Abstract
This state-of-the-art review explores the relationship between depression and diabetes, highlighting the two-way influences that make treatment challenging and worsen the outcomes of both conditions. Depression and diabetes often co-occur and share genetic, lifestyle, and psychosocial risk factors. Lifestyle elements such as diet, physical activity, and sleep patterns play a role on the development and management of both conditions, highlighting the need for integrated treatment strategies. The evidence suggests that traditional management strategies focusing on either condition in isolation fall short of addressing the intertwined nature of diabetes and depression. Instead, integrated care models encompassing psychological support and medical management are recommended to improve treatment efficacy and patient adherence. Such models require collaboration across multiple healthcare disciplines, including endocrinology, psychiatry, and primary care, to offer a holistic approach to patient care. This review also identifies significant patient-related barriers to effective management, such as stigma, psychological resistance, and health literacy, which need to be addressed through patient-centered education and support systems. Future directions for research include longitudinal studies in diverse populations to further elucidate causal relationships and the exploration of novel therapeutic targets, as well as the effectiveness of healthcare models aimed at preventing the onset of one condition in individuals diagnosed with the other.
Similar content being viewed by others
Introduction
Diabetes and depression are global health problems with a rising prevalence, affecting 10.5 and 5% of the world population, respectively [1, 2]. Depression is a disorder characterized by a loss of interest in daily activities, fatigue, low mood, and cognitive symptoms that impair daily functioning [3]. Diabetes is a multifactorial metabolic disease characterized by hyperglycemia due to insulin deficiency or insulin resistance (IR) [4]. IR, a hallmark of type 2 diabetes mellitus (T2DM), manifests in varied tissue-specific forms. Peripheral IR primarily involves reduced insulin-mediated glucose uptake by skeletal muscle and adipose tissue, driven by defects in the insulin receptor substrate and downstream signaling pathways such as phosphoinositide 3-kinase (PI3K)/protein kinase B (Akt), leading to diminished translocation of glucose transporter type 4 (SLC2A4/GLUT4) and glucose uptake [5]. Conversely, brain IR, less recognized but equally important, pertains to impaired insulin signaling in neuronal and glial cells [6]. This central form of IR involves alterations in similar pathways but manifests distinctively in reduced synaptic plasticity and neurotransmitter regulation, impacting mood and cognitive functions [6]. Notably, brain IR is implicated in neurodegenerative processes by affecting amyloid-beta metabolism and tau phosphorylation, linking it to both cognitive decline and mood disorders [7, 8].
Both diabetes and depression are common chronic conditions which reduce a patient’s functionality, quality of life and life expectancy. The co-occurrence of these diseases has been extensively studied, but the underlying reasons that may affect each other remain inadequately elucidated despite several proposed hypotheses. This comorbidity is attributed to various factors, including the psychological impact of managing a chronic illness, potential shared genetic susceptibility, and common pathophysiological abnormalities, such as the dysregulation of the hypothalamic-pituitary-adrenal (HPA) axis, and inflammatory state [9,10,11].
Although there is no definitive evidence regarding the effect of diabetes type on depression, patients with major depressive disorder (MDD) have a twice as high risk of developing T2DM compared to the general population [12,13,14,15]. According to the results of a systematic review, the prevalence rate of depression is three times higher in patients with type 1 diabetes mellitus (T1DM) and more than two times higher in patients with T2DM [16]. Depression and diabetes also share sociodemographic and lifestyle risk factors. Despite the lack of reliable data, there are studies examining sex and age-related demographic variations. The prevalence of depression was found to be higher in women, irrespective of their diabetes status [16]. Although there are controversial studies [17], age may be a contributor as older people have higher risks of diabetes and depression, possibly because of physical limitations and other health problems [18]. Ageing, smoking, poor dietary habits, lack of exercise, comorbidities, poor glycemic control and obesity, which are among the risk factors of diabetes, can also be considered as risk factors for depression [19, 20], possibly due to their association with vascular complications [21, 22].
Trends over time show an increasing prevalence of depression and diabetes due to lifestyle and socioeconomic factors [23]. Moreover, the risk of hospitalizations, cardiovascular disease, and mortality was found to be high in the concurrent presence of these two conditions [24,25,26,27,28]. Further studies are thus required to better understand the interface of these two clinical challenges. Given the plethora of publications on either diabetes or depression or the cooccurrence of these conditions, a synthesis of the published literature on the occurrence of depression and diabetes is needed.
Thus, the aim of this state-of-the-art review is to explore and discuss the interface of depression and diabetes, synthesizing evidence on therapeutic strategies that address both conditions simultaneously. The unique challenge in treating patients suffering from both conditions lies in the necessity for a coordinated approach that takes into account the interplay between metabolic and mental health issues.
The bidirectional relationship between depression and diabetes
The relationship between diabetes and depression is profoundly bidirectional, with each condition influencing the onset and progression of the other [12, 29, 30]. Diabetes significantly increases the risk of developing depressive symptoms influenced by factors such as demanding self-management routines, fear of long-term complications, and the physiological stress imposed by persistent dysglycemia [31, 32]. Conversely, depression can undermine self-care behaviors that are necessary for effective diabetes management, such as regular medication adherence, appropriate dietary choices, and consistent physical activity [30, 33]. This reciprocal influence not only complicates treatment but also exacerbates the burden of each disease, leading to poorer health outcomes [14]. Understanding this bidirectional relationship is important for developing more effective, holistic treatment approaches that address both the psychological and physiological aspects of these intertwined health challenges.
Lifestyle factors influencing diabetes and depression
Poor dietary habits
Depression often leads to changes in appetite and eating behaviors, significantly contributing to the development of diabetes [34]. Individuals with depression may experience increased cravings for high-calorie, high-sugar foods, resulting in excessive caloric intake and subsequent weight gain [35, 36]. These foods, which are typically low in nutritional value but high in simple carbohydrates and unhealthy fats, exacerbates IR and promotes visceral fat accumulation, a key risk factor for T2DM [37]. This dietary pattern not only contributes to obesity but also to dyslipidemia and impaired glucose metabolism, worsening diabetes. Prospective studies have highlighted that patients with diabetes who have depression often exhibit more severe and chronic depressive symptoms, which further complicates their dietary habits and metabolic health over time [14].
Physical inactivity
Physical inactivity is a common behavioral characteristic in individuals with depression, significantly contributing to the risk of developing T2DM [38]. Depression often results in reduced motivation and energy levels, leading to decreased participation in physical activities and exercise [39]. Physical inactivity directly contributes to weight gain, increased adiposity, and the development of IR [40]. Exercise is known to enhance insulin sensitivity, promote glucose uptake in muscles, and reduce inflammatory markers [41]. Therefore, the lack of physical activity in depressed individuals exacerbates metabolic dysfunctions, creating a pathway to diabetes. Furthermore, the chronic nature of depression can lead to persistent physical inactivity, worsening metabolic outcomes over time.
Substance abuse
Substance abuse, including alcohol and tobacco use, is prevalent among individuals with depression and significantly contributes to the development of T2DM and related complications [42, 43]. Excessive alcohol intake may reduce insulin-mediated glucose uptake and harm pancreatic islet β-cells, leading to T2DM [44]. Prudent alcohol consumption, however, has been linked to lower risks of T2DM, stroke, heart failure, and all-cause mortality [45]. Similarly, smoking is associated with increased inflammation, oxidative stress, and endothelial dysfunction, all of which contribute to IR and T2DM [46]. The compounded effects of substance abuse and depression create a heightened risk for the development of diabetes through multiple metabolic and behavioral pathways [47]. Additionally, the interaction between substance abuse and depression may worsen depressive symptoms and its prognosis, leading to a vicious cycle that further complicates metabolic health [48].
Sleep disturbances
Sleep disturbances, common in individuals with depression, significantly elevate diabetes risk by impacting glucose metabolism, appetite, and weight [49]. Sleep deprivation impairs insulin secretion and glucose tolerance, contributing to T2DM risk [50]. On the other hand, extended sleep duration, often observed in atypical depression, may also alter circadian rhythm, which is important for metabolic health, reduce physical activity, and worsen insulin sensitivity, complicating glycemic control [51, 52]. Longitudinal studies reinforce this perspective, illustrating that poor glycemic control in patients with diabetes can further deteriorate sleep quality, perpetuating a detrimental cycle of worsening health outcomes [53]. Effectively addressing sleep disturbances is essential for managing both conditions, as they can exacerbate depressive symptoms and accelerate diabetes progression.
Shared genetic risk factors
Beyond shared environmental risk factors, such as poor diet, sedentary lifestyle, and disturbed sleep, which may also be direct manifestations of psychopathology, shared genetic components have been identified between MDD and T2DM [54]. These conditions are heritable and highly polygenic, with heritability estimates based on twin studies ranging from 39–72% [55, 56]. Both global and local genetic correlation analyses have established positive correlations across the entire genome and at specific genomic regions between MDD and T2DM, indicating a shared etiopathogenesis and synergistic genetic influence on both conditions [54, 57]. Colocalization analyses have pinpointed genetically correlated loci harboring putatively shared causal variants for both MDD and T2DM [57]. Variants near or overlapping genes such as MALAT1, involved in gene regulation, SCYL1, associated with intracellular trafficking, and LTBP3, part of the TGF-β signaling pathway on chromosome 11, along with DENND1A on chromosome 9, which is linked to hormonal regulation and vesicle-mediated transport, suggest mechanisms that jointly influence both disorders [57]. These findings lay a groundwork for future research to explore the specific causal pathways and develop targeted therapeutic interventions.
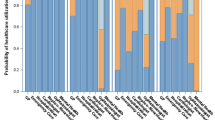
Genetic overlap between MDD and T2DM was also explored through Mendelian randomization studies, revealing insights into the causal relationships. Several MR studies using genome-wide association study (GWAS) data of European ancestry have established a causal effect of MDD on T2DM, confirmed by robust sensitivity analyses excluding horizontal pleiotropy, with 36.5% of the effect mediated by BMI [58,59,60]. Conversely, no causal link between T2DM and MDD was found in the same studies, supported by other data from a Scottish cohort [61]. Moreover, an East-Asian MR study (N = 11,506) reported a probable causal effect of T2DM on MDD [62]. Further studies on diverse ethnic samples are needed to confirm these findings and elucidate the genetic underpinnings of the T2DM-MDD relationship.
The use of polygenic risk scores (PRSs), which summarize the effect of multiple common genetic risk variants across the genome, has further contributed to our understanding of the genetic relationship between MDD and T2DM. A Russian cohort study indicated a nominal association between T2DM PRS and anhedonia, a core symptom of MDD, though the findings did not withstand correction for multiple comparisons [63]. Similarly, the US Yale-Penn sample found no significant associations between T2DM PRS and MDD in individuals of European ancestry, with only a nominal association between MDD PRS and diabetes in the same population [64]. A community sample of adolescents showed no associations between T2DM PRS and depressive symptoms [65], and research from the Taiwan Biobank linked higher MDD PRS with a slightly increased risk of T2DM. However, these results did not reach Bonferroni-corrected significance [66]. Furthermore, analysis of UK Biobank data showed associations between MDD PRS and metabolic markers such as HbA1c and glucose levels, which are relevant to diabetes pathophysiology, although these associations became non-significant in fully adjusted models [67]. In contrast, a large meta-analysis, including 12 cohorts from the Psychiatric Genomics Consortium, Generation Scotland: The Scottish Family Health Study, and UK Biobank, found statistically significant associations between T2DM PRS and MDD, particularly in cases of early onset [68]. Lastly, a Danish population-based register study identified a clear dose-response relationship where increases in T2DM PRS were associated with heightened risk for MDD in both males and females [69]. These findings from diverse PRS studies illustrate both the potential and the inherent challenges in using genetic scores to elucidate the link between MDD and T2DM. The observed inconsistencies across studies likely result from variations in sample sizes, ethnic backgrounds, and age groups. The integration of large-scale, multi-ethnic genetic data remains important for refining our understanding and enhancing the predictive precision of genetic influences on these conditions. Through such comprehensive genetic analyses, PRSs holds the potential to advance our ability to tailor preventive and therapeutic strategies based on individual genetic risk profiles, paving the way for precision medicine for IR-psychiatric multimorbidity.
Hypothalamic-pituitary-adrenal (HPA) axis and cortisol dysregulation
The dysregulation of the HPA axis is a significant pathway linking depression with T2DM [70]. Research has indicated that HPA axis hyperactivity is heightened in chronic hyperglycemic states, with severe hyperglycemic events more likely to result in depressive disorders [71]. Chronic stress, frequently associated with depression, also leads to persistent activation of the HPA axis, resulting in hypercortisolemia [72]. Elevated cortisol levels increase gluconeogenesis in the liver, impair insulin’s ability to translocate GLUT4 to the cell surface, and raise portal and peripheral free fatty acids [72, 73]. These processes collectively contribute to IR and, ultimately, T2DM [70]. Moreover, elevated cortisol levels impair neurogenesis in the hippocampus, a brain region involved in both depression and T2DM [74].
