concerning longer-term psychosocial adaptation to congenital heart disease.
-
Despite ongoing illness uncertainty and reminders of previous medical experiences, parents and siblings of children with dextro-Transposition of the Great Arteries predominantly described positive adaptation and living and valuing their “normal” family lives years after arterial switch operation.
Similar content being viewed by others
Introduction
Infants with dextro-Transposition of the Great Arteries (d-TGA), a complex cyanotic congenital heart disease (CHD), require early open-heart surgery. Long-term survival is high, and freedom from re-operation after arterial switch operation (ASO) is common.1 Nonetheless, lifelong specialized cardiac care is required, with a heightened risk for neurodevelopmental and psychological difficulties2,3,4 and subsequent increased use of developmental services.5,6,7,8
While longer-term outcomes of children with d-TGA have been documented, fewer studies have focused on their families’ experiences.9,10 Increased risk of psychological distress has been reported in parents of children with complex CHD,11,12,13 with both persisting14,15 and decreasing levels10,16,17,18 over time, as well as both negatively impacted family functioning19,20 and greater family cohesion.21,22 In parents of children with d-TGA, significantly less parenting stress and more social support than normative samples have been reported at both 1 and 4 years of age.10 Compared with families of young children with hypoplastic left heart syndrome (HLHS),9 parents of children with d-TGA reported lower negative family impact, with increased closeness because of their child’s medical experiences, reported by 96% of families.
Qualitative research enables the exploration of participants’ lived experiences and perspectives.23 To date, no qualitative studies have focused specifically on the experiences of families of children with d-TGA. With a predominantly homogeneous clinical course, qualitative exploration provides the opportunity for an improved understanding of the experiences of families of children with complex CHD.24,25 Furthermore, the number of qualitative studies inclusive of mothers and fathers beyond early hospitalization,26 and siblings overall, is very limited.27 Thus, our study aimed to explore the longer-term experiences of parents and siblings of children with d-TGA using a qualitative methodology, and informed by a family adaptation to chronic illness conceptual model.28
Methods
Participants
A contemporary cohort of families of all living children with d-TGA with Intact Ventricular Septum or Ventricular Septal Defect born between 1 January 2008 and 31 December 2017 who underwent ASO at the Queensland Paediatric Cardiac Service was established. Exclusion criteria were families of children with complex d-TGA unsuitable for ASO, with chromosomal, syndromic, or major non-cardiac comorbidities (excluding neurodevelopmental disorders) or born <37 weeks gestation; families with insufficient English language skills to participate without an interpreter; and siblings younger than the child with d-TGA or under age 8 years. A matrix was developed to facilitate purposive sampling with representation across three child age groupings, time of diagnosis (prenatal vs. postnatal), and family residential location (urban vs. regional).
Procedures
This study was informed by the Consolidated Criteria for Reporting Qualitative Research guideline.29 Ethics approvals were obtained from Children’s Health Queensland (HREC/19/QCHQ/56798) and The University of Queensland (2019/HE002627) Human Research Ethics Committees. A semi-structured interview guide (Supplement 1) was developed by the multidisciplinary research team (psychology, pediatric cardiology, nursing), and refined based on piloting with parents (n = 2) of children with a cardiac and non-cardiac chronic condition.
Study information was mailed to families to consider their interest in participation. Families were contacted after two weeks to address questions and schedule interviews, either face-to-face in the family home or research center, or virtually via Zoom. Written informed consent was obtained from parents and adult sibling participants, and child assent and parental consent were obtained for sibling participants <18 years.
Interviews took place between February and June 2020. All interviews were conducted individually by the first author (advanced practice pediatric cardiac nurse; female) and audio-recorded with permission. The first author’s dual role as researcher and clinician (including previous care of some participants) was explicitly discussed with families to promote clear boundaries and enable “data collection vs. therapeutic interaction”.30 Three early interviews (five participants) were attended by another author with expertise in qualitative research methodology (SL; male). To support wellbeing, time was spent with participants post-interview, with additional follow-up after approximately one month.
