Abstract
Background
Suicide is a global public health problem with few empirically supported treatments.
Methods
We conducted a systematic review of clinical trials (CT) since 2020 of racemic ketamine or one of its enantiomers’ (R/S) potential to reduce suicidal ideation or behavior (SIB). An initial PubMed search on April 15th, 2024 yielded 2483 results. 104 relevant CTs were identified. An additional search using other search engines on March 19th, 2024 yielded 52 sources. After screening, 14 RCTs met the inclusion criteria which required clinically significant SIB among participants, ketamine or one of its enantiomers as an anti-SIB treatment, and SIB as an outcome. We excluded neuroimaging studies, meta-analyses, reviews, and case reports. Open-label studies were also excluded except in the case of R-ketamine where we included 2 open trials due to limited published data for this enantiomer, yielding a total of 16 CTs. We used the Revised Cochrane risk-of-bias tool for the RCTs. CTs reviewed had suicidal ideation (SI) but none had suicidal behavior as an outcome.
Results
The studies include ketamine augmentation of other treatments such as electroconvulsive therapy (ECT), various routes of administration – intravenous (IV), intramuscular (IM), and intranasal (IN) – and single versus multiple dose designs. Multiple doses of IV ketamine/S-ketamine produced reductions in SI for periods of several days to weeks, while single doses showed shorter, more variable effects. Multiple and single doses of IN ketamine/S-ketamine and single doses of IV ketamine produced less consistent anti-SI results. IN and IV ketamine/S-ketamine administration appears to be well tolerated. R-ketamine appears to produce fewer side effects, but additional clinical research is needed to clarify its antidepressant and anti-SI effects in humans.
Conclusion
This review affirms the time-limited, anti-SI effects of ketamine and the need for personalized treatment. Limitations include study heterogeneity, small samples, and paucity of data for suicidal behavior or R-ketamine.
Similar content being viewed by others
Introduction
Suicide remains a devastating global public health problem, ranking as the fourth leading cause of death worldwide in adolescents and young adults [1]. Suicide rates in the United States have risen almost every year since 2000 and exceeded 49,000 deaths in 2022 [2]. Antidepressant medications and psychotherapy are evidence-based treatments for depressive disorders that most commonly underlie suicidal ideation and behavior (SIB), but despite expanded use, approximately 76% of suicide decedents are not on psychotropic medications at the time of death [3]. Reasons likely include obstacles to treatment such as failure to seek help, poor insight, stigma, inadequate insurance coverage, limited treatment resources, and possibly the slow onset of therapeutic benefit over weeks to months [4].
Ketamine has emerged as a promising and rapid-acting treatment for suicidal ideation (SI) [5,6,7]. Ketamine is novel in its rapid onset of action and efficacy in Treatment-Resistant Depression (TRD) [8]. Ketamine is a racemic mixture of two enantiomers — (S)-ketamine (esketamine) and (R)-ketamine (arketamine). Human studies in psychiatry have mostly used the racemic compound. Most enantiomer-specific data come from industry studies leading to the 2019 approval of S-ketamine in addition to standard medication for TRD and acute suicidal ideation [9, 10].
Early studies in the anesthesiology literature suggested less psychomotor impairment with S- or R- compared with racemic ketamine [11,12,13,14]. More recent RCTs in TRD [15] and healthy volunteers [16] demonstrated similar neurocognitive and hemodynamic side effects with sub-anesthetic S- or racemic ketamine. A meta-analysis in depression found that racemic ketamine had better overall response and remission from depression, as well as fewer drop-outs due to adverse events compared to S-ketamine [17]. Overall, studies suggest that S-ketamine causes greater psychotomimetic and cognitive impairment effects than R-ketamine due to its greater inhibition of NMDA receptors [18]. Clinical research on R-ketamine remains limited with most published studies using animal models. Pre-clinical data suggest that R-ketamine may have potential utility for TRD [19], but additional clinical studies are needed to verify its effectiveness in humans.
The difference in potency of psychotomimetic and dissociative symptoms between the enantiomers may influence the anti-SI and antidepressant responses. There is conflicting research, however, on whether the dissociative effects of ketamine are related to its antidepressant and anti-SI effects [20]. Our recent analysis found that ketamine’s acute dissociative or psychotomimetic effects in an IV midazolam-controlled, randomized trial were not associated with its antidepressant and anti-SI properties [21].
Our goal was to systematically review the most recent evidence on the efficacy of ketamine or one of its R/S enantiomers as a treatment for SIB. Our review focused on randomized controlled trials (RCT) of ketamine treatment in participants presenting with clinically significant suicidal ideation (SI). Given the paucity of human trials of R-ketamine we included two open and one randomized trial, though their primary focus was depression and not SI [22,23,24]. We followed the methodology of our previous systematic review [25], searching subsequent literature on “ketamine” and “suicide” to incorporate the latest research since 2020. We also looked at enantiomer-specific studies, and utilized RCTs with both primary and secondary outcomes for SI. We included post-hoc analyses of past RCTs and examined safety results from the included studies.
Methods
Following PRISMA systematic review guidelines [26], ketamine and/or one of its (R/S) enantiomers’ effects on SIB. We conducted a PubMed search on April 15th, 2024 with the following terms “((ketamine) AND (suicide)) OR (esketamine) OR (arketamine) OR (S-Ketamine) OR (R-Ketamine))” which yielded 2483 results. We refined our search by filtering for “clinical trial” and “randomized controlled trial”(RCT), which yielded 436 studies for possible inclusion. To pick up where our prior review left off [25], the current search was limited to publications from 2020–2024 resulting in 222 findings. Of these, 104 studies were found to be novel and relevant. We incorporated the results of a separate literature review on March 19th, 2024, that used other search engines including Google Scholar, and ClinicalTrials.gov. This identified 52 potential additional sources of which 6 were duplicates from the PubMed search and 17 were found to be relevant.