Pro-inflammatory state
Cortisol acts as a potent immuno suppressant, maintaining immune homeostasis [75]. However, when cortisol resistance occurs, it leads to chronic low-grade inflammation, which is prevalent in about 27% of people with depression [76]. A pro-inflammatory state can be observed, characterized by elevated levels of cytokines such as interleukin (IL)-1, IL-6, IL-8, interferon-γ (IFN-γ), and tumor necrosis factor-α (TNF-α) [77]. Additionally, depression raises markers for epithelial barrier dysfunction, such as zonulin, leading to increased intestinal permeability and circulating lipopolysaccharide (LPS) levels. LPS activates the inflammasome complex, which cleaves IL1-ß into its active form [78], inhibiting downstream mechanisms necessary for GLUT4 translocation, contributing further to IR [78]. Interestingly, non-depressed individuals exposed to pro-inflammatory cytokines present with depressive-like behaviors, or “sickness behaviors”, characterized by anhedonia, increased pain sensitivity, and somnolence [79]. These cytokines also contribute to IR through mechanisms including inhibitory phosphorylation of insulin receptor substrate-1 (IRS-1) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) pathway, while also promoting glucocorticoid resistance and HPA axis hyperactivity [80]. In depression, the inflammatory phenotype is particularly associated with atypical symptoms, including increased sleep and appetite, potentially leading to weight gain and local inflammation and macrophage infiltration in the adipose tissue, creating a self-perpetuating inflammatory loop [81]. Notably, pro-inflammatory cytokines are also secreted by visceral adipose tissue in obesity and, together with the inhibition of IRS-1 mediated by TNF-α, inhibition of c-Jun N-terminal kinase (JNK) and NK- κB inhibitor, serve as major inflammatory mechanisms linking obesity with IR [75, 82].
Microbiota and gut-brain axis
There is an emerging connection between IR, the gut microbiome, and mood regulation. Disruption in microbiota homeostasis enhances the risk of metabolic conditions [83, 84]. Gut microbiota-derived metabolites, such as short-chain fatty acids (SCFAs), tryptophan metabolites, and immune stimulants, are likely mediators in this process [85]. The signaling of molecules that operate primarily in the brain is disturbed by microbial factors, obesity and diabetes. This disturbance is relevant to the onset of mental illness, with the relevant molecules being neuropeptide Y, brain-derived neurotrophic factor (BDNF) and γ-aminobutyric acid (GABA) [85]. Dysbiosis, or imbalance in the gut microbiota, may disrupt homeostasis between the immune, metabolic, and nervous systems, contributing to IR and metabolic syndrome [85]. Therefore, gut dysbiosis in depressed individuals can exacerbate metabolic dysfunction and IR, linking gut health to diabetes and mental health.
Depression and metabolic syndrome: a vicious cycle
Depression is closely linked to metabolic syndrome, a cluster of conditions including abdominal obesity, dyslipidemia, hypertension, and T2DM. The prevalence of metabolic syndrome in individuals with depression is significantly higher compared to the general population [86]. Depression-driven behaviors like consuming high-calorie, low-nutrient foods and reduced physical activity [87] contribute to weight gain and increased visceral fats, which are critical in developing IR. Visceral fat secretes adipokines, such as leptin and adiponectin, influencing inflammatory responses and insulin sensitivity [82]. Altered adipokine levels have also been found in depressed individuals, albeit showing some differences related to sex, age, and body mass index [88]. These alterations could further promote IR and metabolic dysfunction in depression, thereby increasing the susceptibility to developing diabetes.
Insulin signaling and neurotransmission
Insulin can cross the blood-brain barrier from the periphery but it is also locally produced in the brain, where it binds to insulin receptors on neurons and glial cells [6]. Insulin signaling in the brain is pivotal for cell survival, neuroinflammation, synaptic plasticity, and neurotransmission [6]. Disruptions in brain insulin signaling can adversely affect the dopaminergic mesolimbic reward circuit, altering hedonic perceptions [89, 90]. Furthermore, IR, even in the absence of psychiatric comorbidities, can impair cognitive performance. Both anhedonia and cognitive symptoms could be observed in depression and are symptoms particularly resistant to available psychotropic treatments [30, 89].
Insulin also modulates dopamine neurons differently across brain regions. In midbrain areas, such as the substantia nigra and ventral tegmental area, insulin upregulates dopamine transporter expression and reduces excitatory glutamatergic input, decreasing extracellular dopamine levels [90]. Conversely, IR contributes to reduced dopamine transporter expression coupled with increased excitatory glutamatergic input, elevating extracellular dopamine levels. However, in the striatum, which is located in the subcortical forebrain, insulin influences dopamine reuptake and release, with IR opposing these effects, impacting neuronal excitatory projections [90]. The PI3K/Akt pathway involved in insulin signaling also regulates dopamine clearance by modulating dopamine transporter expression and function. Acute insulin application in the ventral tegmental area in vitro diminishes somatodendritic dopamine levels via increased dopamine transporter activity, mediated by PI3K and mammalian target of rapamycin (mTOR) signaling pathways [90]. Long-term hyperglycemia can contribute to persistent disturbances in glutamatergic signaling and neural damage in the medial prefrontal cortex, contributing to depressive behaviors [91]. Furthermore, obesity and T2DM lead to systemic inflammation, increasing pro-inflammatory brain cytokines, which may, in turn, interfere with insulin signaling and neurotransmission [92].
In addition to insulin, insulin-like growth factor 1 (IGF-1) plays a role in brain function [93]. While insulin and IGF-1 share structural similarities and activate overlapping intracellular signaling pathways, such as the PI3K/Akt and MAPK pathways, they exhibit differential localization within the brain, which may impact their distinct roles in neuronal function and mood regulation [94, 95]. Insulin receptors are extensively distributed throughout but are particularly abundant in regions such as the olfactory bulb, cerebral cortex, hippocampus, hypothalamus, and cerebellum—areas integral to learning, memory, and emotional regulation [96]. Conversely, IGF-1 receptors are also widely expressed but exhibit higher densities in the cortex, hippocampus, and thalamus, with moderate expression in the olfactory bulb, hypothalamus, and cerebellum [95]. This distinct distribution pattern suggests that insulin and IGF-1 may influence different neuronal circuits and processes pertinent to depression. For example, impairments in insulin receptor signaling within the hippocampus and prefrontal cortex can disrupt synaptic plasticity and neurotransmitter balance, potentially leading to cognitive deficits and mood disturbances associated with depression [95]. Similarly, alterations in IGF-1 signaling may impact neurogenesis and neuronal survival, thereby affecting mood and cognitive functions [97]. Notably, IGF-1 promotes neurogenesis in the hippocampus, and reduced IGF-1 levels have been linked to depressive-like behaviors in animal models [97, 98]. Additionally, IGF-1 interacts with serotonin receptors, such as the 5-HT3 receptor, mediating neurogenesis and exhibiting antidepressant effects independent of traditional serotonin reuptake mechanisms [99]. Therefore, considering the overlapping yet distinct roles of insulin and IGF-1 in the brain, disruptions in their signaling pathways due to IR may contribute to the neurobiological mechanisms underlying depression in individuals with T2DM.
Overall, the multimorbidity of depression and T2DM involves shared genetic risk factors and multiple underlying biological mechanisms, including HPA axis dysregulation, pro-inflammatory states, gut-brain axis interactions, and insulin signaling alterations, which can affect neurotransmission. Further research on these mechanisms has the potential to lead to more personalized and effective treatment approaches for individuals suffering from both conditions.
Neuroimaging evidence linking depression and type 2 diabetes mellitus
Neuroimaging studies have provided insights into the neural mechanisms linking depression and T2DM, revealing structural and functional brain alterations that may underlie their comorbidity. A meta-analysis revealed that individuals with T2DM exhibit reduced global brain volume and regional atrophy in areas such as the hippocampus, basal ganglia, and orbitofrontal and occipital lobes [100]. Hippocampal atrophy appears to be an independent effect, potentially serving as a common neuropathological basis for the association of T2DM with both dementia and depression [100]. Conversely, global cerebral atrophy in T2DM may reflect atherosclerotic factors [100]. Further evidence demonstrates that patients with diabetes mellitus display increased atrophy in the hippocampus and amygdala compared to non-diabetic individuals, an effect not explained by increased vascular morbidity [101]. Additionally, studies employing cortical pattern matching have shown diminished cortical gray matter thickness in the left anterior cingulate cortex among individuals with T2DM, with those co-diagnosed with major depression exhibiting significant cortical gray matter reductions in bilateral prefrontal areas when compared to healthy controls [102]. Higher HbA1c levels have also been correlated with reduced hippocampal volume, suggesting that metabolic dysregulation in diabetes may have direct neuroanatomical consequences contributing to depressive symptoms [103]. These structural alterations in regions relevant to mood regulation suggest a neuroanatomical link between T2DM and depression.
Functional neuroimaging studies complement these structural findings by highlighting disrupted connectivity patterns in individuals with T2DM. For instance, increased connectivity in frontal and fronto-parietal networks has been found to predict depressive symptoms among middle-aged to elderly diabetics. Specifically, stronger connections between bilateral ventromedial prefrontal cortices and dorsal prefrontal cortices are associated with higher depressive scores, indicating that altered neural circuitry may underlie mood disturbances in this population [104]. Moreover, functional MRI studies have demonstrated impaired connectivity within the default mode network in T2DM patients. The hippocampus shows reduced functional connectivity bilaterally to widespread regions, including the fusiform gyrus, frontal gyrus, temporal gyrus, anterior and posterior cingulate gyri, medial frontal gyrus, precuneus, and inferior parietal lobule, compared to healthy controls [105]. This disrupted connectivity may contribute to cognitive deficits and depressive symptoms observed in T2DM. Further investigations have revealed that patients with T2DM exhibit decreased degree centrality in the left lingual gyrus and increased centrality in the right insula and dorsal anterior cingulate cortex [106]. The occipital network anchored in the lingual gyrus shows extensively reduced connectivity, while connectivity within the salience network is significantly elevated [106]. Correlational analyses also indicate that in the diabetic group, impaired visual memory and executive function are associated with occipital hypoconnectivity. In contrast, higher fasting plasma glucose levels and better executive functioning relate to hyperconnectivity in the anterior cingulate cortex [106]. These findings suggest that specific patterns of neural connectivity are linked to both metabolic control and cognitive performance in T2DM.
Intervention studies have explored the influence of insulin on neural activity. Functional MRI studies investigating the effects of intranasal insulin administration have revealed that insulin can modulate activity in brain regions involved in mood regulation, such as the prefrontal cortex and hypothalamus. Significant insulin-induced attenuation was observed predominantly in the occipital and prefrontal cortical regions, successfully localizing insulin-sensitive areas in the brain [107].
Collectively, these neuroimaging findings underscore the pathophysiological role of hyperglycemia and IR in modulating brain structure and function, thereby contributing to depressive symptomatology in individuals with T2DM.
Impacts of diabetes on psychological wellbeing
Managing diabetes imposes significant challenges that encompass both physiological and psychological dimensions, interlinking in a manner that profoundly affects overall health and quality of life. Studies have shown that chronic hyperglycemia and recurrent hypoglycemia in patients with diabetes reduce brain network efficiency [108], impair hippocampal neurogenesis and memory [109], and lead to microstructural changes in white matter and reduced gray matter density [110]. Hyperglycemia can thus lead to cognitive decline, neurodegeneration, brain atrophy, and altered brain structure and function [110, 111]. Chronic hyperglycemia and depression exhibit a bidirectional relationship in both T1DM and T2DM, with this association being mediated by suboptimal diabetes self-care management [112]. Markers of hyperglycemia, such as fasting glucose and glycated hemoglobin (HbA1c), have been associated with an increased risk of incident depressive symptoms [113].
Psychologically, the constant monitoring of blood glucose levels, adherence to strict dietary restrictions, and regular antidiabetic medication or insulin use contribute to considerable psychological stress and can lead to anxiety and depression [114, 115]. The fear of potential long-term complications such as neuropathy, retinopathy, and kidney disease further exacerbates this stress, which frequently results in a clinically significant apprehension regarding complications [116, 117]. Approximately one-third T2DM patient exhibits a clinically meaningful fear of complications [117]. This fear not only worsens psychological distress but also hampers effective self-management, creating a vicious cycle that leads to a decline in mental health. A cardinal symptom of (atypical) depression, which has been associated with poor glycemic control and mortality [118], is anhedonia (i.e., the lack of experiencing pleasure/joy). In a large study in more than 5000 participants with type 2 diabetes, it was shown that poor glycaemic control was associated with anhedonia but not depression or anxiety [119], suggesting that anhedonia may be more important than general depression scores. Potential mechanisms linking both are impaired dopamine signaling and inflammation (also see below), which both alter reward sensitivity and have been shown to be altered in DM2 and anhedonia [120]. Gruber et al. reviewed the link between anhedonia, IR and dopamine [90].