Data analysis
Our sample size was informed by recommendations concerning thematic analysis, informational saturation, and sampling methodologies.31,32 Informed by Miles et al.33 an inductive and iterative approach to qualitative data analysis was used. Interview recordings were transcribed verbatim,23 with three parent transcriptions reviewed for accuracy by another author (TC; female). First-cycle codes were created, and codebooks were established, with subsequent second-cycle coding (parent interviews only) to organize codes into early themes. An example of theme development is provided in Supplement 2. One-third (n = 12) of transcripts were coded by two authors (KE, TC) with agreement reached through discussion, and selected early parent interview transcripts (n = 2) were independently reviewed by two additional authors (SL, NK) who are experienced coders. Regular discussions occurred within the research team through all stages of analysis, with records kept. NVivo 12 software (Lumivero, Denver, CO) was used to organize coding, theme development, annotations, and reflexive memos. Microsoft Excel was used to develop matrices/summaries to enable comparisons between family members’ responses across themes.
Results
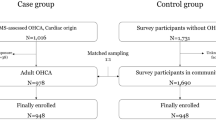
Of the 28 families approached, 16 participated (57% response), with 37 participants (16 mothers, 12 fathers, and 9 siblings) interviewed (see Fig. 1). Clinical and demographic data are shown in Table 1. The mean age of children with d-TGA was 6 ± 3 years, 56% were diagnosed prenatally, and 50% of families lived in regional areas. The mean age of mothers and fathers was 39 ± 7 and 44 ± 7 years, respectively; the mean age of siblings (5 girls, 4 boys) was 13 ± 4 years. The mean interview duration was 46 ± 12 minutes for parents and 15 ± 5 minutes for siblings. While data informing the final key parent themes identified in this study were collected in the first six interviews, all transcripts were coded to ensure maximum variation and to reach informational saturation. Key sibling themes were identified after coding all transcripts, although informational saturation was not reached.
Key parent themes
Figure 2 depicts seven key parent themes and exemplar quotes are shown in Table 2. Exemplar comparisons between responses of family members across themes/codes in two parent-participant families are illustrated in Fig. 3.
Theme 1: Navigating healthcare systems
Parents described challenges navigating healthcare systems from the time of d-TGA diagnosis. Parents of infants diagnosed after birth described experiences of their infant becoming acutely unwell, with sudden separation from them when retrieved to the cardiac center. Parents recalled negative hospitalization experiences, including extended stays due to complications and gaps in physical and emotional care for new mothers in the transition from maternity to cardiac services.
For many parents, attending their child’s annual or biennial follow-up cardiology reviews caused minimal difficulties. Within families, mothers were more likely to experience worry at reviews. Almost half of the families interviewed were accessing developmental services or considering/trying to access assessment or intervention for their child. Of those accessing services, parents from three families identified ongoing concerns and/or additional services needed.
Theme 2: Challenges to wellbeing and family functioning
Irrespective of the d-TGA diagnosis timing, both mothers and fathers described shock, and subsequent fear and devastation. For many, this distress continued throughout hospitalization, especially when witnessing the care of their unwell infant and needing to make difficult decisions about their child’s medical care. Several mothers described feeling vulnerable as new mothers, their grief, and concerns for mental health. Within families, both mothers and fathers reported being concerned about siblings’ needs being met.
Into early childhood and the present day, the decreased impact of CHD on both the individual parent and family in comparison to “back then” was consistently identified. However, some mothers described ongoing personal guilt, worry, and fears, including concerning the potential sudden loss of their child. While most parents felt there were no ongoing negative effects on siblings, both parents in one family described challenges in sibling responses to stressful situations, and both parents in another family described the impact of behavioral challenges of the child with CHD on siblings and broader family life. Despite early relationship/marriage challenges during hospitalization, several parents now described their experiences as strengthening their relationship.
Theme 3: Understanding d-TGA, coping, and support needs
Almost all parents now have an understanding of their child’s heart condition which they describe in varying levels of detail. Regardless of diagnosis timing, clear, simple communication and the use of diagrams were highly effective in helping parents’ understanding. Several parents described the benefits of seeking additional online information and talking to family and friends with a medical background. Cardiology reviews are now a time of reassurance regarding the stability of their child’s condition, with the potential for future re-intervention identified for some.
Parents described their coping with their child’s heart condition as “getting on with” what they needed to do, especially at diagnosis and during hospitalization. Being organized, optimistic, easy-going, and solution-focused were identified as helpful, especially among fathers. Differences in maternal and paternal coping contributed to relationship strain, as well as being complementary and enabling them to function. Where relationships were strained, both mothers and fathers attributed this to the father distancing themselves from the hospital as a way of coping.
