Abstract
Social determinants of health have been shown to have a greater impact on overall health than traditionally considered medical risk factors, especially in people with mental disorders. It is the primary responsibility of healthcare providers to ensure that persons with psychiatric disorders are actively helped in reducing the adverse effects of SDoMH on their health and healthcare. Yet, the current clinical psychiatric practice in the U.S. does not have any standardized guidelines for evaluating or addressing these critical factors even among individuals who are receiving psychiatric and other medical treatment. Although there are several barriers to implementing such interventions, there are also practical approaches to address selected social determinants of mental health and improve the well-being of our patients. In this article, we review the literature on the assessment of relevant social factors and pragmatic psychosocial strategies at the individual, family, and community levels to help reduce their adverse impact. We offer guidelines for psychiatric clinicians and case managers to improve the health and quality of life of persons with mental disorders, using sustained inter-professional collaborative efforts.
Similar content being viewed by others
Introduction
The World Health Organization (WHO) issued its first major report on social determinants of health (SDoH) in [1] and subsequently on social determinants of mental health (SDoMH) in [2]. Since then, the literature on this topic has grown considerably. It is now widely accepted that SDoMH have a major impact on the health of people with mental disorders, including serious mental illnesses (SMI) such as schizophrenia, major depressive disorder, and bipolar disorder [3]. SDoMH of particular relevance to persons with mental disorders include childhood abuse and neglect, trauma, violence, discrimination due to stigma, social isolation, unemployment, food insecurity, housing instability, and incarceration [4].
One challenge in addressing SDoMH is that the number of potential social determinants is so large that it dampens the enthusiasm of interested constituents [5], including policy makers, health care systems, individual clinicians, researchers, educators, and administrators. According to Lundberg [6], despite its importance, this ubiquity of SDoH has made it difficult to communicate the SDoH framework to stakeholders in other sectors, and consequently, we do not yet see much change in the healthcare system. In the area of mental health, we believe that a two-pronged approach is needed: (a) development and implementation of pragmatic strategies to assess and manage relevant SDoMH in individuals with mental disorders who are being treated; and (b) continued collective engagement by clinicians and their respective professional organizations in social-justice initiatives aimed at reducing SDoMH at the community and societal level. The goal of the present article is related to the first prong – i.e., strategies to address SDoMH among individuals with mental disorders, with a primary focus on patients and their families.
MAJOR SDoMH for people with mental disorders
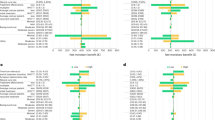
Two comprehensive reviews of meta-analyses and systematic reviews of the association of specific SDoMH with the risk and severity of schizophrenia-spectrum psychotic disorders [7, 8] and of major depressive disorder [9] found moderate-to-large effect sizes for childhood abuse/neglect and food insecurity. Associations with small-to-medium effect sizes were seen for perceived/experienced racial/ethnic discrimination and immigrant status in schizophrenia-spectrum psychotic disorders, and for childhood domestic violence, natural disasters, and terrorist acts in major depressive disorder. Studies that examined the point prevalence of schizophrenia-spectrum psychotic disorders reported markedly elevated rates in incarcerated persons, homeless persons, and in areas with the highest levels of social fragmentation (i.e., neighborhood level of instability in social relationships). Similar studies of major depressive disorder reported elevated prevalence rates in migrants, incarcerated individuals, and homeless persons. In contrast, parental care was associated with a lower prevalence of major depressive disorder.
While several SDoMH are specified above, there are others that are relevant to mental disorders that have not been studied comprehensively enough to be included in our above-mentioned reviews. These include stigma against mental disorders; specific group discriminations such as racism, ageism, sexism, or bias against LGBTQ+ individuals; lack of social connections; use of social media; and disrupted marital status, to name a few. A major methodological limitation of published SDoMH studies is that most are based on simple observational designs and are cross-sectional and therefore, do not show inter-temporal associations and causality. Nonetheless, the reviews clearly show that a number of adverse SDoMH have meaningful associations with mental disorders, and therefore, interventions to successfully address these adversities are needed to help reduce the risk, severity, and/or persistence of psychiatric illnesses. The association of SDoMH with mental disorders is most likely bidirectional [10].
There are currently no formal assessment or treatment guidelines for psychiatric clinicians to address SDoMH in individual patients. Government policies and social structures and systems influence SDoMH such as poverty, food insecurity, housing instability, as well as racism and other forms of discrimination. Addressing these at the societal level would require collective action beyond the control of single individuals. Furthermore, there are complex interactions among the various SDoMH that influence health outcomes. We agree with Gómez et al. [11] that no single individual, organization, community, or sector has sole ownership, accountability, or capacity to maintain or change the health and well-being of an entire population. Among high-priority objectives, healthcare systems need to partner with sectors that manage education, transportation, housing, and other social services. Several such strategies are possible (and many are being tried), such as setting up screening initiatives in schools; locating mental health services in various social-sector settings such as prisons; reimbursing transportation costs to mental health services; developing vocational and other supportive housing programs; and implementing voucher programs for relocation to more stable housing [4, 11].
Beyond these community- and societal-level initiatives, though, it is the primary responsibility of healthcare providers to ensure that persons with mental disorders are actively helped in reducing the adverse effects of SDoMH on their health and healthcare. In this article, we propose several SDoMH-focused strategies that are pragmatic, meaningful, and potentially implementable by clinicians working with individuals having mental disorders who are receiving treatment. These recommended initiatives are far from perfect; however, it is important to prioritize strategies that are within the reach of psychiatric clinicians in their own practices and local health care systems [12], and are practical and cost-effective for the overall healthcare system. Helpful intermediary professionals such as community social workers are critical, yet they are often not reimbursed or financially supported by the healthcare system [13]. Indeed, addressing social determinants of mental health should include involvement of social workers and social agencies that can help modify specific SDoMH or aid in enabling persons with mental disorders to participate in appropriate interventions, such as psychotherapies administered by psychiatrists, psychologists, or well-trained counselors. Peer professionals including nurses and well-trained volunteers can also play an important role.
Barriers to addressing SDoMH in persons with psychiatric disorders
The current mental healthcare system in the U.S. includes several obstacles to properly assessing and managing SDoMH in persons with mental disorders.
Focus on diagnosis
In recent decades, the U.S. healthcare reimbursement system has placed a growing emphasis on linking diagnosis to treatment. Yet psychosocial factors that cut across multiple diagnoses are of considerable importance in treatment outcomes but are not usually included in diagnostic criteria for mental disorders or formally assessed in electronic health record (EHR) systems.
Weak linkage with social services
A close link between healthcare providers and appropriate social resources is critical. However, the US healthcare system does not reimburse most non-medical social services and the availability and capacity of community-based organizations in rural areas may be limited [14]. Furthermore, persons with mental disorders, especially the marginalized groups, often have limited trust in the health care system, usually because of their past negative experiences with it [15]. Empathy, compassion, and awareness of the person’s social reality are needed on the part of the healthcare providers to earn the trust of individual service users and their families, and to improve their relationship with social and healthcare systems. Front-line social case workers or peer providers familiar with community resources should be connected with individuals with mental illnesses as patients would benefit from having a trusted human catalyst to facilitate initial contact and experiences that would lead to relationship-based services.
Lack of training in SDoH
A survey of consortium schools sponsored by American Medical Association showed that most programs do not routinely prioritize SDoH education on par with basic and clinical sciences [16]. The authors recommended increasing the priority level of SDoH training and employing better teaching strategies. For specific SDoMH like social isolation and loneliness, educating the public and medical community about the importance of assessing and promoting social connectedness is critical [17].