People with diabetes who experience complications, and hypoglycemia are more likely to report worse psychological outcomes [115]. Similarly, patients who have a heavier burden of diabetes, such as those who require insulin or experience complications, experience family conflict, are more likely to experience negative psychological effects [121]. Moreover, diabetes management can be overwhelming, leading to feelings of isolation and impacting social interactions. The demands of managing the condition can strain relationships and reduce social activities, thereby decreasing the patient’s quality of life. Effective diabetes management, therefore, requires a comprehensive approach that considers these intertwined psychological and physiological impacts. To address these dual aspects of diabetes, integrated care models that include both pharmacological treatments for the physical aspects of diabetes and psychological support to address mental health are essential [122, 123]. Cognitive-behavioral therapy (CBT) and other psychological interventions have shown promise in improving both glycemic control and psychological outcomes by enhancing coping strategies and reducing diabetes-related distress [124]. These therapeutic strategies underscore the necessity of treating the person as a whole, rather than focusing on separate symptomatology. As an active area of research, it is important to note that DM2 has not only been linked to depression or anhedonia but is associated with several psychiatric disorders [13]. On a more granular level, symptoms or domains such as hopelessness, trait impulsivity and compulsive behaviors have also been linked to DM2. While it is beyond the scope of this review to explore these associations, the interested reader is referred to current literature on the topic (e.g., impulsivity and compulsivity) [125, 126]. By consolidating the management strategies to address both the psychological and physiological impacts of diabetes, healthcare providers can offer more holistic care that potentially improves both health outcomes and quality of life for patients.
Impact of depression on diabetes management
Glycemic control
Depression is known to disrupt glycemic control in diabetes by affecting key self-management behaviors [1]. Reduced motivation, fatigue, and cognitive impairments hinder compliance with necessary diabetes care practices, such as glucose monitoring, dietary adherence, and maintaining physical activity, which may exacerbate hyperglycemia and increases complication risks [127]. Depression also prompts irregular eating behaviors and neglect of established management protocols, negatively influencing glycemic control [128]. Longitudinal studies have indicated that depressive symptoms correlate with elevated HbA1c levels in elderly patients either at risk for or currently experiencing depression [129]. Additionally, a sex-specific impact of MDD on glycemic responses in T2DM has been reported, where females are less likely to achieve normal glycemic levels [130]. Contrarily, larger studies have not observed a consistent link between depression and poorer glycemic control in T2DM [14]. Despite these findings suggesting a minimal direct influence of depression on glycemic control, this condition may still significantly heighten the risk of severe complications in diabetes [14], emphasizing the necessity for comprehensive management approaches that address both psychological and physiological aspects of diabetes care.
Medication adherence
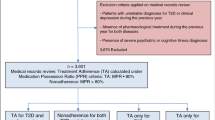
Depression adversely affects medication adherence in individuals with T2DM [131,132,133]. Several studies have highlighted the association between depression and poor adherence to medication and dietary regimens in individuals with T2DM [128, 134, 135]. Additionally, diabetes-related emotional distress and depression symptom severity have been identified as risk factors for medication non-adherence in T2DM [136, 137]. Various factors, such as financial problems, adverse drug reactions, memory issues, and the complexity of diet have been identified as possible mediators of poor adherence to medications in patients with diabetes [138]. The cognitive and motivational deficits associated with depression, along with feelings of hopelessness, and decreased interest in health management, may contribute to poor adherence to antidiabetic treatment. Non-adherence to medication regimens in individuals with depression who develop diabetes may contribute to the increased observed risk of complications such as cardiovascular disease, neuropathy, and retinopathy [139]. It is, therefore, important to address depression at an early stage in order to improve medication adherence and overall diabetes management.
Clinical outcomes
Depression is significantly associated with adverse health outcomes in patients with diabetes [14]. Pre-existing depression in individuals with T2DM is linked to increased risk of micro- and macrovascular complications, and higher mortality rates [24, 25, 140,141,142]. Depressed diabetics face a 1.5-fold increased risk of all-cause mortality and a 1.4-fold increased risk of cardiovascular mortality [140]. Additionally, depression is associated with a 36.8% increase in coronary heart disease and a 32.9% increase in stroke risk among patients with diabetes [27]. Depression also negatively impacts diabetes self-management behaviors and overall quality of life [143].
Treatment strategies for comorbid diabetes and depression
Pharmacological interventions
Antidepressant medications in patients with diabetes
The management of depression in patients with diabetes requires a comprehensive approach, including pharmacological and psychological treatment strategies. Collaborative strategies and integrated care plans, including regular screening, routine follow-up, rational drug use and medication adherence management, should be applied in both depression and diabetes management.
The antidepressant classes, selective serotonin reuptake inhibitors (SSRI), serotonin and noradrenalin reuptake inhibitors (SNRI), tricyclic antidepressants (TCA), monoamine oxidase inhibitors (MAOI), and atypical antidepressants that increase neurotransmitters serotonin, noradrenaline, and dopamine are in the guideline-based treatment strategies of depression [144]. A new study from Scotland has shown that the prevalence of antidepressant and antipsychotic prescribing in patients with T2DM has been increasing in recent years between 2004 and 2021 [145]. It has been proposed that this may be due to the longer duration of use of these drugs, and another reason may be the widespread use of SNRIs such as duloxetine in conditions other than MDD, including chronic pain associated with diabetic neuropathy [146].
While prescribing antidepressants in patients with diabetes, monitoring and minimizing the metabolic adverse effects is important. Potential adverse effects such as weight gain [147], dyslipidemia, and increased risk of cerebrovascular and cardiovascular morbidity [148] are significant concerns. The association of vascular problems creates a bidirectional negative impact with depression [149]. Certain atypical antipsychotics as adjunctive treatment in MDD, such as olanzapine and quetiapine, are also associated with metabolic adverse effects and drug-induced weight gain [150, 151]; however, as in the case of brexpiprazole, which is a partial dopaminergic agonist, this increase in weight might not be clinically important [152].
Several studies reported that SSRIs may increase the risk of T2DM in adults, particularly in long-term use [153], likely attributable to a modest weight gain associated with certain agents in this class [154]. In a nationwide US cohort with 1,582,914 patients, it was found that there may be a small increase in the risk of developing T2DM in children and adolescents who started SSRI treatment [155]. On the other hand, in a UK cohort, it was shown that there was no difference between fluoxetine-citalopram-escitalopram and paroxetine-fluvoxamine-sertraline in youth, and SSRIs did not increase significantly the risk of T2DM [156]. Overall, in any case, the risk/benefit ratio should be carefully weighed, especially in pediatric patients.
Comorbid depression and diabetes worsen glycemic control, and certain antidepressants may inversely contribute to it. In a French longitudinal cohort study conducted with approximately 64,000 women, the patients were followed up for 6 years [157]. It was shown that the risk of T2DM increased after the use of SSRI, imipramine-type and mixed antidepressants compared to those who did not use medications [157]. Increased dietary intake, decreased leptin level, and high affinity to histamine (H1) receptors [158], especially by TCAs such as imipramine-type antidepressants, may be responsible for the underlying mechanisms; however, further investigation is needed. Due to their efficacy and safety profiles, SSRIs and SNRIs are still the drugs of choice in patients with comorbid depression and diabetes, at least for short-term treatment (Fig. 1) [159,160,161,162]. Research indicates that certain serotonergic antidepressants, such as fluoxetine, can decrease blood glucose levels, enhance glucose regulation, and improve insulin sensitivity [163]. Conversely, some noradrenergic antidepressants (e.g., desipramine) have been associated with hyperglycemia [163]. Antidepressants that modulate both serotonin and norepinephrine, including duloxetine and venlafaxine, appear to exert no significant influence on glucose regulation mechanisms [163]. Regarding duloxetine, a review by Crucitti et al. showed a small, albeit statistically significant, increase in HbA1c in one long-term study, while no effect was observed in another long-term study and no significant effects were noted in short-term studies among patients with non-diabetic peripheral neuropathic pain [164].
GLP1-RAs Glucagon-like Peptide-1 Receptor Agonists, HPA Hypothalamic-Pituitary-Adrenal, SGLT2Is Sodium-Glucose Cotransporter-2 Inhibitors, SNRIs Serotonin and Norepinephrine Reuptake Inhibitors, SSRIs Selective Serotonin Reuptake Inhibitors, T2DM Type 2 Diabetes Mellitus. The symbols ↑, ↓, and ↔ indicate an increase, decrease or no impact/effect, respectively. The figure was created with BioRender (www.biorender.com).
In light of all these studies, it should be emphasized that blood glucose should be monitored regularly when initiating or adjusting antidepressant therapy, and patients with diabetes should also be monitored for depressive symptoms due to the bidirectional relationship.
Antidiabetic medications in patients with depression
Because the bidirectional association between IR, T2DM and depression is an evolving research area, studies testing or supporting the beneficial effects of antidiabetic drugs on depression are increasing exponentially. A recent meta-analysis assessing the effect of antidiabetic medications versus placebo in the treatment of acute depressive episodes did not support their efficacy in treating unipolar and bipolar depression, possibly because of the high heterogeneity of retained studies [165]. Notably, only six studies were retained (adopting a randomized, double-blind design), of which four were on pioglitazone [165]. Antidiabetic agents appear safe and well tolerated in the treatment of an acute depressive episode, but only subgroup analyses of the pooled estimates for depression rating scale scores, response rate and remission rate among depressed patients suggest a possible benefit from an antidiabetic medication for depressive symptoms [165]. Further research is needed to understand the modulation by genetics, culture, lifestyle, diet, behavior, metabolic status and other environmental factors.
Metformin, the current first-line treatment in T2DM, has an unclear antidepressant effect [166] despite identified direct mechanisms and pleiotropic effects, including inhibition of angiotensin II and NF-κB factor, normalization of gut microbiota, and intestinal permeabilization, and in vivo experimental data [167] supporting its potential benefits. However, clinical evidence from meta-analyses is limited and controversial, with potential inferiority as compared to pioglitazone [168, 169].
By activating peroxisome proliferator-activated receptors-γ, pioglitazone was largely investigated, driven by the hypothesis that IR and/or inflammatory activation may contribute to depressive episodes [170]. It has also been shown to improve depressive symptoms in obese patients with polycystic ovary syndrome and comorbid depression, in patients with bipolar disorder in a depressive episode [171], and in people with MDD [172]. However, the collected body of evidence does not fully support its clinically relevant antidepressant benefit [165]. Furthermore, its tolerability profile, which includes weight gain, edema/fluid retention, fractures, and (rarely) bladder cancer in long-term use, could hinder its potential repositioning for depression [173].
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and sodium-glucose cotransporter-2 (SGLT2) inhibitors are game-changers in the treatment of T2DM and are currently promoted by major clinical guidelines among potential first-line pharmacological options after failure/intolerance to metformin, especially in individuals with an atherosclerotic cardiovascular disease phenotype (GLP-1 RAs) [174]. Notably, liraglutide and semaglutide are also globally approved for treating obesity [175]. The interest in GLP-1 RAs for depression stems from several factors, including their consistent effect on weight reduction through appetite suppression and delayed gastric emptying, which may counteract antidepressant-related weight gain [176]. Additionally, GLP-1 RAs exhibit neuroprotective and anti-inflammatory effects, increase Akt dephosphorylation, decrease proinflammatory factors such as TNF-α, elevate neurotrophic factors like BDNF, reduce oxidative stress and microglial activation, and enhance gut-brain axis function and gut microbiota stability [176].