All studies were screened for eligibility using an Excel spreadsheet with relevant inclusion and exclusion criteria. Eligibility criteria were: publication year after 2019, RCT, inclusion of participants with clinically significant SIB, administration of ketamine or one of its enantiomers as an anti-SIB treatment, and measurement of SIB as a primary or secondary outcome. Like our previous systematic review, we excluded: neuroimaging studies, meta-analyses, reviews, case reports, or open-label studies. While our inclusion criteria required RCTs, SIB at baseline, and measurement of SIB as a primary or secondary outcome, due to the limited number of studies on R-ketamine, we included 2 published open-label trials and 1 RCT. Of these, only one open-label trial reported SI as an outcome.
We only included post-hoc analyses if the original study was an RCT. We excluded records based on the abstract and title, and then read full-text versions of the remaining 121 studies (from both literature searches) to assess for inclusion.
One reviewer (S.S.), under the supervision of another investigator (M.G.), reviewed the literature and extracted data into a standardized spreadsheet as follows: country of study enrollment, publication year, funding, sample size, age and population, design, intervention, control drug, measure of SIB, and main findings (Tables 1–3). The included studies use various rating scales to quantify SIB as an outcome. Beck’s Scale for Suicidal Ideation, with clinician-rated (SSI) and self-report (BSI) formats, is an established measure for assessing SI severity [27, 28]. The Columbia-Suicide Severity Rating Scale (C-SSRS) has sections assessing SIB [29]. Other instruments such as the Montgomery Asberg Depression Rating Scale (MADRS) [30] and the Hamilton Depression Rating Scale (HDRS) [31] each contain one item assessing SIB but are validated as measures of depression symptom severity. Other rating scales include the Positive and Negative Suicide Ideation Inventory (PANSI), a 14-item self-reported measure assessing SI [32]. The Suicide Probability Scale (SPS), is a 36-item self-report measure that assesses suicide risk, well-being, and coping behavior [33]. The Suicide Ideation and Behavior Assessment Tool (SIBAT) is a clinician- and patient-reported assessment of SIB which includes the Clinical Global Impression–Severity of Suicidality–revised (CGI-SS-r), Clinical Global Impression of Imminent Suicide Risk (CGI-SR-I), and clinician- and patient-reported Frequency of Suicidal Thinking (FoST) [34]. The Clinical Global Impression (CGI) is a 3-item observer-rated scale assessing severity, global improvement or change, and therapeutic response [35].
We used the Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) to examine potential bias in the included RCT studies (see online supplement for details) [36].
Results
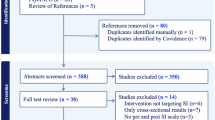
Sixteen studies were included in this systematic review. Four studies were identified from an independent literature review, and twelve were identified from a PubMed search. Figure 1 depicts a flowchart of the article selection process.
Flowchart of literature review and screening for articles per PRISMA guidelines. A database search was combined with an independent search, yielding a total of 16 studies included in the review. The figure outlines all records excluded at each stage of the review, along with the reasons for exclusion.
From the included studies, ten were independent RCTs, and four were secondary analyses of prior RCTs. Two studies were open-label R-ketamine trials. Tables 1, 2, and 3 outline characteristics, respectively, of novel RCTs, post-hoc analyses of prior RCTs, and open-label R-ketamine CTs. The examination of bias using RoB-2 is summarized in Fig. 2 (see online supplement for details). Table 4 provides relevant information on experimental setup (IM, IN, IV), frequency of treatment (single vs multiple), type of drug (racemic vs S- or R-ketamine), and type of analysis (independent vs post-hoc). For brevity, we refer to racemic ketamine as “ketamine” or specify an enantiomer.
Percentage estimates of potential bias using the RoB-2 bias tool with studies reviewed. Studies were assessed for potential bias across five domains: selection of reported results, measurement of the outcome, missing outcome data, deviations from intended interventions, and the randomization process. Green bars represent low risk, yellow bars represent some concern, and red bars represent high risk. All studies showed low risk in the missing outcome data, while most studies showed some concern in the selection of reported results.
Several studies were excluded due to specific criteria. Floden et al. and Turkoz et al. were secondary analyses of previous RCTs (TRANSFORM I and TRANSFORM II) which we excluded because they did not enroll individuals with SI. Cigognini et al. [37], an ongoing trial, and Ren et al. [38] were excluded for the same reason. We removed Averill et al. because the study design involved an open-label ketamine infusion. Lastly, we removed Loo et al. because they did not report results for SI despite the fact that it was designated as a secondary outcome. While some studies included measures examining suicidal behavior (SB), none reported any outcomes for SB, thus all outcomes we describe involve anti-SI effects.
Intravenous ketamine or S-ketamine
The majority of IV studies (6 of 8) used racemic ketamine [39,40,41,42,43,44]. Of these, one parallel assignment, double-blind RCT in a sample of 22 participants with borderline personality disorder and active SI found numerically greater reduction in SI post-injection with ketamine as compared to midazolam though the result was not statistically significant [42]. Others found a significant anti-SI effect of racemic ketamine that persisted till Day 3 [39], Day 5 [43, 44], and Week 2 [40].