Several parents, predominantly mothers, identified the need for psychological support post-hospital discharge, which was not always accessed due to busyness, not feeling ready, or lack of knowledge or availability. A storybook created by one mother to process her experience became a valuable resource for all family members.
The closeness and emotional and practical support of extended family were crucial for families during hospital admission and transition home. Lack of extended family support, through relationship breakdowns or geographical distance, was keenly felt by both mothers and fathers. The importance of close friendships in providing support during hospitalization, as well as in current day-to-day life, was also identified. Some parents also described the positive role of other families affected by CHD and their local community. Formal psychosocial supports offered to parents during their hospital stay were not perceived to be needed by mothers or fathers, especially when well supported by family and friends. Where several parents identified the benefit of formalized peer support and advocacy groups, most did not engage beyond occasional social media access.
Theme 4: Transitions and defining moments
For some parents, reassurance from their child’s cardiac care team at hospital discharge or subsequent visits and reduced frequency of cardiology follow-up were key to moving forward with life. Positive experiences of their child’s development, including reaching milestones, starting school, and sporting achievements, also facilitated knowing that their child was progressing well. Among families that described a shift “back to normal”, the timing of this varied. For example, in one family, both parents felt life went back to normal soon after discharge, while in other families, this did not occur until one or two years post-discharge.
Theme 5: Feeling “lucky” and valuing a “normal” life
Feeling “lucky” regarding their child’s cardiac condition in relation to more complex conditions and modern cardiac care was a shared experience between and within families. Overall, parents identified feeling “lucky” for the place that CHD can hold in their lives and not be at the center of how they live.
Both mothers and fathers predominantly described themselves as a “normal” family, living a “normal” life with busy daily routines. They mostly described close relationships between their child with CHD and siblings, with some challenges due to differing personalities or during the sibling teenage years. Several parents described not seeing their child as having a heart condition and mostly seeing them as progressing as a typical child, with many positive individual qualities. Sibling comparison enabled parents to see similarities as well as developmental and behavioral differences between their children with and without CHD. Early over-protectiveness had eased for most parents, and many described the importance of treating their children just like other children. A few parents across different families described their child as “special” in the context of additional developmental differences, and one due to the cardiac condition.
Parents frequently described deep gratitude for the survival and health of their child, and to be living in Australia, with universal access to healthcare and resources. Many mothers and fathers had a strong awareness of and empathy for families who traveled extensive distances for clinical care, families of children requiring multiple surgeries, and bereaved families. Areas of personal growth, including a greater appreciation for life and compassion towards others, stronger family relationships, and resilience when challenges arise, were also identified between and within families.
Theme 6: Scar as a reminder
Although many parents described not seeing their child as having a heart condition, the surgical scar served as a constant reminder of what they and their child had experienced, as well as their child’s survival and bravery. While the potential for future bullying was identified, the scar was also seen as an opportunity to increase awareness of CHD.
Theme 7: Ongoing illness uncertainty
Some parents voiced ongoing illness uncertainty, including fears about their child’s future health and wellbeing, neurocognitive difficulties, and physical activity limitations. Parents were also aware of the uncertainty of future surgery, with some managing their worries by “dealing with it when it happens”. Within families, worry and anxiety related to ongoing uncertainties, including the need for future surgery, were more likely to be experienced by mothers, although greater worry or overprotectiveness was identified by two fathers.
Sibling themes
Three themes were identified in the siblings’ narratives (see Table 2).
Theme 1: “Normal” family life
Consistent with parents, siblings described busy daily routines, including school/university, time with family and friends, extracurricular activities, and personal interests, contributing to a sense of “normal” life.
Theme 2: Getting along… but they can be annoying
Positive and negative aspects of the sibling relationship were identified, from spending time together and getting along well, to finding them frustrating and annoying, with just one sibling identifying this as a point of difference to other sibling relationships. Several siblings identified enjoying looking after and helping their younger sibling with CHD or feeling empathy when considering their cardiac condition.
Theme 3: Understanding and experiencing my sibling’s CHD
Consistent with their parents, most siblings also saw their sibling with d-TGA as “normal” and no different from other siblings. Differences identified were in the context of the sibling relationship (Theme 2), and the child with CHD being the only one in the family born with “something wrong”. Most thought of their sibling’s cardiac condition infrequently, with the surgical scar a reminder for some. Few could recall details of their sibling’s heart condition, and those who could recall the cardiac hospital admission identified it being a time of greater impact on their family than now. One sibling reflected on how her own (non-CHD related) hospitalization helped her understand the difficulty her parents experienced with “their little baby going through so much”. Although most siblings had minimal awareness of or worry about their sibling’s cardiology follow-up visits, one described feeling scared that “something might go wrong”.
