Abstract
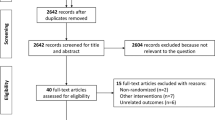
Intermittent catheterization (IMC) is the accepted evidence-based best practice for bladder management in people with voiding dysfunction due to neurogenic bladder. The two methods for performing IMC over the decades since this practice was introduced are reuse and single-use catheters. There are perceived advantages and disadvantages of each method of performing IMC. There is considerable evidence that single-use IMC is associated with better health outcomes, including reduced risk of urinary tract infection, urethral trauma, and quality of life. People performing IMC also indicate a preference for single-use, although there are advantages of reuse that need to be acknowledged. Ideally, further research is needed in this area, particularly around the washing and storage of reuse catheters, as well as an adequately powered multicenter RCT comparing reuse with single-use IMC, but there are numerous challenges associated with progressing this research.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Goetz LL, Droste L, Klausner AP, Newman DK. Catheters used for intermittent catheterization. clinical application of urologic catheters, devices and products. Cham: Springer International Publishing; 2018:47–77.
Lamin E, Newman DK. Clean intermittent catheterization revisited. Int Urol Nephrol. 2016;48:931–9.
Kessler TM, Ryu G, Burkhard FC. Clean intermittent self-catheterization: a burden for the patient? Neurourol Urodyn. 2009;28:18–21.
Guttmann L, Frankel H. The value of intermittent catheterisation in the early management of traumatic paraplegia and tetraplegia. Paraplegia. 1966;4:63–84.
Lapides J, Diokno AC, Silber SJ, Lowe BS. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol. 1972;107:458–61.
Newman DK, New PW, Heriseanu R, Petronis S, Håkansson J, Håkansson MÅ, et al. Intermittent catheterization with single or reuse catheters: Clinical study on safety and impact on quality of life. Intermittent catheterization with single- or multiple-reuse catheters: clinical study on safety and impact on quality of life. Int Urol Nephrol. 2020;8:1443–51.
Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010;31:319–26.
Blok B, Pannek J, Castro-Diaz D, Del Popolo G, Groen J, Hamid R, et al. Guidelines on neuro-urology. European Association of Urology; EAU Guidelines Office, Arnhem, The Netherlands. 2018.
Vahr S, Cobussen-Boekhorst H, Eikenboom J, Geng V, Holroyd S, Lester M, et al. Evidence-based guidelines for best practice in urological health care. Catheterisation urethral intermittent in adults dilatation, urethral intermittent in adults. European Association of Urology Nurses. Arnhem, The Netherlands. 2013.
Chartier-Kastler E, Denys P. Intermittent catheterization with hydrophilic catheters as a treatment of chronic neurogenic urinary retention. Neurourol Urodyn. 2011;30:21–31.
Hedlund H, Hjelmas K, Jonsson O, Klarskov P, Talja M. Hydrophilic versus non-coated catheters for intermittent catheterization. Scand J Urol Nephrol. 2001;35:49–53.
Shamout S, Biardeau X, Corcos J, Campeau L. Outcome comparison of different approaches to self-intermittent catheterization in neurogenic patients: a systematic review. Spinal Cord. 2017;55:629–43.
Christison K, Walter M, Wyndaele J-JJM, Kennelly M, Kessler TM, Noonan VK et al. Intermittent catheterization: the devil is in the details. J Neurotrauma. 2018;35:985–9.
DeFoor W, Reddy P, Reed M, VanderBrink B, Jackson E, Zhang B, et al. Results of a prospective randomized control trial comparing hydrophilic to uncoated catheters in children with neurogenic bladder. J Pediatr Urol. 2017;13:373.e1–5.
Rognoni C, Tarricone R. Intermittent catheterisation with hydrophilic and non-hydrophilic urinary catheters: systematic literature review and meta-analyses. BMC Urol. 2017;17:4.
Avery M, Prieto J, Okamoto I, Cullen S, Clancy B, Moore KN, et al. Reuse of intermittent catheters: a qualitative study of IC users’ perspectives. BMJ Open. 2018;8:e021554.
Sun AJ, Comiter CV, Elliott CS. The cost of a catheter: an environmental perspective on single use clean intermittent catheterization. Neurourol Urodyn. 2018;37:2204–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author was an investigator in the clinical trial sponsored by Wellspect HealthCare, Sweden, that was cited above (ref. 6).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
New, P.W. The evidence supporting single-use intermittent catheters in people with spinal cord injury. Spinal Cord Ser Cases 6, 89 (2020). https://doi.org/10.1038/s41394-020-00339-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41394-020-00339-5
This article is cited by
-
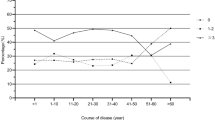
Patterns of neurogenic lower urinary tract dysfunction management and associated factors among Chinese community-dwelling individuals with spinal cord injury
Scientific Reports (2024)
-
Cross-sectional internet survey exploring symptomatic urinary tract infection by type of urinary catheter in persons with spinal cord lesion in Japan
Spinal Cord Series and Cases (2023)
-
Intermittent Catheters: To reuse or not
Spinal Cord Series and Cases (2020)