Abstract
Subthreshold depression (SD) is a prevalent condition among young adults, significantly increasing the risk of developing major depressive disorder (MDD). While the symptoms of MDD are well-documented, the network structure and key symptoms of SD, which forms a complex, interdependent system, have not been fully elucidated. This study sought to identify the central symptoms and their interconnections within the depressive symptom network in young adults with SD. A total of 834 Chinese young adults with SD completed the 21-item Beck Depression Inventory 2nd version (BDI-II) and were included in this study. Network analysis was employed to identify central symptoms (nodes) and associations between symptoms (edges) as assessed by the BDI-II. Additionally, centrality indicators for network robustness underwent assessment through stability and accuracy tests. The analysis revealed that Loss of interest was the most central node in the SD symptom network, with Tiredness/fatigue and Agitation following closely. Significant associations were observed between Loss of energy and Concentration difficulties, Agitation and Irritability, Guilty feelings and Self-dislike, as well as Tiredness and Loss of pleasure. The network demonstrated robustness across stability and accuracy assessments. Loss of interest, Tiredness/fatigue, and Agitation were pivotal symptoms within the depressive symptom network of SD in young adults. These symptoms may serve as critical targets for therapeutic interventions and should be prioritized in future psychological and neurobiological research to advance our understanding of SD.
Similar content being viewed by others
Introduction
Subthreshold depression (SD) is a psychological state characterized by depressive symptoms that fall short of meeting the criteria for major depressive disorder (MDD) as outlined in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) [1, 2]. Epidemiological evidence suggests that approximately 7.3–17.2% of population experiences SD [3]. Moreover, individuals grappling with SD, which is associated with functional impairment, face a 2.95 times greater risk of progressing to MDD compared to those without SD [2, 4, 5].
Research indicates variations in the severity of mental illness across different age groups, with young adulthood being particularly susceptible [6, 7]. Factors such as heavy workloads, competition, financial strains, and other stressors render this age group vulnerable [8,9,10]. Consequently, young adults exhibit a higher prevalence of psychiatric disorders, leading to notable functional impairment, financial burdens, and an elevated risk of suicidal ideation and attempts [11,12,13,14]. Such comprehending the underlying psychopathological mechanisms of SD could help to develop timely and efficacious interventions aimed at mitigating the risk of SD in young adults.
From a conventional causal perspective of psychopathology, psychiatric symptoms are perceived as outward expressions of an underlying cohesive disorder, similar to how an array of elements in psychometric investigation aligns with an implicit underlying dimension [15,16,17]. In this framework, symptoms are aggregated to portray the latent factor, albeit lacking in the illustration of the dynamic interactions among them [17]. Consequently, network modeling has emerged as a promising methodology for the representation and analysis of psychiatric constructs, thereby enhancing the comprehension of the heterogeneity within depressive syndrome [18,19,20]. According to network analysis theory, symptoms do not exist in isolation; rather, they intricately interact to establish and sustain a unified pathological condition [21, 22]. These interactions are distinctly delineated within the network, facilitating the identification of pivotal symptoms that significantly contribute to the onset of a syndrome. Hence, interventions targeting these central symptoms may yield greater efficacy [19].
Given the potential utility of network theory and analysis in advancing the understanding of symptoms central to the perpetuation of depression psychopathology [23], we aimed to characterize item-level depressive symptoms using network analysis among young adults experiencing SD, discerning which symptoms and inter-symptom associations exert the most pronounced influence within the SD symptom network. This study identified the core depressive symptoms in Chinese young adults with SD, offering a foundation and insights for future research and interventions targeting SD.
Materials and methods
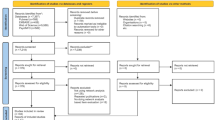
Subject and procedure
We conducted our study in Guangzhou, China, spanning from July 2021 to December 2023. A total of 834 patients diagnosed with SD were invited to participate. All participants met the inclusion criteria outlined as follows: Firstly, they exhibited 2–4 criterion symptoms of depression persisting for at least 2 weeks, with at least one of the core symptoms, namely, depressed mood or anhedonia, as assessed by experienced psychiatrists [24, 25]. Secondly, they obtained a BDI-II score of ≥ 14 [26]. Lastly, the individuals involved in this study were between the ages of 18 and 35. Patients will be excluded if they are receiving medications for depression. The study protocol received approval from the Ethics Committee of the Affiliated Brain Hospital of Guangzhou Medical University (approval numbers AF/SC-07/02.2).
