Abstract
Germline testing is becoming increasingly relevant in prostate cancer (PCa) screening, prognosis, and management. A subset of patients with PCa harbor pathogenic/likely pathogenic variants (P/LPVs) in genes mediating DNA-repair processes, and these P/LPVs have implications for cancer screening, treatment, and cascade testing. As a result, it is recommended that all men with high-risk localized and metastatic PCa undergo routine germline testing. As more PCa patients undergo germline testing, it is important that clinicians and genetics experts recognize current disparities in germline testing rates among racial/ethnic minorities in the United States. The reasons for these disparities are multiple and require similarly manifold consideration to close the germline testing gap and reduce inequities in PCa screening, management, and treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
American Cancer Society. Prostate Cancer. 2020. https://www.cancer.org/cancer/prostate-cancer.html.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71:7–33.
Pritchard CC, Mateo J, Walsh MF, De Sarkar N, Abida W, Beltran H, et al. Inherited DNA-repair gene mutations in men with metastatic prostate cancer. N Engl J Med. 2016;375:443–53.
Chornokur G, Dalton K, Borysova ME, Kumar NB. Disparities at presentation, diagnosis, treatment, and survival in African American men, affected by prostate cancer. Prostate. 2011;71:985–97.
Gilligan T. Social disparities and prostate cancer: mapping the gaps in our knowledge. Cancer Causes Control. 2005;16:45–53.
Gross CP, Smith BD, Wolf E, Andersen M. Racial disparities in cancer therapy: did the gap narrow between 1992 and 2002? Cancer. 2008;112:900–8.
Richert-Boe KE, Weinmann S, Shapiro JA, Rybicki BA, Enger SM, Van Den Eeden SK, et al. Racial differences in treatment of early-stage prostate cancer. Urology. 2008;71:1172–6.
Krimphove MJ, Cole AP, Fletcher SA, Harmouch SS, Berg S, Lipsitz SR, et al. Evaluation of the contribution of demographics, access to health care, treatment, and tumor characteristics to racial differences in survival of advanced prostate cancer. Prostate Cancer Prostatic Dis. 2019;22:125–36.
Odedina FT, Akinremi TO, Chinegwundoh F, Roberts R, Yu D, Reams RR, et al. Prostate cancer disparities in Black men of African descent: a comparative literature review of prostate cancer burden among Black men in the United States, Caribbean, United Kingdom, and West Africa. Infect Agent Cancer. 2009;4 Suppl 1:S2.
Chinea FM, Patel VN, Kwon D, Lamichhane N, Lopez C, Punnen S, et al. Ethnic heterogeneity and prostate cancer mortality in Hispanic/Latino men: a population-based study. Oncotarget. 2017;8:69709–21.
Dobbs RW, Malhotra NR, Abern MR, Moreira DM. Prostate cancer disparities in Hispanics by country of origin: a nationwide population-based analysis. Prostate Cancer Prostatic Dis. 2019;22:159–67.
Katz JE, Chinea FM, Patel VN, Balise RR, Venkatramani V, Gonzalgo ML, et al. Disparities in Hispanic/Latino and non-Hispanic Black men with low-risk prostate cancer and eligible for active surveillance: a population-based study. Prostate Cancer Prostatic Dis. 2018;21:533–8.
Nicolosi P, Ledet E, Yang S, Michalski S, Freschi B, O’Leary E, et al. Prevalence of germline variants in prostate cancer and implications for current genetic testing guidelines. JAMA Oncol. 2019;5:523–8.
Rencsok EM, Bazzi LA, McKay RR, Huang FW, Friedant A, Vinson J, et al. Diversity of enrollment in prostate cancer clinical trials: current status and future directions. Cancer Epidemiol Biomark Prev. 2020;29:1374–80.
Kwon DH, Borno HT, Cheng HH, Zhou AY, Small EJ. Ethnic disparities among men with prostate cancer undergoing germline testing. Urol Oncol. 2020;38:80.e1–7.
Borno HT, Odisho AY, Gunn CM, Pankowska M, Rider JR. Disparities in precision medicine-examining germline genetic counseling and testing patterns among men with prostate cancer. Urol Oncol. 2021;39:233.e9–14.