Discussion
In this qualitative study including parents and siblings of children with d-TGA, participants predominantly described positive adaptation and living and valuing their “normal” family lives, despite some ongoing uncertainties and reminders of their early experiences. Findings align with Rolland’s Family Systems – Illness Model34,35 identified previously among fathers of children with CHD.36 Families in our study have moved beyond the crisis phase of diagnosis and surgery, having achieved an understanding of their child’s condition, positive adaptation within the hospital environment, and maintaining hope while acknowledging potential future challenges.
Normalcy within the family system is subjective, culturally constructed, and does not imply the absence of challenges.37 The importance of a sense of normality has been identified in a systematic review of qualitative studies including families of children with CHD.25,38,39 “Chronic paradoxes” experienced by parents and families with a child with CHD have been described,39 where living a “normal” life is seen as vital but also a source of stress, particularly in the transition home from the hospital. Mothers and fathers in our study have predominantly established what they describe as “normal” family life, where they and others mostly treat their child “normally”, which may reflect the older age of children in this sample. The importance of treating your child “normally” has been reported in other studies of children with CHD.25 In our study, two facilitating factors were identified. First, through reassurance and encouragement by treating clinicians, consistent with earlier studies of parents of children with d-TGA, where parents were encouraged to treat their child as “normal” and considered “fixed”.9,10 Second, parents’ own experiences of seeing their child’s progress and achievements, consistent with the experience of parents of children with single ventricle conditions.26
Results from our study are consistent with others examining families of children and adolescents with CHD, where both predominantly no difference between parent responses has been reported,36,40,41 as well as greater psychological distress among mothers than fathers.40,42,43 While mothers and fathers in the current study predominantly described not living a life focused on their child’s CHD, some mothers described ongoing experiences of guilt, worry, and fear. Parents also identified positive outcomes through personal growth and strengthening of relationships within the family system. Increased compassion, strength in coping, and appreciation for the family have been reported by parents of children with HLHS,44 with greater family closeness identified in other studies of children with childhood heart conditions,21 including families of children with d-TGA.9 Studies of post-traumatic growth and individual resilience in CHD family populations are very limited, as are longitudinal studies of family resilience more broadly.45 Such studies may be valuable in understanding the experiences of, and protective factors for families of children with complex CHD, particularly at times of key clinical and social transitions and where future uncertainty is evident.9,46
To our knowledge, our study is the first to report on parental and sibling perceptions of the surgical scars of their child and sibling with CHD. Studies examining scar perceptions of adolescents and adults with CHD themselves are also limited and, consistent with our findings, identify both negative (impact on self-image)47 and positive (appreciation of their health) effects.48 Those with greater disease complexity were more affected than those with simple conditions,48 however, parental perception of scarring across disease complexity is wholly unknown. Furthermore, optimal strategies for communicating with and supporting parents and siblings regarding their child’s and sibling’s scars are also unknown.
Consistent with recent reviews,49,50 most siblings in our study did not identify being affected in daily life by their sibling’s CHD, likely due to the good health of the child with CHD and lack of CHD-related caregiving needs. Negative feelings such as jealousy and resentfulness identified in studies of siblings of children with CHD21 and other conditions51 were also not described. A lack of discussion of the condition by parents with siblings in our study is consistent with the experiences of siblings of children with other chronic illnesses;52 however, this may be due to a perceived lack of impact on the family as opposed to protecting siblings.
Strengths of the current study include exploration of the experiences of a cohort with a predominantly homogeneous clinical course, as well as the participation of multiple family members and subsequent response comparisons. Limitations of the study, however, are also noted. Our findings may not be generalizable to families of children with other cardiac conditions or those who do not have access to socialized medicine. Data saturation was not achieved for sibling interviews; however, given the importance of, but very limited, qualitative evidence of sibling experiences, the current study makes an important contribution.
