Abstract
The COVID-19 pandemic has posed an unprecedented threat to global health. However, neural substrates underlying mental health vulnerabilities brought by the pandemic remain elusive. We conducted a systematic review relating structural and functional brain abnormalities to mental health issues associated with COVID-19 at brain regional and network levels. A literature search on neuroimaging studies of mental health problems derived by COVID-19 was conducted in the PubMed, Web of Science and MEDLINE databases. We identified 46 studies across various imaging techniques and found that COVID-19-related mental health problems were principally associated with brain structural and functional alterations in the prefrontal cortex, insula, cingulate, hippocampus, and amygdala, as well as the affective cortical network. This review may facilitate the targeted development of therapies tailored to the pandemic context and provide insights for proactive prevention against future collective stressors and traumas.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has had profound global public health effects after its initial outbreak in late 2019 [1]. In addition to the direct health impacts caused by the infection, associated preventive measures disrupted daily routines and hindered social processes, leaving people in a state of uncertainty, shock, fear and helplessness [2,3,4]. The fear of the virus itself, coupled with sudden changes in the social environment and economic pressures, has made a subset of individuals prone to mental health problems, including negative emotions such as anxiety and depression symptoms, decreased cognitive performance, poor sleep quality, and post-traumatic stress symptoms [5, 6]. Consequently, a number of studies have focused on the psychosocial implications of the pandemic [7, 8], and individual differences in psychological reactivity to prolonged exposure to the stress imposed by the pandemic [9].
To identify individuals susceptible to mental health issues arising from stressors such as the COVID-19 pandemic, some researchers are applying neuroimaging tools to investigate and validate biomarkers that characterize the brain’s stress response [10]. Indeed, neuroimaging has been widely used in clinical psychology and psychiatry research as a non-invasive technique for exploring brain mechanisms and determining biomarkers of mental health [11,12,13]. Researchers have used imaging methods such as structural magnetic resonance imaging (sMRI), functional MRI (fMRI), and electroencephalography (EEG) to explore the neural mechanisms at the level of brain regions, connectivity and large-scale networks in the context of mental health problems arising during the COVID-19 pandemic [14,15,16]. However, findings are heterogeneous and reliable neural signatures underlying pandemic-induced mental health problems remain elusive.
Herein, we conducted a systematic review to synthesize neuroimaging-based findings linked to various types of COVID-19-related mental health problems into a coherent framework, which may assist in identifying vulnerable individuals and implementing targeted measures pre-emptively. In particular, in this study, we focused on a large group of general population without pre-existing neurological or psychiatric disorders to ensure that the observed neural correlates were specifically driven by the psychosocial impact of the pandemic in the realm of subclinics. This enables isolation of pandemic-related neural changes from those attributable to other neurobiological abnormalities, thereby strengthening the validity of our findings regarding pandemic-specific neural mechanisms. We also hope to shed light on how to handle other major threatening life events similar to the COVID-19 pandemic in the future.
Methods
Search strategy and study selection
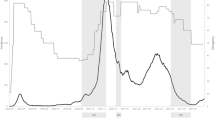
This systematic review was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17]. A systematic strategy was used to search for relevant studies published in PubMed, Web of Science and Medline up to March 19, 2025, with the following search terms: (1) COVID; coronavirus; pandemic; or SARS and (2) brain; magnetic resonance imaging; gray matter; white matter; computer tomography; electroencephalography; diffusion tensor imaging; single-photon emission computed tomography; positron emission tomography; functional near-infrared spectroscopy; MRI; CT; EEG; DTI; SPECT; PET; fNIRS; or neuroimaging and (3) mental health; psychological health; anxiety; depression; stress; PTSD; negative affect; cognition; fear; worry; distress; fatigue; burnout; or emotions. In addition, we conducted manual searches in the reference lists of the obtained articles to identify additional studies that need to be included. Details of the literature search and eligibility assessment for our analysis are shown in Fig. 1.
The inclusion criteria were as follows: (1) using self-reported or other measures for the psychosocial effects of COVID-19; (2) using neuroimaging measures and reporting findings on the brain-mental health association. Studies were excluded if they were: (1) non-English publications; (2) non-human studies; (3) literature review, meta-analysis, conference abstract, case report or letter; (4) exploring biological effects of COVID-19; (5) exclusively enrolled participants with clinically diagnosed neurological or psychiatric disorders. Two authors (Y. G. and N. P.) independently completed the screening and assessment procedures for each article to ensure their appropriateness for inclusion. Any disagreement will be mediated and a consensus was reached after discussion with a third researcher (S. W.).