Abbar and colleagues’ double-blind, saline-controlled RCT (N = 156 participants with an SSI score > 3) found that ketamine treatment led to significantly greater rates of remission of SI (defined as a total SSI score of ≤ 3 at follow-up), on Day 3 compared to those receiving the placebo (95% CI; 1.9 to 7.3, P < 0.001).
Lin et al. conducted a post-hoc analysis of two double-blind, midazolam and saline-controlled clinical trials including 65 participants with TRD and suicidal thoughts, as defined by a MADRS item 10 score ≥ 4. They found superiority of ketamine in the rate of full remission of SI from Day 1 (p = 0.001) to Day 5 post-infusion (p = 0.044) [43].
Similarly, Su and colleagues’ double-blind, RCT of 84 outpatients diagnosed with TRD and SI (MADRS item 10 score ≥ 4) found greater anti-SI effects of ketamine as compared to midazolam, on the Columbia-Suicide Severity Rating Scale Ideation Severity Subscale (P = 0.040) and MADRS item 10 (P = 0.023), which persisted for 5 days post-infusion [44].
Ahmed et al. conducted a parallel-arm randomized saline-controlled trial in 36 patients with TRD and current suicidal risk “based on psychiatric interview.” No scale cut-off was provided. They found a significant decrease in total Suicide Probability Scale (SPS) scores in the ketamine group compared to the control up to 2 weeks post-treatment (P = 0.009) [40].
A secondary analysis of a multisite midazolam-controlled RCT in 56 subjects with unipolar TRD, in a current MDE, on a stable antidepressant dose, and with SI (MADRS suicide item score ≥ 2) found mixed results. Among participants with clinically significant baseline SI (MADRS suicide item score ≥ 2), results showed lower SI at 30 days post-infusion in the IV racemic ketamine group (2.03 ± 1.59 vs. 3.00 ± 1.41, p = 0.049). However, in the subgroup who had an early anti-SI response (MADRS suicide item score < 2 at day 3), there were no subsequent differences between ketamine and midazolam groups from Day 5 to Day 30 post-infusion, indicating a rapid loss of effect [41].
Two studies investigated intravenous S-ketamine [45, 46]. A randomized, midazolam-controlled trial administered 3 infusions of S-ketamine (0.25 mg/kg) or midazolam (0.02 mg/kg) over 5 days, along with standard inpatient care to 54 inpatients with MDD and SI (C-SSRS ideation score ≥ 1 and SSI Item 4 or 5 score ≥ 2) [46]. Zhou et al. found that the S-ketamine group had greater improvements in SI as indicated by the mean change in the C-SSRS ideation score from baseline to day 6 as compared to midazolam (P = 0.002). Additionally, a significant reduction in the C-SSRS Intensity score was also observed for S-ketamine compared to midazolam (P = 0.004). Sustained benefits were not observed.
One double-blind randomized trial in a naturalistic sample of 59 subjects with TRD and SI (score ≥ 1 for MADRS item 10) tested a single IV dose of S-ketamine (0.25 mg/kg) versus racemic ketamine (0.5 mg/kg). Results showed that S- and racemic ketamine were equally effective in reducing SI in TRD subjects up to 7 days post-infusion [45].
Intramuscular ketamine
One parallel assignment, non-blinded clinical trial randomized 45 adults with MDD who had been assessed as candidates for electroconvulsive therapy (ECT) to either ECT or racemic ketamine given intramuscularly (IM) at 0.5 mg/kg or orally at 1 mg/kg. All three groups received 6–9 ketamine doses or ECT sessions during 3 weeks and effects on the Beck SSI were analyzed. Results showed similar anti-SI effects of oral and IM ketamine which were superior to ECT at 2-weeks (p = 0.033) with a trend toward superiority at 3 weeks (p = 0.069). The three groups showed equal anti-depressant effects (P < 0.001 for the HDRS) [47].
Intranasal ketamine or S-ketamine
One of four studies tested intranasal (IN) racemic ketamine in a double-blind, saline-controlled, proof-of-concept RCT in a trans-diagnostic sample of 30 subjects, with SI score > 2 on the clinician-administered C-SSRS and at least 3 on the first five items of the self-report Beck Scale for Suicidal Ideation (BSS) and in need of psychiatric hospitalization. Results showed that four squirts (10 mg each) of IN racemic ketamine each separated by 10 min resulted in a significant decrease in SI at 4 h post-treatment, along with an 80% rate of remission from SI, compared with 33% for the saline placebo group [48].
The other three reports were from the two Janssen Inc. phase 3 trials of IN S-ketamine for MDD with acute SI [49,50,51]. In the first “Aspire 1” study at 51 study sites, 226 adults with non-psychotic MDD and SI with intent in the past 24 h and clinical need of psychiatric hospitalization due to suicide risk, were randomized to 84 mg of S-ketamine or placebo twice weekly for 4 weeks in addition to standard oral antidepressant medication [50]. The primary outcome was change in MADRS total score from baseline to 24 h post-first dose. The main secondary outcome was change in Clinical Global Impression of Severity of Suicidality Revised (CGI-SS-r; rated from 0 [no SI] to 6 [extremely suicidal]) from baseline to 24 h. Results showed superiority for S-ketamine on change in total MADRS score but not on the SI outcome at 24 h [50]. The second identically designed “Aspire 2” study at 47 sites, randomized 227 adults with the same eligibility criteria and replicated the Aspire 1 results finding superiority for S-ketamine on reduction in total MADRS score at 24 h but a non-significant difference from placebo in SI improvement at 24 h [51]. The third report was a post-hoc analysis of the pooled Aspire 1 and 2 data which replicated the MADRS total score and SI results for all patients but found a statistically significant result for superiority of SI improvement at 24 h for S-ketamine in the subgroup with history of a suicide attempt (95%CI −0.61 to −0.01) [49].
