Abstract
People affected by psychotic, depressive and developmental disorders are at a higher risk for alcohol and tobacco use. However, the further associations between alcohol/tobacco use and symptoms/cognition in these disorders remain unexplored. We identified multimodal brain networks involving alcohol use (n = 707) and tobacco use (n = 281) via supervised multimodal fusion and evaluated if these networks affected symptoms and cognition in people with psychotic (schizophrenia/schizoaffective disorder/bipolar, n = 178/134/143), depressive (major depressive disorder, n = 260) and developmental (autism spectrum disorder/attention deficit hyperactivity disorder, n = 421/346) disorders. Alcohol and tobacco use scores were used as references to guide functional and structural imaging fusion to identify alcohol/tobacco use associated multimodal patterns. Correlation analyses between the extracted brain features and symptoms or cognition were performed to evaluate the relationships between alcohol/tobacco use with symptoms/cognition in 6 psychiatric disorders. Results showed that (1) the default mode network (DMN) and salience network (SN) were associated with alcohol use, whereas the DMN and fronto-limbic network (FLN) were associated with tobacco use; (2) the DMN and fronto-basal ganglia (FBG) related to alcohol/tobacco use were correlated with symptom and cognition in psychosis; (3) the middle temporal cortex related to alcohol/tobacco use was associated with cognition in depression; (4) the DMN related to alcohol/tobacco use was related to symptom, whereas the SN and limbic system (LB) were related to cognition in developmental disorders. In summary, alcohol and tobacco use were associated with structural and functional abnormalities in DMN, SN and FLN and had significant associations with cognition and symptoms in psychotic, depressive and developmental disorders likely via different brain networks. Further understanding of these relationships may assist clinicians in the development of future approaches to improve symptoms and cognition among psychotic, depressive and developmental disorders.
Similar content being viewed by others
Introduction
Alcohol and tobacco use are the two representative and prevailing addictive related disorders worldwide [1,2,3]. The estimated prevalence among the adult population is 18.4% for heavy episodic alcohol use and 15.2% for daily tobacco use [4]. Chronic heavy alcohol/tobacco use has clear effects on the brain and further affects other mental disorders amongst people who drink or smoke [5,6,7]. Alcohol and tobacco use are very common in psychiatric disorders that increase the mortality risk [8,9,10]. However, the brain regions affected by alcohol and tobacco use in psychiatric disorders and their associations with symptoms and cognition remain unexplored.
Previous studies indicated that alcohol and tobacco use are associated with specific symptoms and cognitive levels of psychotic, depressive, and developmental disorders. Tobacco use has been associated with lower education level, positive symptoms (changes in behavior or thoughts) and higher physical aggressiveness in schizophrenia (SZ) [11, 12]. Greater alcohol use was associated with a higher reaction time [13] in schizoaffective disorder (SAD). Tobacco use was independently and moderately associated with suicidal acts [14] in bipolar (BP). Early alcohol and tobacco use prior to 18 years old were found to be associated with increased odds [15] in adult major depressive disorder (MDD). Heavier alcohol use was associated with the degree of autistic personality traits at treatment entry, whereas social interaction and rigidity were associated with problematic alcohol use 2.5 years after treatment entry [16] in autism spectrum disorder (ASD). Another study reported that nicotine may have a beneficial effect on aggression, irritability, and sleep in ASD [17]. Non-smoking young adults with attention deficit hyperactivity disorder (ADHD) showed improvements in cognitive performance following nicotine administration in several domains that are central to ADHD [18]. All the above evidence shows that alcohol/tobacco use is an important feature in broader neuropsychiatric disorders.
Some neuroimaging studies suggest that alcohol and tobacco use have different influences on brain structure and function in patients with psychotic (including SZ, SAD and BP) and depressive (including MDD) disorders. Lower gray matter volume (GMV) in the anterior cingulate cortex (ACC) and thalamus was related to cognitive deficits amongst SZ patients who smoked and used alcohol [19]. Higher amygdala reactivity to acute stress was correlated with greater quantity and frequency of alcohol use in BP [20]. People who drink alcohol with comorbid MDD and/or anxiety showed larger volumes in bilateral cerebral and cerebellar gray matter, relative to non-comorbid patients. They were also related to enlarged left nucleus accumbens and bilateral hippocampus [21]. However, most existing studies include one imaging modality in a single substance use group (alcohol or tobacco use) with a single disease group (SZ or MDD) [22]. Furthermore, few studies investigate the relationships between behavior caused brain functional or structural alterations and alcohol/tobacco use in developmental disorders with respect to neuroimaging.
In this study, we aimed to identify: (1) alcohol and tobacco use related multimodal brain patterns through the Alcohol Use Disorder Identification Test (AUDIT)/Fagerström Test for Nicotine Dependence (FTND)-guided fusion for alcohol use (n = 707) and tobacco use (n = 281) groups, separately. Then we examined the associations between the identified alcohol/tobacco use networks and symptoms/cognition in: (2) psychotic disorder (including SZ, n = 178, SAD, n = 134 and BP, n = 143); (3) depressive disorder (MDD, n = 260); and (4) developmental disorder (including ASD, n = 421 and ADHD, n = 346). (5) All the above correlation analyses were conducted within male and female, separately, to identify the sex-specific associations.
Methods and materials
Participants
Subjects with alcohol use (n = 707) and tobacco use (n = 281) were recruited from Albuquerque through advertisements [23]. The exclusion criteria of alcohol/tobacco use included injury to the brain, brain-related medical problems, and bipolar or psychiatric disorders. In addition, the use of illicit drugs confirmed or rejected by urinalysis was also excluded. The Bipolar and Schizophrenia Network for Intermediate Phenotypes (BSNIP) consortium [24] provided information on psychotic disorders (including 178 SZs, 134 SADs and 143 BPs). MDDs (n = 260) were collected from the West China Hospital of Sichuan, Henan Mental Hospital of Xinxiang, Beijing Anding Hospital and First Affiliated Hospital of Zhejiang [25, 26]. ASD (n = 421) and ADHD (n = 346) were obtained from the Autism Brain Imaging Data Exchange II (ABIDE II [27, 28]) and the ADHD-200 project [19] (http://fcon_1000.projects.nitrc.org/indi/adhd200/), respectively. The sufficient number of participants included in this study guaranties adequate statistical power. The diagnosis of SZ, SAD, BP, MDD, ASD and ADHD was based on the Structured Clinical Interview for Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Substance use (alcohol/tobacco) information was not available for the above disorders.