Healthcare finances
The current US healthcare system does not reimburse social assessments, interventions, or associated costs (e.g., childcare while a parent attends healthcare visits) that are seen as not directly associated with medical problems. Healthcare systems located in rural communities face additional financial and resource barriers to addressing SDoH such as workforce, transportation, internet, and housing shortages [14]. Furthermore, financial hardships contribute to chronicity of mental disorders. Interventions designed to reduce the shame and hopelessness of financial hardship can play an important role in recovery [18]. Few SDoMH-addressing intervention studies have demonstrated or even focused on cost-effectiveness, in part because of difficulties in estimating total costs in investigations with a potential long-term goal of primary prevention. Also, the streams of funding vary widely across the nation and benefits are diverse as well as distributed over time. These features make it difficult either to calculate benefit/cost ratios or to determine how to allocate costs sensibly across the different systems affected by the interventions.
Research funding
On the policy side of research funding, a balance is needed between etiology-focused biological investigations and psychosocial prevention and treatment strategies that seek to reduce the social burdens that individuals with mental disorders and their families face every day [19].
Pragmatic assessments of selected SDoMH
It is neither feasible nor necessary for a practicing psychiatric clinician to assess all the SDoMH reportedly associated with health outcomes in individuals with mental disorders. A healthcare system should start by identifying the SDoMH that apply widely in the community/ies it serves. Next, a community task force should determine which interventions to address those SDoMH are feasible locally or regionally. Finally, when assessing an individual patient, the clinician should determine which specific SDoMH are potentially modifiable and are of particular concern to a patient based on their and their family’s input. The process to make that determination should be standardized and structured. We should also add that unmodifiable SDoMH such as climate change or exposure to air pollutants are not easily addressable by most clinicians. However, therapy to cope with the resultant subjective stress can be useful, and in some cases those specific stresses can be reduced. There are examples of non-profit corporations like Citizens Energy Corporation that provide free home heating oil for older adults and for poor people living in Massachusetts and other cold weather states.
Questionnaire on unmet daily needs
In many mental healthcare settings in the U.S., few SDoMH are checked as part of medical visits. However, several organizations have recently developed brief screening tools – e.g., a 15-item Social Needs Screening Tool developed by the American Academy of Family Physicians [20] with simple questions that assess housing, food, transportation, utilities, etc. Another example is a measure proposed by Buitron de la Vega et al. [21]. The Centers for Medicare and Medicaid Services’ Health-Related Social Needs Screening Tool has 26 items, but one can use the first 16 items to assess living situation, food, transportation, utilities, and related SDoMH [22]. In some primary care and mental healthcare settings, an SDoMH form is completed by a social worker or by the patient online.
The Joint Commission [23] has stressed the importance of assessing Health-Related Social Needs, which include individual-level non-medical factors (e.g., childhood abuse, social connections) as well as conditions in the environments in which people live (e.g., neighborhood, access to education) that are critical for designing practical, patient-centered care plans. There has been growing empirical research associating these factors with worse outcomes in people with psychiatric disorders. The assessment of wider forces and systems (e.g., socioeconomic policies, climate change) at the individual level needs more research.
For outpatients, such information can be collected by a case manager interviewing a patient in person or by phone. The case manager could then work with appropriate community agencies to find ways to meet the patient’s needs in a practical and affordable manner. Effective person-centered care programs can orient the care to the individual’s life goals and shape a collaborative effort by the provider and the service user to attain those goals [24].
Assessment of selected SDoMH
The SDoMH questionnaires administered by a case manager should be made available to the treating clinician. The latter should then discuss with the patient (and any patient companions) which SDoMH are most relevant to the purpose of the healthcare visit and need to be assessed. Both community-level information and self-reported ratings may be relevant. At the community level, it is currently technically possible, but typically not implemented, to link the person’s address on the EHR to neighborhood-level indicators of SDoMH such as poverty, crime, or minoritized ethno-racial background. Validated self-report scales for several of these factors can be valuable from a therapeutic perspective [25]. For example, people with a similar level of housing instability may give themselves different ratings of their “experienced homelessness.” Similarly, loneliness is subjective distress due to “perceived isolation” and may differ in severity among groups with comparable levels of objective social isolation. Likewise, different individuals in the same community may have varied degrees of “perceived or experienced racism.” A systematic review of self-stigma in persons with SMI showed that perceived and experienced stigma predicted self-stigma, which was associated with increased transition to psychosis and poor clinical and functional outcomes [26]. The most commonly employed measure of self-stigma is the Internalized Stigma of Mental Illness Scale [27].
In studies of SDoMH, subjective assessment measures are important because it is the subjective distress or self-perceived or experienced discrimination that results in allostatic load. At the same time, self-report scales may result in an inherent selection bias, as the most motivated patients may be more likely to complete these scales. Having large sample sizes, using thoughtful strategies for engaging patients in completing assessments, and including objective (including digital) measures would help in getting a more complete picture and better understanding of SDoMH.
If a longer interview is feasible, a peer specialist could explore the level of person-centered experience of these SDoMH, employing instruments such as the Social Vulnerability Questionnaire to explore the personal impact of individual SDoMH [28]. Additionally, although the literature on SDoMH is mostly focused on adverse factors, positive SDoMH such as social support and parental care should also be evaluated. The suggested assessments can be completed either by the case manager in an in-person or phone interview, or by the patient online. The total time as well as the frequency of SDoMH assessment should vary depending on the situation. Several SDoMH are dynamic, and change over time – e.g., social connections or housing instability. Therefore, they need to be reassessed at appropriate intervals and incorporated into the treatment plans as needed. To formalize this process, major SDoMH should be included as specifiers in the next version of the Diagnostic and Statistical Manual [29] as well as in EHR systems.
SDoMH-focused interventions at individual level
Some SDoMH (e.g., social connections, food insecurity) are potentially more modifiable than others at the individual level, through psychosocial interventions. Although persons with mental disorders and their healthcare providers have limited control over less modifiable SDoMH (e.g., history of early-life trauma, stigma against mental illnesses), peer-led support services and psychotherapy can help individuals cope with these stressors to help mitigate distress and improve well-being, as well as potentially help reduce the risk of future trauma. Promoting a close linkage between persons with mental disorders and community resources would maximize the impact of interventions targeting SDoMH. Notably, although these interventions have been evaluated in a broad range of populations, the evidence base for their efficacy/effectiveness among persons with SMI is limited and clearly warrants more research.
Below, we summarize evidence on interventions that target specific SDoMH. Some promising approaches involve innovative methods that respond to the needs of patients beyond traditional hospital or clinic settings. They indicate the value of leading a multidisciplinary approach to best respond to intersectional needs and may prove to be scalable.
Overall unmet needs: social prescribing and case management
Social prescribing, a major “pillar of healthcare” in the U.K., seeks to integrate healthcare with services provided by link workers (nonclinical professionals with knowledge of local community resources) [30]. These workers support patients to assess and find ways of meeting their practical needs for health and well-being, such as transportation, food, internet, housing, or finances [31]. For example, finding convenient and affordable transportation to the clinic or to urgent care visits can reduce the risk of relapse and hospitalization and, in turn, healthcare costs. A systematic review documented positive effects of social prescribing on measures of depression/anxiety, loneliness, and quality of life; however, the scope for conclusions concerning their clinical relevance and sustainability is limited because of methodological shortcomings of the published studies [32]. A few U.S. healthcare systems have recently begun to adopt social prescribing programs to their consumers (e.g., https://socialprescribingusa.com/).
Social prescribing involves linking people to services and supports in the community and voluntary sectors to address their health-related needs. However, the approaches to social prescribing vary widely. A scoping review yielded 159 social prescribing programs from various countries [33]. Two countries with the largest numbers of programs were the UK and the USA, with 97 and 41 programs, respectively. Three-fourths of the programs pertained to the primary care context and 14% were for people with mental health issues. There was considerable variability in the contexts in which the programs were delivered, the target groups and services/supports to which participants were referred, the staff involved, program funding, and use of digital systems. Osler et al. [33] have described six areas related to the social prescribing process: identifying potential participants, referral to a link worker, screening for non-medical needs, referral to non-medical services and supports, providing additional health coaching/support, and follow-up.