Results from two systematic reviews with meta-analyses of clinical trials and observational studies were conflicting regarding the reduction of depressive symptoms. However, potential benefits in lowering depression rating scale scores, especially for liraglutide, were observed [177, 178]. Another systematic review excluded patients with baseline depression to assess whether GLP-1 RAs reduce the risk of developing depression in subjects with T2DM [179]. Four retrospective observational studies were included, with only two cohort studies indicating a reduced risk, particularly with dulaglutide. The inconsistency and observational study limitations highlight the need for a deeper understanding of GLP-1 RAs’ central mechanisms [179]. The relationship between GLP-1 RAs and depression is complex. Post-marketing reports of suicidal or self-harming thoughts related to liraglutide or semaglutide led to a safety review by Regulatory Agencies. The European Medicines Agency, on April 12, 2024, concluded that there is no causal association between GLP-1 RAs and suicidal thoughts or actions [180]. Conversely, on January 11, 2024, the Food and Drug Administration did not rule out a potential small risk and is conducting a meta-analysis of clinical trials and post-marketing data in the Sentinel System [181]. Notably, the US label for semaglutide for obesity advises monitoring for depression or suicidal thoughts. Different mechanisms have been hypothesized on the controversial relationship between suicidality and GLP-1 Ras [182, 183]. First, overweight and obesity have been associated with increased risk of suicide attempts and completed suicide, although considerable heterogeneity exists. Notably, in one of the few studies in which obesity was associated with suicide completion, the most substantial risk factor was a sudden and unexplained loss of weight [184]. In fact, an alternative hypothesis may consider the perceived negative effects of a very rapid weight loss in highly vulnerable subjects, including taste aversion, possibly disrupting rewarding circuit. Comorbid alcohol use, poor psychosocial coping strategies, and social stigma associated with obesity may also represent additional risk factors. There is a well-established association between bariatric surgery and an increased postoperative risk of suicide, possibly related to unrealistic or thwarted expectations for weight loss, potentiation of the effects of alcohol from alterations in alcohol processing and absorption in the gut, and interference with anti-depressant effect due to pharmacokinetic changes (malabsorption and altered volume of distribution) [185, 186]. A direct detrimental “incretin effect” on the central nervous system could also be hypothesized and susceptible people receiving GLP-1 RAs may, in some circumstances, experience a worsening of hedonic tone predisposing psychopathology and/or self-harm ideation and/or other aspects of suicidality. In fact, anhedonia, especially attenuated anticipatory hedonism, was highly associated with suicidality [187]. Finally, different weight loss medications raised concerns about suicidality in the past, including phentermine/topiramate, bupropion/naltrexone, and especially rimonabant, an inverse agonist for the cannabinoid receptor CB1, which was worldwide withdrawn for increased risk of suicidality.SGLT2 inhibitors for depression are a relatively new topic; intriguingly, low-grade hyperketonemia (not leading to ketoacidosis, a rare, life-threatening side effect) may contribute to cardio-renal benefits and other effects, such as anti-inflammatory and antioxidant effects [188]. Moreover, SGLT2 inhibitors can reduce serum ACTH levels [189] and increase serum BDNF levels [190]. Population studies have confirmed a reduced risk of depression onset in T2DM patients, particularly with SGLT2 inhibitors [191, 192]. A recent clinical trial evaluated empagliflozin as an add-on to citalopram in 90 patients with moderate to severe depression, showing significant reductions in the Hamilton Depression Rating Scale and depressive symptoms at weeks 4 and 8 [193]. Only two patients reported increased urination frequency without other urinary symptoms, which improved gradually without further intervention or discontinuation. Notably, empagliflozin may correct citalopram-induced hyponatremia. These preliminary findings warrant further research in larger, longer clinical studies.
Table 1 provides an overview of key pharmacological features of the main pharmacological classes used in T2DM, including a summary of clinical data on the potential beneficial effect on depression/depressive symptoms.
Anti-inflammatory agents for depression, diabetes and their comorbidity
Anti-inflammatory agents for depression and diabetes comorbidity have been explored extensively due to inflammation’s role in both conditions. Non-steroidal anti-inflammatory drugs (NSAIDs), statins, glucocorticoids and monoclonal antibodies (e.g., targeting IL-6, TNF-α, IL-12/23) have been reported to show moderate anti-depressant capacity in patients with somatic disorders (i.e., rheumatoid arthritis, psoriasis) who also had comorbid symptoms of depression [194, 195]. Particularly antibodies targeting IL-6 and IL-23 were significant even after correcting for somatic symptom improvement.
Yet, disappointingly, when anti-inflammatory agents were used for a primary diagnosis of depression, most studies failed to show significant effects in the primary outcome analysis [196,197,198]. Significant results are often only observed after (mostly unplanned) post-hoc stratification [199, 200], while pre-registered stratified analyses did not show effects [201]. It is also important to note that depression is highly heterogeneous, and anti-inflammatory agents may not help with overall severity but rather alleviate specific symptoms of depression. In line, it has become clear that a connection of inflammation exists, particularly with the atypical symptoms of depression rather than overall symptom severity [202]. Future studies should thus consider atypical scores and baseline inflammatory markers for pre-stratified designs.
While the causal role of inflammation in T2DM is uncertain, circulating pro-inflammatory proteins (e.g., IL-1β, IL-6, IL-18, CRP, TNF-α) are linked to T2DM risk [203]. The presence of adipose tissue inflammation in T2DM has increased interest in anti-inflammatory treatments for T2DM and related vascular, neurological, and immunological complications. TNF-alpha showed potential in reducing tissue IR, improving glucose homeostasis, and preventing T2DM onset in animal models. Since TNF-alpha is a major cytokine produced by tissue-resident macrophages and circulating TNF-alpha is associated with obesity in T2DM [204], blocking TNF-alpha seems a plausible therapeutic strategy. However, clinical trials have yielded mixed results, failing to consistently enhance insulin sensitivity in T2DM [205]. Antibodies targeting IL1-ß have also shown mixed, although more positive effects, particularly in reducing HbA1c with IL1-ß antagonism [206], with recent evidence suggesting that combined TNF-alpha and IL1-ß blockade may be most effective for glycemic control [207]. Additionally, NSAIDs like salasate and acetylsalicylic acid exhibit strong anti-inflammatory properties by inhibiting NF-κB. Although acetylsalicylic acid may reduce major cardiovascular events in T2DM patients, it also increases the risk of hemorrhage and should only be used under strict medical supervision.
However, despite the mounting evidence linking inflammation to T2DM and depression [208, 209], few studies have examined depressive symptoms in diabetes patients using anti-inflammatory agents. One recent publication found statins significantly reduced the risk of depressive symptoms in diabetes patients especially at the 5-year follow-up time point [210]. Another study on hemodialysis patients, over 50% of whom had T2DM, assessed the anti-IL-1 agent anakinra [211]. Baseline depressive symptoms were in the normal range and only a slight, insignificant decrease was observed when comparing anakinra to placebo. This scarcity of literature highlights a research gap. Future studies should explore depressive symptoms in diabetes patients treated with anti-inflammatory agents, particularly in comorbid populations. It should also be noted that considerable risks are associated with the use of immunosuppressive drugs. Immunosuppressants contribute to serious infections, increase the risk of cancers (especially skin, liver, lymphoma, and kidney), lead to cardiovascular toxicity, and result in hospitalizations and complications [212,213,214,215]; hence, their use should not be taken lightly.
Non-pharmacological interventions
Psychotherapy
T2DM comes with an increased risk for both, depression and anxiety disorders [216, 217]. Depressive symptoms and increased anxiety due to diabetes-related distress (i.e., the emotional and psychological burden associated with managing diabetes [140] are associated with poor self-care behaviors and worse intermediate and long-term health outcomes [218]. Psychological treatment of mental health conditions that co-occur with T2DM is ideally performed by healthcare professionals who are specialized in treating the psychological aspects of diabetes management, (i.e., certified clinical psychologists trained to work in a medical setting) [219]. There are several psychological treatment approaches, with CBT and mindfulness-based therapy showing the most effectiveness in the treatment of diabetes-associated mental health problems [220, 221].
Both, CBT and mindfulness-based techniques specifically target diabetes distress, which is related to self-care burden (e.g., the constant need for blood sugar monitoring), emotional burden (e.g. feelings of frustration, guilt and helplessness about managing diabetes), interpersonal issues (feelings of isolation or lack of understanding from others about the challenges of living with diabetes) and poor access to good quality care [222]. 36% of individuals with T2DM are affected by diabetes distress [223]. Cognitive techniques from CBT can help to identify and challenge general and diabetes-specific cognitive distortions resulting in maladaptive behavior and are usually complemented with behavioral techniques, including behavioral activation and specific behavioral change strategies related to diabetes and mood [218]. These can assist patients in developing healthy lifestyle habits, such as a healthy diet, exercise, blood glucose monitoring and medication adherence.
Mindfulness and acceptance-based interventions, such as mindfulness-based cognitive therapy, mindfulness-based stress reduction, and acceptance and commitment therapy, are therapeutic approaches to enhance psychological flexibility, awareness, and non-judgmental acceptance of present-moment experiences, including bodily sensations, thoughts, and feelings [220]. Accepting unwanted experiences can alleviate diabetes distress, which stems from the daily burdens of self-care. Mindfulness-based interventions can help to reduce stress and foster self-compassion. All therapeutic interventions should be accompanied by motivational support, strengthening patient perceptions about their own ability and self-efficacy to self-manage diabetes [224, 225].
Lifestyle interventions
Dietary modifications
Daily healthy food choices are a challenging aspect of diabetes self-care [226]. Current medical nutrition therapy guidelines advocate for personalized, flexible, and healthy eating patterns rather than a one-fits-all approach [227]. Overweight individuals with T2DM should reduce energy intake while maintaining a balanced diet rich in nutrient-dense foods like fruits, vegetables, whole grains, lean proteins, and healthy fats, limiting added sugars, sodium, and saturated fats [148]. Self-monitoring carbohydrate intake, either through counting or estimation, is important for glycemic control [227]. Ideally, this should be complemented by other lifestyle, such as increased physical activity and behavior modifications [228]. Empowering individuals with diabetes in self-care by educating them about diet and lifestyle factors enhances self-efficacy and reduces feelings of helplessness, which can also alleviate anxiety and depressive symptoms [228].
Exercise and physical activity recommendations
The World Health Organization (WHO) recommends that adults engage in 150–350 min of moderate activity per week or half that amount for vigorous activity [229]. Exercise significantly benefits individuals with T2DM by enhancing insulin sensitivity and glycemic control [230] and can prevent or delay T2DM onset [231]. For depression, activities such as walking, jogging, yoga, or strength training exhibit moderate antidepressant effects, while a meta-analysis revealed notable antidepressant effects of exercise therapy in individuals with both diabetes and depression [232]. Mechanistically, exercise promotes insulin sensitivity, enhances blood circulation, and improves glucose uptake via insulin-dependent and independent pathways, such as GLUT-4 translocation. Regular exercise depletes muscle glycogen stores, lowers blood glucose, and improves glycemic control in T2DM over 8 weeks or more. Additionally, it decreases inflammation by reducing pro-inflammatory cytokines and increasing anti-inflammatory ones, thereby improving insulin sensitivity and decreasing tissue inflammation [41, 233].
Conclusions and future directions
This review underscores the complex, bidirectional relationship between depression and diabetes, highlighting how each condition can exacerbate the other, complicating management and adversely impacting clinical outcomes. Our review provides insights into the interplay of lifestyle factors, genetic predispositions, and the significant psychological and physiological burdens associated with managing these comorbid conditions. The evidence reviewed clearly supports that treating these conditions isolated is less effective than a holistic approach that addresses both metabolic and mental health aspects. Integrated care models, combining medical treatment with psychological support to manage the comprehensive health challenges patients face, are essential for effective treatment. Such models require collaborations among endocrinologists, primary care providers, psychiatrists, and other mental health professionals to enhance outcomes and improve adherence.
Despite extensive research, significant gaps remain in the causal pathways linking depression and diabetes. More longitudinal studies, adequately considering possible confounding factors, are needed to clarify these relationships and identify modifiable risk factors for targeted interventions. Exploring novel therapeutic targets like the repurposing of anti-inflammatory and antidiabetic agents could revolutionize treatment approaches in patients suffering from both depression and diabetes. Additionally, the impact of emerging technologies such as digital health tools and telemedicine on patient outcomes and care delivery needs further investigation to enhance care accessibility and cost-effectiveness in diverse settings.
Future research should focus on personalized medicine, considering genetic, environmental, and lifestyle factors that influence both conditions. Comprehensive studies involving diverse populations are needed to develope and validate integrated care models that can effectively manage both of these comorbid conditions. Healthcare policies must support integrated care frameworks that facilitate the co-management of diabetes and depression, emphasizing the creation of interdisciplinary teams equipped to address both mental and physical aspects. Public health initiatives should focus on raising awareness, reducing stigma, and educating individuals about effective management strategies to mitigate health disparities. Advancing our understanding and treatment of this comorbidity holds the potential to substantially improve quality of life and health outcomes for individuals living with these conditions.
References
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119. https://doi.org/10.1016/j.diabres.2021.109119.
World Health Organization. Depressive disorder (depression). 2024. https://www.who.int/news-room/fact-sheets/detail/depression.
Ferrari AJ, Charlson FJ, Norman RE, Patten SB, Freedman G, Murray CJ, et al. Burden of depressive disorders by country, sex, age, and year: findings from the global burden of disease study 2010. PLoS Med. 2013;10:e1001547.
Goldenberg R, Punthakee Z. Definition, classification and diagnosis of diabetes, prediabetes and metabolic syndrome. Can J Diabetes. 2013;37:S8–11.
da Silva Rosa SC, Nayak N, Caymo AM, Gordon JW. Mechanisms of muscle insulin resistance and the cross-talk with liver and adipose tissue. Physiol Rep. 2020;8:e14607.
Arnold SE, Arvanitakis Z, Macauley-Rambach SL, Koenig AM, Wang H-Y, Ahima RS, et al. Brain insulin resistance in type 2 diabetes and Alzheimer disease: concepts and conundrums. Nat Rev Neurol. 2018;14:168–81.