To provide a detailed description of each study in the systematic review, we collected information including sample size, gender ratio, age range, neuroimaging measures, psychometric measures, and primary findings (see Tables 1, 2 and 3).
Results
Included studies and sample characteristics
A total of 6228 candidate articles were retrieved after excluding 8058 duplicates. After reviewing titles and abstracts, 4942 unrelated articles were excluded. Next, we assessed the eligibility of the remaining 1286 full-text articles. The following studies were excluded: studies without neuroimaging measures (n = 433), studies without psychometric measures (n = 45), and studies with unrelated themes (n = 762). Thus, 46 articles that met the inclusion criteria were identified in the systematic review (Fig. 1). 9 studies used sMRI to analyze the relation between COVID-19-related mental health problems and brain structure (for demographic characteristics and research details, see Table 1), 30 fMRI reports analyzed their relation to brain functional connectivity and activation (Table 2), 7 investigations used EEG, and 1 used functional near-infrared spectroscopy (fNIRS) (Table 3).
Regional-level neural substrates
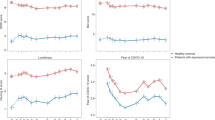
Refer to Fig. 2 for the weighted contributions of brain regional mechanisms to COVID-19-related mental health issues.
Prefrontal cortex (N = 12)
Four articles revealed the role of the lateral prefrontal cortex (PFC) in COVID-19-related mental health issues. First, in a sMRI study using the prospective cohort design, higher right lateral PFC thickness prior to the pandemic was found to be associated with worse mental health outcomes, mainly manifested as a higher risk of anxiety and depression symptoms [18]. Second, another study revealed that COVID-related vicarious traumatization exhibited a positive correlation with gray matter volume (GMV) in the right dorsolateral PFC, while a negative association with resting-state functional connectivity between the right dorsolateral PFC and right precuneus [19]. Furthermore, the right dorsolateral PFC volume and dorsolateral PFC-precuneus connectivity mediated the effect of childhood cumulative trauma on vicarious traumatization [19]. Third, a task-based fMRI research reported that the fear for infection during the pandemic was positively correlated with the right dorsolateral PFC activation patterns prior to COVID-19 during a Theory of Mind task [20]. Forth, in another task-based fMRI research, investigators found that neural response to sad faces in the right ventrolateral PFC was positively correlated with negative memory biases [21].
Several studies have also implicated the medial PFC. For example, an sMRI study found that occupational burnout of medical professionals during the COVID-19 period was negatively correlated with GMV in the ventromedial PFC [22]. Lan et al. found a positive association between post-traumatic stress symptoms during the COVID-19 period and GMV in the left medial PFC, and a negative association between post-traumatic growth and GMV in the left dorsolateral PFC [23]. Specifically, participants with lower GMV in the ventromedial PFC showed higher levels of emotional exhaustion and depersonalization, two subcomponents of burnout [22]. In a resting-state fMRI (rs-fMRI) study, compared to local students, overseas students showed significantly lower regional homogeneity (ReHo) values in left superior and medial frontal gyri, pre-central gyrus, and paracentral lobule during the COVID-19 pandemic. Importantly, these ReHo reductions showed a significant positive correlation with depressive symptoms [24]. Another rs-fMRI study showed that pre-pandemic degree centrality of the PFC (mainly the posterior orbital gyrus) was positively associated with social anxiety during the pandemic [25]. In four studies using brain functional connectivity, weaker connectivity in the PFC was associated with increased anxiety [26], depression [27], post-traumatic stress symptoms [10], and perceived stress [15].
Cingulate cortex (N = 9)
Diffusion-weighted imaging studies on cingulum fiber density and cross-section (FDC) reported different neuroimaging patterns, and after accounting for known sex differences. For example, cingulum FDC was negatively associated with depressive symptom severity during the pandemic in just females, while higher cingulum FDC predicted higher resilience and lower stress in both sexes [28]. Indeed, a positive correlation has been reported between rostral anterior cingulate cortex (ACC) thickness and “tension” symptoms in individuals with low maladaptive coping [14]. Similarly, two sMRI studies found a positive association between GMV in the dorsal ACC and post-traumatic stress symptoms during the pandemic and a negative association between GMV of the dorsal ACC extending to the dorsal medial PFC and the optimism score [23, 29]. Further seed-based structural covariance network (SCN) analysis found an optimism-linked SCN covarying with the combined dorsal ACC and dorsal medial PFC. Additionally, optimism mediated the impact of dorsal ACC-dorsal medial PFC volume and its SCN on COVID-19-specific posttraumatic stress symptoms [29]. In task-based fMRI using sad faces, neural responses in the bilateral dorsal ACC have been positively associated with negative memory biases, and negatively associated with future depressive symptoms during the COVID-19 pandemic [21]. Three functional connectivity studies have shown that there are nodes in the ACC that play a significant role in COVID-19-related anxiety [26, 30] and post-traumatic stress symptoms [10] respectively, while another one suggested that node strength in the posterior cingulate cortex (PCC) is associated with COVID-19-related depression symptoms [27].