Case management (CM), also referred to as care coordination or care management, is necessary for improving the management of complex physical and psychosocial problems. CM is a collaborative process of assessment, planning, facilitation, care coordination, evaluation, and advocacy for options and services to meet an individual’s and family’s comprehensive health needs. Systematic reviews of CM interventions for the care of chronic illnesses found that these interventions positively reduced health care utilization; however, results were mixed [34]. The challenges faced by CM include unclear scope of practice, diverse and complex CM activities, insufficient training, and inadequate reimbursement. Potential solutions include developing clear guidelines and professional standards, incorporating evidence-based practice and situational learning across settings and populations, and making systems improvement [35]. A qualitative study of case managers (CMs) suggested that barriers to successful CM include limited collaborations, excessive documentation requirements, and communication problems [36]. A larger qualitative study of CMs described three characteristics of successful programs: establishing trust, observing change in patients’ mindset or initiative, and promoting stability and independence [37].
Case (or Care) management programs use case managers (trained practitioners or navigators, often social workers) who evaluate, plan, implement, coordinate, and prioritize services based on an individual’s needs and offer support in close collaboration with health, social, and community partners. The Veterans Health Administration has been increasingly focusing on case management or coaching [38, 39] with the goal of promoting whole health, defined as physical, behavioral, spiritual, and socioeconomic well-being as defined by the individuals themselves [40]. A systematic review and meta-analysis of empirical studies in adults with mental disorders found that care management was associated with small but statistically significant improvements in psychiatric symptoms, mental and overall quality of life, and reduction in inpatient psychiatric hospital days [41].
There are several models of care management) that have been shown to be more effective than usual care in the treatment of late-life depression. For example, the Improving Mood–Promoting Access to Collaborative Treatment (IMPACT) collaborative care management program and the Prevention of Suicide in Primary Care Elderly: Collaborative Trial (PROSPECT) programs have been found to be significantly more effective than usual care for late-life depression [42, 43]. While care managers do not directly offer case management, they often connect their patients with social agencies available in their communities. There are different models of CM and it is important to pick the right model for the right situation in older adults with depression and other mental health conditions [44, 45].
The University of Pennsylvania’s person-centered care planning (PCCP) program seeks to promote integrated and recovery-oriented services based on an individual’s most-valued life goals [24]. The PCCP training uses a train-the-trainers model with supervisors as the primary target to prepare them to train their direct care teams. Providers learn how to elicit and empathize with clients’ subjective experiences and how to help clients identify and articulate their interests, preferences, and personal recovery goals in the service plan. A 12-month cluster-randomized controlled trial of PCCP training in community mental health clinics showed significant improvements in delivering person-centered care compared with the control group [24]. At 18 months, this effect was even more pronounced, representing a medium-to-large effect size (d = 0.71).
Social isolation and loneliness: psychological interventions
A systematic review and meta-analysis of psychological interventions to treat loneliness showed encouraging results, but the studies included in the analysis were of mixed quality, mostly in-person group-based interventions delivered weekly [46]. There was considerable heterogeneity in the effectiveness of the interventions. A meta-analysis of 28 studies (N = 3039) of cognitive behavioral therapy (CBT) found significantly reduced loneliness compared to control groups, yielding a small-to-medium effect size improvement (g = 0.43) [46].
Both cross-sectional and longitudinal investigations find an inverse association between wisdom, especially its compassion component, and loneliness [47]. A recent study employing a three-armed RCT targeted loneliness in 287 older adults in Hong Kong [48]. It found that a telephone-delivered wisdom-enhancement narrative therapy-based intervention significantly reduced loneliness at 4-week follow-up assessment.
The U.S. Department of Veterans Affairs has initiated a tele-support social prescription program called Compassionate Contact Corps, which connects isolated or lonely veterans with volunteers for regular conversation via phone calls [49]. Training of volunteers, some of whom are veterans themselves, includes promoting compassion, empathy, support, privacy, and confidentiality. The volunteer typically calls the veteran weekly for 15–60 min to provide socialization and companionship. This program is being implemented at over 80 VA facilities nationwide.
Previous trauma: trauma-focused psychotherapy (TFP)
Toxic stress, generated when challenges exceed perceived strength and resources, causes considerable pain and morbidity, especially for those already stressed under adverse SDoMH. Toxic stress is considered an SDoMH in many frameworks [4]. When it occurs during pregnancy, toxic stress not only affects the pregnant person but also increases the likelihood of mental disorders in the offspring [50]. During fetal development, especially during sensitive periods [51], trauma experiences shape vulnerability to psychopathology through the mechanism of experience-driven plasticity, predisposing the person especially to anxiety disorders and PTSD [52].
Psychotherapy aims to replace maladaptive beliefs and coping mechanisms with more adaptive strategies, such as replacing mistrust with trust and active accessing of resources which can help alleviate the negative effects of toxic stress and trauma. A major impediment to making psychotherapy available to those affected by adverse SDoMH is limited availability of competent therapists [53]. Solving this problem will involve addressing the excessive complexity of training, which limits accessibility to a few highly educated clinicians. Recent advances have made possible the dissemination of more-easily-accessible psychotherapy training to a broader range of healthcare professionals [54], especially in the area of trauma [55].
Trauma-Focused Psychotherapies (TFPs), notably cognitive processing, prolonged exposure, and eye-movement desensitization and reprocessing therapies are considered first-line treatments for posttraumatic stress disorder (PTSD) [56]. TFPs are moderately efficacious in improving interpersonal functioning [57]. Historically, intervention research has focused on PTSD following exposure to single traumatic events, limiting our understanding of how these treatments apply to individuals with a history of exposure to multiple traumatic events or multiple SDoMH over a lifetime [4]. Furthermore, management of current trauma differs from that of past trauma, including early-life events. Many people with PTSD are at heightened risk of future trauma exposure; hence, teaching people with PTSD to avoid future traumas can help address chronic PTSD.
Evidence-based TFP interventions are seldom practiced in routine care. Bragesjo et al. [58, 59] recently reported on the feasibility of treating severe and complex PTSD through a digital prolonged-exposure therapy intervention – viz., Huddinge Online Prolonged Exposure (HOPE) therapy. HOPE therapy was found to be feasible and delivered evidence-based treatment content in a psychiatric outpatient setting with reduced therapist time. The treatment was well-tolerated, with a rather low 17% discontinuation rate. Overall satisfaction was moderate, and significant reductions in PTSD symptoms were sustained at a 6-month follow-up visit.
Food (and Nutrition) insecurity: varied strategies
Compton [60] provides a comprehensive list of strategies focused on food (and nutrition) insecurity, a critical but clinically neglected SDoMH. He suggests that it is important for clinicians to understand and advocate for appropriate federal and state government policies related to food and nutrition, and to promote food banks and pantries, “food is medicine” initiatives, and programs offering better opportunities to afford and access whole foods and fresh produce. At the individual level, in the clinical setting, this can be achieved through screening, assessment, treatment, and follow-up.
Housing instability or homelessness: varied strategies
The rising prevalence of homelessness has become a growing humanitarian, policy, and public health issue, especially among individuals with mental disorders. Interventions that seek to keep individuals housed while also improving their health outcomes include street medicine, intensive case management, assertive community treatment, critical time intervention, supported employment programs, and permanent supportive housing [61, 62]. Evidence-based interventions exist but have not been adequately implemented or funded. Killaspy et al. [63] assessed the quality, costs, and effectiveness of mental health supported accommodation services in England, but did not find clear evidence on the most effective model(s) of mental health supported accommodation. Somers et al. [64] evaluated the effectiveness of Housing First against existing services over a 24-month period at locations not dedicated to Housing First participants only (termed scattered sites) and at sites where Housing First recipients predominated (congregate sites). Both types of sites were associated with greater housing stability than the control condition, and congregate sites were also associated with significantly greater community integration. Psychiatric clinicians can provide direct care and support for mental health issues using local services while also advocating for interdisciplinary evidence-based interventions, such as assertive community treatment and broader structural solutions.
Self-stigma: psychological interventions
Persons with mental disorders commonly experience self-stigma, leading to internalization of stereotypic or stigmatizing views held by other people. Self-stigma has been shown to have negative effects on self-esteem, self-efficacy and continuing adverse impact on psychological well-being [65]. A narrative review of published literature on interventions targeting self-stigma identified several approaches including healthy self-concept, self-stigma reduction, narrative enhancement and cognitive therapy, and anti-stigma photo-voice intervention [66]. The data appear to be limited.