Mullins RJ, Diehl TC, Chia CW, Kapogiannis D. Insulin resistance as a link between amyloid-beta and tau pathologies in Alzheimer’s disease. Front Aging Neurosci. 2017;9:118. https://doi.org/10.3389/fnagi.2017.00118.
van Gils V, Rizzo M, Côté J, Viechtbauer W, Fanelli G, Salas-Salvadó J, et al. The association of glucose metabolism measures and diabetes status with Alzheimer’s disease biomarkers of amyloid and tau: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2024;159:105604.
Golden SH. A review of the evidence for a neuroendocrine link between stress, depression and diabetes mellitus. Curr Diabetes Rev. 2007;3:252–9.
Champaneri S, Wand GS, Malhotra SS, Casagrande SS, Golden SH. Biological basis of depression in adults with diabetes. Curr Diab Rep. 2010;10:396–405.
Zanoveli JM, Morais HD, Dias IC, Schreiber AK, Souza CP, Cunha JM. Depression associated with diabetes: from pathophysiology to treatment. Curr Diabetes Rev. 2016;12:165–78.
Rotella F, Mannucci E. Diabetes mellitus as a risk factor for depression. a meta-analysis of longitudinal studies. Diabetes Res Clin Pract. 2013;99:98–104.
Wimberley T, Horsdal HT, Brikell I, Laursen TM, Astrup A, Fanelli G, et al. Temporally ordered associations between type 2 diabetes and brain disorders—a Danish register-based cohort study. BMC Psychiatry. 2022;22:573.
Possidente C, Fanelli G, Serretti A, Fabbri C. Clinical insights into the cross-link between mood disorders and type 2 diabetes: a review of longitudinal studies and mendelian randomisation analyses. Neurosci Biobehav Rev. 2023;152:105298.
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–78.
Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J Affect Disord. 2012;142:S8–21.
Collins MM, Corcoran P, Perry IJ. Anxiety and depression symptoms in patients with diabetes. Diabet Med J Br Diabet Assoc. 2009;26:153–61.
Lunghi C, Moisan J, Grégoire J-P, Guénette L. Incidence of depression and associated factors in patients with type 2 diabetes in Quebec, Canada: a population-based cohort study. Medicine. 2016;95:e3514.
Meshkat S, Liu Y, Jung H, Tassone VK, Pang H, Janssen-Aguilar R, et al. Temporal associations of BMI and glucose parameters with depressive symptoms among US adults. Psychiatry Res. 2024;332:115709.
Nong Y, Wu G, Lu J, Wei X, Yu D. The mediating role of obesity in the development of depression in individuals with diabetes: a population-based study from NHANES 2005–2014. J Affect Disord. 2024;351:977–82.
Katon W, Fan MY, Unutzer J, Taylor J, Pincus H, Schoenbaum M. Depression and diabetes: a potentially lethal combination. J Gen Intern Med. 2008;23:1571–5.
Knol MJ, Heerdink ER, Egberts AC, Geerlings MI, Gorter KJ, Numans ME, et al. Depressive symptoms in subjects with diagnosed and undiagnosed type 2 diabetes. Psychosom Med. 2007;69:300–5.
Nouwen A, Nefs G, Caramlau I, Connock M, Winkley K, Lloyd CE, et al. Prevalence of depression in individuals with impaired glucose metabolism or undiagnosed diabetes: a systematic review and meta-analysis of the european depression in diabetes (EDID) research consortium. Diabetes Care. 2011;34:752–62.
Lunghi C, Zongo A, Tardif I, Demers É, Diendéré JDR, Guénette L. Depression but not non-persistence to antidiabetic drugs is associated with mortality in type 2 diabetes: a nested case-control study. Diabetes Res Clin Pract. 2021;171:108566.
Messina R, Iommi M, Rucci P, Reno C, Fantini MP, Lunghi C, et al. Is it time to consider depression as a major complication of type 2 diabetes? Evidence from a large population-based cohort study. Acta Diabetol. 2022;59:95–104.
Tardif I, Guénette L, Zongo A, Demers É, Lunghi C. Depression and the risk of hospitalization in type 2 diabetes patients: a nested case-control study accounting for non-persistence to antidiabetic treatment. Diabetes Metab. 2022;48:101334.
Farooqi A, Khunti K, Abner S, Gillies C, Morriss R, Seidu S. Comorbid depression and risk of cardiac events and cardiac mortality in people with diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pr. 2019;156:107816.
Prigge R, Wild SH, Jackson CA. Depression, diabetes, comorbid depression and diabetes and risk of all-cause and cause-specific mortality: a prospective cohort study. Diabetologia. 2022;65:1450–60.
Rotella F, Mannucci E. Depression as a risk factor for diabetes: a meta-analysis of longitudinal studies. J Clin Psychiatry. 2013;74:31–7.
Fanelli G, Serretti A. Depression, antidepressants, and insulin resistance: which link? Eur Neuropsychopharmacol. 2022;60:4–6.
Fisher L, Hessler DM, Polonsky WH, Mullan J. When is diabetes distress clinically meaningful?: establishing cut points for the diabetes distress scale. Diabetes Care. 2012;35:259–64.
Gonzalez JS, Fisher L, Polonsky WH. Depression in diabetes: have we been missing something important? Diabetes Care. 2011;34:236–9.
Gonzalez Heredia T, González-Ramírez LP, Hernández-Corona DM, Maciel-Hernández EA. Anxious depression in patients with type 2 diabetes mellitus and its relationship with medication adherence and glycemic control. Glob Public Health. 2021;16:460–8.
Simmons WK, Burrows K, Avery JA, Kerr KL, Taylor A, Bodurka J, et al. Appetite changes reveal depression subgroups with distinct endocrine, metabolic, and immune states. Mol Psychiatry. 2020;25:1457–68.
Zheng L, Sun J, Yu X, Zhang D. Ultra-processed food is positively associated with depressive symptoms among United States adults. Front Nutr. 2020;7:600449.
Gómez-Donoso C, Sánchez-Villegas A, Martínez-González MA, Gea A, Mendonça RD, et al. Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: the SUN project. Eur J Nutr. 2020;59:1093–103.
Nordström A, Hadrévi J, Olsson T, Franks PW, Nordström P. Higher prevalence of type 2 diabetes in men than in women is associated with differences in visceral fat mass. J Clin Endocrinol Metab. 2016;101:3740–6.
Darwish L, Beroncal E, Sison MV, Swardfager W. Depression in people with type 2 diabetes: current perspectives. Diabetes Metab Syndr Obes. 2018;11:333–43.
Koopmans B, Pouwer F, de Bie RA, van Rooij ES, Leusink GL, Pop VJ. Depressive symptoms are associated with physical inactivity in patients with type 2 diabetes. The DIAZOB primary care diabetes study. Fam Pract. 2009;26:171–3.
García-Pérez-de-Sevilla G, Sánchez-Pinto B. Physical inactivity and chronic disease. Nutr Today. 2022;57:252.
Iaccarino G, Franco D, Sorriento D, Strisciuglio T, Barbato E, Morisco C. Modulation of insulin sensitivity by exercise training: implications for cardiovascular prevention. J Cardiovasc Transl Res. 2021;14:256–70.
Hunt GE, Malhi GS, Lai HMX, Cleary M. Prevalence of comorbid substance use in major depressive disorder in community and clinical settings, 1990–2019: systematic review and meta-analysis. J Affect Disord. 2020;266:288–304.
Winhusen T, Theobald J, Kaelber DC, Lewis D. Medical complications associated with substance use disorders in patients with type 2 diabetes and hypertension: electronic health record findings. Addict Abingdon Engl. 2019;114:1462–70.
Hsieh P-H, Huang J-Y, Nfor ON, Lung C-C, Ho C-C, Liaw Y-P. Association of type 2 diabetes with liver cirrhosis: a nationwide cohort study. Oncotarget. 2017;8:81321–8.
O’Keefe EL, DiNicolantonio JJ, O’Keefe JH, Lavie CJ. Alcohol and CV health: Jekyll and Hyde J-Curves. Prog Cardiovasc Dis. 2018;61:68–75.
Śliwińska-Mossoń M, Milnerowicz H. The impact of smoking on the development of diabetes and its complications. Diab Vasc Dis Res. 2017;14:265–76.
Wu L-T, Ghitza UE, Batch BC, Pencina MJ, Rojas LF, Goldstein BA, et al. Substance use and mental diagnoses among adults with and without type 2 diabetes: results from electronic health records data. Drug Alcohol Depend. 2015;156:162–9.
Platona RI, Căiţă GA, Voiţă-Mekeres F, Peia AO, Enătescu RV. The impact of psychiatric comorbidities associated with depression: a literature review. Med Pharm Rep. 2024;97:143–8.
Chattu VK, Chattu SK, Burman D, Spence DW, Pandi-Perumal SR. The interlinked rising epidemic of insufficient sleep and diabetes mellitus. Healthcare. 2019;7:37.
Saner NJ, Bishop DJ, Bartlett JD. Is exercise a viable therapeutic intervention to mitigate mitochondrial dysfunction and insulin resistance induced by sleep loss? Sleep Med Rev. 2018;37:60–68.
Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: a systematic review and meta-analysis. Sleep Med Rev. 2017;31:91–101.
Brailean A, Curtis J, Davis K, Dregan A, Hotopf M. Characteristics, comorbidities, and correlates of atypical depression: evidence from the UK biobank mental health survey. Psychol Med. 2020;50:1129–38.
Hur MH, Lee M-K, Seong K, Hong JH. Deterioration of sleep quality according to glycemic status. Diabetes Metab J. 2020;44:679–86.
Fanelli G, Franke B, De Witte W, Ruisch IH, Haavik J, van Gils V, et al. Insulinopathies of the brain? Genetic overlap between somatic insulin-related and neuropsychiatric disorders. Transl Psychiatry. 2022;12:1–8.
Willemsen G, Ward KJ, Bell CG, Christensen K, Bowden J, Dalgård C, et al. The concordance and heritability of type 2 diabetes in 34,166 twin Pairs from international twin registers: the Discordant Twin (DISCOTWIN) Consortium. Twin Res Hum Genet. 2015;18:762–71.
Kendler KS, Prescott CA. A population-based twin study of lifetime major depression in men and women. Arch Gen Psychiatry. 1999;56:39–44.
Fanelli G, Franke B, Fabbri C, Werme J, Erdogan I, De Witte W, et al. Local patterns of genetic sharing challenge the boundaries between neuropsychiatric and insulin resistance-related conditions. MedRxiv. 2024. https://doi.org/10.1101/2024.03.07.24303921.
Maina JG, Balkhiyarova Z, Nouwen A, Pupko I, Ulrich A, Boissel M, et al. Bidirectional mendelian randomization and multiphenotype GWAS show causality and shared pathophysiology between depression and type 2 diabetes. Diabetes Care. 2023;46:1707–14.
Tang B, Yuan S, Xiong Y, He Q, Larsson SC. Major depressive disorder and cardiometabolic diseases: a bidirectional mendelian randomisation study. Diabetologia. 2020;63:1305–11.
Tao H, Fan S, Zhu T, You L, Zheng D, Yan L, et al. Psychiatric disorders and type 2 diabetes mellitus: a bidirectional mendelian randomization. Eur J Clin Invest. 2023;53:e13893.
Clarke T-K, Obsteter J, Hall LS, Hayward C, Thomson PA, Smith BH, et al. Investigating shared aetiology between type 2 diabetes and major depressive disorder in a population based cohort. Am J Med Genet B Neuropsychiatr Genet. 2017;174:227–34.
Xuan L, Zhao Z, Jia X, Hou Y, Wang T, Li M, et al. Type 2 diabetes is causally associated with depression: a Mendelian randomization analysis. Front Med. 2018;12:678–87.
Kasyanov E, Pinakhina D, Rakitko A, Vergasova E, Yermakovich D, Rukavishnikov G, et al. Genetic associations of anhedonia: insights into overlap of mental and somatic disorders. Consort Psychiatr. 2024;5:5–15.
Hartwell EE, Jinwala Z, Milone J, Ramirez S, Gelernter J, Kranzler HR, et al. Application of polygenic scores to a deeply phenotyped sample enriched for substance use disorders reveals extensive pleiotropy with psychiatric and somatic traits. Neuropsychopharmacology. 2024;49:1958–67.
Ekberg KM, Michelini G, Schneider KL, Docherty AR, Shabalin AA, Perlman G, et al. Associations between polygenic risk scores for cardiometabolic phenotypes and adolescent depression and body dissatisfaction. Pediatr Res. https://doi.org/10.1038/s41390-024-03323-z.
Su M-H, Shih Y-H, Lin Y-F, Chen P-C, Chen C-Y, Hsiao P-C, et al. Familial aggregation and shared genetic loading for major psychiatric disorders and type 2 diabetes. Diabetologia. 2022;65:800–10.