Insula (N = 6)
Two studies have revealed that anxiety induced by COVID-19 is related to pre-pandemic reduced insula thickness [14] and weaker connectivity from insula [26]. Two other functional studies focused on COVID-19-related depressive symptoms: one rs-fMRI study exhibited that the nodes strength located in the right insular can predict depression during the pandemic [27]; a task-based fMRI study found that adolescent girls with high shy/fearful temperaments showed negative associations between insula activation to social reward and COVID-19 depressive symptoms, whereas girls with lower shy/fearful temperament showed positive associations [31]. In addition, in a task-based fMRI study, greater anterior insula activation to unpredictable shock (U-threat) was associated with greater COVID-related negative affect [32]. Finally, levels of emotional exhaustion in medical professionals were negatively correlated with GMV in the left insula [22].
Temporoparietal regions (N = 7)
One sMRI study found that the GMV in the right supramarginal gyrus might be positively associated with social anxiety symptoms during the pandemic [33]. An rs-fMRI revealed that enhanced pre-COVID neural activity (measured by fractional amplitude of low-frequency fluctuation, fALFF) in the right fusiform gyrus could predict severe COVID-related post-traumatic stress symptoms and social anxiety during the pandemic, and the COVID-related post-traumatic stress symptoms may serve as mediators [34]. One investigation reported that the mother’s subjective burden of care increased during the pandemic, and the higher right temporoparietal junction activation during Theory of Mind task preceded a higher subjective burden [20]. A prospective longitudinal study found that pre-pandemic measures of functional connectivity could predict post-traumatic stress symptoms, and its neural connectome was mainly anchored on the temporoparietal junction [10]. Further, Mao et al. found that weaker connectivity stemming from the right inferior temporal gyrus was associated with depression during the COVID-19 pandemic [27]. In a study aimed to identify the functional connectome that encodes individual variations of pandemic-related vicarious traumatization, only the negative network model stably predicted individuals’ vicarious traumatization scores, with the contributing connected nodes primarily distributed in the bilateral angular gyrus and inferior temporal gyrus, right temporal pole, fusiform gyrus [35]. Similarly, the nodes that play a key role in predicting the individual perceived stress level during the pandemic were located in the bilateral precuneus, right middle temporal gyrus, and left inferior temporal gyrus [15].
Subcortical regions (N = 11)
Three resting-state fMRI studies have respectively proven that hub nodes related to anxiety are located in the thalamus, hippocampus, and parahippocampal gyrus [26], nodes related to post-traumatic stress symptoms are located in the hippocampus and amygdala [10], and nodes that play a key role in predicting individual perceived stress levels are located in the parahippocampal gyrus [15]. Task-based fMRI paradigms showed that higher activation of the left amygdala during fearful faces before the pandemic was related to greater internalizing problems during the pandemic [36]. The hippocampus has been considered the most critical hub region in predicting the emergence of distress after COVID-19 [37], while the node that exerts a critical role in predicting depression during the COVID-19 pandemic has been located in the thalamus [27]. Girls with high levels of shy/fearful temperament showed negative associations between caudate and putamen activation to social reward and COVID-19 depressive symptoms, whereas girls lower in shy/fearful temperament showed positive associations [31]. In a passive avoidance task, lower expected value signaling in the right nucleus accumbens predicted higher withdrawn symptoms throughout the pandemic [38]. Hardi et al. identified a distinct neural network variation associated with greater anxiety symptoms during the COVID-19 pandemic, characterized by more connections involving the left amygdala and ventral striatum [30]. Morphologically, higher levels of depersonalization (a dimension of occupational burnout) were related to the lower GMV in the left thalamus [22]. Another sMRI study revealed that there was a negative correlation between amygdala volume and anhedonia symptoms in individuals with high maladaptive coping [14].