Bannatyne et al. [67] noticed a growing body of literature showing that many medical students and doctors do not seek professional help for their mental health due to fear of stigma (both public- and self-stigma) and questioning of their clinical competency. A systematic review of mental health interventions to reduce self-stigma uncovered three studies of moderate quality that reported significant reductions in self-stigma in medical students following combined education and contact interventions [67].
Social discrimination due to racism and anti-LGBTQ bias: psychosocial interventions
Social discrimination due to marginalized status (e.g., racism) has been associated with worse severity of psychopathology [68]. In a systematic review, a majority of the 24 publications showed an association between perceived discrimination (racial, religious, sexual orientation, gender orientation, social class) and frequency and severity of psychotic symptoms [69]. Promising interventions to address discrimination among individual patients have been developed, but there are limited data on their efficacy, especially for individuals with mental disorders. Over 25 VA settings are implementing the Race-Based Stress and Trauma Empowerment approach [70], which involves 8 group sessions with Veterans of Color who have experienced distress due to racial discrimination. Modules span psychoeducation, skill development, and ethno-racial identity-based activities to foster healthy coping, empowerment, and self-advocacy.
Promoting Resilience in Discriminatory Environments is an eight-session group intervention that seeks to improve coping skills and ameliorate negative mental health outcomes and risky behaviors among gay and bisexual men that may result from internalized homonegativity or rejection due to sexual orientation [71]. Session content includes psychoeducation on emotion-focused and problem-focused coping, the development of appropriate goals, and relaxation techniques. In a pilot study of 33 participants, measures of self-esteem significantly increased between pre-test and 3-month follow-up while internalized homonegativity and loneliness significantly decreased. In another group-therapy approach, a 12-session CBT group for mood disorders was modified to include content on LGBT issues (coming out and internalized homophobia, biphobia, and transphobia) and how these experiences contribute to depression [72]. Between pre- and post-intervention, depressive symptoms significantly decreased while self-esteem increased.
Unemployment: psychosocial interventions
Individuals with mental disorders often encounter marked difficulties obtaining and/or retaining gainful employment; these difficulties can stem from their psychiatric disability and from stigmatization by potential employers, clinicians, and even family members. Supportive employment interventions can interrupt this negative cycle. Suijkerbuijk et al. [73] conducted a meta-analysis of 48 RCTs (n = 8743) evaluating employment interventions (pre-vocational training, transitional employment, supported employment, and supported employment augmented with additional interventions) for individuals with psychiatric disorders. Supportive employment, termed Individual Placement and Support (IPS), aims to find individuals employment quickly and to provide ongoing job maintenance assistance using specific principles including incorporation of client preferences in job searches, personalized benefits counseling, and integration of employment and mental health services. For studies with long-term follow-ups (n = 22), augmented supportive employment, supported employment, and pre-vocational training were significantly more effective than psychiatric care alone in obtaining competitive employment. In addition to positive employment outcomes, an RCT of IPS versus traditional vocational rehabilitation found that IPS participants demonstrated significantly higher scores on quality of life, empowerment, and work motivation metrics at an 18-month follow-up [74].
SDoMH-focused interventions at family and community levels
We have summarized above a number of individual -level strategies for addressing SDoMH in people with mental disorders that are currently available, and many more are expected to be developed and evaluated in the near future. More research is needed to strengthen their feasibility and evidence base regarding their impact on patients’ health and on the overall cost-benefit ratio, including the cost savings from primary, secondary, and tertiary prevention.
Below we list some family- and community-level intervention strategies for different age groups that address SDoMH, but most of them are not currently affiliated with most mental healthcare systems in the U.S. We hope that in near future, closer connections will be established between the two, enabling psychiatric clinicians to refer patients and their families to appropriate sources.
Pre-natal period and early childhood
Nurse-Family Partnership, a home visiting program for families, beginning in pregnancy and continuing for 2 years post-natally, focuses on low-income mothers bearing their first child. This program has been shown to reduce child maltreatment and to improve pregnancy outcomes by helping women engage in good preventive health practices, and improve child health and development [75]. A meta-analysis of studies of nurse home visiting programs demonstrated a significant decline in the risk of recurrence of child maltreatment by parents, after this program was implemented [76]. Such programs should be provided to families in which maltreatment has occurred, so as to reduce its recurrence and foster a child-friendly home environment.
Youth and adulthood
A successful integration of SDoMH-focused and clinical services is the Coordinated Specialty Care (CSC) approach for first-episode psychosis, typically serving young adults [77]. Core components of the program include personalized clinical elements (medication management, resilience-focused individual psychotherapy), family psychoeducation, and SDoMH-focused services such as supported employment and education, and case management [78]. Each therapeutic plan is developed following a shared decision-making model focused on the patient’s preferences, and attention to work and school aspects can include use of evidence-based programs such as Individual Placement and Support [79]. A 2-year NIMH-supported randomized control trial of NAVIGATE, an early CSC intervention, found improvement in quality of life, psychopathology, work and school indices, and treatment retention compared to community care [77]. CSC programs have been implemented in various states, notably statewide in New York as the OnTrackNY program [78].
Mass incarceration of U.S. youth and adults with mental illnesses is a multi-determined social practice driven largely by SDoMH such as racist social policies, unemployment, residential segregation, and neighborhood-level violence, with deleterious health effects on individual inmates [80]. An intensive family- and community-based mental health intervention, labeled multisystemic therapy (MST), has been reported to be effective and cost-efficient in preventing or reducing the likelihood of antisocial behavior, and promoting a healthy course of youth development and adult maturity [81]. A long-term follow-up study showed that siblings in the MST condition had significantly lower arrest rates than the control group (43 vs. 72%, respectively), and were 2–3 times less likely to be convicted of a felony and sentenced to incarceration and probation [82].
Later life
In older adults with mental disorders, social isolation and loneliness are highly prevalent and are associated with worsening of mental, physical, and cognitive functioning [83, 84]. Interventions that promote social engagement improve social connections in older adults but their effects on cognitive function remain uncertain [85]. Early-life adversities and subsequent adverse events over the life course contribute to impaired well-being, and warrant psychosocial and caregiver support [86, 87]. Community-level strategies such as age-friendly communities [88] and compassionate community movement [89] have been reported to be helpful. These can be implemented at county or even local community levels, without needing policy changes at national or state levels.
Across the lifespan
There are several volunteering-based programs to help people with mental disorders. Volunteers constitute often-untapped health and social care capital that can be mobilized to promote the health of persons with mental illnesses. Being a volunteer and giving to others creates purpose in life and expands social networks. Persons with mental disorders who have recovered and are functioning at a healthy level can also serve as volunteers to help their peers who need help. Such volunteers often serve as role models for those suffering from mental disorders. At the same time, volunteering can be stressful and therefore, the organizations must ensure the volunteers’ well-being too. Examples of well-known voluntary organizations include: National Alliance on Mental Illness, Depression and Bipolar Support Alliance, Schizophrenia & Psychosis Action Alliance, Alcoholics Anonymous, the Clubhouse Model which focuses on strengths of people with SMIs, and Community Mental Health Centers – a U.S. government program since the 1970s.
Translational aspects of addressing SDoMH
Given that optimal healthcare should be comprehensively psycho-bio-social, translational research on SDoMH needs to involve interdisciplinary collaborations. There is strong evidence showing that the association of psychosocial and biological impairments in persons with mental illnesses is bi-directional, and involves a vicious cycle of adverse outcomes. SDoMH-induced toxic stress leads to increased allostatic load with worsening inflammation, accelerated aging, epigenetic changes demonstrated in exposomics, and adverse impact on gut microbiome [10]. These systemic changes lead to neurobiological alterations affecting the structure, function, chemistry, and plasticity of the brain. Thus, SDoMH shape brain development and there is now evidence that SDoMH can accelerate brain aging across the lifespan [90, 91]. The result is an increase in mental, physical, and cognitive morbidity, which then worsens socioeconomic adversities. It is the primary healthcare providers’ job to help replace this vicious cycle with a virtuous one in which positive SDoMH such as close social connections lead to healthy biology, resulting in positive mental health.