Single vs multiple doses
The efficacy of IV ketamine or IV S-ketamine in reducing SI may vary depending on the frequency of administration. Three abovementioned studies reported a decline in the anti-SI effects of a single administration of IV ketamine from Day 3 to Day 7 [41, 43, 44]. In contrast, multiple doses of IV ketamine or S-ketamine were associated with anti-SI effects over longer periods of 2 days to 6 weeks [39, 40, 46]. Abbar et al. (subjects received 2 doses over 2 days) observed a greater reduction of SI in the ketamine compared to the saline placebo group on Day 3, with a significantly higher remission rate at 72 h post-infusion. At week 6, the remission rate was numerically greater in the ketamine than the placebo group (69.5 v 56.3%) though the difference was not statistically significant (p = 0.7). Ahmed et al. (2 doses ketamine vs saline placebo over 2 weeks) found greater reductions in SI at 90 min and Week 1 post-ketamine compared to placebo. Zhou et al. (3 infusions over 5 days) found that, compared with midazolam, the S-ketamine group had greater improvements in SI and depressive symptoms from Days 1 to 6 post-infusion. In one SI measure, the SSI-5, they found a greater number of participants free of SI up to Day 12.
In the post-hoc, pooled analysis of the Janssen Aspire 1 and 2 trials of S-ketamine, more patients in the S-ketamine group achieved resolution of SI (CGI-SS-r score 0–1) at 4 h after the first dose compared to placebo (95% CI for difference 5.1–21.3) but the difference from placebo was not statistically significant at 24 h or 25 days [49]. The authors conclude, “Esketamine nasal spray is approved in conjunction with an oral antidepressant to treat depressive symptoms, but not for reducing suicidal ideation or behavior, in adults with MDD and acute suicidal ideation or behavior” [49].
Ketamine for augmentation
There were conflicting findings on whether psychiatric diagnosis or past treatment course could moderate ketamine effects on SI. Ahmed et al. found that other psychiatric symptoms or personality disorders did not influence ketamine’s anti-SI response. Meanwhile, Abbar et al. found a stronger anti-SI effect of ketamine in individuals with bipolar compared to unipolar mood disorder. A study by Su et al. [44] found the anti-SI effects of ketamine were particularly notable in participants whose current depressive episode lasted less than 24 months or who had four or fewer prior failed trials of antidepressant medication. Similarly, S-ketamine showed a greater reduction of SI at 24 h among patients with a history of suicide attempts, compared to placebo [49]. Another study found that lower cognitive impairment at baseline was associated with quicker and more sustained anti-SI effects of ketamine [43]. None of these findings are replicated by other independent studies.
R-ketamine
Studies in rodent models of depression suggest that R-ketamine may be a more potent and longer-lasting antidepressant compared to S-ketamine [52,53,54,55] with fewer dissociative and psychotomimetic effects and lower abuse potential [16, 52, 55,56,57]. The long-lasting antidepressant effect has been thought to be due to increases in BDNF-TrkB signaling and synaptogenesis [55]. A comparative study of behavioral side effects in animal models showed that S-ketamine increased locomotion and muscle rigidity while R-ketamine did not induce these effects [58]. Pre-clinical studies yield valuable insights into ketamine’s potential antidepressant effects and mechanism, however, their applicability to human psychiatric illness has obvious limitations, particularly so for suicidal ideation and behavior which are not seen in animal models [59].
There are few studies of R-ketamine in depressed human participants and none report effects on SI. A within-subject, placebo-controlled PET study in ten healthy volunteers found that R-ketamine induced relaxation whereas S-ketamine produced psychotic symptoms, including derealization, hallucinations, and ego-disintegration, however, it is unclear if this non-clinical sample is relevant to depression [60].
Three R-ketamine studies were included in this review [22,23,24]. One trial looked at SI as an outcome [24], while the other two reported on depressive symptoms [22, 23]. An open-label trial in 7 depressed adults found that IV R-ketamine produced fast-onset and sustained antidepressant effects with a favorable safety profile [22]. Another open-label trial of R-ketamine in 6 participants with bipolar depression administered two infusions one week apart at 0.5 and 1.0 mg/kg and found almost 50% improvement in depressive symptoms 24 h after the 1.0 mg/kg dose and decreased SI (based on MADRS item 10) by 60% without significant dissociation [24]. However, the only randomized, saline-controlled trial, to our knowledge, in 10 depressed adults, found that R-ketamine had almost no dissociative or psychotomimetic effects, in line with animal studies, but its antidepressant effect did not separate from placebo [23].
Adverse effects and safety
Most studies found that common adverse effects (e.g. dissociation, dizziness, hypertension, nausea) occurred during the infusion but subsided within the same day [22,23,24, 40, 44, 46,47,48,49]. Other studies highlighted the mild nature of the adverse effects, reporting that ketamine was well-tolerated with no serious incidents [39, 42, 45]. Some studies indicated that the observed adverse effects were consistent with the established safety profile of S-ketamine nasal spray [50, 51].