Network-level neural substrates
Refer to Fig. 3 for the weighted contributions of large-scale brain network mechanisms to COVID-19-related mental health issues.
Affective cortical network (AFN, N = 10)
Perica et al found that greater connectivity within the AFN (mainly between anterior ventromedial PFC and posterior hippocampus) predicted greater COVID-19-related stress in youth under 18 years old [39]. Perceived stress is also related to weaker connectivity between AFN and two other networks [DMN and visual network (VN)] [15]. Additionally, Pan et al. identified an anxiety-related mode characterized by high loadings in connectivity between the AFN and VN when exploring the multivariate patterns of brain functional connectome predicting COVID-19-related negative affect symptoms [40]. Higher AFN system segregation (SyS, a graph-theoretical parameter to quantify the balance between within- and between-network integration and represent efficient functioning of the network, which is formally calculated as the difference between the mean magnitudes of between-system correlations from the within-system correlations as a proportion of mean within-system correlation [41]) could increase the effect of coping strategies that regulate COVID-19-related perceived stress, anxiety and depression symptoms [42]. Using rs-fMRI analyses, one study found that fear symptoms and their severity during the COVID-19 pandemic were associated with stronger connectivity within the AFN and between AFN and salience network (SN) [43]. COVID-19-related depressive symptoms have been associated with weaker connectivity within the AFN [27] and between the AFN and VN, especially between the left amygdala and the bilateral lingual gyrus [44]. In another study, stronger AFN-SN connectivity (mainly the basolateral amygdala–subgenual ACC connectivity) was associated with heightened depressive symptoms in adolescents, both before and during the pandemic [45]. Some investigators have reported that pre-pandemic measures of functional connectivity between AFN and SN can predict COVID-19-related post-traumatic stress symptoms [10]. However, an fMRI region of interest (ROI) analysis failed to find any significant association between depression or anxiety symptoms during the pandemic and AFN functional connectivity [46].
Central executive network (CEN, N = 4)
One study reported that higher CEN-SyS levels enhance the positive association between perceived stress and anxiety and depression symptoms during the COVID-19 pandemic [42], and another showed that lower pre-pandemic CEN coherence predicted more severe internalizing symptoms during the pandemic in early-maturing youths [47]. An investigation reported an association between COVID-19 vicarious traumatization and lower connectivity within the CEN pre-pandemic [35]. Researchers also found weaker local connections within the CEN in participants with post-traumatic stress symptoms compared to those without such symptoms during the COVID-19 pandemic [10].
Default mode network (DMN, N = 6)
Higher levels of DMN-SyS were found to attenuate the positive association between perceived stress and anxiety and depression symptoms during the COVID-19 pandemic [42]. Further, a connectome-based predictive modeling analysis showed that the negative DMN model stably predicted individuals’ COVID-19 vicarious traumatization. Mediation analysis revealed that this vicarious traumatization mediated the influence of DMN on general distress [35]. Another rs-fMRI study also found that lower connectivity between inferior temporal gyrus and the DMN predicted worse vicarious traumatization during the pandemic [48]. Pan et al. found that the weaker connections within DMN and between network connections of AFN-DMN and dorsal attention network-DMN predicted more severe distress symptoms during the pandemic [37]. An fMRI study investigating the multivariate patterns of brain functional connectome in predicting COVID-19-related negative affect symptoms revealed that connectivity of the DMN with dorsal attention network were remarkably prominent in mode stress [40]. In addition, it was reported that functional connectivity between the DMN and SMN/attention networks was decreased during the pandemic. And the absolute values of the DMN-SMN connectivity changes showed a negative correlation with the improvement in stress, anxiety, depression, and negative affect symptoms (positive correlation with improvement in positive affect symptoms), while the absolute values of the DMN-attention network connectivity changes showed a negative correlation with the improvement in mental status measurements in stress, anxiety, and depression [49].
Salience network (SN, N = 4)
Lower connectivity within the SN may predict COVID-19-related vicarious traumatization [35]. Further, depression during the COVID-19 pandemic is associated with weaker intrinsic connectivity within the SN [27]. Higher connectivity within the SN and between the SN and two other networks (DMN and CEN) are associated with less negative emotions during and after COVID-19. Further, the buffering effect of these functional networks was stronger in the context of higher levels of social support [50]. Similarly, Hu et al. found that higher resilience of the SN predicted better mental health during the COVID-19. Further, lower connectivity of left SN, reward, limbic, and PFC and its thalamic, striatal, amygdala connections, predicted higher stress and sadness. And lower bilateral robustness (higher fragility) and/or connectivity of these networks predicted higher sadness [51].
