Abstract
A family history (FH) of depression significantly influences the progress of major depressive disorder (MDD). However, the underlying neural mechanism of FH remains unclear. This study examined the association between brain structural and connectivity alterations, inflammation, and FH in MDD. A total of 134 MDD patients with (FH group, n = 43) and without (NFH group, n = 91) first-degree FH and 96 demographic-matched healthy controls (HCs) were recruited. Voxel-based morphometry (VBM) and sliding-window dynamic functional connectivity (dFC) analyses were performed, and inflammatory biomarkers (C-reactive protein (CRP) and interleukin-6 (IL-6)) were detected. Compared with HCs, FH and NFH groups showed decreased gray matter volume (GMV) in the left cerebellum posterior lobe and increased dFC between this region and the left inferior parietal lobule. The FH group showed increased dFC between the cerebellum region and medial prefrontal cortex (mPFC) compared to NFH and HCs. The combination of these brain measurements further differentiated between FH and NFH. Moreover, the GMV of the cerebellum was positively correlated with CRP in the NFH group, while the dFC between the cerebellum and mPFC was positively correlated with IL-6 in the FH group. The present findings indicate that cerebellar structure and dynamic function vary according to FH of MDD and are related to inflammatory factors, potentially offering novel insights into the underlying pathogenic mechanisms of MDD.
Similar content being viewed by others
Introduction
Major depressive disorder (MDD) is a prevalent mental illness affecting 4.4% of the global population [1]. MDD seriously impairs the physical and psychological well-being of patients and their families and is often transmitted across the pedigree [2]. Family history (FH) is one of the prominent risk factors for MDD, with a nearly 3-fold increased lifetime risk of developing this disorder in the offspring of patients compared to healthy controls (HCs) [3]. Familial MDD is reported to be more severe, recurrent, and resistant to treatment than non-familial MDD [4, 5]. Furthermore, MDD patients with FH typically exhibit an earlier age of onset, generally occurring between 15 and 25 years [6, 7]. Therefore, it is critical to gain a thorough understanding of the underlying neurobiological mechanisms of FH to develop treatment and prevention strategies for depression.
Emerging evidence suggests that FH of depression alters brain structure and function related to emotional regulation and reward processing [8], and neural circuits involved in emotional regulation [9] and mentalization [10,11,12]. However, few studies have focused on brain alterations in patients with MDD having FH. MDD patients with FH exhibited reduced gray matter volume (GMV) in the amygdala compared to patients without FH [13], thinner subcallosal cortex and insula [14], altered activation in the superior frontal gyrus, cuneus, and middle frontal gyrus during reward processing [15] compared to young women with high family risk. Furthermore, activation in the ventral anterior cingulate cortex and putamen could effectively differentiate individuals with high familial risk from patients with familial MDD [15]. The white matter network of MDD patients with FH also exhibited higher average controllability based on network control theory [16]. These findings indicate that the pathological mechanisms of MDD with and without FH may differ and were mediated by not only neuroanatomic patterns but also the interaction between brain regions.
This literature raises two concerns. First, previous studies focusing on single brain modality restricted the potential to build across units of analysis-a tenet of Research Domain Criteria adopted by the National Institute of Mental Health. Integrating neuroanatomic and functional connectivity (FC) analyses offer complementary insights into the brain’s organization [17], potentially enhancing the understanding of structure-function relationship and yielding new perspectives on the pathophysiology of FH of depression. Second, inflammatory markers including C-reactive protein (CRP) and interleukin-6 (IL-6), are also implicated in the pathophysiology of MDD [18, 19] and exhibit changes concerning FH [20]. Animal studies have demonstrated that peripheral inflammatory cytokines can cross the blood-brain barrier, resulting in a generalized inflammatory condition in the brain and thus disrupting brain function and structure [21, 22]. Moreover, the altered brain structure [23, 24] and connectivity [25] were correlated with elevated IL-6 and CRP levels in patients with MDD. Nevertheless, the relationship between inflammation, brain structure and connectivity, and FH remains unknown in MDD.