The alcohol and tobacco dependence severity in people who drink alcohol and smoke tobacco was assessed with AUDIT and FTND, respectively. Subjects with alcohol/tobacco use who participated in the assessment of AUDIT/FTND were all used in the multimodal fusion analysis. The detailed information on the total number of calendar days, number of drinks, number of drinking days and other relevant subdomains for alcohol and tobacco use was included in the Supplementary Table 1. The continuous clinical phenotypes of SZ, SAD and BP were measured using the Schizo-Bipolar Scale (SBS) [29]. Cognition of SZ, SAD and BP was assessed with the Wide Range Achievement Test-IV (WRAT) and Brief Assessment of Cognition in Schizophrenia (BACS) [30]. The Ruminative Response Scale (RRS) [31], the Wechsler Memory Scale (WMS-IV) [32], and the Hamilton Depression Rating Scale (HAMD) [33] were used, respectively, to evaluate the symptoms and cognition of MDD. The symptoms of ASD and ADHD were determined by the Social Responsiveness Scale (SRS) [34] and Inattention and Hyperactivity (IH) (Conners’ Parent Rating Scale-Revised, Long Version [35]), respectively. Cognition of ASD and ADHD was evaluated using the Wechsler Abbreviated Scale of Intelligence (WASI) [36]. Both resting functional magnetic resonance imaging (fMRI) and structural magnetic resonance imaging (sMRI) were collected from different sites using different scanners (imaging parameters and preprocessing procedures can be found in Supplementary Tables 2–11 and Supplementary “Preprocessing” section). The demographic and clinical information were summarized in Supplementary Table 12. Detailed information on the subdomains measuring each disorder’s symptoms and cognitive scale can be found in the Supplementary Table 13. Ethical approval was granted by each relevant Ethics Committee, and informed consent was obtained from each subject prior to scanning according to each site’s Institutional Review Boards.
Analysis framework
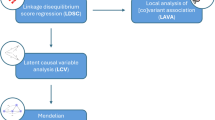
According to the goals stated in the introduction, we conducted the following analyses: (1) AUDIT and FTND scores were used as references to guide MRI (fALFF + GMV) fusion to identify the multimodal brain patterns (fALFF and GMV covaried brain regions) related to alcohol and tobacco use, individually (Fig. 1a); (2) alcohol/tobacco/alcohol + tobacco use-associated brain patterns were used as regions of interest (ROIs) to extract fALFF and GMV features from psychotic (including 178 SZs, 134 SADs and 143 BPs), depressive (MDD, n = 260) and developmental (including 421 ASDs and 346 ADHDs) disorders, respectively (Fig. 1b); (3) correlation analyses between the extracted brain features of 6 brain disorders with symptoms/cognition were performed (Fig. 1c).
a AUDIT/FTND-guided “fALFF+GMV” fusion was performed for alcohol and tobacco use groups individually to identify alcohol and tobacco use related multimodal brain networks. b alcohol/tobacco use-associated brain regions were used as ROIs to extract features for psychotic (including 178 SZs, 134 SADs and 143 BPs), depressive (MDD, n = 260) and developmental (including 421 ASDs and 346 ADHDs) disorders. c Correlation analyses were performed between alcohol/tobacco use related features with symptoms and cognition for 6 brain disorders.
Specifically, subject-wise AUDIT/FTND scores were used as references to jointly decompose the preprocessed multimodal MRI features (fALFF and GMV) via multi-site canonical correlation analysis with reference + joint independent component analysis (MCCAR + jICA) [37] to identify AUDIT/FTND-associated multimodal brain patterns in alcohol/tobacco use, individually. This method can simultaneously maximize the inter-modality covariation and correlations of neuroimaging components with clinical measures of interest (i.e., AUDIT/FTND), as shown in Eq. (1).
where \({{\boldsymbol{A}}}_{{\rm{k}}}\) is the mixing matrix for each modality, \({\rm{corr}}\left({{\boldsymbol{A}}}_{{\rm{k}}},{{\boldsymbol{A}}}_{{\rm{j}}}\right)\) is the column-wise correlation between \({{\boldsymbol{A}}}_{{\rm{k}}}\) and \({{\boldsymbol{A}}}_{{\rm{j}}}\), and \({\rm{corr}}\left({{\boldsymbol{A}}}_{{\rm{k}}},{ref}\right)\) is the column-wise correlation between \({{\boldsymbol{A}}}_{{\rm{k}}}\) and the reference signal (AUDIT/FTND). As a result, the joint multimodal component(s) correlated with AUDIT/FTND will be identified for both alcohol use and tobacco use groups.
After identifying the joint multimodal components, each component was divided into positive (Z > 2) and negative (Z < −2) brain regions by Z-scored spatial maps. The shared brain regions between alcohol and tobacco use were determined by overlapping the identified AUDIT/FTND-associated multimodal brain patterns between alcohol use and tobacco use groups. As shown in Figs. 1b, 6 fALFF/GMV covarying patterns related to AUDIT or (and) FTND were identified. Thus, we can obtain separate positive and negative brain masks for each of the 6 brain patterns. Then, 10 positive and negative brain masks (8 from separating the positive and negative brain regions in multimodal components, 2 from the overlapping between alcohol and tobacco use) were used as ROIs to extract fALFF/GMV features from psychotic (including SZ, SAD and BP), depressive (including MDD) and developmental (including ASD and ADHD) disorders, respectively, and the mean of the voxels within the masked region was calculated for each subject.
Finally, correlation analyses between the extracted brain features (the mean of the voxels within the 10 masked regions) and symptoms (including SBS, RRS, SRS and IH) or cognition (including WRAT, BACS, WMS-IV and WAIS) were performed to evaluate the relationships between alcohol and tobacco use with symptoms and cognition in psychotic, depressive and developmental disorders. We also calculated the correlations between identified brain regions and symptoms/cognition of disorders across sex. The stability of the brain features identified from fMRI and sMRI was tested by 10-fold cross-validation, which can be found in Supplementary “Similar results comparing fMRI and sMRI in correlations” section and Supplementary Tables 14 and 15.
Results
AUDIT-associated multimodal components within alcohol use group
AUDIT-associated fALFF+GMV joint components (Fig. 2a) were identified for the alcohol use group, which were correlated with AUDIT scores (fALFF: r = 0.22, p = 1.9e−09*; GMV: r = 0.20, p = 4.5e−08*, false discovery rate (FDR) corrected, Fig. 2b). Statistical significance that passed the FDR correction (Supplementary “FDR correction”) was denoted with an asterisk (*). The spatial maps were transformed into Z scores and visualized at |Z| > 2. The positive/negative brain regions (red/blue) represented positive/negative correlations with AUDIT in fALFF or GMV. Alcohol use-related multimodal brain patterns included positive fALFF in calcarine, precentral cortex (PRC), postcentral cortex (POC) and lingual gyrus (LG), accompanied with negative fALFF in prefrontal cortex (PFC), ACC, angular gyrus (AG), middle temporal cortex (MTC), LG and caudate. Alcohol use-related multimodal brain patterns included positive GMV in MTC, middle occipital cortex (MOC), inferior parietal cortex (IPC) and AG, accompanied with negative GMV in medial prefrontal cortex (MPFC), precuneus, PRC, midcingulate cortex (MCC), ACC, insula, striatum (caudate and putamen) and amygdala. The identified brain regions for alcohol use were summarized in Supplementary Table 16 for fALFF and GMV in Talairach labels, respectively. Note that subdomains of AUDIT, including alcohol consumption, alcohol dependence and alcohol problems, were also used as references to guide the multimodal fusion on alcohol use dataset, separately. It is clear that subdomain related brain patterns (Supplementary Fig. 1b–d) are highly similar (>85%) to AUDIT related maps (Supplementary Fig. 1a).