There are also some recent examples of positive psycho-bio-social interactions at the therapy level. Epigenetic mechanisms play a role in the detrimental effects of traumatic stress including the development of PTSD. A recent study found that successful treatment of PTSD in soldiers with trauma-focused psychotherapy was accompanied by significant changes in DNA methylation at 12 differentially methylated regions in the genes [92]. These data provided longitudinal evidence that ZFP57 methylation seemed to be involved in both the development and successful treatment of deployment-related PTSD. Another study reported epigenome-wide data changes associated with trauma-focused psychotherapies, especially eye movement desensitization and reprocessing therapy, in persons with treatment-resistant depression [93]. Genes and biological pathways related to inflammatory and immune systems were among the most statistically significant results.
Clearly, more translational research of this and other types is needed to broaden our understanding and management of SDoMH in persons with psychiatric disorders.
Recommendations for mental healthcare providers
It is important that clinicians – including psychiatrists, psychologists, primary care physicians, social workers, and pharmacists – work together and partner with peer providers such as nurse practitioners [94] as well as workers in other social sectors, such as education, transportation, correction, and housing. However, the single most vital constituency is that of persons with mental disorders and their families. In a recent report, the National Academies of Sciences, Engineering and Medicine [95] have defined whole health as physical, behavioral, spiritual, and socioeconomic well-being as defined by individuals, families, and communities – and not by healthcare providers. Importantly. whole health care is described as an interprofessional, team-based approach anchored in trusted relationships. This concept has been adopted by the Veterans Administration and is spreading to other healthcare systems [96, 97]. When families feel responsiveness in local systems and people, they are more likely to advocate effectively. Local government agencies, businesses, news media, and large and small donors can provide invaluable help. A lot can be done by a county community health center or by a large health system working with a community health system and a larger county human services system.
There is no single perfect management scheme for SDoMH that will work for all (or most) individuals with mental disorders. Every individual has their own set of SDoMH and these too vary over time. Nonetheless, a knowledgeable and open-minded clinician may attempt to use suitable processes to address SDoMH in a given patient at a given time. The clinician may hold conversations with their colleagues and group leaders or local psychiatric organization. Additionally, their service leadership can have discussions with the Chief Financial Officer of the local health system. An individual clinician cannot be expected to be knowledgeable about all the community resources. But a human services professional could gather information about such resources, keep tabs on changes, and investigate problems when clinicians cannot use the listed resources. We believe that every town in the US should have some civic organization that assembles such a list and makes it available to health care professionals. Local medical organizations should make efforts to find ways to connect with people putting together such a list and providing training for healthcare providers in how to use the list. There are a number of existing SDoMH-focused social programs that have been found to have positive effects on mental health and should be considered as a way of improving the mental healthcare system and even reducing long-term costs of care.
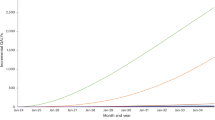
An important target for prevention of psychiatric disorders should be addressing SDoMH that contribute to lower level and quality of education despite access to schools. It is well known that low education is associated with reduced income and increased psychosocial problems such as family disruption, childhood neglect or abuse, alcohol and substance use, employment instability, car accidents, violence, etc. These social problems impact mental health and interfere with acceptance of, adherence to, and effectiveness of care. On the positive side, a surprising finding is that the incidence rate of dementia among octogenarians in Europe and North America has declined by 13% per decade over the past 25 years [98, 99]. A possible explanation is believed to be improved access to quality education for older adults in Europe and the US during recent decades [100]. A focus on improving education levels across the lifespan may have a notable impact on some neuropsychiatric disorders.
One model for overcoming health inequity involves promoting social entrepreneurship and fostering meaningful collaborations to operate with innovation, significant community connections, and systems thinking to address SDoMH [101]. Social entrepreneurs can help reshape access to resources, care, and opportunities for communities, especially those that have been historically underserved. Organizations supporting social entrepreneurs can enable them to bridge systemic gaps and foster sustainable, community-driven solutions through strategies for equitable care delivery, economic stability, and food access. This approach is not just a moral imperative but also a driver of economic growth.
In view of the legal issues frequently affecting people with serious mental illnesses, it will be useful to assess the possible impact of SDoMH on a variety of outcomes such as competency to make treatment decisions, supported decision making, civil commitment, and insanity defense [102, 103].
It is the clinical, medical, and ethical responsibility of mental healthcare providers to ensure that the patients they are serving receive the best care feasible, and this must include addressing the SDoMH that have been clearly shown to have a significant impact on the health and well-being of persons with mental illnesses.
References
Wilkinson R, Marmot M. Social determinants of health: the solid facts. World Health Organization. Copenhagen, Denmark. Regional Regional Office for Europe. 1998; https://iris.who.int/handle/10665/108082
World Health Organization. Social determinants of mental health. Geneva, Switzerland: WHO Press, World Health Organization; 2014. https://www.who.int/publications/i/item/9789241506809
Jeste DV, Pender VB. Social determinants of mental health: recommendations for research, training, practice, and policy. JAMA psychiatry. 2022;79:283–4. https://doi.org/10.1001/jamapsychiatry.2021.4385
Kirkbride JB, Anglin DM, Colman I, Dykxhoorn J, Jones PB, Patalay P, et al. The social determinants of mental health and disorder: evidence, prevention and recommendations. World Psychiatry. 2024;23:58–90
Islam MM. Social determinants of health and related inequalities: confusion and implications. Front Public Health. 2019;7:11. https://doi.org/10.3389/fpubh.2019.00011
Lundberg O. Next steps in the development of the social determinants of health approach: the need for a new narrative. Scand J Public Health. 2020;48:473–9. https://doi.org/10.1177/1403494819894789
Jester, Kohn DJ, Tibiriçá JN, Thomas L, Brown ML, Murphy LL, et al. Differences in social determinants of health underlie racial/ethnic disparities in psychological health and well-being: study of 11,143 older adults. Am J Psychiatry. 2023;180:483–94. https://doi.org/10.1176/appi.ajp.20220158
Jester DJ, Thomas ML, Sturm ET, Harvey PD, Keshavan M, Davis BJ, et al. Review of major social determinants of health in schizophrenia-spectrum psychotic disorders: I. Clinical outcomes. Schizophr Bull. 2023b;49:837–50. https://doi.org/10.1093/schbul/sbad023
Noy A, Natalia M, Jester DJ, Matcheri K, Reynolds CF, Saxena S, et al. Social determinants of mental health in major depressive disorder: umbrella review of 26 meta-analyses and systematic reviews. Psychiatry Res. 2024;335:115854. https://doi.org/10.1016/j.psychres.2024.115854
Jeste DV, Malaspina D, Bagot K, Barch DM, Cole S, Dickerson F, et al. Review of major social determinants of health in schizophrenia-spectrum psychotic disorders: III. Biology. Schizophr Bull. 2023;49:867–80. https://doi.org/10.1093/schbul/sbad031
Gómez CA, Kleinman DV, Pronk N, Wrenn Gordon GL, Ochiai E, Blakey C, et al. Addressing health equity and social determinants of health through healthy people 2030. J Public Health Manag Pract. 2021;27(Suppl 6):S249–S257.
Kessler RC. Challenges in implementing interventions to address the social determinants of mental health. World Psychiatry. 2024;23:92–3.