Therefore, we aimed to perform an exploratory study to investigate whether MDD patients with and without FH exhibit distinct alterations in brain structure and connectivity compared to HCs using voxel-based morphometry (VBM) and dynamic FC (dFC) analyses. Different from time-averaged FC, dFC can track real-time activity changes in brain connectivity across different brain states [26]. Whether the altered structure and dFC constitute potential neuromarkers for distinguishing MDD with and without FH was then examined. Finally, we examined the association between the altered GMV and dFC, inflammatory index, and FH in patients with MDD. Based on previous literature, we hypothesized that MDD patients with and without FH would exhibit distinct patterns of altered GMV and dFC within the regions subserving cognition and emotion processing, and these alterations further can be used to differentiate these two groups. We also hypothesized that these altered brain measurements correlate with inflammation and are influenced by FH in patients with MDD.
Methods and materials
Participants
A total of 134 MDD patients were recruited from the First Affiliated Hospital of Zhengzhou University. The inclusion criteria were: (1) meeting the diagnostic criteria for MDD as specified by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) and (2) being of Han Chinese ethnicity. The exclusion criteria were: (1) presenting with comorbid psychotic illness, (2) having an FH of inherited diseases, (3) having organic mental disorders, (4) having psychoactive substance abuse, and (5) contraindications for magnetic resonance imaging (MRI). The 24-item Hamilton Depression Rating Scale (HAMD) was used to estimate the severity of depression. Patients with MDD were divided into the FH (FH) and without FH (NFH) groups based on whether they had at least one first-degree relative with a known history of either past or current MDD.
Ninety-six HCs were recruited from the community via poster advertisements. Inclusion criteria comprised: (1) having no FH of mental disorders, (2) lifetime absence of psychiatric illnesses and substance abuse, (3) having no contraindications to MRI, and (4) from Han Chinese ethnicity. The study was approved by the Medical Research Ethics Committee of the First Affiliated Hospital of Zhengzhou University and is registered on the Chinese Clinical Trial Registry (ChiCTR, number: ChiCTR1900022331, https://www.chictr.org.cn/showproj.html?proj=37724). All participants or their guardians provided informed consent before the experiment. All methods were performed in accordance with the guidelines and relevant regulations.
Inflammatory indexes measurement
A 5 ml of peripheral fasting blood samples were drawn from the patients at 8:00 AM. The blood samples were placed in an EP tube. The measurement of plasma CRP and IL-6 levels was completed in the Laboratory Department of the First Affiliated Hospital of Zhengzhou University. The plasma levels of CRP were determined by the immune scattering turbidimetry using an Aristo automated analyzer (Shenzhen Guosai Biological Co., China) according to the manufacturer’s instructions. The plasma levels of IL-6 were quantified by electrochemiluminescence immunoassay using the Roche cobas e801 automated analyzer (Roche Diagnostics, Switzerland) according to the manufacturer’s protocol.
Image acquisition
MRI data was obtained on a 3.0T GE DISCOVERY MR750 scanner (General Electric, Fairfield Connecticut, USA) equipped with a high-speed gradient and an 8-channel head coil. Foam pads and headphones were used to minimize head movement and scanner noise. The main parameters for structural MRI images were set as follows: repetition time (TR)/echo time (TE) = 8.2/3.2 ms, flip angle = 7°, slice thickness = 1 mm, slices = 188, field of view (FOV) = 256 × 256 mm2, matrix size = 256 × 256, and voxel size = 1 × 1 × 1 mm3, no gap. Resting-state functional MRI images were scanned using an echo-planar imaging sequence with the following parameters: TR/TE = 2000/40 ms, slices = 32, matrix size = 64 × 64, flip angle = 90°, FOV = 220 × 220 mm2, voxel size = 3.44 × 3.44 × 3.44 mm3, thickness = 4 mm, gap = 0.5 mm, and a total of 180 volumes.
VBM analysis
The voxel-wise GMV of the structural T1-weighted images was measured using the VBM toolbox (http://dbm.neuro.uni-jena.de/vbm8) in the SPM12 software (http://www.fil.ion.ucl.ac.uk/spm). First, the artifacts of the images were checked, and the origins of the images were adjusted to the anterior commissure. Subsequently, the images were segmented into gray matter, white matter, and cerebral spinal fluid maps, and then normalized to the standard Montreal Neurological Institute (MNI) space with a voxel size of 1.5 × 1.5 × 1.5 mm3. After the data quality of the segmented maps was checked, the gray matter maps were further smoothed using an 8 mm full width at half maximum Gaussian kernel.