The spatial brain maps of alcohol use (a) and tobacco use (c) were visualized at |Z| > 2. Correlation scatter plot between AUDIT (b), FTND (d) and the loadings of the identified component for each modality within alcohol use and tobacco use groups. IC refers to independent component. Asterisk (*) is used to indicate results which pass false discovery rate (FDR) correction for multiple comparisons.
FTND-associated multimodal components within tobacco use group
FTND-associated fALFF+GMV joint components (visualized at |Z| > 2, Fig. 2c) were identified for tobacco use group, which were correlated with FTND scores (fALFF: r = 0.26, p = 1.5e−05*; GMV: r = 0.28, p = 2.2e−06*, Fig. 2d). Tobacco use-related multimodal patterns included positive fALFF in MPFC, AG, precuneus, posterior cingulate cortex (PCC) and MTC, accompanied with negative fALFF in thalamus and LG. Tobacco use-related multimodal patterns included positive GMV in PFC, accompanied with negative GMV in insula, striatum, amygdala, parahippocampal, hippocampus and fusiform gyrus (FG). The identified brain regions for tobacco use were summarized in Supplementary Table 17 for fALFF and GMV in Talairach labels, respectively.
Overlap of brain maps between alcohol and tobacco use groups
After overlapping between alcohol and tobacco use associated brain maps, AUDIT + FTND related multimodal patterns included negative fALFF in LG accompanied with negative GMV in insula, striatum and amygdala. (AUDIT + FTND-associated multimodal joint components can be found in Supplementary Fig. 2).
Associations between alcohol/tobacco use and psychotic disorder
Correlations between alcohol/tobacco/alcohol + tobacco use-associated brain regions with symptom and cognitive scores within SZ, SAD and BP groups were calculated, respectively (Fig. 3). Asterisk (*) signifies FDR for multiple comparisons. Within SZ, alcohol use-associated positive GMV in MTC, MOC, IPC and AG was correlated with WRAT (r = 0.22, p = 3.5e−05*); tobacco use-associated positive GMV in PFC was correlated with SBS (r = −0.24, p = 1.5e−03, this was also significant within males, r = -0.29, p = 1.6e−03*). Within SAD, alcohol use-associated positive GMV in MTC, MOC, IPC and AG was correlated with WRAT (r = 0.29, p = 5.2e−09*, this was also significant within males, r = 0.41, p = 1.6e−08*) and BACS tower (male) (r = 0.40, p = 1.4e−05*); tobacco use-associated positive GMV in PFC was correlated with WRAT (r = 0.23, p = 1.8e−04*, this was also significant within males, r = 0.33, p = 2.4e−04*) and BACS tower (male) (r = 0.42, p = 1.2e−03); alcohol + tobacco use-associated negative GMV in insula, striatum and amygdala was correlated with BACS (r = 0.24, p = 5.8e−03) and WRAT (r = 0.28, p = 1.3e−03). Within BP, alcohol use-associated positive fALFF in calcarine, PRC, POC and LG was correlated with SBS (r = −0.29, p = 3.3e−09*) and positive GMV in MTC, MOC, IPC and AG was correlated with WRAT (r = 0.30, p = 2.8e−04*); tobacco use-associated positive fALFF in MPFC, AG, precuneus, PCC and MTC was correlated with SBS (r = −0.30, p = 2.9e−07*, this was also significant within females, r = −0.29, p = 6.1e−05*); alcohol + tobacco use-associated negative fALLF in LG was correlated with SBS (r = −0.29, p = 7.1e−04*).
Associations between alcohol/tobacco use and depressive disorder
Correlations between alcohol/tobacco/alcohol + tobacco use-associated brain regions with symptom and cognitive scores within MDD group were also calculated (Fig. 4). Alcohol use-associated positive GMV in MTC, MOC, IPC and AG was correlated with RRS (r = 0.53, p = 3.5e−03, this was also significant within males, r = 0.76, p = 4.0e−05*) and digit symbol (r = 0.29, p = 5.8e−05*) within MDD.
Associations between alcohol/tobacco use and developmental disorder
Correlation analyses between alcohol/tobacco/alcohol+tobacco use-associated brain regions with symptom and cognitive scores within ASD and ADHD groups were performed (Fig. 5). Within ASD, alcohol use-associated negative fALFF in PFC, ACC, AG, MTC, LG and caudate was correlated with SRS mannerisms (r = −0.17, p = 3.3e−05*); tobacco use-associated positive fALFF in MPFC, AG, precuneus, PCC and MTC was correlated with SRS mannerisms (r = −0.17, p = 2.8e−05*); alcohol+tobacco use-associated negative fALFF in LG was correlated with SRS mannerisms (r = −0.17, p = 3.9e−03) within ASD. Within ADHD, alcohol use-associated negative GMV in MPFC, precuneus, PRC, MCC, ACC, insula, striatum and amygdala was correlated with verbal IQ (r = 0.17, p = 4.6e−03); tobacco use-associated negative GMV in insula, striatum, amygdala, parahippocampal, hippocampus and FG was correlated with verbal IQ (r = 0.16, p = 1.3e−04*); alcohol+tobacco use-associated negative GMV in insula, striatum and amygdala was correlated with verbal IQ (r = 0.16, p = 7.5e−03).
Besides, other associations between alcohol/tobacco/alcohol + tobacco use and psychotic, depressive and developmental disorders were added in the Supplementary Fig. 3.
Discussion
This study identified multimodal brain patterns related to alcohol and tobacco use using AUDIT/FTND-guided fusion and investigated the associations between the identified brain patterns and symptoms and cognition in psychotic, depressive and developmental disorders. Results showed that: (1) default mode network (DMN) and salience network (SN) were associated with alcohol use, whereas DMN and fronto-limbic network (FLN) were associated with tobacco use; (2) alcohol and tobacco use may have associations with symptom severity and cognitive ability of psychotic disorder through DMN and fronto-basal ganglia (FBG) (Fig. 6a); (3) alcohol and tobacco use may be correlated with cognitive deficits in depressive disorder through MTC (Fig. 6b); (4) alcohol and tobacco use may be related to both symptom and cognition in developmental disorder through DMN, SN and limbic system (LB) (Fig. 6c). The above results indicate that alcohol and tobacco use associated structural and functional brain abnormalities may be further connected with symptom severity and cognitive performance differently in 6 different psychiatric disorders.
Symptoms and cognition associated brain areas were summarized into DMN and FBG for psychotic (a), MTC for depressive (b), DMN, SN and LB for developmental (c) disorders, respectively. PRC precentral cortex, POC postcentral cortex, LG lingual gyrus, CAL calcarine, AG angular gyrus, PREC precuneus, PFC prefrontal cortex, PCC posterior cingulate cortex, MTC middle temporal cortex, IPC inferior parietal cortex, MOC middle occipital cortex, ACC anterior cingulate cortex, CAU caudate, MPFC, medial prefrontal cortex, MCC midcingulate cortex, STR striatum, INS insula, AMY, amygdala, HIP hippocampus, PH parahippocampal, FG fusiform gyrus, DMN default mode network, FBG fronto-basal ganglia, SN salience network, LB limbic system.