In conclusion, while parents and siblings of children with d-TGA value living “normal” family lives, opportunities exist for improved care and future research. Persisting distress for some parents and variability in transition to a sense of normality highlight the need for ongoing communication with families regarding their wellbeing including at routine cardiac review. Our study supports the identified need for further exploration of positive processes and outcomes, including individual and family resilience, across time. Further understanding of family members’ perceptions of surgical scars is also needed to ensure information and support of families is inclusive of their own experience, as well as that of the child with CHD. Finally, self-reported sibling experiences are needed to better understand and address education and support needs over time.
Data availability
Datasets generated and/or analyzed for this study will be available on reasonable request from the corresponding author.
References
Morfaw, F. et al. Outcomes after corrective surgery for congenital dextro-transposition of the arteries using the arterial switch technique: a scoping systematic review. Syst. Rev. 9, 1–13 (2020).
de Koning, W. B. et al. Follow-up outcomes 10 years after arterial switch operation for transposition of the great arteries: comparison of cardiological health status and health-related quality of life to those of the a normal reference population. Eur. J. Pediatr. 167, 995–1004 (2008).
Villafañe, J. et al. D-Transposition of the great arteries: the current era of the arterial switch operation. J. Am. Coll. Cardiol. 64, 498–511 (2014).
Martins, P. & Castela, E. Transposition of the great arteries. Orphanet J. Rare Dis. 3, 27 (2008).
Bellinger, D. C. et al. Behaviour at eight years in children with surgically corrected transposition: the Boston Circulatory Arrest Trial. Cardiol. Young. 19, 86–97 (2009).
Calderon, J. et al. Executive function and theory of mind in school-aged children after neonatal corrective cardiac surgery for transposition of the great arteries. Dev. Med. Child Neurol. 52, 1139–1144 (2010).
Kasmi, L. et al. Neuropsychological and psychiatric outcomes in dextro-transposition of the great arteries across the lifespan: a state-of-the-art review. Front. Pediatr. 5, 59 (2017).
Bellinger, D. C. et al. Neurodevelopmental status at eight years in children with dextro-transposition of the great arteries: the Boston Circulatory Arrest Trial. J. Thorac. Cardiovasc. Surg. 126, 1385–1396 (2003).
Brosig, C., Mussatto, K., Kuhn, E. & Tweddell, J. Psychosocial outcomes for preschool children and families after surgery for complex congenital heart disease. Pediatr. Cardiol. 28, 255–262 (2007).
Visconti, J. K., Saudino, J. K., Rappaport, A. L., Newburger, W. J. & Bellinger, C. D. Influence of parental stress and social support on the behavioral adjustment of children with transposition of the great arteries. J. Dev. Behav. Pediatr. 23, 314–321 (2002).
Woolf-King, S. E., Anger, A., Arnold, E. A., Weiss, S. J. & Teitel, D. Mental health among parents of children with critical congenital heart defects: a systematic review. J. Am. Heart Assoc. 6, e004862 (2017).
Soulvie, M. A., Desai, P. P., White, C. P. & Sullivan, B. N. Psychological distress experienced by parents of young children with congenital heart defects: a comprehensive review of literature. J. Soc. Serv. Res. 38, 484–502 (2012).
Kasparian, N. A. et al. Mental health care for parents of babies with congenital heart disease during intensive care unit admission: systematic review and statement of best practice. Early Hum. Dev. 139, 104837–104837 (2019).
Solberg, Ø et al. Trajectories of maternal mental health: a prospective study of mothers of infants with congenital heart defects from pregnancy to 36 months postpartum. J. Pediatr. Psychol. 37, 687–696 (2012).
Denniss, D. L., Sholler, G. F., Costa, D. S. J., Winlaw, D. S. & Kasparian, N. A. Need for routine screening of health-related quality of life in families of young children with complex congenital heart disease. J. Pediatr. 205, 21–28 (2019).
Jantien Vrijmoet-Wiersma, C. M., Ottenkamp, J., van Roozendaal, M., Grootenhuis, M. A. & Koopman, H. M. A multicentric study of disease-related stress, and perceived vulnerability, in parents of children with congenital cardiac disease. Cardiol. Young. 19, 608–614 (2009).
Spijkerboer, A. et al. Long-term psychological distress, and styles of coping, in parents of children and adolescents who underwent invasive treatment for congenital cardiac disease. Cardiol. Young. 17, 638–645 (2007).
Menahem, S., Poulakis, Z. & Prior, M. Children subjected to cardiac surgery for congenital heart disease. Part 2 - parental emotional experiences. Interact Cardiovasc. Thorac. Surg. 7, 605–608 (2008).