DFC analysis
Preprocessing of functional MRI images was performed using the DPARSF toolbox (http://rfmri.org/dpabi). The pipeline included as following: (1) remove the first 5 volumes (remaining 175 volumes), (2) slice-timing, (3) head motion correction, all participants were retained under the head motion criteria of translation <2 mm or rotation <2° in any direction, (4) normalized to the standard MNI space with a voxel size of 3 × 3 × 3 mm3, (5) regression of nuisance covariates (i.e., white matter, cerebrospinal fluid, the Friston-24 parameters of head motion, and global signal), (6) spatial smoothed with full width at half maximum = 6 mm, (7) linear detrend, (8) filtering (0.01–0.1 Hz). Subsequently, the framewise displacement (FD) across time points for each subject was calculated to assess head motion. Scrubbing was performed with an FD threshold of 0.5 mm, and the “bad” time points and their 1-back and 2-forward volumes were interpolated using the cubic spline [27].
The sliding window correlation approach was performed to assess the time-varying dFC of the brain regions identified by VBM analysis. Based on our previous dFC studies [26, 28], the window length was set to 50 TRs (100 s) and the shift step size was 5 TRs (10 s). In each window, Fisher’s z-transformed Pearson’s correlation coefficient between the average time series of each seed region and the remaining voxels in the whole brain was calculated. Thus, a set of sliding-window correlation maps for each participant was obtained. Finally, the dFC was estimated by calculating the standard deviation at each voxel across sliding-windows.
Statistical analyses
A one-way analysis of variance (ANOVA) was conducted to investigate the differences in GMV and dFC among the HCs, FH, and NFH groups while controlling for age, gender, and years of education. To remove the influence of head movement, the mean FD was also included as a covariate during the one-way ANOVA of dFC. Multiple comparison correction was performed using Gaussian random field theory with cluster corrected p < 0.05 and a voxel height of p < 0.005. Post-hoc comparisons were then conducted using two-tailed, two-sample t-tests, and the significance threshold was set at p < 0.05/3 (Bonferroni corrected).
The identified altered GMV and dFC were then used to test the association between clinical and inflammatory variables in FH and NFH groups. A two-tailed Pearson correlation analysis was conducted between the altered GMV/dFC values and HAMD, CRP, and IL-6 scores with the significance threshold at p < 0.05.
Based on the aforementioned analysis results and the understanding that inflammation affects the brain in depression, a mediation analysis was performed to examine whether IL-6 mediates the relationship between FH and altered dFC between the cerebellum and mPFC in patients with MDD, utilizing the PROCESS macro in SPSS software. Several paths between variables were established with FH as the independent variable, altered dFC as the dependent variable, and IL-6 as a mediator. The analysis was adjusted for age, sex, and education level. The mediation effect was estimated using 5000 bias-corrected bootstraps and deemed significant if the 95% confidence interval (CI) excluded zero. Comprehensive details regarding the mediation analysis can be found in [29].
Classification analysis
A classification analysis was implemented to test whether abnormal GMV and dFC of the cerebellum can be used as potential biomarkers for distinguishing FH from NFH groups. Furthermore, to determine whether the combined structure and dynamic function yield better classification performance than structure or dynamic function alone, the identified altered GMV, altered dFC, and their combination were utilized as features, respectively. We selected the radial basis function kernel for the support vector machine classifier as the classification model. A grid search algorithm was employed to choose the optimal parameters for the classifier. Additionally, to tackle the issue of imbalanced data, the Random Under Sampler function was utilized to selectively remove some samples from the majority class [30], thereby aligning its sample count with that of the minority class. Subsequently, a five-fold cross-validation method was applied to obtain stable model performance. Lastly, the receiver-operating characteristic (ROC) curve was implemented to evaluate the classification performance, and the average area under the curve (AUC) value of the five-fold cross-validation was reported. The non-parametric permutation test was utilized to test whether the AUC is significantly greater than random occurrences. Detailed information on the permutation test can be found in [28].
Results
Demographic and clinical variables
The demographic and clinical data of all the participants are summarized in Table 1. Three groups were matched in age, gender, and mean FD except for education level. There were no significant differences between FH and NFH group in clinical data (i.e., age of onset, number of depressive episodes, and HAMD socres) and inflammatory indices (i.e., CRP and IL-6). But a significant group difference was observed in the duration of illness, with the FH group exhibiting a longer duration than NFH group.