Sensorimotor network (SMN, N = 1)
COVID-19 vicarious traumatization was associated with weaker connectivity of the motor network, and mediation analysis indicated that this vicarious traumatization mediated the influence of the motor network on general distress [35].
Other studies
EEG (N = 7)
Compared to pre-pandemic controls, who completed two test sessions of EEG recording and cognitive tasks before the pandemic, participants during the pandemic who completed a second testing session of EEG recording and cognitive tasks during lockdown, were characterized by higher extraversion (tested by self-reported measures before the pandemic), improved cognitive performance and stronger EEG brain global connectivity. Importantly, stronger EEG connectivity and higher extroversion was inferred as a potential defense mechanism against stress-related deterioration of cognitive functions [52]. Among COVID-19 frontline healthcare professionals, reduced cognitive performance and poorer sleep quality was related to higher theta relative power, lower peak alpha frequency, and higher interhemispheric coherence of both alpha and theta rhythms [53]. In one event-related potential (ERP) study, greater COVID-19-related depressive symptoms were associated with reduced late positive potentials (LPPs) while viewing pleasant interpersonal images. In another study, enhanced LPPs while viewing threatening interpersonal images predicted increases in traumatic intrusions after the outbreak of COVID-19 [16]. Interactions between anxiety and LPPs recorded during passively viewing task of affective pictures could predict pandemic-related post-traumatic stress symptoms: greater anxiety symptoms predicted post-traumatic stress symptoms specifically in individuals with greater LPPs to unpleasant stimuli and with reduced LPPs to pleasant stimuli [54]. In two other publications using ERP analyses, larger pre-pandemic error-related negativity (ERN) and correct-response negativity (CRN) amplitudes were associated with increased perceived internalizing symptoms [55, 56]. Specifically, enhanced delta-ERN predicted greater anxiety among adolescents with an increased reliance on reactive control [55]. Further, pre-pandemic ERN and CRN correlated with increased perceived risk regarding a COVID-19 infection and increased stress during the pandemic, which mediated indirect effects of ERN and CRN on internalizing psychopathology, including anxiety, depression, and obsessive-compulsive symptoms [56]. Finally, EEG response to transcranial magnetic stimulation (TMS) could predict an individual’s capacity to resist COVID-19-related psychological stress, where larger late EEG responses locally post-left dorsolateral PFC stimulation predicted increased mental distress [57].
Functional near-infrared spectroscopy (fNIRS, N = 1)
One publication using fNIRS reported that the reduced hemodynamic response of the PFC is associated with negative emotions, especially anxiety, during the COVID-19 lockdown, but immediate music stimulation alleviated those negative emotions by altering connectivity patterns in the PFC [58].
Discussion
To our knowledge, this is the first systematic review examining neural substrates of COVID-related psychosocial impact. Despite some discrepancies in results between studies, our study shows that COVID-related mental health problems are mainly associated with brain structural and functional patterns in the PFC, insula, cingulate, hippocampus, and amygdala, as well as AFN at the brain-network level. These findings provide insights about the neural basis of adverse psychological issues triggered by COVID-19, which may provide inform the development of non-invasive clinical interventions. Below, we will discuss our results briefly, integrating the brain regional findings into a framework of large-scale network systems that may be relevant to pandemic-related mental health impact.
The AFN mainly includes the amygdala and ventromedial PFC, which widely participates in engendering and regulating vigilance and arousal responses to biologically salient stimuli [59, 60]. The structural and functional changes within the AFN may be associated with symptoms such as reactive aggression, anger, and irritability [61, 62] and manifest in mood and personality disorders [63,64,65]. The amygdala is widely known to generate negative and unpleasant emotions, especially fear, and in associating environmental stimuli with emotionally charged and aversive sensory inputs [66]. Long term chronic stress partially mediates changes in amygdala neuron excitability through potassium channel function, which may lead to overactivity of circuits related to fear and anxiety, and reduce the ability of other regions involved in fear inhibition, such as the hippocampus and medial PFC, to dampen amygdala output [67]. The unprecedented uncertainty of the COVID-19 infection and enforced quarantine [7] likely increased the risk of stress activation processing. During the COVID-19 pandemic, weaker AFN connectivity was associated with the negative emotions (perceived stress, anxiety and depression) [27, 40, 42]. However, Perica et al. found the opposite: the higher connectivity within AFN predicted greater COVID-19-related stress [39]. In addition, the inter-connections between AFN and other networks were also involved in regulating negative emotions. Specifically, weaker AFN-DMN and AFN-VN connectivity respectively predicted more severe perceived stress and depression symptoms during the COVID-19 pandemic [15, 44], while the AFN-SN and AFN-VN connectivity was positively correlated with depressive and anxiety symptoms, respectively [40, 45]. Meanwhile, dysregulated interaction between AFN and SN was also associated with COVID-19-related fear and PTSD symptoms [10, 43]. For example, higher bottom-up arousal signaling from amygdala, insula, ACC, and thalamus could increase the susceptibility of negative emotions to COVID-19 [68,69,70], whereas the stronger top-down control by the PFC of these subcortical regions could inverse this process [71].