Jackson, A. C., Higgins, R. O., Frydenberg, E., Liang, R. P. & Murphy, B. M. Parent’s perspectives on how they cope with the impact on their family of a child with heart disease. J. Pediatr. Nurs. 40, e9–e17 (2018).
Gregory, M. R. B., Prouhet, P. M., Russell, C. L. & Pfannenstiel, B. R. Quality of life for parents of children with congenital heart defect: a systematic review. J. Cardiovasc Nurs. 33, 363–371 (2018).
Wray, J. & Maynard, L. Living with congenital or acquired cardiac disease in childhood: maternal perceptions of the impact on the child and family. Cardiol. Young. 15, 133–140 (2005).
Wray, J. et al. Psychosocial functioning of parents of children with heart disease—describing the landscape. Eur. J. Pediatr. 177, 1811–1821 (2018).
Braun V. & Clarke V. Successful qualitative research: a practical guide for beginners (SAGE, 2013).
Wei, H., Roscigno, C. I., Hanson, C. C. & Swanson, K. M. Families of children with congenital heart disease: a literature review. Heart Lung 44, 494–511 (2015).
Lumsden M., Smith D., Wittkowski A. Coping in parents of children with congenital heart disease: a systematic review and meta-synthesis. J. Child Fam. Stud. 1–18, https://doi.org/10.1007/s10826-019-01406-8 (2019).
Lumsden, M. R., Smith, D. M., Twigg, E., Guerrero, R. & Wittkowski, A. Children with single ventricle congenital heart defects: an interpretative phenomenological analysis of the lived parent experience. Prog. Pediatr. Cardiol. 59, 101297 (2020).
Zahra, D., Abbas, H., Hossein, K. & Zahra Sadat, M. Coping with caregiving stress in families of children with congenital heart disease: a qualitative study. Int. J. Community Based Nurs. Midwifery 8, 127–139 (2020).
Mussatto, K. Adaptation of the child and family to life with a chronic illness. Cardiol. Young. 16, 110–116 (2006).
Tong, A., Sainsbury, P. & Craig, J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J. Qual. Health Care 19, 349–357 (2007).
McConnell-Henry T., James A., Chapman Y. & Francis K. Researching with people you know: Issues in interviewing. Contemp. Nurse. 34, 2–9 (2010)
Vasileiou K., Barnett J., Thorpe S. & Young T. Characterising and justifying sample size sufficiency in interview-based studies: systematic analysis of qualitative health research over a 15-year period. BMC Med. Res. Methodol. 18, https://doi.org/10.1186/s12874-018-0594-7 (2018).
Levitt, H. M., Motulsky, S. L., Wertz, F. J., Morrow, S. L. & Ponterotto, J. G. Recommendations for designing and reviewing qualitative research in psychology: promoting methodological integrity. Qualitative Psychol. 4, 2–22 (2017).
Miles, M. B., Huberman, A. M. & Saldana, J. Fundamentals of qualitative data analysis. In Qualitative data analysis: a methods sourcebook, chap 4. (Sage, 2014)
Rolland, J. S. Chronic illness and the life cycle: a conceptual framework. Fam. Process 26, 203–221 (1987).
Rolland, J. S. Cancer and the family: an integrative model. Cancer 104, 2584–2595 (2005).
Gower, C., Higgins, A., Doherty, N. & McCormack, D. Understanding the experiences of fathers of children with congenital heart disease: an interpretative phenomenological analysis. J. Health Psychol. 22, 1447–1457 (2017).
Walsh, F. Changing families in a changing world: reconstructing family normality. In: Normal family processes: growing diversity and complexity (ed. Walsh, F.) 3–26 (The Guilford Press, 2003).
Lin, P. J., Liu, Y. T., Huang, C. H., Huang, S. H. & Chen, C. W. Caring perceptions and experiences of fathers of children with congenital heart disease: a systematic review of qualitative evidence. Int J. Nurs. Pr. 27, e12952 (2021).
Svensson, M. K., Wahlberg, A. & Gislason, G. H. Chronic paradoxes: a systematic review of qualitative family perspectives on living with congenital heart defects. Qual. Health Res. 30, 119–132 (2020).
Hoffman, M. F. et al. Fathers of children with congenital heart disease: sources of stress and opportunities for intervention. Pediatr. Crit. Care Med. 21, e1002–e1009 (2020).