Group differences in GMV
One-way ANOVA revealed a significant group effect of the GMV in the left cerebellum posterior lobe (Cere8, MNI coordinates: x, y, z = \(-\)26, \(-\)57, \(-\)51; F = 7.60, cluster size = 589 voxels) (Fig. 1). Post hoc analysis revealed a decreased GMV in the cerebellum region in both FH and NFH groups compared to HCs.
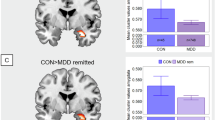
Group differences in dFC of the cerebellum
One-way ANOVA revealed a significant group effect on dFC between the cerebellum and medial prefrontal cortex (mPFC, MNI coordinates: x, y, z = 12, 54, 9; F = 11.86; cluster size = 35 voxels) and left inferior parietal lobule (L_IPL, MNI coordinates: x, y, z = \(-\)51, \(-\)60, 42; F = 8.35, cluster size = 45 voxels) (Fig. 2). Post hoc analysis showed that the FH-specific increased dFC between the cerebellum and mPFC compared to NFH and HCs. FH and NFH groups demonstrated increased dFC between the cerebellum and IPL compared to HCs.
Association of altered GMV/dFC of cerebellum with inflammatory variables
The GMV of the cerebellum was positively correlated with CRP in the NFH group (r = 0.46, p = 0.006), while there was no significant correlation with CRP in the FH group (r = \(-\)0.29, p = 0.13) (Fig. 3A). Moreover, the dFC between the cerebellum and mPFC was positively correlated with IL-6 in the FH group (r = 0.34, p = 0.005), while no significant correlation with IL-6 in the NFH group (r = \(-\)0.14, p = 0.54) (Fig. 3B). No significant correlations were found between other altered GMV/dFC and HAMD, CRP, and IL-6.
A Altered GMV of the cerebellum posterior lobe correlated with CRP in NFH group. B Altered dFC between the cerebellum posterior lobe and mPFC correlated with IL-6 in FH group. L left, Cere cerebellum, mPFC medial prefrontal cortex, CRP C-reactive protein, IL-6 interleukin-6. FH major depressive disorder with a first-degree family history, NFH major depressive disorder without family history.
Mediation analysis result
Mediation analysis revealed that FH had a significant direct effect on dFC between the cerebellum and mPFC (direct effect = \(0.04\), p = 0.006, 95% CI from the bootstrap test including zero [0.02–0.07]), but had no significant indirect effect on the dFC via IL-6 (indirect effect = 0.001, 95% CI from the bootstrap test excluding zero [\(-\)0.002 to 0.02]).
Classification result
In the classification analysis between FH and NFH groups, the combination of the GMV and dFC of the cerebellum demonstrated a higher AUC (AUC = 0.80, p < 0.01) than either GMV (AUC = 0.66, p = 0.02) or dFC (AUC = 0.67, p = 0.01) alone (Fig. 4).
Discussion
This is the first study to examine the relationship between cerebellar anatomical and connectivity alterations, inflammation, and FH in MDD. Results indicated that FH and NFH exhibited reduced GMV in the left cerebellum posterior lobe and increased dFC between the cerebellum posterior lobe and IPL, whereas the FH group showed specifically increased dFC between the cerebellum posterior lobe and mPFC. The altered GMV and dFC of the cerebellum contributed to differentiating FH from NFH and were linked to inflammatory factors. Altogether, our results provide new insights into the pathophysiological mechanisms underlying depression.
The cerebellum is well-known to be involved in motor function [31]; however, it has been demonstrated to significantly contribute to higher-order functions, including executive processes and emotion regulation, through its connections with various cerebral regions [32,33,34]. MDD patients have been frequently shown structure and brain connectivity abnormalities of the cerebellar regions [35]. For instance, MDD patients exhibited decreased cerebellar gray matter density and GMV [36], and increased inter-module connections between the cerebellum and central executive network [37]. Lower GMV in the left cerebellar area VIIa, VIIB, and crus II was correlated with impaired attention and executive dysfunction in remitted MDD patients with cognitive deficits [38, 39]. After electroconvulsive therapy treatment, the GMV of cerebellar area VIIa and crus I increased [40], and the FC between the cerebellum and IPL changed and mediated the effect of the whole-brain electric field on antidepressant outcomes in MDD [41]. Extensions to previous findings, we further found that both FH and NFH groups exhibited shared reduced GMV in the left cerebellum posterior lobe and increased dFC between the cerebellum region and IPL compared to HCs. Furthermore, although not statistically significant, the FH group showed lower volume and larger dFC than the NFH group. Taken together, we speculated that the cerebellum makes outstanding contributions to the etiology of depression and is likely associated with the FH of MDD. This point happens to be evidenced by that individuals carrying the MDD risk allele of rs12415800 exhibiting reduced GMV in the left posterior cerebellar lobe compared to those with non-risk allele [42].