Sewell MDE, Jiménez-Sánchez L, Shen X, Edmondson-Stait AJ, Green C, Adams MJ, et al. Associations between major psychiatric disorder polygenic risk scores and blood-based markers in UK biobank. Brain Behav Immun. 2021;97:32–41.
Hagenaars SP, Coleman JRI, Choi SW, Gaspar H, Adams MJ, Howard DM, et al. Genetic comorbidity between major depression and cardio-metabolic traits, stratified by age at onset of major depression. Am J Med Genet B Neuropsychiatr Genet. 2020;183:309–30.
Wimberley T, Brikell I, Astrup A, Larsen JT, Petersen LV, Albiñana C, et al. Shared familial risk for type 2 diabetes mellitus and psychiatric disorders: a nationwide multigenerational genetics study. Psychol Med. 2024;27:1–10. https://doi.org/10.1017/S0033291724001053. Epub ahead of print.
Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes Endocrinol. 2015;3:461–71.
Mosili P, Mkhize BC, Sibiya NH, Ngubane PS, Khathi A. Review of the direct and indirect effects of hyperglycemia on the HPA axis in T2DM and the co-occurrence of depression. BMJ Open Diabetes Res Care. 2024;12:e003218.
Kyrou I, Tsigos C. Stress hormones: physiological stress and regulation of metabolism. Curr Opin Pharmacol. 2009;9:787–93.
Coderre L, Vallega GA, Pilch PF, Chipkin SR. In vivo effects of dexamethasone and sucrose on glucose transport (GLUT-4) protein tissue distribution. Am J Physiol. 1996;271:E643–48.
Herbert J, Goodyer IM, Grossman AB, Hastings MH, de Kloet ER, Lightman SL, et al. Do corticosteroids damage the brain? J Neuroendocrinol. 2006;18:393–411.
Zefferino R, Di Gioia S, Conese M. Molecular links between endocrine, nervous and immune system during chronic stress. Brain Behav. 2021;11:e01960.
Osimo EF, Baxter LJ, Lewis G, Jones PB, Khandaker GM. Prevalence of low-grade inflammation in depression: a systematic review and meta-analysis of CRP levels. Psychol Med. 2019;49:1958–70.
Makhija K, Karunakaran S. The role of inflammatory cytokines on the aetiopathogenesis of depression. Aust N Z J Psychiatry. 2013;47:828–39.
Américo-Da-Silva L, Aguilera J, Quinteros-Waltemath O, Sánchez-Aguilera P, Russell J, Cadagan C, et al. Activation of the NLRP3 inflammasome increases the IL-1β level and decreases GLUT4 translocation in skeletal muscle during insulin resistance. Int J Mol Sci. 2021;22:10212.
Schiepers OJG, Wichers MC, Maes M. Cytokines and major depression. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:201–17.
Copps KD, White MF. Regulation of insulin sensitivity by serine/threonine phosphorylation of insulin receptor substrate proteins IRS1 and IRS2. Diabetologia. 2012;55:2565–82.
Milaneschi Y, Lamers F, Berk M, Penninx BWJH. Depression heterogeneity and Its biological underpinnings: toward immunometabolic depression. Biol Psychiatry. 2020;88:369–80.
Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021;320:C375–91.
Soto M, Herzog C, Pacheco JA, Fujisaka S, Bullock K, Clish CB, et al. Gut microbiota modulate neurobehavior through changes in brain insulin sensitivity and metabolism. Mol Psychiatry. 2018;23:2287–301.
Borgiani G, Possidente C, Fabbri C, Oliva V, Bloemendaal M, Arias Vasquez A, et al. The bidirectional interaction between antidepressants and the gut microbiota: are there implications for treatment response? Int Clin Psychopharmacol. 2025;40:3–26. https://doi.org/10.1097/YIC.0000000000000533.
Silva YP, Bernardi A, Frozza RL. The role of short-chain fatty acids from gut microbiota in gut-brain communication. Front Endocrinol. 2020;11:25.
Repousi N, Masana MF, Sanchez-Niubo A, Haro JM, Tyrovolas S. Depression and metabolic syndrome in the older population: a review of evidence. J Affect Disord. 2018;237:56–64.
Yu ZM, Parker L, Dummer TJB. Depressive symptoms, diet quality, physical activity, and body composition among populations in Nova Scotia, Canada: report from the Atlantic partnership for tomorrow’s health. Prev Med. 2014;61:106–13.
Cao B, Chen Y, Brietzke E, Cha D, Shaukat A, Pan Z, et al. Leptin and adiponectin levels in major depressive disorder: a systematic review and meta-analysis. J Affect Disord. 2018;238:101–10.
Fanelli G, Mota NR, Salas-Salvadó J, Bulló M, Fernandez-Aranda F, Camacho-Barcia L, et al. The link between cognition and somatic conditions related to insulin resistance in the UK biobank study cohort: a systematic review. Neurosci Biobehav Rev. 2022;143:104927.
Gruber J, Hanssen R, Qubad M, Bouzouina A, Schack V, Sochor H, et al. Impact of insulin and insulin resistance on brain dopamine signalling and reward processing—an underexplored mechanism in the pathophysiology of depression? Neurosci Biobehav Rev. 2023;149:105179.
Baek JH, Son H, Kang JS, Yoo DY, Chung HJ, Lee DK, et al. Long-term hyperglycemia causes depressive behaviors in mice with hypoa ctive glutamatergic activity in the medial prefrontal cortex, which is not reversed by insulin treatment. Cells. 2022;11:4012.
Leonard BE, Wegener G. Inflammation, insulin resistance and neuroprogression in depression. Acta Neuropsychiatr. 2020;32:1–9.
Fernandez AM, Torres-Alemán I. The many faces of insulin-like peptide signalling in the brain. Nat Rev Neurosci. 2012;13:225–39.
Kleinridders A. Deciphering brain insulin receptor and insulin‐like growth factor 1 receptor signalling. J Neuroendocrinol. 2016;28:jne.12433.
Kleinridders A, Ferris HA, Cai W, Kahn CR. Insulin action in brain regulates systemic metabolism and brain function. Diabetes. 2014;63:2232–43.
Ghasemi R, Haeri A, Dargahi L, Mohamed Z, Ahmadiani A. Insulin in the brain: sources, localization and functions. Mol Neurobiol. 2013;47:145–71.
Wrigley S, Arafa D, Tropea D. Insulin-like growth factor 1: at the crossroads of brain development and aging. Front Cell Neurosci. 2017;11:14. https://doi.org/10.3389/fncel.2017.00014.
Szczęsny E, Slusarczyk J, Głombik K, Budziszewska B, Kubera M, Lasoń W, et al. Possible contribution of IGF-1 to depressive disorder. Pharmacol Rep. 2013;65:1622–31.
Kondo M, Koyama Y, Nakamura Y, Shimada S. A novel 5HT3 receptor-IGF1 mechanism distinct from SSRI-induced antidepressant effects. Mol Psychiatry. 2018;23:833–42.
Moulton CD, Costafreda SG, Horton P, Ismail K, Fu CHY. Meta-analyses of structural regional cerebral effects in type 1 and type 2 diabetes. Brain Imaging Behav. 2015;9:651–62.
den Heijer T, Vermeer SE, van Dijk EJ, Prins ND, Koudstaal PJ, Hofman A, et al. Type 2 diabetes and atrophy of medial temporal lobe structures on brain MRI. Diabetologia. 2003;46:1604–10.
Ajilore O, Narr K, Rosenthal J, Pham D, Hamilton L, Watari K, et al. Regional cortical gray matter thickness differences associated with type 2 diabetes and major depression. Psychiatry Res. 2010;184:63–70.
Hsu F-C, Yuan M, Bowden DW, Xu J, Smith SC, Wagenknecht LE, et al. Adiposity is inversely associated with hippocampal volume in African Americans and European Americans with diabetes. J Diabetes Complications. 2016;30:1506–12.
Salardini A, Shen X, Hashemi-Aghdam A, Laltoo E, Savoia S, Tokoglu F, et al. Increased connectivity in several bilateral frontal and fronto-parietal networks predicts depressive symptoms in mid- to late-life diabetics. Alzheimers Dement. 2020;16:e043619.
Zhou H, Lu W, Shi Y, Bai F, Chang J, Yuan Y, et al. Impairments in cognition and resting-state connectivity of the hippocampus in elderly subjects with type 2 diabetes. Neurosci Lett. 2010;473:5–10.
Cui Y, Li S-F, Gu H, Hu Y-Z, Liang X, Lu C-Q, et al. Disrupted brain connectivity patterns in patients with type 2 diabetes. Am J Neuroradiol. 2016;37:2115–22.
Kullmann S, Heni M, Fritsche A, Preissl H. Insulin action in the human brain: evidence from neuroimaging studies. J Neuroendocrinol. 2015;27:419–23.
Kim D-J, Yu JH, Shin M-S, Shin Y-W, Kim M-S. Hyperglycemia reduces efficiency of brain networks in subjects with type 2 diabetes. PLoS ONE. 2016;11:e0157268.
Ferreiro E, Lanzillo M, Canhoto D, Carvalho da Silva AM, Mota SI, Dias IS, et al. Chronic hyperglycemia impairs hippocampal neurogenesis and memory in an Alzheimer’s disease mouse model. Neurobiol Aging. 2020;92:98–113.
Seaquist ER. The impact of diabetes on cerebral structure and function. Psychosom Med. 2015;77:616.
Hamed SA. Brain injury with diabetes mellitus: evidence, mechanisms and treatment implications. Expert Rev Clin Pharmacol. 2017;10:409–28.
Schmitt A, Reimer A, Hermanns N, Kulzer B, Ehrmann D, Krichbaum M, et al. Depression is linked to hyperglycaemia via suboptimal diabetes self-ma nagement: a cross-sectional mediation analysis. J Psychosom Res. 2017;94:17–23.
Geraets AFJ, Köhler S, Muzambi R, Schalkwijk CG, Oenema A, Eussen SJPM, et al. The association of hyperglycaemia and insulin resistance with incident depressive symptoms over 4 years of follow-up: the Maastricht study. Diabetologia. 2020;63:2315–28.
Bhat NA, Muliyala KP, Chaturvedi SK. Psychological aspects of diabetes. EMJ Diabetes. 2020;8:90–98.
Jones A, Olsen MZ, Perrild HJ, Willaing I. The psychological impact of living with diabetes: descriptive findings from the DAWN2 study in Denmark. Prim Care Diabetes. 2016;10:83–6.
Jimenez-Garcia R, Martinez Huedo MA, Hernandez-Barrera V, Lopez de Andres A, Martinez D, Jimenez-Trujillo I, et al. Psychological distress and mental disorders among spanish diabetic adults: a case-control study. Prim Care Diabetes. 2012;6:149–56.
Kuniss N, Freyer M, Müller N, Kielstein V, Müller UA. Expectations and fear of diabetes-related long-term complications in people with type 2 diabetes at primary care level. Acta Diabetol. 2019;56:33–38.
Carter J, Swardfager W. Mood and metabolism: anhedonia as a clinical target in type 2 diabetes. Psychoneuroendocrinology. 2016;69:123–32.
Nefs G, Pouwer F, Denollet J, Kramer H, Wijnands - van Gent CJM, Pop VJM. Suboptimal glycemic control in type 2 diabetes: a key role for anhedonia? J Psychiatr Res. 2012;46:549–54.
Boyle CC, Bower JE, Eisenberger NI, Irwin MR. Stress to inflammation and anhedonia: mechanistic insights from preclinical and clinical models. Neurosci Biobehav Rev. 2023;152:105307.
Speight J. DAWN2 shines more light on the psychological burden of living with diabetes and on the correlates of quality psychological care. Diabet Med J Br Diabet Assoc. 2016;33:1172–3.
Doherty AM, Gayle C, Morgan-Jones R, Archer N, Laura-Lee, Ismail K, et al. Improving quality of diabetes care by integrating psychological and social care for poorly controlled diabetes: 3 dimensions of care for diabetes. Int J Psychiatry Med. 2016;51:3–15.
Harkness E, Macdonald W, Valderas J, Coventry P, Gask L, Bower P. Identifying psychosocial interventions that improve both physical and mental health in patients with diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33:926–30.
Uchendu C, Blake H. Effectiveness of cognitive–behavioural therapy on glycaemic control and psychological outcomes in adults with diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Diabet Med. 2017;34:328–39.
Gómez-Martínez C, Paolassini-Guesnier P, Fezeu L, Srour B, Hercberg S, Touvier M, et al. Trait impulsivity is associated with an increased risk of type 2 diabetes incidence in adults over 8 years of follow-up: results from the NutriNet-Santé cohort. BMC Med. 2024;22:332.