Discussion
This systematic review of CTs since 2020 supports the efficacy of ketamine and S-ketamine for rapid but short-term treatment of SI, with stronger effects in IV and multi-dose administrations compared, respectively, to IN or single doses. The one RCT reviewed involving IM ketamine found an equivalent anti-SI effect to ECT. Our systematic review synthesized evidence from various administration routes, including IV, IM, and IN, as well as dose frequencies, and preparations of racemic, S- or R-ketamine. Multiple doses of IN racemic ketamine or S-ketamine rapidly reduce SI, within several hours to one day, and suggest a stronger anti-SI effect with IV compared to IN administration and an advantage for repeated ketamine treatments to prolong anti-SI effect beyond a few days to a week [41], Day 5 [44], or Day 7 post-infusion [43].
Previous studies found equivalent antidepressant responses in IV versus IM ketamine [61]. As noted above, one study found that oral and IM ketamine have equal anti-depressant and anti-SI effects compared with ECT [47]. IM ketamine has 93% bioavailability in adult humans and a plasma half-life similar to IV [62, 63], whereas IN S-ketamine is about 50% bioavailable [64,65,66]. Since the antidepressant response to ketamine is dose-sensitive [67], lower bioavailability may explain less robust SI benefits from IN compared with IV ketamine. Consistent with previous studies, this review found that repeated and single administrations of ketamine and S-ketamine have common, short-lived side effects, but generally are well tolerated [8, 68, 69]. Preliminary studies suggest R-ketamine may have fewer psychomotor side effects, but an antidepressant effect has yet to be clearly demonstrated in humans [22,23,24].
These results for the parent R-enantiomer are consistent with studies on R-ketamine metabolites, which have also been investigated for their antidepressant effects and safety properties. In a Phase I trial, the ketamine metabolite (2R,6R)-Hydroxynorketamine (RR-HNK) was found to be well tolerated at all tested doses, without serious adverse events in healthy volunteers [70]. However, published reports on potential antidepressant and anti-SI effects of RR-HNK are conflicting. A pre-clinical study finding that RR-HNK had antidepressant effects in mice [71] supports the reported antidepressant [22, 24] and anti-SI effects [24] of R-ketamine in this review. In contrast, a post-hoc analysis of our midazolam-controlled RCT in patients with MDD and clinically significant SI found an inverse association between post-infusion plasma levels of RR-HNK and improvements in SI and overall depression from baseline to 24 h post-infusion [72].
This systematic review of recent trials involving varying ketamine formulations, routes, and frequencies of administration underscores the complexity of ketamine effects on SI and the need for personalized treatment. For example, one RCT found promising effects on SI by oral and IM ketamine as compared to ECT [47]. A separate RCT of ketamine augmentation that was excluded from this review found promising effects on SI by combining IV S-ketamine with ECT [38]. Furthermore, bipolarity, the length of a depressive episode, and the number of failed trials of antidepressant treatments may play a moderating role in ketamine’s anti-SI effect [39, 44]. The age of the study population may also influence outcomes in that while most studies involved adult participants, one trial in adolescent inpatients with MDD and SI reported somewhat longer seeming improvements in SI of up to 6 days though this is only a single study [46].
Limitations of this review include the heterogeneity of studies in terms of trial designs, participant characteristics, and SI outcome measures (Table 1), which may limit the ability to draw overall conclusions. The relatively small sample sizes of some studies [42, 48] and the lack of RCT studies of R-ketamine effects on SI since 2020 are other limitations. Furthermore, due to the inclusion of secondary analyses, approximately half of the included studies were found to have ‘some’ concern in the selection of reported results as they involved a statistical plan developed after the publication of the original study.
Nonetheless, we believe the review overall supports the potential role of ketamine – in a range of formulations and dosing strategies – for the relatively rapid, short-term reduction of SI. Further research is needed to determine optimal dosing and administration methods for specific clinical populations. Larger samples will be required to study potential effects of ketamine on suicidal behavior, and follow-up studies of long-term safety are needed. Additional research on efficacy and safety of ketamine in adolescents would also be important, as suicide is the fourth leading cause of death worldwide in this age group [1]. Given the significance of suicide as a public health issue, research to optimize treatment strategies and clinical outcomes would advance the field.
Other information
This systematic review followed PRISMA guidelines; a formal protocol was not registered. All relevant materials, forms, and data used in the review will be made available upon appropriate request to the corresponding author. This work was supported by the National Institutes of Health (NIH) grant MH125155 (PI: Grunebaum).
References
World Health Organization. Mental Health of Adolescents. 2021; Available from: https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health#:~:text=Suicide%20is%20the%20fourth%20leading,lead%20fulfilling%20lives%20as%20adults.
Center for Disease Control and Prevention. Provisional suicide deaths in the United States, 2022. 2023 [cited 2024; Available from: https://www.cdc.gov/media/releases/2023/s0810-US-Suicide-Deaths-2022.html#:~:text=The%20provisional%20estimates%20released%20today,an%20increase%20of%20approximately%202.6%25.
Liu GS, Nguyen BL, Lyons BH, Sheats KJ, Wilson RF, Betz CJ, et al. Surveillance for violent deaths — national violent death reporting system, 48 states, the district of Columbia, and Puerto Rico, 2020. MMWR Surveill Summ. 2023;72:1–38.
Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, Ritz L, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40.
Zarate CA Jr., Singh JB, Carlson PJ, Brutsche NE, Ameli R, Luckenbaugh DA, et al. A randomized trial of an N-methyl-D-aspartate antagonist in treatment-resistant major depression. Arch Gen Psychiatry. 2006;63:856–64.
Grunebaum MF, Galfalvy HC, Choo TH, Keilp JG, Moitra VK, Parris MS, et al. Ketamine for rapid reduction of suicidal thoughts in major depression: a midazolam-controlled randomized clinical trial. Am J Psychiatry. 2018;175:327–35.