The CEN, mainly consisting of the dorsolateral PFC and posterior parietal cortex [72], is crucial for the cognitive regulation of emotion, behavior, and thought, especially activating in efforts to exert self-control, reassess threatening stimuli, and suppress invasive and unpleasant thoughts [73,74,75]. The deficits in these processes are often characteristics of multiple adverse mental health outcomes [76,77,78]. The dorsolateral PFC is a well-recognized cognitive control region that subserves inhibitory control, cognitive flexibility, and working memory [79], especially the right dorsolateral PFC is involved in the downregulation of negative emotional conditions [80]. COVID-related vicarious traumatization is associated with dorsolateral PFC GMV and connectivity, which is broadly consistent with a previous study showing that trauma-exposed individuals had greater dorsolateral PFC thickness relative to controls over a year after trauma, and greater dorsolateral PFC thickness was associated with greater post-traumatic stress symptoms reductions and better recovery [81]. Therefore, it can be inferred that a larger dorsolateral PFC GMV may facilitate better management and suppression of distressing memories and emotions, which are more frequently arised from witnessing others’ traumatic experiences in these individuals. One task-based emotion regulation fMRI study showed that lateral PFC activity was associated with greater stress reduction in participants with elevated trait anxiety scores, suggesting that lateral PFC dysfunction may be associated with psychiatric symptoms that manifest dysfunctional down-regulation of negative emotion and excessive fluctuation of emotions [82]. Similarly, research from the COVID-19 pandemic also confirmed that abnormalities in lateral PFC contributed to robust predictive markers of during-pandemic negative mental health symptoms [10, 18, 20, 21]. Deficits in the CEN, including weaker intrinsic connectivity within its nodes, aberrant cross-network connectivity patterns, or impaired access to salient task-relevant stimuli, have all been reported in psychiatric disorders such as depression, schizophrenia and autism [83,84,85]. Similarly, lower CEN coherence has also been associated with severe mental health problems during the COVID-19 pandemic period [10, 35, 47].
The DMN is a large-scale brain network identified in this review to be associated with severe mental symptoms during the COVID-19 pandemic. As this review summarizes, DMN plays a crucial role in attenuating the positive association between perceived stress and anxiety/depression symptoms, predicting vicarious traumatization, and influencing general distress during the COVID-19 pandemic [30, 32, 34, 40]. Additionally, the functional connectivity between the DMN and other networks (e.g. the SMN and attention network) is also involved in the impact of COVID-19-related negative mental status from the prolonged isolation, reduced physical and social activities [49]. This is in line with prior research on neural correlates of broad psychological impairments [86, 87]. DMN dysfunction has been recognized as a critical biomarker in various psychiatric disorders involving disrupted self-referential processing, such as PTSD [88], depression [83], anxiety [89], and schizophrenia [90]. Concerning DMN’s components, the medial PFC subsystem plays an important role in regulating emotion and stress responses [85, 86, 91]. Medial PFC impairment may be associated with anxiety and PTSD through impaired fear memory regulation [92], which could be exacerbated by pandemic-related stressors. The dorsomedial PFC is instrumental in mentalizing and metacognitive processing [93], and its hyperactivity coincides with rumination, a core symptom of major depressive disorder [94]. The hippocampus, another key region of the DMN, is crucial for cognitive functioning and the regulation of stress and emotion [95, 96]. Besides being generally regarded as a major target of stress mediators [97], the hippocampus is also involved in the extinction of fear memories, and lesions in the hippocampus may be associated with extinction deficits in PTSD [97]. Reduced activation of brain regions of DMN (including medial PFC, PCC, posterior inferior parietal lobule, and the parahippocampal gyrus), as well as decreased functional connectivity within DMN nodes (including the PCC, posterior hippocampus and ventromedial PFC), have been reported in PTSD patients [98, 99]. A decrease in DMN coherence is also believed to be the basis for impairments in self-referential processes, autobiographical memory and altered sense of self in PTSD patients [88]. Altogether, individuals with weaker connections of DMN are more likely to experience mental distress, especially during the period of the COVID-19 pandemic with a high risk of stress [35, 37, 42].