Dharwadkar P, Greenan G, Stoffel EM, Burstein E, Pirzadeh-Miller S, Lahiri S, et al. Racial and ethnic disparities in germline genetic testing of patients with young-onset colorectal cancer. Clin Gastroenterol Hepatol. 2020;S1542-3565:31721–3.
Yip CH, Evans DG, Agarwal G, Buccimazza I, Kwong A, Morant R, et al. Global disparities in breast cancer genetics testing, counselling and management. World J Surg. 2019;43:1264–70.
Parikh DA, Dickerson JC, Kurian AW. Health disparities in germline genetic testing for cancer susceptibility. Cur Breast Cancer Rep. 2020;12:51–8.
Bureau UC. Table 4. Projected race and Hispanic origin 2017. 2021. https://www.census.gov/data/tables/2017/demo/popproj/2017-summary-tables.html.
Berchuck JE, Zhang Z, Silver R, Kwak L, Xie W, Lee GM, et al. Impact of pathogenic germline DNA damage repair alterations on response to intense neoadjuvant androgen deprivation therapy in high-risk localized prostate cancer. Eur Urol. 2021;S0302-2838:00237–2.
Shaya JNS, Hatchell KE, Esplin ED, Nussbaum L, Weise N, Madlensky L, et al. Germline alterations among Hispanic men with prostate cancer. J Clin Oncol. 2021;39:10534.
Ledet EM, Burgess EF, Sokolova AO, Jaeger EB, Hatton W, Moses M, et al. Comparison of germline mutations in African American and Caucasian men with metastatic prostate cancer. Prostate. 2021;81:433–9.
Mahal BA, Alshalalfa M, Kensler KH, Chowdhury-Paulino I, Kantoff P, Mucci LA, et al. Racial differences in genomic profiling of prostate cancer. N Engl J Med. 2020;383:1083–5.
Hall MJ, Olopade OI. Disparities in genetic testing: thinking outside the BRCA box. J Clin Oncol. 2006;24:2197–203.
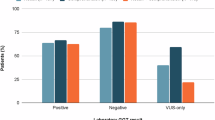
Ndugga-Kabuye MK, Issaka RB. Inequities in multi-gene hereditary cancer testing: lower diagnostic yield and higher VUS rate in individuals who identify as Hispanic, African or Asian and Pacific Islander as compared to European. Fam Cancer. 2019;18:465–9.
Daly MB, Pal T, Buys SS, Dickson P, Domchek SM, Elkhanany A, et al. Genetic/familial high-risk assessment: breast, ovarian, and pancreatic, version 1.2022, NCCN Clinical Practice Guidelines in Oncology. 2021. https://www.nccn.org/professionals/physician_gls/pdf/genetics_bop.pdf.
Schaeffer E, Srinivas S, Antonarakis ES, Armstrong AJ, Cheng HH, D’Amico AV, et al. Prostate Cancer, Version 1.2022, NCCN Clinical Practice Guidelines in Oncology. 2021. https://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf.
Spratt DE, Chan T, Waldron L, Speers C, Feng FY, Ogunwobi OO, et al. Racial/ethnic disparities in genomic sequencing. JAMA Oncol. 2016;2:1070–4.
Na R, Zheng SL, Han M, Yu H, Jiang D, Shah S, et al. Germline mutations in ATM and BRCA1/2 distinguish risk for lethal and indolent prostate cancer and are associated with early age at death. Eur Urol. 2017;71:740–7.
Merseburger AS, Waldron N, Ribal MJ, Heidenreich A, Perner S, Fizazi K, et al. Genomic testing in patients with metastatic castration-resistant prostate cancer: a pragmatic guide for clinicians. Eur Urol. 2021;79:519–29.
Food and Drug Administration. FDA approves olaparib for HRR gene-mutated metastatic castration-resistant prostate cancer. 2020. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-olaparib-hrr-gene-mutated-metastatic-castration-resistant-prostate-cancer.
Food and Drug Administration. FDA grants accelerated approval to rucaparib for BRCA-mutated metastatic castration-resistant prostate cancer. 2020. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-rucaparib-brca-mutated-metastatic-castration-resistant-prostate.
Loeb S, Giri VN. Clinical implications of germline testing in newly diagnosed prostate cancer. Eur Urol Oncol. 2021;4:1–9.