Wilkinson ST, Ballard ED, Bloch MH, Mathew SJ, Murrough JW, Feder A, et al. The effect of a single dose of intravenous ketamine on suicidal ideation: a systematic review and individual participant data meta-analysis. Am J Psychiatry. 2018;175:150–8.
Serafini G, Howland RH, Rovedi F, Girardi P, Amore M. The role of ketamine in treatment-resistant depression: a systematic review. Curr Neuropharmacol. 2014;12:444–61.
National Institutes of Health. Ketamine research at NIMH leads to FDA-approved anti-depressant nasal spray spravato®. 2019 November 13, 2024]; Available from: https://www.techtransfer.nih.gov/news/ketamine-research-at-nimh-leads-to-fda-approved-anti-depressant-nasal-spray-spravato-r.
Floriano I, Silvinato A, Bernardo WM. The use of esketamine in the treatment of patients with severe depression and suicidal ideation: systematic review and meta-analysis. Rev Assoc Med Bras. 2023;69:e2023D694.
White PF, Ham J, Way WL, Trevor AJ. Pharmacology of ketamine isomers in surgical patients. Anesthesiology. 1980;52:231–9.
White PF, Schüttler J, Shafer A, Stanski DR, Horai Y, Trevor AJ. Comparative pharmacology of the ketamine isomers. studies in volunteers. Br J Anaesth. 1985;57:197–203.
Muller J, Pentyala S, Dilger J, Pentyala S. Ketamine enantiomers in the rapid and sustained antidepressant effects. Ther Adv Psychopharmacol. 2016;6:185–92.
Pfenninger EG, Durieux ME, Himmelseher S. Cognitive impairment after small-dose ketamine isomers in comparison to equianalgesic racemic ketamine in human volunteers. Anesthesiology. 2002;96:357–66.
Correia-Melo FS, Leal GC, Vieira F, Jesus-Nunes AP, Mello RP, Magnavita G, et al. Efficacy and safety of adjunctive therapy using esketamine or racemic ketamine for adult treatment-resistant depression: a randomized, double-blind, non-inferiority study. J Affect Disord. 2020;264:527–34.
Passie T, Adams HA, Logemann F, Brandt SD, Wiese B, Karst M. Comparative effects of (S)-ketamine and racemic (R/S)-ketamine on psychopathology, state of consciousness and neurocognitive performance in healthy volunteers. Eur Neuropsychopharmacol. 2021;44:92–104.
Bahji A, Vazquez GH, Zarate CA Jr. Comparative efficacy of racemic ketamine and esketamine for depression: a systematic review and meta-analysis. J Affect Disord. 2021;278:542–55.
Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018;23:801–11.
Shafique H, Demers JC, Biesiada J, Golani LK, Cerne R, Smith JL, et al. (R)-(-)-ketamine: the promise of a novel treatment for psychiatric and neurological disorders. Int J Mol Sci. 2024;25:6804.
Ballard ED, Zarate CA. The role of dissociation in ketamine’s antidepressant effects. Nat Commun. 2020;11:6431.
Sajid S, Galfalvy HC, Keilp JG, Burke AK, Mann JJ, Grunebaum MF. Acute dissociation and Ketamine’s antidepressant and anti-suicidal ideation effects in a midazolam-controlled trial. Int J Neuropsychopharmacol. 2024;27:pyae017.
Leal GC, Bandeira ID, Correia-Melo FS, Telles M, Mello RP, Vieira F, et al. Intravenous arketamine for treatment-resistant depression: open-label pilot study. Eur Arch Psychiatry Clin Neurosci. 2021;271:577–82.
Leal GC, Souza-Marques B, Mello RP, Bandeira ID, Caliman-Fontes AT, Carneiro BA, et al. Arketamine as adjunctive therapy for treatment-resistant depression: a placebo-controlled pilot study. J Affect Disord. 2023;330:7–15.
Bandeira ID, Leal GC, Correia-Melo FS, Souza-Marques B, Silva SS, Lins-Silva DH, et al. Arketamine for bipolar depression: open-label, dose-escalation, pilot study. J Psychiatr Res. 2023;164:229–34.
Hochschild A, Grunebaum MF, Mann JJ. The rapid anti-suicidal ideation effect of ketamine: a systematic review. Prev Med. 2021;152:106524.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the scale for suicide ideation. J Consult Clin Psychol. 1979;47:343–52.
Beck AT, Steer RA, Ranieri WF. Scale for suicide ideation: psychometric properties of a self-report version. J Clin Psychol. 1988;44:499–505.
Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168:1266–77.
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9.
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62.
Osman A, Gutierrez PM, Kopper BA, Barrios FX, Chiros CE, et al. The positive and negative suicide ideation inventory: development and validation. Psychol Rep. 1998;82:783–93.
Cull, JG and WS Gill, Suicide Probability Scale. APA PsycTests, 1982.
Alphs L, Fu DJ, Williamson D, Jamieson C, Greist J, Harrington M. SIBAT-A computerized assessment tool for suicide ideation and behavior: Development and psychometric properties. Innov Clin Neurosci. 2022;19:36–47.
Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry. 2007;4:28–37.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Cigognini MA, Guirado AG, van de Meene D, Schneider MA, Salomon MS, de Alexandria VS. et al. Intramuscular ketamine vs. escitalopram and aripiprazole in acute and maintenance treatment of patients with treatment-resistant depression: Arandomized double-blind clinical trial. Front Psychiatry. 2022;13:830301. https://doi.org/10.3389/fpsyt.2022.830301.