Alcohol use associated DMN (including MPFC, AG, precuneus, MCC and MTC) and SN (including ACC and insula) were identified from multimodal MRI. Accumulating evidence suggests that DMN abnormalities are associated with memory encoding in people who drink alcohol [38]. Consistent with our study, SN structural abnormalities in people who drink alcohol have been reported to be associated with memory [39]. These results suggest that DMN and SN abnormalities associated with alcohol use may underlie the neural mechanisms that induce behavioral deficits in people who drink alcohol, particularly memory deficits. Tobacco use associated DMN (including MPFC, AG, precuneus, PCC and MTC) and FLN (including PFC, amygdala, hippocampus, parahippocampal and striatum) were identified. Previous studies have found a significant reduced connectivity strength within the DMN of people who smoke tobacco [23]. Nicotine biases resting-state brain function away from the DMN and toward the SN, which may reduce internally focused cognition and enhance salience processing [40]. Nicotine modulates affect by increasing the concentration of dopamine in the FLN [41], which involves the mesocorticolimbic dopamine system, contributing to the processing of rewarding sensory stimuli during the overall shaping of successful behaviors [42, 43]. Hence, this study suggests that DMN and FLN abnormalities may underlie the attentional and emotional deficits in substance users.
The neuroimaging investigations involving the associations between co-morbid substances and psychotic and depressive disorders are complex. Alcohol and tobacco use associated DMN (including PFC, AG, precuneus, PCC and MTC) was correlated with symptoms in psychotic disorders. PFC D2 receptors were associated with negative symptom severity in SZ [44, 45]. Several studies reported group differences in PFC brain volume between patients with comorbid SZ and alcohol use disorder compared to individuals with either diagnosis alone [46]. Besides, lower in-vivo D2 receptor availability in the PFC was found in smokers compared to nonsmokers [47]. Prior studies suggest that abnormalities in AG and MTG, and illness severity are likely to be correlated with one another in SZ [48]. Correlation analysis has shown that the decreased precuneus activation negatively correlated with the depression symptom levels in BP compared to healthy controls (HCs) [49]. Clinical severity may be related to impaired function of the PCC in SAD [50]. Alcohol and tobacco use associated FBG (including PFC, striatum and amygdala) were related to cognitive deficits in psychotic disorder. PFC is considered as a core region in psychotic disorder that is related to cognitive impairment [51]. Nicotine facilitates dopamine release in the striatum [52] and greater amygdala reactivity to acute stress correlates with greater quantity and frequency of alcohol use in BP [53]. The FBG is considered to be involved in processing and integrating many complex and diverse cognitive functions [54]. Our results suggest that the DMN and FBG are two key brain networks that reveal potential links of the neural mechanisms between alcohol/tobacco use and the symptoms/cognition in psychotic disorder. Alcohol and tobacco use associated MTC was related to cognition in depressive disorder. A one-way analysis of variance found significant GM abnormalities in right MTC among the MDD and HCs [55], which was connected with rumination (a symptom of MDD) and executive control [56]. This result suggests that MTC is a key brain region that underlines the neural mechanisms in cognitive deficits in depressive disorder comorbid with alcohol/tobacco use.
There are several neuroimaging studies in developmental disorders examining the associations with co-morbid substance use, and the findings are complex. The alcohol and tobacco use associated DMN (including MPFC, AG, precuneus, PCC and MTC) was related to some symptoms in our developmental sample. The MPFC has been implicated in anxiety symptoms and executive dysfunction [57]. A dysfunction of the AG is reported to be associated with social deficits in ASD patients [58]. ADHD and ASD show abnormal activity and structure in the precuneus and MTC [59, 60], which were associated with social and communication dysfunction. Abnormalities in PCC have been shown to correlate with the symptom severity of ASD [61], especially the ability to interpret social signals [62]. In our sample, two alcohol and tobacco use associated networks, SN (including ACC and insula) and LB (including hippocampus, parahippocampal, and amygdala), were related to cognition in developmental disorders. Reports have shown SN connectivity in ASD and ADHD to be related to operating social cognition and self-referential processing [63,64,65]. The amygdala is involved in the production and recognition of memory formation [66], self-awareness and social perception [67], and it has been consistently implicated in the social cognitive deficits of ASD [68]. Hippocampus and parahippocampal are involved in long-term and working memory, and larger volumes were found in children with ADHD [69, 70]. In the current study, reduced GMV (in the alcohol and tobacco use associated DMN, SN and LB networks) was associated with worse cognition. Actually, all the associations between GM and cognitive performance, across diagnosis, co-morbid substance use and network, were in the positive direction: the thicker the cortex, the better performance. This is consistent with the broad literature of neuro-psychological function and brain structure [71]. Within psychosis, alcohol use associated positive GMV in MTC and MOC was correlated with WRAT, which provides measure of academic skills and diagnoses learning disabilities. As a common cognitive measure of psychiatric disorders, WRAT has significant associations with brain regions affected by alcohol use. Thus, alcohol use psychosis patients may have a specific association in academic skills (i.e., the reading skills), as compared to their nonusing counterparts.
In terms of symptoms, the negative relationship between GMV and SBS in SZ is also consistent with the broad literature in psychosis. Global reductions in GMV are present in both disorders but are greater in SZ than BP disorder [72,73,74]. A larger SBS score means the subject is closer to the SZ than to the BP end of the psychotic spectrum. The positive relationship between GMV and ruminations is not consistent with the broad structural MRI literature in MDD that reports volume reductions [75, 76]. However, ruminations are not core symptoms of MDD so this association should be interpreted cautiously. Only two associations with the resting-state fMRI metric, FALFF, were apparent in our sample. In ASD, greater fALFF in the DMN was linked to lower mannerism ratings. Similarly, in BP lower SBS (closer to the BP end of the psychosis spectrum) was related to higher fALFF in the DMN. In BP antipsychotic-naïve patients, fALFF has been reported increased in the left MTG and postcentral gyri [77]. Also left fALFF positively correlated with verbal fluency in BP, MDD and HCs [77]. Interpretation on the meaning of the directionality of an association with FALFF is far from clear [78], but the results from Chai et al. [77] suggest that, at least for the MTG, a greater value is associated with improved neuropsychological performance.
Our overall hypothesis was that some of the shared networks between alcohol/tobacco use and several co-morbid disorders, would be particularly relevant to the severity of symptoms and cognitive deficits in those disorders. It means that some of the brain circuits impacted by substance use are also involved in neuropsychiatric disorders. For psychotic disorder amongst tobacco use, the strongest previously reported association with negative symptom (r = −0.17) was in the PFC [79, 80]. In our study we found the PFC related to tobacco use to have a stronger correlation with negative symptom (r = −0.24) in psychotic subjects. For depressive disorder amongst alcohol use, the strongest previously reported association with depressive cognition (r = 0.33) was in the MTC [81, 82]. In our study we found the MTC related to alcohol use to have a stronger correlation with cognitive deficit (r = 0.53) in depressed subjects. Finally, for developmental disorder amongst tobacco use, the strongest previously reported association with developmental symptom (r = 0.10) was in the ACC [83, 84]. In our study we found the ACC related to alcohol use to have a stronger correlation with symptom (r = 0.17) in the developmental disorder group. This study serves as a preliminary exploration into the potential associations between alcohol/tobacco use and brain networks across a range of psychiatric disorders. Our intention is not to replace an analysis of comorbid disorders but rather to offer a complementary perspective.