Testa G, Mora-Maltas B, Camacho-Barcia L, Granero R, Lucas I, Agüera Z, et al. Transdiagnostic perspective of impulsivity and compulsivity in obesity: from cognitive profile to self-reported dimensions in clinical samples with and without diabetes. Nutrients. 2021;13:4426.
Egede LE, Osborn CY. Role of motivation in the relationship between depression, self-care, and glycemic control in adults with type 2 diabetes. Diabetes Educ. 2010;36:276–83.
Gonzalez JS, Safren SA, Cagliero E, Wexler DJ, Delahanty L, Wittenberg E, et al. Depression, self-care, and medication adherence in type 2 diabetes: relationships across the full range of symptom severity. Diabetes Care. 2007;30:2222–7.
Sirirak T, Sangsupawanich P, Wongpakaran N, Srisintorn W. The geriatric depression scale predicts glycemic control in older adult with type 2 diabetes mellitus: a longitudinal study. Healthcare. 2022;10:1990.
Nübel J, Truthmann J, Heidemann C, Du Y, Paprott R, Hapke U, et al. Sex-specific impact of major depressive disorder on 12-year change in glycaemic status: results from a nationwide cohort study of adults without diabetes in Germany. Diabet Med. 2022;39:e14767.
Lunghi C, Moisan J, Gregoire JP, Guenette L. The association between depression and medication nonpersistence in new users of antidiabetic drugs. Value Health. 2017;20:728–35.
Lunghi C, Zongo A, Moisan J, Grégoire J-P, Guénette L. The impact of incident depression on medication adherence in patients with type 2 diabetes. Diabetes Metab. 2017;43:521–8.
Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. 2008;31:2398–403.
Gonzalez JS, Safren SA, Delahanty LM, Cagliero E, Wexler DJ, Meigs JB, et al. Symptoms of depression prospectively predict poorer self-care in patients with Type 2 diabetes. Diabet Med. 2008;25:1102–7.
Lin EH, Katon W, Von Korff M, Rutter C, Simon GE, Oliver M, et al. Relationship of depression and diabetes self-care, medication adherence, and preventive care. Diabetes Care. 2004;27:2154–60.
Kamrul-Hasan ABM, Hannan MA, Asaduzzaman M, Rahman MM, Alam MS, Amin MN, et al. Prevalence and predictors of diabetes distress among adults with type 2 diabetes mellitus: a facility-based cross-sectional study of Bangladesh. BMC Endocr Disord. 2022;22:28.
Gonzalez JS, Kane NS, Binko DH, Shapira A, Hoogendoorn CJ. Tangled up in blue: unraveling the links between emotional distress and treatment adherence in type 2 diabetes. Diabetes Care. 2016;39:2182–9.
Dehvan F, Baghi V, Lotfi A, Ghanei Gheshlagh R. Medication adherence inhibitors and facilitators in type 2 diabetic patients: an integrative review. Sci J Nurs Midwifery Paramed Fac. 2017;3:1–17.
Lin EH, Rutter CM, Katon W, Heckbert SR, Ciechanowski P, Oliver MM, et al. Depression and advanced complications of diabetes: a prospective cohort study. Diabetes Care. 2010;33:264–9.
van Dooren FE, Nefs G, Schram MT, Verhey FR, Denollet J, Pouwer F. Depression and risk of mortality in people with diabetes mellitus: a systematic review and meta-analysis. PLoS ONE. 2013;8:e57058.
Egede LE. Effect of depression on self-management behaviors and health outcomes in adults with type 2 diabetes. Curr Diabetes Rev. 2005;1:235–43.
Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28:1339–45.
Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life: a population study. Diabetes Care. 2004;27:1066–70.
Lam RW, Kennedy SH, Adams C, Bahji A, Beaulieu S, Bhat V, et al. Canadian network for mood and anxiety treatments (CANMAT) 2023 update on clinical guidelines for management of major depressive disorder in adults: réseau canadien pour les traitements de l’humeur et de l’anxiété (CANMAT) 2023: Mise à jour des lignes directrices cliniques pour la prise en charge du trouble dépressif majeur chez les adultes. Can J Psychiatry. 2024;69:641–87.
Greene CRL, Blackbourn LAK, McGurnaghan SJ, Mercer SW, Smith DJ, Wild SH, et al. Antidepressant and antipsychotic prescribing in patients with type 2 diabetes in Scotland: a time-trend analysis from 2004 to 2021. Br J Clin Pharmacol. 2024;90:2802–10.
National Institute for Health and Care Excellence (NICE). Neuropathic pain in adults: pharmacological management in non-specialist settings. London: National Institute for Health and Care Excellence (NICE); 2020. https://www.ncbi.nlm.nih.gov/books/NBK552848/.
Serretti A, Mandelli L. Antidepressants and body weight: a comprehensive review and meta-analysis. J Clin Psychiatry. 2010;71:1259–72.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018;17:83.
Kahl KG, Westhoff-Bleck M, Krüger THC. Effects of psychopharmacological treatment with antidepressants on the vascular system. Vascul Pharmacol. 2017;96–98:11–18.
Spielmans GI, Berman MI, Linardatos E, Rosenlicht NZ, Perry A, Tsai AC. Adjunctive atypical antipsychotic treatment for major depressive disorder: a meta-analysis of depression, quality of life, and safety outcomes. PLoS Med. 2013;10:e1001403.
Manu P, Correll CU, Wampers M, van Winkel R, Yu W, Shiffeldrim D, et al. Insulin secretion in patients receiving clozapine, olanzapine, quetiapine and risperidone. Schizophr Res. 2013;143:358–62.
Newcomer JW, Meehan SR, Chen D, Brubaker M, Weiss C. Changes in metabolic parameters and body weight in patients with prediabetes treated with adjunctive brexpiprazole for major depressive disorder: pooled analysis of short- and long-term clinical studies. J Clin Psychiatry. 2023;84:23m14786.
Salvi V, Grua I, Cerveri G, Mencacci C, Barone-Adesi F. The risk of new-onset diabetes in antidepressant users—a systematic review and meta-analysis. PLoS ONE. 2017;12:e0182088.
Kivimäki M, Hamer M, Batty GD, Geddes JR, Tabak AG, Pentti J, et al. Antidepressant medication use, weight gain, and risk of type 2 diabetes. Diabetes Care. 2010;33:2611–6.
Sun JW, Hernández-Díaz S, Haneuse S, Bourgeois FT, Vine SM, Olfson M, et al. Association of selective serotonin reuptake inhibitors with the risk of type 2 diabetes in children and adolescents. JAMA Psychiatry. 2021;78:91–100.
Cao TXD, Filliter C, Montastruc F, Yu OHY, Fergusson E, Rej S, et al. Selective serotonin reuptake inhibitors and the risk of type 2 diabetes mellitus in youths. J Affect Disord. 2022;318:231–7.
Azevedo Da Silva M, Fournier A, Boutron-Ruault M-C, Balkau B, Bonnet F, Nabi H, et al. Increased risk of type 2 diabetes in antidepressant users: evidence from a 6-year longitudinal study in the E3N cohort. Diabet Med. 2020;37:1866–73.
Salvi V, Barone-Adesi F, D’Ambrosio V, Albert U, Maina G. High H1-affinity antidepressants and risk of metabolic syndrome in bipolar disorder. Psychopharmacology. 2016;233:49–56.
Amsterdam JD, Shults J, Rutherford N, Schwartz S. Safety and efficacy of s-citalopram in patients with co-morbid major depression and diabetes mellitus. Neuropsychobiology. 2006;54:208–14.
Bansal N, Hudda M, Payne RA, Smith DJ, Kessler D, Wiles N. Antidepressant use and risk of adverse outcomes: population-based cohort study. BJPsych Open. 2022;8:e164.
Gehlawat P, Gupta R, Rajput R, Gahlan D, Gehlawat VK. Diabetes with comorbid depression: role of SSRI in better glycemic control. Asian J Psychiatry. 2013;6:364–8.
Goodnick PJ. Use of antidepressants in treatment of comorbid diabetes mellitus and depression as well as in diabetic neuropathy. Ann Clin Psychiatry. 2001;13:31–41.
McIntyre RS, Soczynska JK, Konarski JZ, Kennedy SH. The effect of antidepressants on glucose homeostasis and insulin sensitivity: synthesis and mechanisms. Expert Opin Drug Saf. 2006;5:157–68.
Crucitti A, Zhang Q, Nilsson M, Brecht S, Yang CR, Wernicke J. Duloxetine treatment and glycemic controls in patients with diagnoses other than diabetic peripheral neuropathic pain: a meta-analysis. Curr Med Res Opin. 2010;26:2579–88.
Zhang J, Sun R, Cai Y, Peng B, Yang X, Gao K. Efficacy and safety of antidiabetic agents for major depressive disorder and bipolar depression: a meta-analysis of randomized, double-blind, placebo-controlled trials. J Clin Med. 2024;13:1172.
Woo YS, Lim HK, Wang S-M, Bahk W-M. Clinical evidence of antidepressant effects of insulin and anti-hyperglycemic agents and implications for the pathophysiology of depression—a literature review. Int J Mol Sci. 2020;21:6969.
Pedreañez A, Carrero Y, Vargas R, Hernandez-Fonseca JP, Mosquera-Sulbaran J. Possible role of metformin as an antidepressant in diabetes. J Affect Disord. 2024;351:349–55.
Moulton CD, Hopkins CWP, Ismail K, Stahl D. Repositioning of diabetes treatments for depressive symptoms: a systematic review and meta-analysis of clinical trials. Psychoneuroendocrinology. 2018;94:91–103.
Nibber A, Singh H, Burnet P, Lennox B, Minichino A. Investigating the pro-cognitive and anti-depressant efficacy of metformin: a systematic review and meta-analysis of randomised controlled trials. J Affect Disord. 2022;310:52–59.
Aftab A, Kemp DE, Ganocy SJ, Schinagle M, Conroy C, Brownrigg B, et al. Double-blind, placebo-controlled trial of pioglitazone for bipolar depression. J Affect Disord. 2019;245:957–64.
Zeinoddini A, Sorayani M, Hassanzadeh E, Arbabi M, Farokhnia M, Salimi S, et al. Pioglitazone adjunctive therapy for depressive episode of bipolar disorder: a randomized, double-blind, placebo-controlled trial. Depress Anxiety. 2015;32:167–73.
Sepanjnia K, Modabbernia A, Ashrafi M, Modabbernia M-J, Akhondzadeh S. Pioglitazone adjunctive therapy for moderate-to-severe major depressive disorder: randomized double-blind placebo-controlled trial. Neuropsychopharmacology. 2012;37:2093–2100.
Shah P, Mudaliar S. Pioglitazone: side effect and safety profile. Expert Opin Drug Saf. 2010;9:347–54.
Palmer SC, Tendal B, Mustafa RA, Vandvik PO, Li S, Hao Q, et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2021;372:m4573.
Knudsen LB, Lau J. The discovery and development of liraglutide and semaglutide. Front Endocrinol. 2019;10:155.
Detka J, Głombik K. Insights into a possible role of glucagon-like peptide-1 receptor agonists in the treatment of depression. Pharmacol Rep. 2021;73:1020–32.
Chen X, Zhao P, Wang W, Guo L, Pan Q. The antidepressant effects of GLP-1 receptor agonists: a systematic review and meta-analysis. Am J Geriatr Psychiatry. 2024;32:117–27.
Pozzi M, Mazhar F, Peeters GGAM, Vantaggiato C, Nobile M, Clementi E, et al. A systematic review of the antidepressant effects of glucagon-like peptide 1 (GLP-1) functional agonists: further link between metabolism and psychopathology: special section on ‘translational and neuroscience studies in affective disorders’. Section Editor, Maria Nobile MD, PhD. This section of JAD focuses on the relevance of translational and neuroscience studies in providing a better understanding of the neural basis of affective disorders. The main aim is to briefly summaries relevant research findings in clinical neuroscience with particular regards to specific innovative topics in mood and anxiety disorders. J Affect Disord. 2019;257:S0165-0327(19)30593–2.
Cooper DH, Ramachandra R, Ceban F, Di Vincenzo JD, Rhee TG, Mansur RB, et al. Glucagon-like peptide 1 (GLP-1) receptor agonists as a protective factor for incident depression in patients with diabetes mellitus: a systematic review. J Psychiatr Res. 2023;164:80–89.
European Medicine Agency. Meeting highlights from the pharmacovigilance risk assessment committee (PRAC). European Medicines Agency (EMA); 2024. https://www.ema.europa.eu/en/news/meeting-highlights-pharmacovigilance-risk-assessment-committee-prac-8-11-april-2024.
U.S. Food and Drug Administration (FDA). Update on FDA’s ongoing evaluation of reports of suicidal thoughts or actions in patients taking a certain type of medicines approved for type 2 diabetes and obesity. FDA; 2024. https://www.fda.gov/drugs/drug-safety-and-availability/update-fdas-ongoing-evaluation-reports-suicidal-thoughts-or-actions-patients-taking-certain-type.