Antonarakis ES, Piulats JM, Gross-Goupil M, Goh J, Ojamaa K, Hoimes CJ, et al. Pembrolizumab for treatment-refractory metastatic castration-resistant prostate cancer: multicohort, open-label phase II KEYNOTE-199 study. J Clin Oncol. 2020;38:395–405.
Sabol RA, Ledet EM, Jaeger E, Hatton W, Moses M, Lankford A, et al. Family history and pathogenic/likely pathogenic germline variants in prostate cancer patients. Prostate. 2021;81:427–32.
Berninger T, Nusbaum R, Redlinger-Grosse K, Davis C, Reiser C. A narrative literature review: Growing the workforce through increased fieldwork capacity in genetic counseling training programs. J Genet Couns. 2021;30:574–87.
Delikurt T, Williamson GR, Anastasiadou V, Skirton H. A systematic review of factors that act as barriers to patient referral to genetic services. Eur J Hum Genet. 2015;23:739–45.
Szymaniak BM, Facchini LA, Giri VN, Antonarakis ES, Beer TM, Carlo MI, et al. Practical considerations and challenges for germline genetic testing in patients with prostate cancer: recommendations from the germline genetics working group of the PCCTC. JCO Oncol Pract. 2020;16:811–9.
Villegas C, Haga SB. Access to genetic counselors in the southern United States. J Pers Med. 2019;9:1–33.
Shur N, Atabaki SM, Kisling MS, Tabarani A, Williams C, Fraser JL, et al. Rapid deployment of a telemedicine care model for genetics and metabolism during COVID-19. Am J Med Genet A 2021;185:68–72.
Rana HQSJ, Petrucelli N, Koeller DR, Pirzadeh-Miller S, Reys B, Kipnis L, et al. A randomized controlled trial of video-education or in-person genetic counseling for men with prostate cancer (ProGen). J Clin Oncol. 2020;38:1507.
Nelson A. Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc. 2002;94:666–8.
Rogers CR, Rovito MJ, Hussein M, Obidike OJ, Pratt R, Alexander M, et al. Attitudes toward genomic testing and prostate cancer research among Black men. Am J Prev Med. 2018;0 5 Suppl 1:S103–11.
Shields AE, Burke W, Levy DE. Differential use of available genetic tests among primary care physicians in the United States: results of a national survey. Genet Med. 2008;10:404–14.
Zhen JT, Syed J, Nguyen KA, Leapman MS, Agarwal N, Brierley K, et al. Genetic testing for hereditary prostate cancer: current status and limitations. Cancer. 2018;124:3105–17.
Hammond WP, Matthews D, Mohottige D, Agyemang A, Corbie-Smith G. Masculinity, medical mistrust, and preventive health services delays among community-dwelling African-American men. J Gen Intern Med. 2010;25:1300–8.
LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44:2093–105.
Sarver JH, Cydulka RK, Baker DW. Usual source of care and nonurgent emergency department use. Acad Emerg Med. 2002;9:916–23.
Allen JD, Kennedy M, Wilson-Glover A, Gilligan TD. African-American men’s perceptions about prostate cancer: implications for designing educational interventions. Soc Sci Med. 2007;64:2189–200.
American Academy of Medical Colleges. Diversity in medicine: facts and figures 2019. 2019. https://www.aamc.org/data-reports/workforce/interactive-data/figure-18-percentage-all-active-physicians-race/ethnicity-2018.
National Society of Genetic Counselors. 2021 Professional status survey: executive summary. 2020. https://www.nsgc.org/Portals/0/Executive%20Summary%202021%20FINAL%2005-03-21.pdf.
Alsan MGO, Graziani GC. Does diversity matter for health? Experimental evidence from Oakland. Am Econ Rev. 2019;109:4071–111.
Shaw A, Ahmed M. Translating genetics leaflets into languages other than English: lessons from an assessment of Urdu materials. J Genet Couns. 2004;13:321–42.
Bouye KE, McCleary KJ, Williams KB. Increasing diversity in the health professions: reflections on student pipeline programs. J Health Sci Humanit. 2016;6:67–79.
Halbert CH, Harrison BW. Genetic counseling among minority populations in the era of precision medicine. Am J Med Genet C Semin Med Genet. 2018;178:68–74.
Chapman EN, Kaatz A, Carnes M. Physicians and implicit bias: how doctors may unwittingly perpetuate health care disparities. J Gen Intern Med. 2013;28:1504–10.