Ren L, Chen Q, Gao J, Liu Y, Tao Y, Li X, et al. Clinical efficacy of adjunctive esketamine anesthesia in electroconvulsive therapy for major depressive disorders: a pragmatic, randomized, controlled trial. Psychiatry Res. 2024;335:115843.
Abbar M, Demattei C, El-Hage W, Llorca PM, Samalin L, Demaricourt P, et al. Ketamine for the acute treatment of severe suicidal ideation: double blind, randomised placebo controlled trial. BMJ. 2022;376:e067194.
Ahmed GK, Elserogy YM, Elfadl GMA, Ghada Abdelsalam K, Ali MA. Antidepressant and anti-suicidal effects of ketamine in treatment-resistant depression associated with psychiatric and personality comorbidities: a double-blind randomized trial. J Affect Disord. 2023;325:127–34.
Feeney A, Hock RS, Freeman MP, Flynn M, Hoeppner B, Iosifescu DV, et al. The effect of single administration of intravenous ketamine augmentation on suicidal ideation in treatment-resistant unipolar depression: results from a randomized double-blind study. Eur Neuropsychopharmacol. 2021;49:122–32.
Fineberg SK, Choi EY, Shapiro-Thompson R, Dhaliwal K, Neustadter E, Sakheim M, et al. A pilot randomized controlled trial of ketamine in borderline personality disorder. Neuropsychopharmacology. 2023;48:991–9.
Lin WC, Su TP, Li CT, Wu HJ, Tsai SJ, Bai YM, et al. Baseline cognitive function predicts full remission of suicidal symptoms among patients with treatment-resistant depression and strong suicidal ideation after low-dose ketamine infusion. J Psychopharmacol. 2023;37:795–801.
Su TP, Li CT, Lin WC, Wu HJ, Tsai SJ, Bai YM, et al. A randomized, double-blind, midazolam-controlled trial of low-dose ketamine infusion in patients with treatment-resistant depression and prominent suicidal ideation. Int J Neuropsychopharmacol. 2023;26:331–9.
Vieira F, Correia-Melo FS, Santos-Lima C, Souza-Marques B, Leal GC, Jesus-Nunes AP, et al. Ketamine and esketamine augmentation for suicidal ideation: a randomized, double-blinded clinical trial. Gen Hosp Psychiatry. 2021;68:97–99.
Zhou Y, Lan X, Wang C, Zhang F, Liu H, Fu L, et al. Effect of repeated intravenous esketamine on adolescents with major depressive disorder and suicidal ideation: a randomized active-placebo-controlled trial. J Am Acad Child Adolesc Psychiatry. 2024;63:507–18.
Kheirabadi D, Kheirabadi GR, Mirlohi Z, Tarrahi MJ, Norbaksh A. Comparison of rapid antidepressant and antisuicidal effects of intramuscular ketamine, oral ketamine, and electroconvulsive therapy in patients with major depressive disorder: a pilot study. J Clin Psychopharmacol. 2020;40:588–93.
Domany Y, McCullumsmith CB. Single, fixed-dose intranasal ketamine for alleviation of acute suicidal ideation. an emergency department, trans-diagnostic approach: a randomized, double-blind, placebo-controlled, proof-of-concept trial. Arch Suicide Res. 2022;26:1250–65.
Canuso CM, Ionescu DF, Li X, Qiu X, Lane R, Turkoz I, et al. Esketamine nasal spray for the rapid reduction of depressive symptoms in major depressive disorder with acute suicidal ideation or behavior. J Clin Psychopharmacol. 2021;41:516–24.
Fu DJ, Ionescu DF, Li X, Lane R, Lim P, Sanacora G, et al. Esketamine nasal spray for rapid reduction of major depressive disorder symptoms in patients who have active suicidal ideation with intent: double-blind, randomized study (ASPIRE I). J Clin Psychiatry. 2020;81:19m13191.
Ionescu DF, Fu DJ, Qiu X, Lane R, Lim P, Kasper S, et al. Esketamine nasal spray for rapid reduction of depressive symptoms in patients with major depressive disorder who have active suicide ideation with intent: results of a phase 3, double-blind, randomized study (ASPIRE II). Int J Neuropsychopharmacol. 2021;24:22–31.
Chang L, Zhang K, Pu Y, Qu Y, Wang SM, Xiong Z, et al. Comparison of antidepressant and side effects in mice after intranasal administration of (R,S)-ketamine, (R)-ketamine, and (S)-ketamine. Pharmacol Biochem Behav. 2019;181:53–59.
Fukumoto K, Toki H, Iijima M, Hashihayata T, Yamaguchi JI, Hashimoto K, et al. Antidepressant potential of (R)-ketamine in rodent models: comparison with (S)-ketamine. J Pharmacol Exp Ther. 2017;361:9–16.
Zhang JC, Li SX, Hashimoto K. R (-)-ketamine shows greater potency and longer lasting antidepressant effects than S (+)-ketamine. Pharmacol Biochem Behav. 2014;116:137–41.
Yang C, Shirayama Y, Zhang JC, Ren Q, Yao W, Ma M, et al. R-ketamine: a rapid-onset and sustained antidepressant without psychotomimetic side effects. Transl Psychiatry. 2015;5:e632.
Bonaventura J, Lam S, Carlton M, Boehm MA, Gomez JL, Solís O, et al. Pharmacological and behavioral divergence of ketamine enantiomers: implications for abuse liability. Mol Psychiatry. 2021;26:6704–22.