Sood, C. E. et al. Mothers and fathers experience stress of congenital heart disease differently: recommendations for pediatric critical care. Pediatr. Crit. Care Med. 19, 626–634 (2018).
Hwang, J. H. & Chae, S. M. Experiences of fathers of young children with severe congenital heart defects in Korea: a qualitative descriptive study. J. Pediatr. Nurs. 53, e108–e113 (2020).
Clark, S. M. & Miles, M. S. Conflicting responses: the experiences of fathers of infants diagnosed with severe congenital heart disease. J. Soc. Pediatr. Nurs. 4, 7–14 (1999).
Cantwell-Bartl, A. & Tibballs, J. Parenting a child at home with hypoplastic left heart syndrome: experiences of commitment, of stress, and of love. Cardiol. Young. 27, 1341–1348 (2017).
Maurović, I., Liebenberg, L. & Ferić, M. A review of family resilience: understanding the concept and operationalization challenges to inform research and practice. Child Care Pr. 26, 337–357 (2020).
Rempel, G. R. & Harrison, M. J. Safeguarding precarious survival: parenting children who have life-threatening heart disease. Qual. Health Res. 17, 824–837 (2007).
Kovacs, A. H. et al. Psychological outcomes and interventions for individuals with congenital heart disease: a Scientific Statement From the American Heart Association. Circ. Cardiovasc. Qual. Outcomes 15, e000110 (2022).
Kańtoch, M. J. et al. The significance of cardiac surgery scars in adult patients with congenital heart disease. Kardiologia Pol. 64, 51–56 (2006).
Schamong, A. S., Liebermann-Jordanidis, H., Brockmeier, K., Sticker, E. & Kalbe, E. Psychosocial well-being and quality of life in siblings of children with congenital heart disease: a systematic review. J. Child Health Care 26, 319–337 (2022).
Parker, R., Houghton, S., Bichard, E. & McKeever, S. Impact of congenital heart disease on siblings: a review. J. Child Health Care 24, 297–316 (2020).
Bichard, E., McKeever, S., Bench, S. & Wray, J. Experiences of siblings of children with congenital heart disease during Coronavirus disease 2019; a qualitative interview study. J. Pediatr. Nurs. 63, 96–101 (2022).
Deavin, A., Greasley, P. & Dixon, C. Children’s perspectives on living with a sibling with a chronic illness. Pediatrics 142, e20174151 (2018).
Acknowledgements
We gratefully acknowledge the families who participated in this study, as well as Ms. Holly Williams and Ms. Jessica Suna for their assistance in piloting the interview guide. This work was supported by the Australian Government Research Training Program scholarship to Dr. Karen J. Eagleson, a National Heart Foundation of Australia Future Leader Fellowship (101229) along with support from the Heart Institute Research Core at Cincinnati Children’s Hospital to Dr. Nadine A. Kasparian, and a Mater Foundation Principal Research Fellowship and the University Hospitals Cleveland Medical Center and Case Western Reserve University School of Medicine’s Joint Strategic Research Investment to Dr. Samudragupta Bora. The funding sources had no role in the design and conduct of the study; data collection, management, analysis, and interpretation; and writing of the manuscript or the decision to submit it for publication.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
Dr. Karen J. Eagleson conceptualized the study, designed the study protocol, performed data collection and analyses, interpreted the results, drafted and revised the initial manuscript, and approved the final manuscript as submitted. Dr. Theresa I. Chin performed data analyses, interpreted the results, critically reviewed and revised the initial manuscript, and approved the final manuscript as submitted. Dr. Stephen Larmar, Dr. Robert N. Justo, and Dr. Nadine A. Kasparian supervised data collection and analyses, interpreted the results, critically reviewed and revised the initial manuscript, and approved the final manuscript as submitted. Dr. Samudragupta Bora acquired funds and resources, conceptualized the study, designed the study protocol, supervised data collection and analyses, interpreted the results, critically reviewed and revised the initial manuscript, and approved the final manuscript as submitted. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
Written informed consent was obtained from parents and adult sibling participants, and child assent and parental consent were obtained for sibling participants <18 years.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Eagleson, K.J., Chin, T.I., Larmar, S. et al. Longer-term experiences of families of children with dextro-transposition of the great arteries: a qualitative study. Pediatr Res (2025). https://doi.org/10.1038/s41390-025-04201-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41390-025-04201-y