Novilla MLB, Goates MC, Leffler T, Novilla NKB, Wu CY, Dall A, et al. Integrating social care into healthcare: a review on applying the social determinants of health in clinical settings. Int J Environ Res Public Health. 2023;20:6873. https://doi.org/10.3390/ijerph20196873
Dauner KN, Loomer L. A qualitative assessment of barriers and facilitators associated with addressing social determinants of health among members of a health collaborative in the rural Midwest. BMC Health Serv Res. 2021;21:867. https://doi.org/10.1186/s12913-021-06859-6
Henderson RC, Williams P, Gabbidon J, Farrelly S, Schauman O, Hatch S, et al. Mistrust of mental health services: ethnicity, hospital admission and unfair treatment. Epidemiol Psychiatr Sci. 2015;24:258–65. https://doi.org/10.1017/S2045796014000158
Lewis JH, Lage OG, Grant BK, Rajasekaran SK, Gemeda M, Like RC, et al. Addressing the social determinants of health in undergraduate medical education curricula: a survey report. Adv Med Educ Pract. 2020;11:369–77. https://doi.org/10.2147/AMEP.S243827
Na P, Jeste DV, Pietrzak R. Social disconnection as a global behavioral epidemic: a call to action to address social disconnection in health policy, education, research, and clinical practice. JAMA Psychiatry. 2023;80:101–2. https://doi.org/10.1001/jamapsychiatry.2022.4162
Jiménez-Solomon OG, Méndez-Bustos P, Swarbrick M, Díaz S, Silva S, Kelley M, et al. Peer-supported economic empowerment: a financial wellness intervention framework for people with psychiatric disabilities. Psychiatr Rehabil J. 2016;39:222–33.
Lewis-Fernández R, Rotheram-Borus MJ, Betts VT, Greenman L, Essock SM, Escobar JI, et al. Rethinking funding priorities in mental health research. Br J Psychiatry. 2016;208:507–9. https://doi.org/10.1192/bjp.bp.115.179895
American Academy of Family Physicians. Social determinants of health: guide to social needs screening. The EveryONE Project. 2019. Available at: https://www.aafp.org/dam/AAFP/documents/patient_care/everyone_project/hops19-physician-guide-sdoh.pdf
Buitron de la Vega P, Losi S, Sprague Martinez L, Bovell-Ammon A, Garg A, James T, et al. Implementing an EHR-based screening and referral system to address social determinants of health in primary care. Med Care. 2019;57:S133–9. https://doi.org/10.1097/MLR.0000000000001029
Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: The accountable health communities screening tool. Discussion Paper, National Academy of Medicine, Washington, DC. 2017. https://nam.edu/wpcontent/uploads/2017/05/Standardized-Screening-for-Health-Related-Social-Needs-in-Clinical-Settings.pd
The Joint Commission. (2022, December 20). National patient safety goal to improve health care equity. R3 Report: Requirement, Rationale, Reference, 38. https://www.jointcommission.org/-/media/tjc/documents/standards/r3-reports/r3_npsg-16.pdf
Stanhope V, Choy-Brown M, Williams N, Marcus SC. Implementing person-centered care planning: a randomized controlled trial. Psychiatr Serv. 2021;72:641–6. https://doi.org/10.1176/appi.ps.202000361
Sturm ET, Thomas ML, Sares AG, Dave S, Baron D, Compton MT, et al. Review of major social determinants of health in schizophrenia-spectrum disorders: II. Assessments. Schizophr Bull. 2023;49:851–66. https://doi.org/10.1093/schbul/sbad024
Dubreucq J, Plasse J, Franck N. Self-stigma in serious mental illness: a systematic review of frequency, correlates, and consequences. Schizophr Bull. 2021;47:1261–87. https://doi.org/10.1093/schbul/sbaa181
Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003;121:31–49.
Bourgois P, Holmes SM, Sue K, Quesada J. Structural vulnerability: Operationalizing the concept to address health disparities in clinical care. Acad Med. 2017;92:299–307.
American Psychiatric Association: Diagnostic and statistical manual of mental disorders, Fifth Edition, Text Revision (DSM-5-TRTM). Washington, DC: American Psychiatric Publishing; 2021.
Roland M, Everington S, Marshall M. Social prescribing - transforming the relationship between physicians and their patients. N Engl J Med. 2020;383:97–99.
Wakefield JRH, Kellezi B, Stevenson C, McNamara N, Bowe M, Wilson I, et al. Social prescribing as ‘Social Cure’: a Longitudinal study of the health benefits of social connectedness within a social prescribing pathway. J Health Psychol. 2022;27:386–96. https://doi.org/10.1177/1359105320944991
Napierala H, Krüger K, Kuschick D, Heintze C, Herrmann WJ, Holzinger F. Social prescribing: systematic review of the effectiveness of psychosocial community referral interventions in primary care. Int J Integr Care. 2022;22:11. https://doi.org/10.5334/ijic.6472
Oster C, Skelton C, Leibbrandt R, Hines S, Bonevski B. Models of social prescribing to address non-medical needs in adults: a scoping review. BMC Health Serv Res. 2023;23:642. https://doi.org/10.1186/s12913-023-09650-x
Joo JY, Huber DL. Case management effectiveness on health care utilization outcomes: a systematic review of reviews. West J Nurs Res. 2019;41:111–33. https://doi.org/10.1177/0193945918762135
Harris RC, Popejoy LL. Case management: an evolving role. West J Nurs Res. 2019;41:3–5. https://doi.org/10.1177/0193945918797601
Perez M, Ceballos V, Rubio N, Garcia J, Rubi D, Cabrera A, et al. Defining case management and outreach: perspectives from community health workers in New Mexico. Cogent Soc Sci. 2024;10:2306921. https://doi.org/10.1080/23311886.2024.2306921
Knox M, Esteban EE, Hernandez EA, Fleming MD, Safaeinilli N, Brewster AL. Defining case management success: a qualitative study of case manager perspectives from a large-scale health and social needs support program. BMJ Open Qual. 2022;11:e001807. https://doi.org/10.1136/bmjoq-2021-001807
Denneson LM, Purcell N, McGrath SL, Abadjian LR, Becker WC, Seal KH. Integration of health coaches in a whole health team model of chronic pain care: a qualitative study. J Gen Intern Med. 2023;38:3574–80. https://doi.org/10.1007/s11606-023-08317-x
Purcell N, Zamora K, Bertenthal D, Abadjian L, Tighe J, Seal KH. How va whole health coaching can impact Veterans’ health and quality of life: a mixed-methods pilot program evaluation. Glob Adv Health Med. 2021;10:2164956121998283. https://doi.org/10.1177/2164956121998283
National Academies of Sciences, Engineering, and Medicine. Achieving whole health: a new approach for veterans and the nation. Washington, DC: The National Academies Press;2023. https://doi.org/10.17226/26854
Lim CT, Caan MP, Kim CH, Chow CM, Leff HS, Tepper MC. Care management for serious mental illness: a systematic review and meta-analysis. Psychiatr Serv. 2022;73:180–7. https://doi.org/10.1176/appi.ps.202000473
Unützer J, Katon W, Callahan CM, Williams JW Jr, Hunkeler E, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–45. https://doi.org/10.1001/jama.288.22.2836
Bruce ML, Ten Have TR, Reynolds CF 3rd, Katz II, Schulberg HC, Mulsant BH, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–91. https://doi.org/10.1001/jama.291.9.1081
Reynolds CF, Jeste DV, Sachdev P, Blazer DG. Mental health care for older adults: recent advances and new directions in clinical practice and research. World Psychiatry. 2022;21:336–63. https://doi.org/10.1002/wps.20996
Jeste DV, Alexopoulos GS, Blazer DG, Lavretsky H, Sachdev PS, Reynolds CF. Wisdom, Resilience, and Well-Being in Later Life. Annu Rev Clin Psychol. Advance online publication, 2024;21. https://doi.org/10.1146/annurev-clinpsy-081423-031855
Hickin N, Käll A, Shafran R, Sutcliffe S, Manzotti G, Langan D. The effectiveness of psychological interventions for loneliness: a systematic review and meta-analysis. Clin Psychol Rev. 2021;88:102066. https://doi.org/10.1016/j.cpr.2021.102066
Lee EE, Govind T, Ramsey M, Wu TC, Daly R, Liu J, et al. Compassion toward others and self-compassion predict mental and physical well-being: a 5-year Longitudinal study of 1090 community-dwelling adults across the lifespan. Transl Psychiatry. 2021;11:397. https://doi.org/10.1038/s41398-021-01491-8
Jiang D, Tang VFY, Kahlon M, Chow EO, Yeung DY, Aubrey R, et al. Effects of wisdom-enhancement narrative-therapy and empathy-focused interventions on loneliness over 4 weeks among older adults: a randomized controlled trial. Am J Geriatr Psychiatry. 2025;33:18–30. https://doi.org/10.1016/j.jagp.2024.07.003
Sullivan J, Gualtieri L, Campbell M, Davila H, Pendergast J, Taylor P. VA compassionate contact corps: a phone-based intervention for veterans interested in speaking with peers. Innov Aging. 2021;5(Suppl 1):204. https://doi.org/10.1093/geroni/igab046.788
Sperlich M, Seng JS, Li Y, Taylor J, Bradbury-Jones C. Integrating trauma-informed care into maternity care practice: conceptual and practical issues. J Midwifery Womens Health. 2017;62:661–72. https://doi.org/10.1111/jmwh.12674
Casey BJ, Oliveri ME, Insel T. A neurodevelopmental perspective on the Research Domain Criteria (RDoC) framework. Biol Psychiatry. 2014;76:350–3. https://doi.org/10.1016/j.biopsych.2014.01.006
McLaughlin KA, Gabard-Durnam LG. Experience-driven plasticity and the emergence of psychopathology: a mechanistic framework integrating development and the environment into the Research Domain Criteria (RDoC) model. J Psychopathol Clin Sci. 2022;131:575–87.