The FH group showed specifically increased dFC between the posterior cerebellar lobe and mPFC compared to both NFH and HC groups. MPFC is a hub area of the default mode network (DMN) which regulates cognition, motivation, emotion, and sociability [43]. Major connections to the DMN are considered to originate from the posterior part of crus I and II of lobule VIIA [32, 44], and the lobule IX area is an essential cerebellar representation of the DMN [45], which participates in social inference [46]. The increased cerebellar-anterior DMN connectivity [47, 48], and decreased cerebellar connectivity with posterior DMN regions [49, 50] were reported in MDD patients. Decreased dFC between left cerebellar vermis and ventromedial PFC was positively related to the severity of depressive symptoms in MDD patients [51]. Moreover, individuals with a high family risk for depression also exhibit increased FC between the posterior cerebellum lobe and ventromedial PFC during social cognition task [12]. Here, our result suggests that MDD patients with FH exhibit more abnormalities in brain dynamic function compared to those without FH, which is probably associated with more severe clinical manifestations in familial depression. The cerebellar-DMN connectivity may play a central role in the underlying risk for developing MDD, potentially serving as a target for prevention and treatment in familial MDD.
The cerebellar structure and connectivity present significant potential for diagnosing MDD [52, 53], our findings further showed that the combination of structure and dynamic connectomes as features achieved higher AUC values than either GMV or dFC alone for the classification of MDD with and without FH. This indicates that altered multimodal MRI characteristics provide complementary information for the neural markers of FH of depression, and is recommended for future neuroimaging research.
As expected, the positive relationship between the decreased cerebellar GMV and CRP was observed in NFH group, while the increased dFC between the posterior cerebellum lobe and mPFC was positively associated with IL-6 in FH group. In line with previous literature [24, 25, 54], our finding highlights the relationship between inflammatory markers and neuroimaging traits and further suggests the influence of FH in this context. The inflammation-related deficit in cerebellar structure and connectivity has important implications on the pathophysiologic mechanism of MDD, and may inform future research on precision therapies for patients with elevated inflammation. Furthermore, although not reaching statistical significance, the mean levels of CRP and IL-6 were higher in the FH group compared to NFH group, suggesting that neuroinflammatory alterations are more prominent in familial MDD patients [20]. Unfortunately, as we did not find a mediation effect of IL-6 on the relationship between FH and dFC, it remains uncertain whether the more pronounced neuroinflammatory changes induced by FH lead to more significant alterations in brain connectivity in familial MDD. Further research is necessary to verify the mediating role of inflammatory factors.
Several limitations should be noted. First, our study of FH encapsulates not merely an estimation of genetics but also reflects the impact of a stressful familial environment. Future research should designed to distinguish the unique contributions of genetic and environmental effects. Second, the current results may be attributed to the small size of the FH group, which limited the statistical significance of the clinical variables between NFH and FH groups, as well as the mediation effect. Third, the cross-sectional design made it difficult to determine whether the abnormal structure and dFC are consequences or precursors of MDD, a longitudinal study design is needed to figure out this issue. Last, most MDD patients in our study were administered psychotropic medications, future research should consider the impact of these medications on structure and connectivity of the cerebellum, and inflammation.
In conclusion, the present study utilizing combined structural and dFC analyses indicates that cerebellar structure and dynamic function vary according to the FH of MDD, and these alterations may serve as biomarkers for distinguishing between FH and NFH groups. Furthermore, the changed brain measurements are associated with inflammatory factors and the relationship is influenced by FH. Our results imply that the interaction of the brain and inflammation plays a pivotal role in the etiology of depression, offering novel insights into precise treatment and prevention strategies for depression.
Data availability
All data and code in the article will be made available upon reasonable request.
References
Friedrich MJ. Depression is the leading cause of disability around the world. JAMA. 2017;317:1517–17.
Grillon C, Warner V, Hille J, Merilangas KR, Bruder GE, Tenke CE, et al. Families at high and low risk for depression: a three-generation startle study. Biol Psychiatry. 2005;57:953–60.
Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000;157:1552–62.
Peterson BS, Wang Z, Horga G, Warner V, Rutherford B, Klahr KW, et al. Discriminating risk and resilience endophenotypes from lifetime illness effects in familial major depressive disorder. JAMA Psychiatry. 2014;71:136–48.
Hardeveld F, Spijker J, De Graaf R, Hendriks SM, Licht CM, Nolen WA, et al. Recurrence of major depressive disorder across different treatment settings: results from the NESDA study. J Affect Disord. 2013;147:225–31.
Tozzi F, Prokopenko I, Perry JD, Kennedy JL, McCarthy AD, Holsboer F, et al. Family history of depression is associated with younger age of onset in patients with recurrent depression. Psychol Med. 2008;38:641–49.
Weissman MM, Wickramaratne P, Nomura Y, Warner V, Verdeli H, Pilowsky DJ, et al. Families at high and low risk for depression: A 3-generation study. Arch Gen Psychiatry. 2005;62:29–36.
Nazarova A, Schmidt M, Cookey J, Uher R. Neural markers of familial risk for depression–a systematic review. Dev Cogn Neurosci. 2022;58:101161.
Wackerhagen C, Wüstenberg T, Mohnke S, Erk S, Veer IM, Kruschwitz JD, et al. Influence of familial risk for depression on cortico-limbic connectivity during implicit emotional processing. Neuropsychopharmacology. 2017;42:1729–38.
Posner J, Cha J, Wang Z, Talati A, Warner V, Gerber A, et al. Increased default mode network connectivity in individuals at high familial risk for depression. Neuropsychopharmacology. 2016;41:1759–67.
Cai Y, Elsayed NM, Barch DM. Contributions from resting state functional connectivity and familial risk to early adolescent-onset MDD: results from the adolescent brain cognitive development study. J Affect Disord. 2021;287:229–39.
Tepfer LJ, Alloy LB, Smith DV. Family history of depression is associated with alterations in task-dependent connectivity between the cerebellum and ventromedial prefrontal cortex. Depress Anxiety. 2021;38:508–20.
Saleh K, Carballedo A, Lisiecka D, Fagan AJ, Connolly G, Boyle G, et al. Impact of family history and depression on amygdala volume. Psychiatry Res. 2012;203:24–30.
Burhanoglu BB, Dinçer G, Yilmaz A, Ozalay O, Uslu O, Unaran E, et al. Brain areas associated with resilience to depression in high-risk young women. Brain Struct Funct. 2021;226:875–88.
Fischer AS, Ellwood-Lowe ME, Colich NL, Cichocki A, Ho TC, Gotlib IH. Reward-circuit biomarkers of risk and resilience in adolescent depression. J Affect Disord. 2019;246:902–09.
Hahn T, Winter NR, Ernsting J, Gruber M, Mauritz MJ, Fisch L, et al. Genetic, individual, and familial risk correlates of brain network controllability in major depressive disorder. Mol Psychiatry. 2023;28:1057–63.
Li W, Tang L, Wang M, Wang J, Guo T, He Q, et al. Altered gray matter volume and functional connectivity in medial orbitofrontal cortex of bulimia nervosa patients: a combined VBM and FC study. Front Psychiatry. 2022;13:963092.
Zeng Y, Chourpiliadis C, Hammar N, Seitz C, Valdimarsdottir UA, Fang F, et al. Inflammatory biomarkers and risk of psychiatric disorders. JAMA Psychiatry. 2024;81:1118–29.
Miller AH. Beyond depression: the expanding role of inflammation in psychiatric disorders. World Psychiatry. 2020;19:108–09.
Yibulaiyin H, Sun H, Yang Y. Depression is associated with CRP SNPs in patients with family history. Transl Neurosci. 2017;8:201–06.
Barnes J, Mondelli V, Pariante CM. Genetic contributions of inflammation to depression. Neuropsychopharmacology. 2017;42:81–98.
Han KM, Ham BJ. How inflammation affects the brain in depression: a review of functional and structural MRI studies. J Clin Neurol. 2021;17:503–15.
Green C, Shen X, Stevenson AJ, Conole ELS, Harris MA, Barbu MC, et al. Structural brain correlates of serum and epigenetic markers of inflammation in major depressive disorder. Brain Behav Immun. 2021;92:39–48.