National Institutes of Health NHGRP. The Genetic Information Nondiscrimination Act of 2008. 2021. https://www.genome.gov/27568492/the-genetic-information-nondiscrimination-act-of-2008.
Saulsberry K, Terry SF. The need to build trust: a perspective on disparities in genetic testing. Genet Test Mol Biomark. 2013;17:647–8.
Cackowski FC, Mahal B, Heath EI, Carthon B. Evolution of disparities in prostate cancer treatment: is this a new normal? Am Soc Clin Oncol Educ Book. 2021;41:1–12.
Allford A, Qureshi N, Barwell J, Lewis C, Kai J. What hinders minority ethnic access to cancer genetics services and what may help? Eur J Hum Genet. 2014;22:866–74.
Keisler-Starkey KBL Health Insurance Coverage in the United States: 2019 Current Population Reports: US Department of Commerce, US Census Bureau. 2020. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p60-271.pdf.
Ward E, Halpern M, Schrag N, Cokkinides V, DeSantis C, Bandi P, et al. Association of insurance with cancer care utilization and outcomes. CA Cancer J Clin. 2008;58:9–31.
Yabroff KR, Zhao J, de Moor JS, Sineshaw HM, Freedman AN, Zheng Z, et al. Factors associated with oncologist discussions of the costs of genomic testing and related treatments. J Natl Cancer Inst. 2020;112:498–506.
Color Genomics. Products. 2021. https://www.color.com/providers/products.
Invitae. Detect Hereditary Prostate Cancer. 2021. https://www.invitae.com/en/detect-hereditary-prostate-cancer/.
Promise. 2021. https://www.prostatecancerpromise.org/.
Petrucelli N, Daly MB, Pal T. BRCA1- and BRCA2-associated hereditary breast and ovarian cancer. GeneReviews. 1998:1993–2021.
Giri VN, Hegarty SE, Hyatt C, O’Leary E, Garcia J, Knudsen KE, et al. Germline genetic testing for inherited prostate cancer in practice: implications for genetic testing, precision therapy, and cascade testing. Prostate. 2019;79:333–9.
Armstrong K, Micco E, Carney A, Stopfer J, Putt M. Racial differences in the use of BRCA1/2 testing among women with a family history of breast or ovarian cancer. JAMA. 2005;293:1729–36.
Pritchard CC. New name for breast-cancer syndrome could help to save lives. Nature. 2019;571:27–9.
Sweeney CJ, Chen YH, Carducci M, Liu G, Jarrard DF, Eisenberger M, et al. Chemohormonal therapy in metastatic hormone-sensitive prostate cancer. N Engl J Med. 2015;373:737–46.
James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387:1163–77.
Fizazi K, Tran N, Fein L, Matsubara N, Rodriguez-Antolin A, Alekseev BY, et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N Engl J Med. 2017;377:352–60.
James ND, de Bono JS, Spears MR, Clarke NW, Mason MD, Dearnaley DP, et al. Abiraterone for prostate cancer not previously treated with hormone therapy. N Engl J Med. 2017;377:338–51.
Chi KN, Agarwal N, Bjartell A, Chung BH, Pereira de Santana Gomes AJ, Given R, et al. Apalutamide for metastatic, castration-sensitive prostate cancer. N Engl J Med. 2019;381:13–24.
Armstrong AJ, Szmulewitz RZ, Petrylak DP, Holzbeierlein J, Villers A, Azad A. at al. ARCHES: a randomized, phase III study of androgen deprivation therapy with enzalutamide or placebo in men with metastatic hormone-sensitive prostate cancer. J Clin Oncol. 2019 ;37:2974–86.
Davis ID, Martin AJ, Stockler MR, Begbie S, Chi KN, Chowdhury S, et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N Engl J Med. 2019;381:121–31.
Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med. 2004;351:1502–12.
de Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet. 2010;376:1147–54.
Kantoff PW, Higano CS, Shore ND, Berger ER, Small EJ, Penson DF, et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med. 2010;363:411–22.
Parker C, Nilsson S, Heinrich D, Helle SI, O’Sullivan JM, Fosså SD, et al. Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med. 2013;369:213–23.
de Bono JS, Logothetis CJ, Molina A, Fizazi K, North S, Chu L, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med. 2011;364:1995–2005.