Assessment of depressive symptoms
In our analysis of the symptom network of depression, we employed the BDI-II scale for evaluation. The BDI-II scale stands as one of the most widely used tools for assessing depressive symptoms globally, having been employed in over 7000 studies and encompassing the largest array of symptoms among six other common depression scales [27, 28]. Comprising 21 items, the BDI-II assesses symptoms in alignment with the criteria for depressive disorders outlined in the International Classification of Diseases and DSM-V. Patients were tasked with selecting the sentences that best reflected their feelings over the preceding two weeks. Each item was rated on a 4-point scale (0–3), with higher scores indicating more severe symptoms [29]. The value of Cronbach’s alpha reported in Titov et al.’s research was 0.87 [30], while in our study, it yielded a Cronbach’s alpha of 0.83.
Data collection
The researchers first clarified the objectives, methodology, relevance, and questionnaire of the investigation to the subjects. Following this, clinical psychologists evaluated depressive symptoms among patients from the Outpatient Department of the Affiliated Brain Hospital of Guangzhou Medical University. Subsequently, potential participants were invited to complete the BDI-II scales. Informed consent was obtained from all individuals before their inclusion in the study.
Analysis
Network estimation
We employed the Gaussian graphical model to construct the psychological network of depressive symptoms [21, 31]. To establish a conservative network model, we utilized the ‘least absolute shrinkage and selection operator’ (LASSO) approach, coupled with a tuning parameter to optimize the extended Bayesian information criterion [21]. This method involves identifying neighborhoods among the nodes and then attenuating inconsequential edge coefficients to zero. In the resulting psychological network, each node corresponds to one of the 21 items from the BDI-II, with the inter-node edges representing the relationships between respective item pairs. The thickness of these edges indicates the strength of these associations. To assess the accuracy of edge weights, we employed a non-parametric bootstrapping technique, conducting 2500 iterations with 95% confidence intervals. This approach allowed us to evaluate the significance of variations among edge weights. In the network analysis, each variable was represented as a node, and each binary association between variables was depicted as an edge, with the thickness of these edges reflecting the strength of the correlation. Positive correlations were depicted by green edges, while red edges indicated negative correlations.
Identification of central symptoms
To delineate the central symptoms within the network of depressive symptoms of SD, we performed calculations for three major centrality indices: Strength, Closeness, and Betweenness [32, 33]. Strength is determined by the total of the absolute edge weights connecting a specific node to all other nodes in the network. Closeness is denoted by the reciprocal of the sum of the lengths of the shortest paths originating from a given node to every other node. Betweenness is computed as the number of shortest paths passing through a particular node between any two nodes in the network [31]. These analyses were performed using the “networktool” and “qgraph” packages within the R statistical environment (version 3.5.3).
Network stability and accuracy
We computed the correlation stability coefficient (CS-coefficient) to validate the stability of the centrality estimates. The CS-coefficient signifies the maximum percentage of cases that can be excluded without diminishing the probability of achieving a 95% confidence level in the ranking correlation between the full network and a randomly subsampled network, reaching a substantial effect size (≥ 0.7) [31, 34]. Hence, it is advisable to interpret centrality indices only when their CS-coefficients exceed 0.25, with a preference for those surpassing 0.5 [31]. To identify significant differences between pairs of centrality indices, we employed 95% non-parametric bootstrap confidence intervals (comprising 1000 bootstrap replications) to estimate the disparities.
Comparison of network characteristics by gender
In line with previous studies, we investigated gender differences in network characteristics using the Network Comparison Test (NCT) - a permutation-based method developed to assess differences between two separate networks, such as those of male and female participants [35, 36]. We began by comparing the distribution of edge weights within each gender-specific network to understand their structural properties. After applying the Holm-Bonferroni correction to account for multiple comparisons, we examined the differences in edge strength between the male and female networks.
Results
Baseline characteristics of the study subjects
This research included a total of 834 participants, comprising 639 women and 195 men. The mean age of the patients was 22.68 years (SD: 3.67 years). Table 1 presents the clinical characteristics of the participants. Table 2 displays the detailed mean and SD of depressive symptoms measured by the BDI-II. According to the BDI-II, the mean (SD) of the BDI-II total score was 25.15 (8.80). The item “Loss of energy” had the highest mean score, while symptoms of “Suicidal thoughts or wishes” had the lowest mean score.