Opel N, Cearns M, Clark S, Toben C, Grotegerd D, Heindel W, et al. Large-scale evidence for an association between low-grade peripheral inflammation and brain structural alterations in major depression in the BiDirect study. J Psychiatry Neurosci. 2019;44:423–31.
Felger JC, Li Z, Haroon E, Woolwine BJ, Jung MY, HuA X, et al. Inflammation is associated with decreased functional connectivity within corticostriatal reward circuitry in depression. Mol Psychiatry. 2016;21:1358–65.
Pang Y, Zhang H, Cui Q, Yang Q, Lu F, Chen H, et al. Combined static and dynamic functional connectivity signatures differentiating bipolar depression from major depressive disorder. Aust N Z J Psychiatry. 2020;54:832–42.
Power JD, Barnes KA, Snyder AZ, Schlaggar BL, Petersen SE. Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion. Neuroimage. 2012;59:2142–54.
Pang Y, Chen H, Wang Y, Long Z, He Z, Zhang H, et al. Transdiagnostic and diagnosis-specific dynamic functional connectivity anchored in the right anterior insula in major depressive disorder and bipolar depression. Prog Neuropsychopharmacol Biol Psychiatry. 2018;85:7–15.
Pang Y, Zhao S, Li Z, Li N, Yu J, Zhang R, et al. Enduring effect of abuse: childhood maltreatment links to altered theory of mind network among adults. Hum Brain Mapp. 2022;43:2276–88.
Batista GE, Prati RC, Monard MC. A study of the behavior of several methods for balancing machine learning training data. ACM SIGKDD Explor Newsl. 2004;6:20–9.
Schmahmann JD. Disorders of the cerebellum: ataxia, dysmetria of thought, and the cerebellar cognitive affective syndrome. J Neuropsychiatry Clin Neurosci. 2004;16:367–78.
Buckner RL, Krienen FM, Castellanos A, Diaz JC, Yeo BT. The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106:2322–45.
Buckner RL. The cerebellum and cognitive function: 25 years of insight from anatomy and neuroimaging. Neuron. 2013;80:807–15.
Lugo-Candelas C, Cha J, Hong S, Bastidas V, Weissman M, Fifer WP, et al. Associations between brain structure and connectivity in infants and exposure to selective serotonin reuptake inhibitors during pregnancy. JAMA Pediatr. 2018;172:525–33.
Depping MS, Schmitgen MM, Kubera KM, Wolf RC. Cerebellar contributions to major depression. Front Psychiatry. 2018;9:634.
Xu L, Xu F, Liu C, Ji Y, Wu J, Wang Y, et al. Relationship between cerebellar structure and emotional memory in depression. Brain Behav. 2017;7:e00738.
Lan Z, Zhang W, Wang D, Tan Z, Wang Y, Pan C, et al. Decreased modular segregation of the frontal–parietal network in major depressive disorder. Front Psychiatry. 2022;13:929812.
Depping MS, Schmitgen MM, Bach C, Listunova L, Kienzle J, Kubera KM, et al. Abnormal cerebellar volume in patients with remitted major depression with persistent cognitive deficits. Cerebellum. 2020;19:762–70.
Wise T, Radua J, Via E, Cardoner N, Arnone D. Common and distinct patterns of grey matter volume alteration in major depression and bipolar disorder: evidence from voxel-based meta-analysis. Mol Psychiatry. 2016;22:1455–63.
Depping MS, Nolte HM, Hirjak D, Palm E, Hofer S, Stieltjes B, et al. Cerebellar volume change in response to electroconvulsive therapy in patients with major depression. Prog NeuroPsychopharmacol Biol Psychiatry. 2017;73:31–5.
Fu Z, Abbott CC, Miller J, Deng Z-D, McClintock SM, Sendi MS, et al. Cerebro-cerebellar functional neuroplasticity mediates the effect of electric field on electroconvulsive therapy outcomes. Transl Psychiatry. 2023;13:43.
Liu W, Yan H, Zhou D, Cai X, Zhang Y, Li S, et al. The depression GWAS risk allele predicts smaller cerebellar gray matter volume and reduced SIRT1 mRNA expression in Chinese population. Transl Psychiatry. 2019;9:333.
Xu P, Chen A, Li Y, Xing X, Lu H. Medial prefrontal cortex in neurological diseases. Physiol Genomics. 2019;51:432–42.
Krienen FM, Buckner RL. Segregated fronto-cerebellar circuits revealed by intrinsic functional connectivity. Cereb Cortex. 2009;19:2485–97.