For sex-specific results, BACS tower was correlated with alcohol and tobacco use in males only in SAD, which may indirectly indicate that alcohol and tobacco use have greater effects on executive function in male SAD patients [85]. The effects of alcohol and tobacco use on brain structure and function display sexual dimorphisms. Alcoholic males show detectable deficits in cortical gray and white matter volumes as well as enlargement of sulci, lateral and third ventricles, relative to alcoholic females [86]. Females who smoke tobacco had lower GMV in the left cerebellum, ventral medial cortex and medial orbitofrontal cortex with no areas of greater GMV [87]. Males who smoke tobacco had lower GMV in bilateral cerebellum and greater GMV in bilateral parahippocampus extending into the left putamen [88]. Comorbidities with alcohol/tobacco use and 6 psychiatric disorders in male and female individuals exhibit distinct patterns in symptoms and cognition. Gender differences in SZ affect many domains, including symptoms, cognition, comorbidity and mortality [87]. Tobacco is strongly related to male gender and violent behavior after onset of SAD compared to females [89]. Tobacco has a greater impact on reducing the life expectancy of female patients with BP disorder than male patients [90]. A previous study suggests a stronger tobacco use exposure-MDD association in females than in males [91]. Stronger associations between hyperactivity-impulsivity and heavy alcohol use in adolescent females than males in ADHD [92] were reported. By including sex difference analyses, we aim to analyze the relationship between alcohol/ tobacco use and 6 psychiatric disorders from a sex-specific perspective, which may help develop more tailored and effective interventions and strategies for both male and female patients.
There are several limitations to consider in this study. First, the multimodal brain imaging data were collected from multiple sites. The lack of standardization across MRI acquisitions, inclusion criteria, and clinical assessments should be considered. However, prior to fusion analysis, site and other confounding factors including age, gender and head motion were regressed out from fALFF and GMV matrices, which helped diminish possible confounds of site, age, gender and motion as major covariates for the current investigation. We additionally performed the AUDIT/FTND-guided fusion after ComBat harmonization to compare ComBat harmonization and linear regression of the identified AUDIT/FTND-associated multimodal patterns. It was clear that ComBat harmonization and linear regression were highly similar (>86%, Supplementary Table 18) in both alcohol use (Supplementary Fig. 4a, b) and tobacco use (Supplementary Fig. 4c, d) related maps. Second, the fusion network was initially identified in alcohol and tobacco use populations and then applied to various disorders without considering co-morbid substance use in those disorders (substance use information was not available for BSNIP, MDD subjects, ABIDE-II and ADHD-2000 project participants). It is possible that the alcohol and tobacco use associated networks are different in psychotic, depressive and developmental disorders than in otherwise healthy individuals. However, this is a preliminary investigation about the potential associations between substance use and different psychiatric disorders, and a more informative design would have examined multimodal brain networks in (a) alcohol/tobacco use subjects, (b) psychotic subjects with and without alcohol/tobacco use, (c) depressive subjects with and without alcohol/tobacco use and (d) developmental disorders with and without alcohol/tobacco use. Then the extent to which any overlap between the affected networks is attributable to substance use and/or psychiatric disease could be more clearly interpreted. Third, the analyses are cross-sectional so interpretations of causality are problematic. A more robust test of these relationships would involve a longitudinal MRI study of substances, using patients of 6 disorders before and after alcohol or tobacco cessation therapy. We would expect that patients who successfully quit such substance would show normalization in related brain regions, as well as improvement in symptoms and cognitive deficits. Forth, subjects with alcohol/tobacco use who participated in the assessment of AUDIT/FTND were all used in the multimodal fusion analysis. The AUDIT/FTND scores of some subjects were under the WHO harmful/hazardous alcohol/tobacco use level. This may impact the understanding of the alcohol/tobacco related results to severe samples. Finally, the psychiatric populations had other common potential confounds, like psychotropic medications.
In summary, to the best of our knowledge, this is the first attempt to identify alcohol and tobacco use-related brain patterns and further investigate the associations between the identified brain patterns and different clinical subdomains in psychotic, depressive and developmental disorders. Alcohol and tobacco use related DMN, SN and FLN multimodal MRI brain networks were associated with the symptoms and cognition in psychotic, depressive and developmental disorders differently. There are two broad implications from our results. Methodologically, co-morbid substance use has to be accounted for in neuroimaging studies of psychotic, depressive developmental populations. In clinical terms, alcohol and tobacco use disorders are extremely common and especially difficult to treat amongst mentally-ill populations. However, our results, like the overwhelming majority of neuroimaging studies, have no current clinical relevance to the management of these psychiatric disorders. Still, if our findings are confirmed, we can envision future translational studies. For example, if tobacco use represents in part an attempt by psychotic patients to self-treat negative symptoms and cognitive deficits, future studies using neurostimulation targeting tobacco use related DMN and/or FBG brain networks, may result in improvements of in these symptoms. Understanding the brain pathophysiology in these co-morbid conditions may assist clinical scientists in the development of better substance cessation approaches.
Data availability
The supervised fusion code has been released and integrated in the Fusion ICA Toolbox (FIT, https://trendscenter.org/software/FIT/), which can be downloaded and used directly by users worldwide. The multimodal MRI data of psychiatric disorders (SZ, SAD, BP and MDD) and substance use (alcohol use and tobacco use) can be accessed upon request to Vince D. Calhoun and Jing Sui. The developmental disorders (ASD and ADHD) data can be accessed upon application from ABIDE and ADHD-200.
References
He H, Pan L, Cui Z, Sun J, Yu C, Cao Y, et al. Smoking prevalence, patterns, and cessation among adults in Hebei province, central China: implications from China National Health Survey (CNHS). Front Public Health. 2020;8. https://doi.org/10.3389/fpubh.2020.00177.
Bartoli F, Carretta D, Crocamo C, Schivalocchi A, Brambilla G, Clerici M, et al. Prevalence and correlates of binge drinking among young adults using alcohol: a cross-sectional survey. Biomed Res Int. 2014. https://doi.org/10.1155/2014/930795.
Katulanda P, Ranasinghe C, Rathnapala A, Karunaratne N, Sheriff, R Matthews D. Prevalence, patterns and correlates of alcohol consumption and its’ association with tobacco smoking among Sri Lankan adults: a crosssectional study. Bmc Public Health. 2014;14. https://doi.org/10.1186/1471-2458-14-612.
Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction. 2018;113:1905–26. https://doi.org/10.1111/add.14234.
MacKillop J, Agabio R, Feldstein Ewing SW, Heilig M, Kelly JF, Leggio L, et al. Hazardous drinking and alcohol use disorders. Nat Rev Dis Prim. 2022;8 1:81.
Perez-Garcia JM, Cadaveira F, Canales-Rodriguez EJ, Suarez-Suarez S, Holguin SR, Corral M, et al. Effects of persistent binge drinking on brain structure in emerging adults: a longitudinal study. Front Psychiatry. 2022;13. https://doi.org/10.3389/fpsyt.2022.935043.