Depressive symptoms network of SD young adults
In order to identify the central symptoms network of SD young adults, we performed the depressive symptoms network estimation, centrality stability test, and strength comparison.
Network structure estimation
We explored the network structure of depressive symptoms in young adults with SD by constructing a regularized network encompassing all 21 depressive symptoms, resulting in 210 possible edges (21*(21–1)/2). Among them, 143 (68%) of the 210 edges were estimated to be above zero. Figure 1 illustrated several nodes highly connected within the network, including “Loss of interest” (BDI.12), “Self-criticalness” (BDI. 8), “Tiredness/fatigue” (BDI. 20), and “Guilty feeling” (BDI. 5). Furthermore, strong positive correlations were observed between the following symptom pairs: “Loss of energy” and “Concentration difficulty,” “Agitation” and “Irritability,” “Guilty feeling” and “Self-dislike,” and “Tiredness/fatigue” and “Loss of pleasure.” We utilized a weighted adjacency matrix to examine the numerical interactions among these symptoms (Supplementary Fig. 1).
Network centrality estimation
To evaluate network centrality and identify the most influential node in the network, we measured centrality indices, encompassing strength, closeness, and betweenness. As shown in Fig. 2 and Supplementary Table 1, “Loss of interest” (BDI.12) emerged as the most central node, with a strength value of 2.09, a closeness value of 2.27, and a betweenness value of 2.74, indicating its pivotal role in the depressive symptom network of young adults with SD. Additionally, “Tiredness/fatigue” (BDI.20) showed significant network centrality, with a strength of 1.56, closeness of 1.61, and betweenness of 2.41. Similarly, “Agitation” (BDI.11) also displayed considerable centrality, scoring a strength of 1.31, closeness of 1.36, and a betweenness of 1.77. The three central symptoms “Loss of interest,” “Tiredness,” and “Agitation” exhibited positive correlations within the network, with “Loss of interest” correlating with “Tiredness” (weight of 0.12), “Loss of interest” with “Agitation” (weight of 0.06), and “Tiredness” with “Agitation” (weight of 0.15). Furthermore, “Loss of energy” (BDI.15) had notable centrality measures, including strength (0.99), closeness (0.72), and betweenness (−0.49). “Worthlessness” (BDI.14) and “Past failure” (BDI.3) displayed relatively high betweenness centrality, indicating their significant roles within the network despite lower strength and closeness values.
Stability and accuracy of the network
To further test the network accuracy and stability, edge-weight bootstrapping and CS-coefficient were calculated. The results of edge-weight bootstrapping indicated moderate accuracy, as depicted in Supplementary Fig. 2. The gray area in the figure represents the 95% confidence interval of the edge weight obtained through the bootstrap method. Furthermore, Fig. 3 illustrates that even with significant sample reductions, the values of strength, betweenness, and closeness remained consistent using the case-dropping subset bootstrap approach. Although betweenness exhibited slightly lower stability (CS-C = 0.205) compared to the primary index, closeness demonstrated better stability. Conversely, the strength index proved robust and trustworthy (CS-C = 0.361). In other words, even after dropping up to 36.1% of the sample, the order of symptoms in terms of strength remained correlated with the original order (r = 0.7), indicating relative stability suitable for explaining symptom importance. Thus, our focus shifted to interpreting symptom strength based on this network analysis. Regarding strength, BDI.20 (Tiredness/fatigue), BDI.12 (Loss of interest), and BDI.15 (Loss of energy) emerged as statistically stronger compared to other symptoms, as illustrated in Fig. 4. Additionally, bootstrapped difference tests indicated a significant proportion of comparisons among edge weights were statistically significant (Supplementary Fig. 3).
The x-axis denotes the percentage of cases from the original sample employed at each stage. The y-axis signifies the mean correlation between the centrality metrics from the initial network and those from the re-estimated networks following the exclusion of increments of case percentages. Each line represents the intercorrelations among betweenness, closeness, and strength centralities.