Behavioral Health Workforce, 2023. Rockville, MD, National Center for Health Workforce Analysis, 2023. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/Behavioral-Health-Workforce-Brief-2023.pdf
Gennaro A, Kleinbub JR, Mannarini S, Salvatore S, Palmieri A. Training in psychotherapy: a call for embodied and psychophysiological approaches. Res Psychother. 2019;22:395. https://doi.org/10.4081/ripppo.2019.395
Sansen LM, Saupe LB, Steidl A, Fegert JM, Hoffmann U, Neuner F. Daring to process the trauma: using a web-based training to reduce psychotherapists’ fears and reservations around implementing trauma-focused therapy. Eur J Psychotraumatol. 2019;10:1696590. https://doi.org/10.1080/20008198.2019.1696590
Martin A, Naunton M, Kosari S, Peterson G, Thomas J, Christenson JK. Treatment guidelines for PTSD: a systematic review. J Clin Med. 2021;10:4175. https://doi.org/10.3390/jcm10184175
Swerdlow BA, Baker SN, Leifker FR, Straud CL, Rozek DC, Sippel LM. The impact of trauma-focused psychotherapy for posttraumatic stress disorder on interpersonal functioning: a systematic review and meta-analysis of randomized clinical trials. J Trauma Stress. 2023;36:496–510. https://doi.org/10.1002/jts.22906
Bragesjö M. Rethinking the effectiveness of trauma-focused psychological treatments for PTSD. Lancet Psychiatry. 2024;11:83–85. https://doi.org/10.1016/S2215-0366(23)00432-7
Bragesjö M, Ivanov VZ, Andersson E, Rück C. Exploring the feasibility and acceptance of huddinge online prolonged exposure therapy (HOPE) for severe and complex PTSD. Eur J Psychotraumatol. 2024;15:2320607. https://doi.org/10.1080/20008066.2024.2320607
Compton MT. Food and nutrition insecurity: a social determinant hungry for attention by mental health professionals. Psychiatr Serv. 2023;74:1303–6. https://doi.org/10.1176/appi.ps.20220511
Gutwinski S, Schreiter S, Deutscher K, Fazel S. The prevalence of mental disorders among homeless people in high-income countries: an updated systematic review and meta-regression analysis. PLoS Med. 2021;18:e1003750. https://doi.org/10.1371/journal.pmed.1003750
Rafla-Yuan E, Handunge VL, White JJ, and Castillo EG: Housing, Homelessness, and Mental Health. Psychiatric Annals, 2024 (in press). https://doi.org/10.3928/00485713-20240618-02
Killaspy H, Priebe S, King M, Eldridge S, McCrone P, Shepherd G, et al. Supported accommodation for people with mental health problems: the QuEST research programme with feasibility RCT. Southampton (UK): NIHR Journals Library; 2019.
Somers JM, Moniruzzaman A, Patterson M, Currie L, Rezansoff SN, Palepu A, et al. A randomized trial examining housing first in congregate and scattered site formats. PLoS ONE. 2017;12:e0168745. https://doi.org/10.1371/journal.pone.0168745
Mills H, Mulfinger N, Raeder S, Rüsch N, Clements H, Scior K. Self-help interventions to reduce self-stigma in people with mental health problems: a systematic literature review. Psychiatry Res. 2020;284:112702. https://doi.org/10.1016/j.psychres.2019.112702
Yanos PT, Lucksted A, Drapalski AL, Roe D, Lysaker P. Interventions targeting mental health self-stigma: a review and comparison. Psychiatr Rehabil J. 2015;38:171–8. https://doi.org/10.1037/prj0000100
Bannatyne AJ, Jones C, Craig BM, Jones D, Forrest K. A systematic review of mental health interventions to reduce self-stigma in medical students and doctors. Front Med. 2023;10:1204274. https://doi.org/10.3389/fmed.2023.1204274
Oh H, Yang LH, Anglin DM, DeVylder JE. Perceived discrimination and psychotic experiences across multiple ethnic groups in the United States. Schizophr Res. 2014;157:259–65.
Pearce J, Rafiq S, Simpson J, Varese F. Perceived discrimination and psychosis: a systematic review of the literature. Soc Psychiatry Psychiatr Epidemiol. 2019;54:1023–44. https://doi.org/10.1007/s00127-019-01729-3
Wang J, Lloyd-Evans B, Giacco D, Forsyth R, Nebo C, Mann F, et al. Social isolation in mental health: a conceptual and methodological review. Soc Psychiatry Psychiatr Epidemiol. 2017;52:1451–61. https://doi.org/10.1007/s00127-017-1446-1
Smith NG, Hart TA, Kidwai A, Vernon JRG, Blais M, Adam B. Results of a pilot study to ameliorate psychological and behavioral outcomes of minority stress among young gay and bisexual men. Behav Ther. 2017;48:664–77. https://doi.org/10.1016/j.beth.2017.03.005
Ross LE, Doctor F, Dimito A, Kuehl D, Armstrong MS. Can talking about oppression reduce depression? Modified CBT group treatment for LGBT people with depression. J Gay Lesbian Soc Se. 2007;19:1–15. https://doi.org/10.1300/J041v19n01_01
Suijkerbuijk YB, Schaafsma FG, van Mechelen JC, Ojajärvi A, Corbière M, Anema JR. Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta-analysis. Cochrane Database Syst Rev. 2017;9:CD011867. https://doi.org/10.1002/14651858.CD011867.pub2
Areberg C, Bejerholm U. The effect of IPS on participants’ engagement, quality of life, empowerment, and motivation: a randomized controlled trial. Scand J Occup Ther. 2013;20:420–8. https://doi.org/10.3109/11038128.2013.765911
Miller TR. Projected outcomes of nurse-family partnership home visitation during 1996–2013, USA. Prev Sci. 2015;16:765–77. https://doi.org/10.1007/s11121-015-0572-9
Han K, Oh S. The effectiveness of home visiting programs for the prevention of child maltreatment recurrence at home: a systematic review and meta-analysis. Child Health Nurs Res. 2022;28:41–50. https://doi.org/10.4094/chnr.2022.28.1.41
Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL, Rosenheck RA, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. Am J Psychiatry. 2016;173:362–72. https://doi.org/10.1176/appi.ajp.2015.15050632
Bello I, Lee R, Malinovsky I, Watkins L, Nossel I, Smith T, et al. OnTrackNY: the development of a coordinated specialty care program for individuals experiencing early psychosis. Psychiatr Serv. 2017;68:318–20.