The SN, anchored in the ACC and insular cortex, is responsible for detecting, integrating, and filtering relevant interoceptive, autonomic and emotional information [72]. Reduced volumetric patterns of ACC might represent a biomarker of depression and predict long-term prognosis [100, 101]. Existing evidence has demonstrated that the dorsal ACC strongly communicates with dorsomedial PFC in the process of emotion regulation, especially in regulating negative emotions, such as fear and anxiety [102, 103]. Dysfunctional increasing neural activity in the dorsal ACC and dorsomedial PFC potentially leads to severe anxiety symptoms and even major depressive disorders [102, 104]. The indirect connection from ACC and the PFC to the amygdala through a top-down inhibitory pathway contributes to the assessment, acquisition, and cognitive regulation of fear [105]. An increase in the strength of connectivity between the amygdala-ACC and dorsolateral PFC may be related to increased fear processing function and PTSD symptoms [106]. As for the insular section of SN, disturbances including those related to several sensory and multimodal perceptions, as well as body awareness, the emotion of disgust, mood and willed action, may all appear following insular damage [107]. Insular activation patterns might also serve as a focal point in addressing the mental health challenges arising from the pandemic given their involvement in processing aversive interoceptive stimuli and altered prediction of an aversive body state that may trigger an increase in anxious and worrisome thoughts in individuals prone to anxiety symptoms [108]. The anterior insula plays a key role in the anticipation and emotional experience of aversive stimuli, and participates in the allocation of attention and initiation of appropriate action through the ACC [109]. Patients with generalized anxiety disorder have shown reduced insula activation after taking anti-anxiety drug citalopram to reduce worry symptoms [110]. The SN plays a dynamic switching role between self and inner world attention mediated by the DMN and task-related directed attention of outside stimuli maintained by the CEN [111]. This may explain the findings that individuals with higher SN-DMN and SN-CEN connectivity exhibited less negative emotions during and after the COVID-19 pandemic [50]. Overall, strength and robustness of the SN prior to the pandemic may have been a protective factor for mental health, whereas its fragility and weaker connections were risk factors that increased vulnerability to the pandemic’s adverse effects.
Quantitative parameter analysis of EEG signals could evaluate altered rhythms that are related to mental health [112, 113]. Higher theta relative power and lower peak alpha frequency during COVID-19 in frontline healthcare workers were associated with experiences of increased work stress, reduced cognitive performance, and poor sleep quality [53]. Theta waves are commonly present in EEG images during trance or hypnotic states and excessive theta activity may indicate depression, while low alpha frequency may indicate greater stress or anxiety [114, 115]. EEG also reflects brain functional connectivity and quantifies the interactions between different neuronal networks [116]. Overall, stronger EEG connectivity during the pandemic may have served as a protective mechanism to prevent stress-related cognitive deterioration [52]. The LPPs, as a neurophysiological measure of emotional reactivity, have sensitivity to discriminate emotional relative to neutral cues [117]. Specifically, reduced LPPs to positive stimuli were found in individuals at risk for depression [118], while elevated LPPs, generally to negative or threatening stimuli, were recorded in individuals at risk for anxiety [119, 120]. Therefore, LPPs may be a potential signal to reflect mental health during COVID-19 period. TMS interferes with ongoing brain activity by suddenly injecting a certain amount of current into the neural circuit, resulting in phase reset and being recorded by EEG [121]. Therefore, EEG quantification of TMS response could be used to track an individual’s capacity to resist COVID-19-related psychological stress [57]. Finally, fNIRS, with the advantages of relatively high spatial and temporal resolution and better comfort, may indirectly monitor brain activity by measuring changes in oxyhemoglobin and deoxyhemoglobin concentrations in cerebral blood vessels [122]. A study using fNIRS analysis revealed the relationship between the reduced hemodynamic response of the PFC and negative emotions during the pandemic [58], illustrating its potential utility as a tool to track neuropsychiatric symptoms.