Network comparisons between gender
We conducted a comparative analysis of the network models between males and females (Fig. 5). There were no significant differences observed in the global network strength (network strength among male participants: 8.95 versus female participants: 8.15, p = 0.712) or in edge weights (p = 0.316). Similarly, there were no gender differences in the mean levels of certain individual symptoms, as detailed in Supplementary Table 2.
Discussion
Our study identifies “Loss of interest,” “Tiredness/fatigue,” and “Agitation” as central symptoms in young adults with SD, which aligns partially with findings from previous research. A study in Hong Kong, which included a sample of 11,072 participants, found that “Guilt,” “Sad Mood,” and “Energy” symptoms were the most central nodes in the depressive symptom network among adult community members during the COVID-19 pandemic [23]. This differs from our findings, which may be attributed to their use of the Patient Health Questionnaire-9 as the assessment tool and the broader age range (18–59 years) of their sample compared to ours. Nevertheless, the analysis of gender differences in network outcomes showed no significant difference in the global network strength between males and females, a result that is consistent with our findings. Additionally, a psychiatric study from South Korea (n = 223) identified “loss of interest” as the most central node in the depressive symptom network among individuals with MDD, with “Pessimism” and “Past failure” showing a strong connection [37], which is in line with our study’s outcomes. In contrast to our findings, the National Comorbidity Survey-Adolescent Supplement indicated that Poor self-esteem and Suicidal symptoms were central in the symptom network for MDD in the United States of America [38].
It is worth noting that we found that loss of interest, identified as a manifestation of anhedonia [1], held the highest centrality within the depression network. This observation resonates with the diagnostic criteria for SD outlined in the DSM-5, which requires the presence of two to four criterion symptoms of depression, including at least one of the core symptoms (depressed mood or anhedonia) [24, 25]. Similarly, findings from the Sequenced Treatment Alternatives to Relieve Depression study, involving 3463 depressed outpatients, revealed that loss of interest was more central than sadness in a network analysis of the 15-item Inventory of Depressive Symptomatology, Clinician Rating [39]. Furthermore, anhedonia severity was robustly correlated with the emergence of suicidal ideation [40]. It was suggests the RDoC Positive Valence Systems constructs were instrumental in examining a broad spectrum of dimensions and characteristics that correlate with anhedonia, thereby highlighting the involvement of multiple neurotransmitter systems, including dopaminergic and glutamate pathways [41, 42]. The concept of anhedonia has evolved, expanding from a simple reduction in pleasure or interest to encompass a wider range of disturbances in reward processing [43]. Consequently, the prevalence of “loss of interest” in young adults with SD may be related to alterations in the reward circuitry [44]. Neuroimaging studies have shown decreased activation in the reward circuitry, particularly in the nucleus accumbens (NAc) and anterior cingulate cortex (ACC) [45], in individuals with depression. Furthermore, deep brain stimulation targeting either the NAc or ACC has shown potential in mitigating anhedonia in treatment-resistant depression [46, 47]. Therefore, it is imperative to prioritize the assessment and treatment of loss of interest in young adults with SD.
In the network of SD among young adults, fatigue emerged as the second most central depressive symptom, showing a positive correlation with alterations in sleep patterns. This observation resonates with existing evidence in the Asian demographic, indicating a tendency for individuals to express distress through physical symptoms, such as fatigue and insomnia [48]. Similarly, fatigue is widely acknowledged as one of the most prevalent symptoms of MDD and is often linked to sleep disturbances in young patients with depression [49]. Moreover, it is noteworthy that fatigue has been identified as a predictor of depression and is associated with poorer functional outcomes, including absenteeism, work productivity, and social functioning [50,51,52]. Additionally, individuals experiencing subjective fatigue and disturbed sleep exhibit elevated levels of C-reactive protein and Interleukin 6, markers also found to be increased in patients with depression [53,54,55]. Thus, it is plausible that the immune system plays a role in the perception of objective fatigue and sleep disturbances in SD young adults.
In this study, agitation also displayed high centrality within the SD symptom network and was strongly correlated with irritability, a known specific predictor of depression [56]. An online survey found that patients with mania and depressive symptoms self-reported the combination of “irritability or agitation” more frequently compared to those without depressive symptoms [57]. While the precise mechanisms underlying the convergent association between irritability and depressive symptoms remain to be fully elucidated [56], there is a consensus that common risk factors contribute to this relationship, including genetic predisposition, a family history of depression, early temperamental and personality attributes, and parenting approaches [58, 59]. Therefore, further comprehensive inquiries are warranted to delve deeper into the interplay between these aspects.