Zanos P, Highland JN, Liu X, Troppoli TA, Georgiou P, Lovett J, et al. (R)-ketamine exerts antidepressant actions partly via conversion to (2R,6R)-hydroxynorketamine, while causing adverse effects at sub-anaesthetic doses. Br J Pharmacol. 2019;176:2573–92.
Witkin JM, Kranzler J, Kaniecki K, Popik P, Smith JL, Hashimoto K, et al. R-(-)-ketamine modifies behavioral effects of morphine predicting efficacy as a novel therapy for opioid use disorder(1). Pharmacol Biochem Behav. 2020;194:172927.
Nestler EJ, Hyman SE. Animal models of neuropsychiatric disorders. Nat Neurosci. 2010;13:1161–9.
Vollenweider FX, Leenders KL, Oye I, Hell D, Angst J. Differential psychopathology and patterns of cerebral glucose utilisation produced by (S)- and (R)-ketamine in healthy volunteers using positron emission tomography (PET). Eur Neuropsychopharmacol. 1997;7:25–38.
Chilukuri H, Reddy NP, Pathapati RM, Manu AN, Jollu S, Shaik AB. Acute antidepressant effects of intramuscular versus intravenous ketamine. Indian J Psychol Med. 2014;36:71–6.
Clements JA, Nimmo WS, Grant IS. Bioavailability, pharmacokinetics, and analgesic activity of ketamine in humans. J Pharm Sci. 1982;71:539–42.
Zanos P, Moaddel R, Morris PJ, Riggs LM, Highland JN, Georgiou P, et al. Ketamine and ketamine metabolite pharmacology: insights into therapeutic mechanisms. Pharmacol Rev. 2018;70:621–60.
Bahr R, Lopez A, Rey JA. Intranasal esketamine (spravato(TM)) for use in treatment-resistant depression in conjunction with an oral antidepressant. P T. 2019;44:340–75.
Morrison RL, Fedgchin M, Singh J, Van Gerven J, Zuiker R, Lim KS, et al. Effect of intranasal esketamine on cognitive functioning in healthy participants: a randomized, double-blind, placebo-controlled study. Psychopharmacology. 2018;235:1107–19.
Yanagihara Y, Ohtani M, Kariya S, Uchino K, Hiraishi T, Ashizawa N, et al. Plasma concentration profiles of ketamine and norketamine after administration of various ketamine preparations to healthy Japanese volunteers. Biopharm Drug Dispos. 2003;24:37–43.
Milak MS, Rashid R, Dong Z, Kegeles LS, Grunebaum MF, Ogden RT, et al. Assessment of relationship of ketamine dose with magnetic resonance spectroscopy of Glx and GABA responses in adults with major depression: a randomized clinical trial. JAMA Netw Open. 2020;3:e2013211.
Fedgchin M, Trivedi M, Daly EJ, Melkote R, Lane R, Lim P, et al. Efficacy and safety of fixed-dose esketamine nasal spray combined with a new oral antidepressant in treatment-resistant depression: results of a randomized, double-blind, active-controlled study (TRANSFORM-1). Int J Neuropsychopharmacol. 2019;22:616–30.
Feifel D, Dadiomov D, C Lee K. Safety of repeated administration of parenteral ketamine for depression. Pharmaceuticals. 2020;13:151.
Raja SM, Guptill JT, Mack M, Peterson M, Byard S, Twieg R, et al. A phase 1 assessment of the safety, tolerability, pharmacokinetics and pharmacodynamics of (2R,6R)-hydroxynorketamine in healthy volunteers. Clin Pharmacol Ther. 2024;116:1314–24.
Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, et al. NMDAR inhibition-independent antidepressant actions of ketamine metabolites. Nature. 2016;533:481–6.
Grunebaum MF, Galfalvy HC, Choo TH, Parris MS, Burke AK, Suckow RF, et al. Ketamine metabolite pilot study in a suicidal depression trial. J Psychiatr Res. 2019;117:129–34.
Fava M, Freeman MP, Flynn M, Judge H, Hoeppner BB, Cusin C. et al. Double-blind, placebo-controlled, dose-ranging trial of intravenous ketamine as adjunctive therapy in treatment-resistant depression (TRD). MolPsychiatry. 2020;25:1592–603. https://doi.org/10.1038/s41380-018-0256-5.
Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978;133:429–35.
Bremner JD, Krystal JH, Putnam FW, Southwick SM, Marmar C, Charney DS, Mazure CM. Measurement of dissociative states with the Clinician-Administered Dissociative States Scale (CADSS). J Trauma Stress. 1998;11:125–36. https://doi.org/10.1023/A:1024465317902.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the analysis, interpretation, and editing of the manuscript. SS conducted the systematic review and drafted the manuscript, with MG supervising the entire process including both authors reading the included articles and agreeing on the synthesis and interpretation of results. JJM, MG, and SS reviewed and revised the manuscript. The authors have read and approved the manuscript and are accountable for the accuracy and integrity of the work.
Corresponding author
Ethics declarations
Competing interests
Dr Mann receives royalties for the commercial use of the C-SSRS from the Research Foundation for Mental Hygiene and from Columbia University for the Columbia Pathways App. The other authors report no conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Sajid, S., Mann, J.J. & Grunebaum, M.F. Clinical trials since 2020 of rapid anti-suicidal ideation effects of ketamine and its enantiomers: a systematic review. Transl Psychiatry 15, 44 (2025). https://doi.org/10.1038/s41398-025-03255-0
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03255-0