Liang HJ, Ernst T, Cunningham E, Chang LD. Contributions of chronic tobacco smoking to HIV-associated brain atrophy and cognitive deficits. Aids. 2022;36:513–24. https://doi.org/10.1097/qad.0000000000003138.
Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJL, Comparative Risk Assessment Collaborating G. Selected major risk factors and global and regional burden of disease. Lancet (Lond, Engl). 2002;360:1347–60. https://doi.org/10.1016/s0140-6736(02)11403-6.
Torrens M, Gilchrist G, Domingo-Salvany A. Psychiatric comorbidity in illicit drug users: substance-induced versus independent disorders. Drug Alcohol Depend. 2011;113 2-3:147–56.
Conway KP, Compton WM, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67 2:247–57.
Mallet J, Le Strat Y, Schurhoff F, Mazer N, Portalier C, Andrianarisoa M, et al. Tobacco smoking is associated with antipsychotic medication, physical aggressiveness, and alcohol use disorder in schizophrenia: results from the FACE-SZ national cohort. Eur Arch Psych Clin Neurosci 2019;269:449–57. https://doi.org/10.1007/s00406-018-0873-7.
Qi S, Sui J, Pearlson G, Bustillo JR, Perrone-Bizzozero NI, Kochunov PV, et al. Derivation and utility of schizophrenia polygenic risk associated multimodal MRI frontotemporal network. Nat Commun. 2022;13:4929.
Mazumder AH, Barnett J, Lindberg N, Torniainen-Holm M, Lahteenvuo M, Lahdensuo K, et al. Reaction time and visual memory in connection with alcohol use in schizophrenia and schizoaffective disorder. Brain Sci. 2021;11:16 https://doi.org/10.3390/brainsci11060688.
Baethge C, Tondo L, Lepri B, Baldessarini RJ. Coffee and cigarette use: association with suicidal acts in 352 Sardinian bipolar disorder patients. Bipolar Disord. 2009;11:494–503. https://doi.org/10.1111/j.1399-5618.2009.00727.x.
Wang KS, Liu Y, Ouedraogo Y, Wang NY, Xie X, Xu C, et al. Principal component analysis of early alcohol, drug and tobacco use with major depressive disorder in US adults. J Psychiatr Res. 2018;100:113–20. https://doi.org/10.1016/j.jpsychires.2018.02.022.
Karlen MH, Stalheim J, Berglund K, Wennberg P. Autistic personality traits and treatment outcome for alcohol use disorders. J Nerv Ment Dis. 2021;209:665–73. https://doi.org/10.1097/nmd.0000000000001357.
Lewis AS, van Schalkwyk GI, Lopez MO, Volkmar FR, Picciotto MR, Sukhodolsky DG. An exploratory trial of transdermal nicotine for aggression and irritability in adults with autism spectrum disorder. J Autism Develop Disord. 2018;48:2748–57.
Potter AS, Newhouse PA. Acute nicotine improves cognitive deficits in young adults with attention-deficit/hyperactivity disorder. Pharmacol Biochem Behav. 2008;88:407–17.
Qi SL, Bustillo J, Turner JA, Jiang R, Zhi DM, Fu ZN, et al. The relevance of transdiagnostic shared networks to the severity of symptoms and cognitive deficits in schizophrenia: a multimodal brain imaging fusion study. Transl Psychiatr 2020;10:10 https://doi.org/10.1038/s41398-020-0834-6.
Le V, Kirsch DE, Tretyak V, Weber W, Strakowski SM, Lippard ETC. Recent perceived stress, amygdala reactivity to acute psychosocial stress, and alcohol and cannabis use in adolescents and young adults with bipolar disorder. Front Psychiatry. 2021;12:9 https://doi.org/10.3389/fpsyt.2021.767309.
Uhlmann A, Bandelow B, Stein DJ, Bloch S, Engel KR, Havemann-Reinecke U, et al. Grey matter structural differences in alcohol-dependent individuals with and without comorbid depression/anxiety-an MRI study. Eur Arch Psych Clin Neurosci. 2019;269:285–94. https://doi.org/10.1007/s00406-018-0870-x.
Lange S, Rehm J, Anagnostou E, Popova S. Prevalence of externalizing disorders and Autism Spectrum Disorders among children with Fetal Alcohol Spectrum Disorder: systematic review and meta-analysis. Biochem Cell Biol. 2018;96:241–51. https://doi.org/10.1139/bcb-2017-0014.
Weiland BJ, Sabbineni A, Calhoun VD, Welsh RC, Hutchison KE. Reduced executive and default network functional connectivity in cigarette smokers. Hum Brain Mapp. 2015;36:872–82.
Liang C, Pearlson G, Bustillo J, Kochunov P, Turner JA, Wen X, et al. Psychotic symptom, mood, and cognition-associated multimodal MRI reveal shared links to the salience network within the psychosis spectrum disorders. Schizophr Bull. 2023;49:172–84. https://doi.org/10.1093/schbul/sbac158.
Qi S, Yang X, Zhao L, Calhoun VD, Perrone-Bizzozero N, Liu S, et al. MicroRNA132 associated multimodal neuroimaging patterns in unmedicated major depressive disorder. Brain. 2018;141:916–26. https://doi.org/10.1093/brain/awx366.
Qi S, Calhoun VD, Zhang D, Miller J, Deng Z-D, Narr KL, et al. Links between electroconvulsive therapy responsive and cognitive impairment multimodal brain networks in late-life major depressive disorder. BMC Med. 2022;20:477.
Di Martino A, Yan CG, Li Q, Denio E, Castellanos FX, Alaerts K, et al. The autism brain imaging data exchange: towards a large-scale evaluation of the intrinsic brain architecture in autism. Mol Psychiatr 2014;19:659–67. https://doi.org/10.1038/mp.2013.78.
Di Martino A, O’Connor D, Chen B, Alaerts K, Anderson JS, Assaf M, et al. Data descriptor: enhancing studies of the connectome in autism using the autism brain imaging data exchange II. Sci Data. 2017;4:15. https://doi.org/10.1038/sdata.2017.10.
Keshavan MS, Morris DW, Sweeney JA, Pearlson GD, Thaker GK, Seidman LJ, et al. A dimensional approach to the psychosis spectrum between bipolar disorder and schizophrenia: The Schizo-Bipolar Scale. Schizophrenia Res. 2011;133:250–4.
Hill SK, Reilly JL, Keefe RSE, Gold JM, Bishop JR, Gershon ES, et al. Neuropsychological impairments in schizophrenia and psychotic bipolar disorder: findings from the bipolar-schizophrenia network on intermediate phenotypes (B-SNIP) study. Am J Psychiatr. 2013;170:1275–84. https://doi.org/10.1176/appi.ajp.2013.12101298.
Nolen-Hoeksema S, Morrow J, Fredrickson BL. Response styles and the duration of episodes of depressed mood. J Abnorm Psychol. 1993;102:20.
Benson NF, Hulac DM, Kranzler JH. Independent examination of the Wechsler Adult Intelligence Scale-Fourth Edition (WAIS-IV): what does the WAIS-IV measure? Psychol Assess. 2010;22 1:121–30.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Constantino JN, Gruber CP. Social responsiveness scale: SRS-2. Torrance, CA: Western Psychological Services; 2012.