The present study has several limitations. Firstly, the cross-sectional nature of the data used to construct the network structure of depression-related somatic symptoms among patients limits the ability to depict symptom development over time or establish causal relationships between symptoms. Future studies should employ longitudinal follow-up to explore the temporal causal relationship between symptoms. Secondly, the sample size of this study was relatively small, underscoring the need to examine the network structure of depressive symptoms in SD young adults using larger samples in future investigations. Thirdly, the network structure in this study pertains specifically to young adults with SD in Guangzhou, China. As social and cultural backgrounds may influence the symptom network, the generalizability of the study’s findings to the national population of SD patients is limited. Lastly, the study relied solely on the BDI-II to measure self-reported symptoms over the past two weeks; future research should employ additional scales for a more comprehensive assessment of SD depressive symptoms.
In summary, this network analysis revealed that Loss of interest is the most central symptom of SD, followed by Tiredness/fatigue and Agitation. This research represents the first endeavor to delineate the depressive symptom network in young adults with SD, offering fresh insights for a better understanding of the depressive symptoms associated with SD and underscoring the necessity for targeted prevention and intervention programs for SD young adults.
References
Diagnostic and statistical manual of mental disorders. DSM-5TM. 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc.; 2013. https://doi.org/10.1176/appi.books.9780890425596.
Cuijpers P, Smit F. Subthreshold depression as a risk indicator for major depressive disorder: a systematic review of prospective studies. Acta Psychiatr Scand. 2004;109:325–31. https://doi.org/10.1111/j.1600-0447.2004.00301.x
Rodríguez MR, Nuevo R, Chatterji S, Ayuso-Mateos JL. Definitions and factors associated with subthreshold depressive conditions: a systematic review. BMC Psychiatry. 2012;12:181 https://doi.org/10.1186/1471-244X-12-181
Naber D, Bullinger M. Should antidepressants be used in minor depression? Dialogues Clin Neurosci. 2018;20:223–8.
Zhang R, Peng X, Song X, Long J, Wang C, Zhang C, et al. The prevalence and risk of developing major depression among individuals with subthreshold depression in the general population. Psychol Med. 2023;53:3611–20. https://doi.org/10.1017/S0033291722000241
Höglund P, Hakelind C, Nordin S. Severity and prevalence of various types of mental ill-health in a general adult population: age and sex differences. BMC Psychiatry. 2020;20:209 https://doi.org/10.1186/s12888-020-02557-5
Askari MS, Mauro PM, Kaur N, Keyes KM. Age, period, and cohort trends in perceived mental health treatment need and differences by mental health severity in the United States, 2008–2019. Community Ment Health J. 2023;59:631–40. https://doi.org/10.1007/s10597-022-01044-3
Lew B, Huen J, Yu P, Yuan L, Wang D-F, Ping F, et al. Associations between depression, anxiety, stress, hopelessness, subjective well-being, coping styles and suicide in Chinese university students. PLoS ONE. 2019;14:e0217372 https://doi.org/10.1371/journal.pone.0217372
Fernández-Rodríguez C, Soto-López T, Cuesta M. Needs and demands for psychological care in university students. Psicothema. 2019;31:414–21. https://doi.org/10.7334/psicothema2019.78
Sarabia-Cobo C, Alconero-Camarero AR, González-Gómez S, Catalán-Piris MJ, Del Amo Setien F, González-López JR. The Spanish version of the stressors in nursing students scale. J Psychiatr Ment Health Nurs. 2020;27:362–7. https://doi.org/10.1111/jpm.12590
Kwong ASF, López-López JA, Hammerton G, Manley D, Timpson NJ, Leckie G, et al. Genetic and environmental risk factors associated with trajectories of depression symptoms from adolescence to young adulthood. JAMA Netw Open. 2019;2:e196587 https://doi.org/10.1001/jamanetworkopen.2019.6587
Janaway BM, Kripalani M. Early intervention for depression in young people: a blind spot in mental health care. Lancet Psychiatry. 2019;6:283 https://doi.org/10.1016/S2215-0366(19)30089-6
Balázs J, Miklósi M, Keresztény A, Hoven CW, Carli V, Wasserman C, et al. Adolescent subthreshold-depression and anxiety: psychopathology, functional impairment and increased suicide risk. J Child Psychol Psychiatry. 2013;54:670–7. https://doi.org/10.1111/jcpp.12016
Mental Illness - National Institute of Mental Health (NIMH) n.d. https://www.nimh.nih.gov/health/statistics/mental-illness.