Ryan CJ, Smith MR, de Bono JS, Molina A, Logothetis CJ, de Souza P, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med. 2013;368:138–48.
Scher HI, Fizazi K, Saad F, Taplin ME, Sternberg CN, Miller K, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med. 2012;367:1187–97.
Beer TM, Armstrong AJ, Rathkopf DE, Loriot Y, Sternberg CN, Higano CS, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med. 2014;371:424–33.
Smith MR, Saad F, Chowdhury S, Oudard S, Hadaschik BA, Graff JN, et al. Apalutamide treatment and metastasis-free survival in prostate cancer. N Engl J Med. 2018;378:1408–18.
Hussain M, Fizazi K, Saad F, Rathenborg P, Shore N, Ferreira U, et al. Enzalutamide in men with nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2018;378:2465–74.
Fizazi K, Shore N, Tammela TL, Ulys A, Vjaters E, Polyakov S, et al. Darolutamide in nonmetastatic, castration-resistant prostate cancer. N Engl J Med. 2019;380:1235–46.
Giri VN, Knudsen KE, Kelly WK, Cheng HH, Cooney KA, Cookson MS, et al. Implementation of germline testing for prostate cancer: Philadelphia Prostate Cancer Consensus Conference 2019. J Clin Oncol. 2020;38:2798–811.
Lowrance WT, Breau RH, Chou R, Chapin BF, Crispino T, Dreicer R, et al. Advanced prostate cancer: AUA/ASTRO/SUO Guideline PART I. J Urol. 2021;205:14–21.
Lowrance WT, Breau RH, Chou R, Chapin BF, Crispino T, Dreicer R, et al. Advanced prostate cancer: AUA/ASTRO/SUO Guideline PART II. J Urol. 2021;205:22–9.
Sanda MG, Chen RC, Crispino T, Freedland S, Greene K, Klotz LH, et al. Clinically localized prostate cancer: AUA/ASTRO/SUO Guideline: American Urological Association. 2017. https://www.auanet.org/guidelines/guidelines/prostate-cancer-clinically-localized-guideline#x6914.
Acknowledgements
PNW SPORE CA097186; Congressional Designated Medical Research Program (CDMRP) award W81XWH-17-2-0043; P30 CA015704; Prostate Cancer Foundation
Author information
Authors and Affiliations
Contributions
Concept and design: RRM. Acquisition, analysis or interpretation of data: NW, JS. Drafting of paper: NW, RRM. Critical revisions of paper for important intellectual content: NW, JS, JJD, HHC, LM, and RRM. Approval of final paper: NW, JS, JJD, HHC, LM, and RRM. Supervision: RRM.
Corresponding author
Ethics declarations
Competing interests
HHC received research funding to her institution from Astellas, Clovis Oncology, Color Foundation, Janssen, Medivation, Phosplatin, and Sanofi; is a consultant for AstraZeneca. RRM received research funding from Bayer, Pfizer, Tempus; serves on Advisory Board for AstraZeneca, Bayer, Bristol Myers Squibb, Calithera, Exelixis, Janssen, Merck, Novartis, Pfizer, Sanofi, Tempus; is a consultant for Dendreon, Myovant, Vividion; serves on the molecular tumor board at Caris. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Weise, N., Shaya, J., Javier-Desloges, J. et al. Disparities in germline testing among racial minorities with prostate cancer. Prostate Cancer Prostatic Dis 25, 403–410 (2022). https://doi.org/10.1038/s41391-021-00469-3
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41391-021-00469-3
This article is cited by
-
Germline and somatic testing for homologous repair deficiency in patients with prostate cancer (part 1 of 2)
Prostate Cancer and Prostatic Diseases (2025)
-
“Hope at a better chance”: perspectives on genetic counseling and testing among black individuals with prostate cancer
Journal of Community Genetics (2025)
-
Olaparib Monotherapy or in Combination with Abiraterone for the Treatment of Patients with Metastatic Castration-Resistant Prostate Cancer (mCRPC) and a BRCA Mutation
Targeted Oncology (2025)
-
Germline Mutations and Ancestry in Prostate Cancer
Current Oncology Reports (2024)
-
Adaptation of the socioecological model to address disparities in engagement of Black men in prostate cancer genetic testing
BMC Public Health (2024)