Drake RE, Bond GR. IPS support employment: a 20-year update. Am J Psychiatr Rehabil. 2011;14:155–64.
Wildeman C, Wang EA. Mass incarceration, public health, and widening inequality in the USA. Lancet. 2017;389:1464–74.
Henggeler, SW (2018). Multisystemic family therapy. In: Lebow, J, Chambers, A, Breunlin, D (eds) Encyclopedia of couple and family therapy. Cham: Springer. https://doi.org/10.1007/978-3-319-15877-8_165-1
Wagner DV, Borduin CM, Sawyer AM, Dopp AR. Long-term prevention of criminality in siblings of serious and violent juvenile offenders: a 25-year follow-up to a randomized clinical trial of multisystemic therapy. J Consult Clin Psychol. 2014;82:492–9. https://doi.org/10.1037/a0035624
Eglit GML, Palmer BW, Martin AS, Tu X, Jeste DV. Loneliness in schizophrenia: construct clarification, measurement, and clinical relevance. PLoS ONE. 2018;13:e0194021. https://doi.org/10.1371/journal.pone.0194021
Su Y, Rao W, Li M, Caron G, D’Arcy C, Meng X. Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: a systematic review and meta-analysis. Int Psychogeriatr. 2023;35:229–41. https://doi.org/10.1017/S1041610222000199
Joshi P, Hendrie K, Jester DJ, Dasarathy D, Lavretsky H, Ku BS, et al. Social connections as determinants of cognitive health and as targets for social interventions in persons with or at risk of Alzheimer’s disease and related disorders: a scoping review. Int Psychogeriatr. 2024;36:92–118. https://doi.org/10.1017/S1041610223000923
Richardson S, Carr E, Netuveli G, Sacker A. Adverse events over the life course and later-life wellbeing and depressive symptoms in older people. Int Psychogeriatr. 2023;35:243–57. https://doi.org/10.1017/S1041610220003373
Rowland G, Hindman E, Hassmén P, Radford K, Draper B, Cumming R, et al. Depression, childhood trauma, and physical activity in older Indigenous Australians. Int Psychogeriatr. 2023;35:259–69. https://doi.org/10.1017/S1041610221000132
Meeks S. Age-friendly communities: introduction to the special issue. Gerontologist. 2022;62:1–5. https://doi.org/10.1093/geront/gnab163
Mills J, Abel J, Kellehear A, Noonan K, Bollig G, Grindod A, et al. The role and contribution of compassionate communities. Lancet. 2024;404:104–6. https://doi.org/10.1016/S0140-6736(23)02269-9
Moguilner S, Baez S, Hernandez H, Migeot J, Legaz A, Gonzalez-Gomez R, et al. Brain clocks capture diversity and disparities in aging and dementia across geographically diverse populations. Nat Med. 2024;30:3779. https://doi.org/10.1038/s41591-024-03209-x. Epub ahead of print. Erratum in: Nat Med. 2024 Sep 16. 10.1038/s41591-024-03294-y. PMID: 39187698
Ibanez A, Kringelbach ML, Deco G. A synergetic turn in cognitive neuroscience of brain diseases. Trends Cogn Sci. 2024;28:319–38. https://doi.org/10.1016/j.tics.2023.12.006
Vinkers CH, Geuze E, van Rooij SJH, Kennis M, Schür RR, Nispeling DM, et al. Successful treatment of post-traumatic stress disorder reverses DNA methylation marks. Mol Psychiatry. 2021;26:1264–71. https://doi.org/10.1038/s41380-019-0549-3
Carvalho Silva R, Martini P, Hohoff C, Mattevi S, Bortolomasi M, Menesello V, et al. DNA methylation changes in association with trauma-focused psychotherapy efficacy in treatment-resistant depression patients: a prospective longitudinal study. Eur J Psychotraumatol. 2024;15:2314913. https://doi.org/10.1080/20008066.2024.2314913
Balestra ML. Family nurse practitioner scope of practice issues when treating patients with mental health issues. J Nurse Pract. 2019;15:479–82. https://doi.org/10.1016/j.nurpra.2018.11.007
National Academies of Sciences. Engineering and medicine: achieving whole health: a new approach for veterans and the nation. Washington, DC: National Academies Press; 2023.
Falconi AM, Johnson M, Chi W, Stephenson JJ, Marc Overhage J, Agrawal S. Health related social needs and whole person health: relationship between unmet social needs, health outcomes, and healthcare spending among commercially insured adults. Prev Med Rep. 2023;36:102491. https://doi.org/10.1016/j.pmedr.2023.102491
Reddy B, Wisneski LA. Whole person health: the role of advocacy. Glob Adv Health Med. 2022;11:2164957X221082650. https://doi.org/10.1177/2164957X221082650
Wolters FJ, Chibnik LB, Waziry R, Anderson R, Berr C, Beiser A, et al. Twenty-seven-year time trends in dementia incidence in Europe and the United States: the Alzheimer Cohorts Consortium. Neurology. 2020;95:e519–e531. https://doi.org/10.1212/WNL.0000000000010022
Wetterberg H, Najar J, Sterner TR, Rydén L, Erhag HF, Sacuiu S, et al. Decreasing incidence and prevalence of dementia among octogenarians. A population-based study on three cohorts born 30 years apart. Gerontol A Biol Sci Med Sci. 2023;78:1069–77. https://doi.org/10.1093/gerona/glad071
Knopman DS. The enigma of decreasing dementia incidence. JAMA Netw Open. 2020;3:e2011199. https://doi.org/10.1001/jamanetworkopen.2020.11199
Landrum A, Fakeye MK, Kelm N, Sapra K, Bhatt J: Social entrepreneurs on the front line of equity are building bridges to better health. Health Affairs Branded Post, 2024. https://doi.org/10.1016/j.hjdsi.2024.100735
Jeste DV, Eglit GML, Palmer BW, Martinis JG, Blanck P, Saks ER. Supported decision making in serious mental illness. Psychiatry. 2018;81:28–40. https://doi.org/10.1080/00332747.2017.1324697
Mahomed F, Stein MA, Sunkel C, Restivo JL, Patel V. Mental health, human rights, and legal capacity. Lancet Psychiatry. 2022;9:341–2. https://doi.org/10.1016/S2215-0366(21)00463-6
Acknowledgements
Sources of support: RL-F is supported by the New York State Office of Mental Health, New York, NY. ERS is supported by the Saks Institute at University of Southern California, Los Angeles, CA. PJN is supported by the U.S. Department of Veterans Affairs via 1IK1CX002532-01. RHP is supported by the U.S. Department of Veterans Affairs National Center for PTSD. MQ is supported by the New York State Psychiatric Institute, New York, NY. RCK is a consultant for Cambridge Health Alliance, Canandaigua VA Medical Center, Child Mind Institute, Holmusk, Massachusetts General Hospital, Partners Healthcare, Inc., RallyPoint Networks, Inc., Sage Therapeutics, and University of North Carolina.
Author information
Authors and Affiliations
Contributions
DVJ Prepared the first draft of the manuscript, developed the overall research framework, and managed overall project coordination, timelines, and resource allocation. JS Revised and refined the manuscript; and developed the overall research framework. RL-F Prepared the first draft of the manuscript, developed the overall research framework, and secured financial support through grants, institutional funding, or sponsorships. ERS Revised and refined the manuscript and developed the overall research framework. PJN Revised and refining the manuscript, and secured financial support through grants, institutional funding, or sponsorships. RHP Revised and refined the manuscript, and secured financial support through grants, institutional funding, or sponsorships. MQ Revised and refined the manuscript, and managed overall project coordination, timelines, and resource allocation. RCK Prepared the first draft of the manuscript, developed the overall research framework, and secured financial support through grants, institutional funding, or sponsorships.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jeste, D.V., Smith, J., Lewis-Fernández, R. et al. Addressing social determinants of health in individuals with mental disorders in clinical practice: review and recommendations. Transl Psychiatry 15, 120 (2025). https://doi.org/10.1038/s41398-025-03332-4
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03332-4