Fried EI, Nesse RM. Depression sum-scores don’t add up: why analyzing specific depression symptoms is essential. BMC Med. 2015;13:72 https://doi.org/10.1186/s12916-015-0325-4
Gijzen MWM, Rasing SPA, Creemers DHM, Smit F, Engels RCME, De Beurs D. Suicide ideation as a symptom of adolescent depression. a network analysis. J Affect Disord. 2021;278:68–77. https://doi.org/10.1016/j.jad.2020.09.029
Schmittmann VD, Cramer AOJ, Waldorp LJ, Epskamp S, Kievit RA, Borsboom D. Deconstructing the construct: a network perspective on psychological phenomena. New Ideas in Psychology. 2013;31:43–53. https://doi.org/10.1016/j.newideapsych.2011.02.007
Cramer AOJ, Waldorp LJ, van der Maas HLJ, Borsboom D. Comorbidity: a network perspective. Behav Brain Sci. 2010;33:137–50. https://doi.org/10.1017/S0140525X09991567. discussion 150-193
Borsboom D, Cramer AOJ. Network analysis: an integrative approach to the structure of psychopathology. Annu Rev Clin Psychol. 2013;9:91–121. https://doi.org/10.1146/annurev-clinpsy-050212-185608
Saxe GN. Network psychiatry: computational methods to understand the complexity of psychiatric disorders. J Am Acad Child Adolesc Psychiatry. 2017;56:639–41. https://doi.org/10.1016/j.jaac.2017.06.001
Epskamp S, Fried EI. A tutorial on regularized partial correlation networks. Psychol Methods. 2018;23:617–34. https://doi.org/10.1037/met0000167
Costantini G, Perugini M. A framework for testing causality in personality research. Eur J Pers. 2018;32:254–68. https://doi.org/10.1002/per.2150
Cheung T, Jin Y, Lam S, Su Z, Hall BJ, Xiang Y-T, et al. Network analysis of depressive symptoms in Hong Kong residents during the COVID-19 pandemic. Transl Psychiatry. 2021;11:460 https://doi.org/10.1038/s41398-021-01543-z
Kroenke K. When and how to treat subthreshold depression. JAMA. 2017;317:702–4. https://doi.org/10.1001/jama.2017.0233
Tolentino JC, Schmidt SL. DSM-5 criteria and depression severity: implications for clinical practice. Front Psychiatry. 2018;9:450 https://doi.org/10.3389/fpsyt.2018.00450
Takagaki K, Okamoto Y, Jinnin R, Mori A, Nishiyama Y, Yamamura T, et al. Behavioral characteristics of subthreshold depression. J Affect Disord. 2014;168:472–5. https://doi.org/10.1016/j.jad.2014.07.018
Fried EI. The 52 symptoms of major depression: lack of content overlap among seven common depression scales. J Affect Disord. 2017;208:191–7. https://doi.org/10.1016/j.jad.2016.10.019
Wang Y-P, Gorenstein C. Psychometric properties of the beck depression Inventory-II: a comprehensive review. Braz J Psychiatry. 2013;35:416–31. https://doi.org/10.1590/1516-4446-2012-1048
Keller F, Kirschbaum-Lesch I, Straub J. Factor structure and measurement invariance across gender of the beck depression Inventory-II in adolescent psychiatric patients. Front Psychiatry. 2020;11:527559 https://doi.org/10.3389/fpsyt.2020.527559
Titov N, Dear BF, McMillan D, Anderson T, Zou J, Sunderland M. Psychometric comparison of the PHQ-9 and BDI-II for measuring response during treatment of depression. Cogn Behav Ther. 2011;40:126–36. https://doi.org/10.1080/16506073.2010.550059
Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behav Res Methods. 2018;50:195–212. https://doi.org/10.3758/s13428-017-0862-1
Valente TW. Network interventions. Science. 2012;337:49–53. https://doi.org/10.1126/science.1217330