Conners CK, Sitarenios G, Parker JD, Epstein JN. The revised Conners’ Parent Rating Scale (CPRS-R): factor structure, reliability, and criterion validity. J Abnorm child Psychol. 1998;26:257–68.
Mccrimmon A, Smith AD. Review of the Wechsler abbreviated scale of intelligence, second edition (WASI-II). J Psychoeduc Assess. 2013;31:337–41.
Qi SL, Calhoun VD, van Erp TGM, Bustillo J, Damaraju E, Turner JA, et al. Multimodal fusion with reference: searching for joint neuromarkers of working memory deficits in schizophrenia. IEEE Trans Med Imaging. 2018;37:93–105. https://doi.org/10.1109/tmi.2017.2725306.
Fang X, Deza-Araujo YI, Petzold J, Spreer M, Riedel P, Marxen M, et al. Effects of moderate alcohol levels on default mode network connectivity in heavy drinkers. Alcohol Clin Exp Res.2021;45:1039–50.
Galandra C, Basso G, Manera MR, Crespi C, Giorgi I, Vittadini G, et al. Salience network structural integrity predicts executive impairment in alcohol use disorders. Sci Rep. 2018;8:14481.
Wang KS, Brown K, Frederick BB, Moran LV, Olson DP, Pizzagalli DA, et al. Nicotine acutely alters temporal properties of resting brain states. Drug Alcohol Depend. 2021;226:108846.
Benowitz NL. Pharmacology of nicotine: addiction, smoking-induced disease, and therapeutics. Annu Rev Pharmacol Toxicol. 2009;49:57–71.
De Biasi M, Dani JA. Reward, addiction, withdrawal to nicotine. Annu Rev Neurosci. 2011;34:105–30.
Qi S, Schumann G, Bustillo JR, Turner JA, Jiang R, Zhi D, et al. Reward processing in novelty seekers: a transdiagnostic psychiatric imaging biomarker. Biol Psychiatry. 2021;90:529–39.
Brisch R, Saniotis A, Wolf R, Bielau H, Bernstein H-G, Steiner J, et al. The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Front Psychiatry. 2014;5:110.
McCutcheon RA, Abi-Dargham A, Howes OD. Schizophrenia, dopamine and the striatum: from biology to symptoms. Trends Neurosci. 2019;42:205–20.
Mathalon DH, Pfefferbaum A, Lim KO, Rosenbloom MJ, Sullivan EV. Compounded brain volume deficits in schizophrenia-alcoholism comorbidity. Arch Gen Psychiatry. 2003;60:245–52.
Brown AK, Mandelkern MA, Farahi JB, Robertson CL, Ghahremani DG, Sumerel B, et al. Sex differences in striatal dopamine D2/D3 receptor availability in smokers and non-smokers. Int J Neuropsychopharmacol. 2012;15 7:989–94.
Gao Y, Tong X, Hu J, Huang H, Guo T, Wang G, et al. Decreased resting-state neural signal in the left angular gyrus as a potential neuroimaging biomarker of schizophrenia: an amplitude of low-frequency fluctuation and support vector machine analysis. Front Psychiatry. 2022;13:949512.
Sun F, Liu Z, Yang J, Fan Z, Xi C, Cheng P, et al. Shared and distinct patterns of dynamical degree centrality in bipolar disorder across different mood states. Front Psychiatry. 2022;13:941073.
Wada M, Nakajima S, Tarumi R, Masuda F, Miyazaki T, Tsugawa S, et al. Resting-state isolated effective connectivity of the cingulate cortex as a neurophysiological biomarker in patients with severe treatment-resistant schizophrenia. J Personal Med. 2020;10:89.
Lesh TA, Niendam TA, Minzenberg MJ, Carter CS. Cognitive control deficits in schizophrenia: mechanisms and meaning. Neuropsychopharmacology. 2011;36:316–38.
Schmidt HD, Rupprecht LE, Addy NA. Neurobiological and neurophysiological mechanisms underlying nicotine seeking and smoking relapse. Mol Neuropsychiatry. 2018;4:169–89.
Le V, Kirsch DE, Tretyak V, Weber WA, Strakowski SM, Lippard ETC. Recent perceived stress, amygdala reactivity to acute psychosocial stress, and alcohol and cannabis use in adolescents and young adults with bipolar disorder. Front Psychiatry. 2021;12:767309.
Li X, Luo F, Shi L-H, Woodward DJ, Chang J. Ensemble neural activity of the frontal cortical basal ganglia system predicts reaction time task performance in rats. Neurosci Res. 2011;71:149–60.
Ma CQ, Ding J, Li J, Guo W, Long Z, Liu F, et al. Resting-state functional connectivity bias of middle temporal gyrus and caudate with altered gray matter volume in major depression. PLoS ONE. 2012;7:e45263.
Zhu Z-Q, Wang Y, Lau WK-W, Wei X, Liu Y, Huang R, et al. Hyperconnectivity between the posterior cingulate and middle frontal and temporal gyrus in depression: based on functional connectivity meta-analyses. Brain Imaging Behav. 2021;16:1538–51.
van Noordt SJR, Segalowitz SJ. Performance monitoring and the medial prefrontal cortex: a review of individual differences and context effects as a window on self-regulation. Front Hum Neurosci. 2012;6:197.
Assaf M, Jagannathan K, Calhoun VD, Miller L, Stevens MC, Sahl R, et al. Abnormal functional connectivity of default mode sub-networks in autism spectrum disorder patients. NeuroImage. 2010;53:247–56.
Cherkasova M V, Hechtman LT. Neuroimaging in attention-deficit hyperactivity disorder: beyond the frontostriatal circuitry. Can J Psychiatry. 2009;54:651–64.
Firouzabadi FD, Ramezanpour S, Firouzabadi MD, Yousem IJ, Puts NAJ, Yousem DM. Neuroimaging in attention-deficit/hyperactivity disorder: recent advances. Am J Roentgenol. 2021.
Kennedy DP, Redcay E, Courchesne E. Failing to deactivate: Resting functional abnormalities in autism. Proc Natl Acad Sci USA. 2006;103:8275–80. https://doi.org/10.1073/pnas.0600674103.
Leung M-K, Lau WK-W. Resting-state abnormalities of posterior cingulate in autism spectrum disorder. Prog Mol Biol Transl Sci. 2020;173:139–59.
Green SA, Hernandez LM, Bookheimer SY, Dapretto M. Salience network connectivity in autism is related to brain and behavioral markers of sensory overresponsivity. J Am Acad Child Adolesc Psychiatry. 2016;55 7:618–26.e611.
Cai W, Griffiths KR, Korgaonkar MS, Williams LM, Menon V. Inhibition-related modulation of salience and fronto-parietal networks predicts cognitive control ability and inattention symptoms in children with ADHD. Mol Psychiatr 2019;26:4016–25.
Toyomaki A, Murohashi H. “Salience network” dysfunction hypothesis in autism spectrum disorders. Jpn Psychol Res. 2013;55:175–85.