McIntyre RS. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) and suicidality: what do we know and future vistas. Expert Opin Drug Saf. 2024;23:539–42.
Lau D, Gamble J-M. Suicidality among users of glucagon-like peptide-1 receptor agonists: an emerging signal? Diabetes Obes Metab. 2024;26:1150–6.
Elovainio M, Shipley MJ, Ferrie JE, Gimeno D, Vahtera J, Marmot MG, et al. Obesity, unexplained weight loss and suicide: the original whitehall study. J Affect Disord. 2009;116:218–21.
Peterhänsel C, Petroff D, Klinitzke G, Kersting A, Wagner B. Risk of completed suicide after bariatric surgery: a systematic review. Obes Rev. 2013;14:369–82.
Castaneda D, Popov VB, Wander P, Thompson CC. Risk of suicide and self-harm is increased after bariatric surgery—a systematic review and meta-analysis. Obes Surg. 2019;29:322–33.
Gillissie ES, Le GH, Rhee TG, Cao B, Rosenblat JD, Mansur RB, et al. Evaluating anhedonia as a risk factor in suicidality: a meta-analysis. J Psychiatr Res. 2023;158:209–15.
Liebers DT, Ebina W, Iosifescu DV. Sodium-glucose cotransporter-2 inhibitors in depression. Harv Rev Psychiatry. 2023;31:214–21.
Kobayashi K, Toyoda M, Hatori N. Clinical comparison of tofogliflozin and empagliflozin based on an analysis of 24-h accumulated urine in Japanese patients with type 2 diabetes mellitus. Obes Med. 2019;14:100088.
Mousa HH, Sharawy MH, Nader MA. Empagliflozin enhances neuroplasticity in rotenone-induced parkinsonism: role of BDNF, CREB and Npas4. Life Sci. 2023;312:121258.
Mui JV, Li L, Chou OHI, Azfar N, Lee A, Hui J, et al. Comparing sodium-glucose cotransporter 2 inhibitors and dipeptidyl peptidase-4 inhibitors on new-onset depression: a propensity score-matched study in Hong Kong. Acta Diabetol. 2023;60:917–27.
Wium-Andersen IK, Osler M, Jørgensen MB, Rungby J, Wium-Andersen MK. Diabetes, antidiabetic medications and risk of depression—a population-based cohort and nested case-control study. Psychoneuroendocrinology. 2022;140:105715.
Zandifar A, Panahi M, Badrfam R, Qorbani M. Efficacy of empagliflozin as adjunctive therapy to citalopram in major depressive disorder: a randomized double-blind, placebo-controlled clinical trial. BMC Psychiatry. 2024;24:163.
Wittenberg GM, Stylianou A, Zhang Y, Sun Y, Gupta A, Jagannatha PS, et al. Effects of immunomodulatory drugs on depressive symptoms: a mega-analysis of randomized, placebo-controlled clinical trials in inflammatory disorders. Mol Psychiatry. 2020;25:1275–85.
Köhler-Forsberg O, Lydholm C, Hjorthøj C, Nordentoft M, Mors O, Benros ME. Efficacy of anti-inflammatory treatment on major depressive disorder or depressive symptoms: meta-analysis of clinical trials. Acta Psychiatr Scand. 2019;139:404–19.
Hellmann-Regen J, Clemens V, Grözinger M, Kornhuber J, Reif A, Prvulovic D, et al. Effect of minocycline on depressive symptoms in patients with treatment-resistant depression: a randomized clinical trial. JAMA Netw Open. 2022;5:e2230367.
Miller AH, Pariante CM. Trial failures of anti-inflammatory drugs in depression. Lancet Psychiatry. 2020;7:837.
Bavaresco DV, Uggioni MLR, Ferraz SD, Marques RMM, Simon CS, Dagostin VS, et al. Efficacy of infliximab in treatment-resistant depression: a systematic review and meta-analysis. Pharmacol Biochem Behav. 2020;188:172838.
McIntyre RS, Subramaniapillai M, Lee Y, Pan Z, Carmona NE, Shekotikhina M, et al. Efficacy of adjunctive infliximab vs placebo in the treatment of adults with bipolar I/II depression: a randomized clinical trial. JAMA Psychiatry. 2019;76:783–90.
Raison CL, Rutherford RE, Woolwine BJ, Shuo C, Schettler P, Drake DF, et al. A randomized controlled trial of the tumor necrosis factor antagonist infliximab for treatment-resistant depression: the role of baseline inflammatory biomarkers. JAMA Psychiatry. 2013;70:31–41.
Husain MI, Chaudhry IB, Khoso AB, Kiran T, Khan N, Ahmad F, et al. Effect of adjunctive simvastatin on depressive symptoms among adults with treatment-resistant depression: a randomized clinical trial. JAMA Netw Open. 2023;6:e230147.
Moriarity DP, van Borkulo C, Alloy LB. Inflammatory phenotype of depression symptom structure: a network perspective. Brain Behav Immun. 2021;93:35–42.
Liu C, Feng X, Li Q, Wang Y, Li Q, Hua M. Adiponectin, TNF-α and inflammatory cytokines and risk of type 2 diabetes: a systematic review and meta-analysis. Cytokine. 2016;86:100–9.
Olson NC, Callas PW, Hanley AJG, Festa A, Haffner SM, Wagenknecht LE, et al. Circulating levels of TNF-α are associated with impaired glucose tolerance, increased insulin resistance, and ethnicity: the insulin resistance atherosclerosis study. J Clin Endocrinol Metab. 2012;97:1032–40.
Rohm TV, Meier DT, Olefsky JM, Donath MY. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55:31–55.
Kataria Y, Ellervik C, Mandrup-Poulsen T. Treatment of type 2 diabetes by targeting interleukin-1: a meta-analysis of 2921 patients. Semin Immunopathol. 2019;41:413–25.
Li D, Zhong J, Zhang Q, Zhang J. Effects of anti-inflammatory therapies on glycemic control in type 2 diabetes mellitus. Front Immunol. 2023;14:1125116. https://doi.org/10.3389/fimmu.2023.1125116.
Herder C, Schmitt A, Budden F, Reimer A, Kulzer B, Roden M, et al. Association between pro- and anti-inflammatory cytokines and depressive symptoms in patients with diabetes—potential differences by diabetes type and depression scores. Transl Psychiatry. 2018;7:1–10.
Laake J-PS, Stahl D, Amiel SA, Petrak F, Sherwood RA, Pickup JC, et al. The association between depressive symptoms and systemic inflammation in people with type 2 diabetes: findings from the South London diabetes study. Diabetes Care. 2014;37:2186–92.
Li Q, Wu H, Cao X, Tang S, Zhao J. The association between statin use and depression in diabetes. J Affect Disord. 2024;349:342–8.
Dember LM, Hung A, Mehrotra R, Hsu JY, Raj DS, Charytan DM, et al. A randomized controlled pilot trial of anakinra for hemodialysis inflammation. Kidney Int. 2022;102:1178–87.
Singh JA, Hossain A, Kotb A, Wells G. Risk of serious infections with immunosuppressive drugs and glucocorti coids for lupus nephritis: a systematic review and network meta-analys is. BMC Med. 2016;14:137. https://doi.org/10.1186/s12916-016-0673-8.
Coghill AE, Johnson LG, Berg D, Resler AJ, Leca N, Madeleine MM. Immunosuppressive medications and squamous cell skin carcinoma: nested case-control study within the skin cancer after organ transplant (SCOT) cohort. Am J Transplant. 2016;16:565–73.
Rollan MP, Cabrera R, Schwartz RA. Current knowledge of immunosuppression as a risk factor for skin cance r development. Crit Rev Oncol Hematol. 2022;177:103754.
Opałka B, Żołnierczuk M, Grabowska M. Immunosuppressive agents—effects on the cardiovascular system and sele cted metabolic aspects: a review. J Clin Med. 2023;12:6935.
Lin EHB, Von Korff M, Alonso J, Angermeyer MC, Anthony J, Bromet E, et al. Mental disorders among persons with diabetes–results from the world mental health surveys. J Psychosom Res. 2008;65:571–80.
Li C, Barker L, Ford ES, Zhang X, Strine TW, Mokdad AH. Diabetes and anxiety in US adults: findings from the 2006 behavioral risk factor surveillance system. Diabet Med. 2008;25:878–81.
Cummings DM, Lutes LD, Littlewood K, Solar C, Carraway M, Kirian K, et al. Randomized trial of a tailored cognitive behavioral intervention in type 2 diabetes with comorbid depressive and/or regimen-related distress symptoms: 12-month outcomes from COMRADE. Diabetes Care. 2019;42:841–8.
Snoek FJ, Anarte-Ortiz MT, Anderbro T, Cyranka K, Hendrieckx C, Hermanns N, et al. Roles and competencies of the clinical psychologist in adult diabetes care—a consensus report. Diabet Med. 2024;41:e15312.
Ngan HY, Chong YY, Chien WT. Effects of mindfulness- and acceptance-based interventions on diabetes distress and glycaemic level in people with type 2 diabetes: systematic review and meta-analysis. Diabet Med. 2021;38:e14525.
Vlachou E, Ntikoudi A, Owens DA, Nikolakopoulou M, Chalimourdas T, Cauli O. Effectiveness of cognitive behavioral therapy-based interventions on psychological symptoms in adults with type 2 diabetes mellitus: an update review of randomized controlled trials. J Diabetes Complications. 2022;36:108185.
Polonsky WH, Fisher L, Earles J, Dudl RJ, Lees J, Mullan J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28:626–31.
Perrin NE, Davies MJ, Robertson N, Snoek FJ, Khunti K. The prevalence of diabetes-specific emotional distress in people with type 2 diabetes: a systematic review and meta-analysis. Diabet Med. 2017;34:1508–20.
Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39:2126–40.
King DK, Glasgow RE, Toobert DJ, Strycker LA, Estabrooks PA, Osuna D, et al. Self-efficacy, problem solving, and social-environmental support are associated with diabetes self-management behaviors. Diabetes Care. 2010;33:751–3.
American Diabetes Association. 3. Foundations of care and comprehensive medical evaluation. Diabetes Care. 2015;39:S23–S35.
Evert AB, Boucher JL, Cypress M, Dunbar SA, Franz MJ, Mayer-Davis EJ, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care. 2014;37:S120–43.
Kurnik Mesarič K, Pajek J, Logar Zakrajšek B, Bogataj Š, Kodrič J. Cognitive behavioral therapy for lifestyle changes in patients with obesity and type 2 diabetes: a systematic review and meta-analysis. Sci Rep. 2023;13:12793.
World Health Organization. Physical activity. 2024. https://www.who.int/news-room/fact-sheets/detail/physical-activity.
Shah SZA, Karam JA, Zeb A, Ullah R, Shah A, Haq IU, et al. Movement is improvement: the therapeutic effects of exercise and general physical activity on glycemic control in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Diabetes Ther. 2021;12:707–32.
Syeda USA, Battillo D, Visaria A, Malin SK. The importance of exercise for glycemic control in type 2 diabetes. Am J Med Open. 2023;9:100031.
Noetel M, Sanders T, Gallardo-Gómez D, Taylor P, Del Pozo Cruz B, van den Hoek D, et al. Effect of exercise for depression: systematic review and network meta-analysis of randomised controlled trials. BMJ. 2024;384:e075847.
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11:607–15.
Acknowledgements
CL is supported by the “PON Ricerca e Innovazione-Istruzione e ricerca per il recupero-REACT-EU ”fundsfromtheItalian Ministry of University and Research.
Author information
Authors and Affiliations
Contributions
CL conceptualized and defined the scope and content of the review. GF, ER, GH, SM, CS, EP, and CL each authored specific sections of the manuscript based on their respective areas of expertise. CL also coordinated and harmonized all contributions to ensure consistency and coherence throughout the manuscript. GH designed the figure included in the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fanelli, G., Raschi, E., Hafez, G. et al. The interface of depression and diabetes: treatment considerations. Transl Psychiatry 15, 22 (2025). https://doi.org/10.1038/s41398-025-03234-5
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03234-5
This article is cited by
-
Social, psychosocial, and lifestyle determinants of diabetes and prediabetes in US adults before and after COVID-19: a cross-sectional NHANES analysis
Diabetology & Metabolic Syndrome (2026)
-
Systemic impacts of diabetes on spermatogenesis and intervention strategies: multilayered mechanism analysis and cutting-edge therapeutic approaches
Reproductive Biology and Endocrinology (2025)
-
Integrative technologies in nursing-led interventions for diabetes management: a systematic review of efficacy and outcomes
BMC Nursing (2025)
-
Non-linear association between Life’s Essential 8 and diabetic retinopathy: mediating role of depression in US adults with diabetes
BMC Public Health (2025)
-
Insulin resistance as an early marker in youth with mood disorders
Nature Mental Health (2025)