Opsahl T, Agneessens F, Skvoretz J. Node centrality in weighted networks: generalizing degree and shortest paths. Soc Networks. 2010;32:245–51. https://doi.org/10.1016/j.socnet.2010.03.006
Costenbader E, Valente TW. The stability of centrality measures when networks are sampled. Soc Networks. 2003;25:283–307. https://doi.org/10.1016/S0378-8733(03)00012-1
Mullarkey MC, Marchetti I, Beevers CG. Using network analysis to identify central symptoms of adolescent depression. J Clin Child Adolesc Psychol. 2019;48:656–68. https://doi.org/10.1080/15374416.2018.1437735
van Borkulo C, Boschloo L, Borsboom D, Penninx BWJH, Waldorp LJ, Schoevers RA. Association of symptom network structure with the course of [corrected] depression. JAMA Psychiatry. 2015;72:1219–26. https://doi.org/10.1001/jamapsychiatry.2015.2079
Park S-C, Kim D. The centrality of depression and anxiety symptoms in major depressive disorder determined using a network analysis. J Affect Disord. 2020;271:19–26. https://doi.org/10.1016/j.jad.2020.03.078
de la Torre-Luque A, Essau CA. Symptom network connectivity in adolescents with comorbid major depressive disorder and social phobia. J Affect Disord. 2019;255:60–8. https://doi.org/10.1016/j.jad.2019.05.015
Fried EI, Epskamp S, Nesse RM, Tuerlinckx F, Borsboom D. What are “good” depression symptoms? Comparing the centrality of DSM and non-DSM symptoms of depression in a network analysis. J Affect Disord. 2016;189:314–20. https://doi.org/10.1016/j.jad.2015.09.005
Ducasse D, Loas G, Dassa D, Gramaglia C, Zeppegno P, Guillaume S, et al. Anhedonia is associated with suicidal ideation independently of depression: a meta-analysis. Depress Anxiety. 2018;35:382–92. https://doi.org/10.1002/da.22709
Sj R, Da P, Ba S, Sh K. Assessing anhedonia in depression: potentials and pitfalls. Neurosci Biobehav Rev. 2016;65:21–35. https://doi.org/10.1016/j.neubiorev.2016.03.004
Der-Avakian A, Markou A. The neurobiology of anhedonia and other reward-related deficits. Trends Neurosci. 2012;35:68–77. https://doi.org/10.1016/j.tins.2011.11.005
Wang S, Leri F, Rizvi SJ. Anhedonia as a central factor in depression: Neural mechanisms revealed from preclinical to clinical evidence. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2021;110:110289 https://doi.org/10.1016/j.pnpbp.2021.110289
Fox ME, Lobo MK. The molecular and cellular mechanisms of depression: a focus on reward circuitry. Mol Psychiatry. 2019;24:1798–815. https://doi.org/10.1038/s41380-019-0415-3
Satterthwaite TD, Kable JW, Vandekar L, Katchmar N, Bassett DS, Baldassano CF, et al. Common and dissociable dysfunction of the reward system in bipolar and unipolar depression. Neuropsychopharmacology. 2015;40:2258–68. https://doi.org/10.1038/npp.2015.75
Schlaepfer TE, Cohen MX, Frick C, Kosel M, Brodesser D, Axmacher N, et al. Deep brain stimulation to reward circuitry alleviates anhedonia in refractory major depression. Neuropsychopharmacology. 2008;33:368–77. https://doi.org/10.1038/sj.npp.1301408
Bewernick BH, Hurlemann R, Matusch A, Kayser S, Grubert C, Hadrysiewicz B, et al. Nucleus accumbens deep brain stimulation decreases ratings of depression and anxiety in treatment-resistant depression. Biol Psychiatry. 2010;67:110–6. https://doi.org/10.1016/j.biopsych.2009.09.013
Chentsova-Dutton Y, Ryder AG, Yi J Understanding depression across cultural contexts. 2016.