Habas C, Kamdar N, Nguyen D, Prater K, Beckmann CF, Menon V, et al. Distinct cerebellar contributions to intrinsic connectivity networks. J Neurosci. 2009;29:8586–94.
Buckner RL, DiNicola LM. The brain’s default network: updated anatomy, physiology and evolving insights. Nat Rev Neurosci. 2019;20:593–608.
Ding Y, Ou Y, Yan H, Fu X, Yan M, Li H, et al. Disrupted cerebellar-default mode network functional connectivity in major depressive disorder with gastrointestinal symptoms. Front Cell Neurosci. 2022;16:833592.
Anteraper SA, Guell X, Lee YJ, Raya J, Demchenko I, Churchill NW, et al. Cerebello-cerebral functional connectivity networks in major depressive disorder: A CAN-BIND-1 study report. Cerebellum. 2023;22:26–36.
Wang X, Xia J, Wang W, Lu J, Liu Q, Fan J, et al. Disrupted functional connectivity of the cerebellum with default mode and frontoparietal networks in young adults with major depressive disorder. Psychiatry Res. 2023;324:115192.
Guo W, Liu F, Xue Z, Gao K, Liu Z, Xiao C, et al. Abnormal resting-state cerebellar–cerebral functional connectivity in treatment-resistant depression and treatment sensitive depression. Prog Neuropsychopharmacol Biol Psychiatry. 2013;44:51–7.
Zhu D-M, Yang Y, Zhang Y, Wang C, Wang Y, Zhang C, et al. Cerebellar-cerebral dynamic functional connectivity alterations in major depressive disorder. J Affect Disord. 2020;275:319–28.
Lin H, Xiang X, Huang J, Xiong S, Ren H, Gao Y. Abnormal degree centrality values as a potential imaging biomarker for major depressive disorder: a resting-state functional magnetic resonance imaging study and support vector machine analysis. Front Psychiatry. 2022;13:960294.
Liu F, Guo W, Yu D, Gao Q, Gao K, Xue Z, et al. Classification of different therapeutic responses of major depressive disorder with multivariate pattern analysis method based on structural MR scans. PLoS ONE. 2012;7:e40968.
Beckmann FE, Seidenbecher S, Metzger CD, Gescher DM, Carballedo A, Tozzi L, et al. C-reactive protein is related to a distinct set of alterations in resting-state functional connectivity contributing to a differential pathophysiology of major depressive disorder. Psychiatry Res Neuroimaging. 2022;321:111440.
Acknowledgements
The authors thank all the patients and the healthy volunteers who participated in this study. Thanks to my colleagues for their help in this study. This work was supported by the Natural Science Foundation of China (62103377, 62303423), the STI 2030-Major Project (2022ZD0208500), the Provincial and Ministry Co-construction Funds of Henan Provincial Health Commission (SB201901012), the Youth Project of Provincial and Ministry Co-construction Funds of Henan Provincial Health Commission (SBGJ202403022, SBGJ202103048), the Science and Technology Project of Henan Province (252102311096, 222102310205), the Key Scientific Research Program of the Higher Education Institutions of Henan Province (22A416013), and the Postdoctoral Science Foundation of China (2023M733245, 2024T170844).
Author information
Authors and Affiliations
Contributions
JYP conceived and designed the experiments, data curation, and writing original draft; HMT and YC perfected the MRI; LC, CXS, and JH collected and organized clinical and laboratory data; JYX, ZYZ, LYG, RZ, and GL managed and analyzed the data; YJP conceived and designed the experiments, review/editing; HFL conceived and designed the experiments, review/editing, supervision and resource. All authors contributed to and have approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pang, J., Xu, J., Chen, L. et al. Family history, inflammation, and cerebellum in major depression: a combined VBM and dynamic functional connectivity study. Transl Psychiatry 15, 188 (2025). https://doi.org/10.1038/s41398-025-03409-0
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03409-0
This article is cited by
-
Cerebellar astrocytic alterations in depression
Translational Psychiatry (2026)
-
Multivariate associations of motor performance, sleep quality, depressive symptoms, and grey matter volume in younger and mid-to-older adults
Scientific Reports (2026)
-
Nuclear Medicine in Depression: Insights into Brain Metabolism and Treatment Responses: a Literature Review
Nuclear Medicine and Molecular Imaging (2025)