Packard MG, Cahill L. Affective modulation of multiple memory systems. Curr Opin Neurobiol. 2001;11:752–6.
Goldin PR, McRae K, Ramel W, Gross JJ. The neural bases of emotion regulation: reappraisal and suppression of negative emotion. Biol Psychiatry. 2008;63:577–86.
Gibbard CR, Ren J, Skuse DH, Clayden JD, Clark CA. Structural connectivity of the amygdala in young adults with autism spectrum disorder. Hum Brain Mapp 2017;39:1270–82.
Plessen KJ, Bansal R, Zhu H, Whiteman R, Amat JA, Quackenbush GA, et al. Hippocampus and amygdala morphology in attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63 7:795–807.
Carmona S, Vilarroya Ó, Bielsa A, Trémols V, Soliva JC, Rovira M, et al. Global and regional gray matter reductions in ADHD: a voxel-based morphometric study. Neurosci Lett. 2005;389:88–93.
Ramanoël S, Hoyau E, Kauffmann L, Renard F, Pichat C, Boudiaf N, et al. Gray matter volume and cognitive performance during normal aging. A voxel-based morphometry study. Front Aging Neurosci. 2018;10:235.
Ellison-Wright I, Bullmore ET. Anatomy of bipolar disorder and schizophrenia: a meta-analysis. Schizophr Res. 2010;117:1–12.
Gupta CN, Calhoun VD, Rachakonda S, Chen J, Patel V, Liu J, et al. Patterns of gray matter abnormalities in schizophrenia based on an international mega-analysis. Schizophr Bull. 2015;41:1133–42.
Selvaraj S, Arnone D, Job DE, Stanfield AC, Farrow TFD, Nugent AC, et al. Grey matter differences in bipolar disorder: a meta‐analysis of voxel‐based morphometry studies. Bipolar Disord. 2012;14:135–45.
Shad MU, Muddasani S, Rao U. Gray matter differences between healthy and depressed adolescents: a voxel-based morphometry study. J Child Adolesc Psychopharmacol. 2012;22 3:190–7.
Hellewell SC, Welton T, Maller JJ, Lyon M, Korgaonkar MS, Koslow SH, et al. Profound and reproducible patterns of reduced regional gray matter characterize major depressive disorder. Transl Psychiatr. 2019;9:176.
Chai X, Zhang R, Xue C, Li Z, Xiao W, Huang QL, et al. Altered patterns of the fractional amplitude of low-frequency fluctuation in drug-naive first-episode unipolar and bipolar depression. Front Psychiatry. 2020;11:587803.
Egorova N, Veldsman M, Cumming TB, Brodtmann A. Fractional amplitude of low-frequency fluctuations (fALFF) in post-stroke depression. NeuroImage : Clin. 2017;16:116–24.
Padmanabhan JL, Tandon N, Haller CS, Mathew IT, Eack SM, Clementz BA, et al. Correlations between brain structure and symptom dimensions of psychosis in schizophrenia, schizoaffective, and psychotic bipolar I disorders. Schizophr Bull. 2015;41:154–62.
Fritz H-CJ, Wittfeld K, Schmidt CO, Domin M, Grabe HJ, Hegenscheid K, et al. Current smoking and reduced gray matter volume—a voxel-based morphometry study. Neuropsychopharmacology. 2014;39:2594–2600.
Zhao K, Xie H, Fonzo GA, Tong X, Carlisle NB, Chidharom M, et al. Individualized fMRI connectivity defines signatures of antidepressant and placebo responses in major depression. Mol Psychiatry. 2022;28:2490–9.
Ruan X, Song Z, Zhang J, Yu T, Chen J, Zhou T. Alterations of brain activity in patients with alcohol use disorder: a resting-state fMRI study. BMC Psychiatry. 2023;23:894.
Bayard F, Nymberg Thunell C, Abé C, Almeida R, Banaschewski T, Barker GJ, et al. Distinct brain structure and behavior related to ADHD and conduct disorder traits. Mol Psychiatry. 2020;25:3020–33.
Chen Y, Chaudhary S, Wang W, Li CSR. Gray matter volumes of the insula and anterior cingulate cortex and their dysfunctional roles in cigarette smoking. Addict Neurosci. 2021;1:100003.
Kaneda Y, Sumiyoshi T, Keefe RSE, Ishimoto Y, Numata S, Ohmori T. Brief assessment of cognition in schizophrenia: validation of the Japanese version. Psychiatry Clin Neurosci. 2007;61:602–9.
Pfefferbaum A, Rosenbloom MJ, Deshmukh A, Sullivan EV. Sex differences in the effects of alcohol on brain structure. Am J Psychiatry. 2001;158:188–97.
Sommer IEC, Tiihonen J, van Mourik AG, Tanskanen AJ, Taipale H. The clinical course of schizophrenia in women and men—a nation-wide cohort study. NPJ Schizophr. 2020;6:12.
Franklin TR, Wetherill RR, Jagannathan K, Johnson B, Mumma JM, Hager NM, et al. The effects of chronic cigarette smoking on gray matter volume: influence of sex. PLoS ONE. 2014;9:e104102.
Bosgelmez, S, Yıldız, M. Cigarette consumption and related factors in schizophrenia, schizoaffective disorder and delusional disorder. Düşünen Adam. 2017;30:233–42.
Chesney E, Robson DC, Patel R, Shetty H, Richardson S, Chang C-K, et al. The impact of cigarette smoking on life expectancy in schizophrenia, schizoaffective disorder and bipolar affective disorder: an electronic case register cohort study. Schizophr Res. 2021;238:29–35.
Fan Z, Gong X, Xu H, Wang H-Z, Zeng N, Li L, et al. Gender differences in the associations between tobacco smoke exposure and depressive symptoms among U.S. adults: NHANES 2007-18. J Psychiatric Res. 2021;146:249–57.
Elkins IJ, Saunders GRB, Malone SM, Keyes MA, McGue M, Iacono WG. Associations between childhood ADHD, gender, and adolescent alcohol and marijuana involvement: a causally informative design. Drug Alcohol Depend. 2017;184:33–41.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (62376124), the Natural Science Foundation of Jiangsu Province, China (BK20220889), the Key Research and Development Plan of Jiangsu Province, China (BE2023668), and the National Institutes of Health (R01MH118695).
Author information
Authors and Affiliations
Contributions
LQ and CL performed the data analysis and wrote the initial draft. SQ conceptualized the study and wrote the paper. JRB, PK, RJ, DZ, XY, DZ and VMV revised the paper. KEH provided the alcohol and tobacco use data. JS contributed the MDD data. VDC provided data of psychosis and developmental disorders. ZF preprocessed the fMRI and sMRI.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study adhered to the ethical principles outlined in the Declaration of Helsinki. Ethical approval was granted by each relevant Ethics Committee, and informed consent was obtained from each subject according to each site’s Institutional Review Boards.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qiu, L., Liang, C., Kochunov, P. et al. Associations of alcohol and tobacco use with psychotic, depressive and developmental disorders revealed via multimodal neuroimaging. Transl Psychiatry 14, 326 (2024). https://doi.org/10.1038/s41398-024-03035-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-024-03035-2