Crouse JJ, Carpenter JS, Song YJC, Hockey SJ, Naismith SL, Grunstein RR, et al. Circadian rhythm sleep-wake disturbances and depression in young people: implications for prevention and early intervention. Lancet Psychiatry. 2021;8:813–23. https://doi.org/10.1016/S2215-0366(21)00034-1
Nierenberg AA, Husain MM, Trivedi MH, Fava M, Warden D, Wisniewski SR, et al. Residual symptoms after remission of major depressive disorder with citalopram and risk of relapse: a STAR*D report. Psychol Med. 2010;40:41–50. https://doi.org/10.1017/S0033291709006011
Robinson RL, Stephenson JJ, Dennehy EB, Grabner M, Faries D, Palli SR, et al. The importance of unresolved fatigue in depression: costs and comorbidities. Psychosomatics. 2015;56:274–85. https://doi.org/10.1016/j.psym.2014.08.003
Corfield EC, Martin NG, Nyholt DR. Co-occurrence and symptomatology of fatigue and depression. Compr Psychiatry. 2016;71:1–10. https://doi.org/10.1016/j.comppsych.2016.08.004
Osimo EF, Baxter LJ, Lewis G, Jones PB, Khandaker GM. Prevalence of low-grade inflammation in depression: a systematic review and meta-analysis of CRP levels. Psychol Med. 2019;49:1958–70. https://doi.org/10.1017/S0033291719001454
Irwin MR, Olmstead R, Carroll JE. Sleep disturbance, sleep duration, and inflammation: a systematic review and meta-analysis of cohort studies and experimental sleep deprivation. Biol Psychiatry. 2016;80:40–52. https://doi.org/10.1016/j.biopsych.2015.05.014
Dantzer R, Heijnen CJ, Kavelaars A, Laye S, Capuron L. The neuroimmune basis of fatigue. Trends Neurosci. 2014;37:39–46. https://doi.org/10.1016/j.tins.2013.10.003
Vidal-Ribas P, Brotman MA, Valdivieso I, Leibenluft E, Stringaris A. The status of irritability in psychiatry: a conceptual and quantitative review. J Am Acad Child Adolesc Psychiatry. 2016;55:556–70. https://doi.org/10.1016/j.jaac.2016.04.014
Vieta E, Grunze H, Azorin J-M, Fagiolini A. Phenomenology of manic episodes according to the presence or absence of depressive features as defined in DSM-5: results from the IMPACT self-reported online survey. J Affect Disord. 2014;156:206–13. https://doi.org/10.1016/j.jad.2013.12.031
Vidal-Ribas P. Editorial: the paradox of reward processing in the association between irritability and depression. J Am Acad Child Adolesc Psychiatry. 2023;62:853–5. https://doi.org/10.1016/j.jaac.2023.05.001
Vidal-Ribas P, Stringaris A. How and why are irritability and depression linked? Child Adolesc Psychiatr Clin N Am. 2021;30:401–14. https://doi.org/10.1016/j.chc.2020.10.009
Acknowledgements
We extend our heartfelt appreciation to all the participants and their families who generously contributed to this study. A special thank you goes to the Key Laboratory of Traditional Chinese Medicine Classical Theory, Ministry of Education, Shandong University of Traditional Chinese Medicine, Jinan 250355, PR China, for their invaluable support.
Funding
This research was funded by the National Key R&D Program of China (2022YFC3500405), the National Science Foundation of China (82374586, 82274128), the Shanghai Institute of Traditional Chinese Medicine for mental health (SZB2024101), and the Natural Science Foundation of Shandong Province (ZR2022QH083).
Author information
Authors and Affiliations
Contributions
YJC and XMJ conceived and designed the study. LY and JH managed the project. XMJ, XTW, SWW, LY, YYZ, MZ, YJZ, JLY acquired the data and participated in cohort recruitment. XMJ and XTW performed the analysis and interpretation. XMJ and YJC wrote the manuscript. All authors made contributions to the preparation of this manuscript and have given their approval for the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was granted ethical approval by the Affiliated Brain Hospital of Guangzhou Medical University (Approval No. AF/SC-07/02.2), and all methods were performed in accordance with relevant guidelines and regulations. Written informed consent was obtained from all enrolled participants after comprehensive explanation of the study objectives and procedures. Consent to reproduce images: not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiang, X., Wang, X., Yu, L. et al. Network analysis of central symptoms in Chinese young adults with subthreshold depression. Transl Psychiatry 15, 103 (2025). https://doi.org/10.1038/s41398-025-03307-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-025-03307-5