There are several limitations of our systematic review. First, the imaging modalities used in the literature are mostly fMRI and EEG. It is well known that fMRI exhibits notable spatial resolution, but poor temporal resolution, while EEG does the opposite [123]; simultaneous EEG and fMRI, to bridge the high temporal resolution of EEG and the high spatial resolution of fMRI, could be a promising research approach in the future. In addition, other imaging technologies, such as positron emission tomography (PET), which can quantify brain metabolic information [124], has not been applied to relevant research. Second, many psychometric measures in research rely on participants self-administered questionnaires, introducing a notable degree of subjectivity into the obtained results; future studies that combine self-reports with biological and validated clinical and neuropsychological tests could improve objectivity. Third, the sample of participants across studies varied widely in terms of sociodemographic characteristics, and the primary psychological outcomes measured, the imaging modalities, the assessment tools and analysis protocols were highly heterogeneous across studies. This heterogeneity hindered the comparability of findings and synthesis of results. With more studies using more standard measures, quantitative meta-analysis could be conducted. Forth, this review primarily focuses on elucidating neural mechanisms underlying COVID-19-related mental health issues. While these findings provide important mechanistic insights, we recognize the current limitations in direct clinical application, highlighting the need for future translational studies to bridge this gap. Finally, it is recommended that future studies should incorporate large and diverse samples of well-characterized participants (i.e., frontline healthcare workers and other vulnerable samples), contributing to more reliability and validity of the subject matter.
Conclusion
The COVID-19 pandemic caused tremendous harm to human health, including an unprecedented threat to mental health in various populations. To our knowledge, this is the first systematic review of neuroimaging applications aimed to characterize neural features associated with adverse mental symptoms related to the COVID-19 pandemic. Our study identified how COVID-19 related-mental health problems are linked to specific brain regions and networks, principally including the PFC, insula, cingulate, hippocampus, amygdala and AFN. Our findings may serve as a foundation to effectively address the acute stress-related effects of the pandemic, and may also provide insights for proactively preventing adverse mental symptoms in individuals during future large-scale stressful events.
References
Lee K, Jeong GC, Yim J. Consideration of the psychological and mental health of the elderly during COVID-19: a theoretical review. Int J Environ Res Public Health. 2020;17:8098.
Zhang JJ, Dong X, Liu GH, Gao YD. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. 2023;64:90–107.
Hossain MM, Tasnim S, Sultana A, Faizah F, Mazumder H, Zou L, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636.
Zaami S, Sirignano A, García-Algar Ó, Marinelli E. COVID-19 pandemic, substance use disorders and body image issues, a worrisome correlation. Eur Rev Med Pharmacol Sci. 2022;26:291–7.
Chen PJ, Pusica Y, Sohaei D, Prassas I, Diamandis EP. An overview of mental health during the COVID-19 pandemic. Diagnosis (Berl). 2021;8:403–12.
Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav Immun. 2020;89:531–42.
Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–20.
Raza SH, Haq W, Sajjad M. COVID-19: A Psychosocial Perspective. Front Psychol. 2020;11:554624.
Zhang J, Lu H, Zeng H, Zhang S, Du Q, Jiang T, et al. The differential psychological distress of populations affected by the COVID-19 pandemic. Brain Behav Immun. 2020;87:49–50.
Chen Z, Feng P, Becker B, Xu T, Nassar MR, Sirois F, et al. Neural connectome prospectively encodes the risk of post-traumatic stress disorder (PTSD) symptom during the COVID-19 pandemic. Neurobiol Stress. 2021;15:100378.
Moran JM, Zaki J. Functional neuroimaging and psychology: what have you done for me lately? J Cogn Neurosci. 2013;25:834–42.
Jensen CD, Duraccio KM, Carbine KM, Kirwan CB. Topical review: unique contributions of magnetic resonance imaging to pediatric psychology research. J Pediatr Psychol. 2016;41:204–9.
Ma Y, Zou Y, Liu X, Chen T, Kemp GJ, Gong Q, et al. Social intelligence mediates the protective role of resting-state brain activity in the social cognition network against social anxiety. Psychoradiology. 2024;4:kkae009.
Holt-Gosselin B, Tozzi L, Ramirez CA, Gotlib IH, Williams LM. Coping strategies, neural structure, and depression and anxiety during the COVID-19 pandemic: a longitudinal study in a naturalistic sample spanning clinical diagnoses and subclinical symptoms. Biol Psychiatry Glob Open Sci. 2021;1:261–71.
Liu P, Yang W, Zhuang K, Wei D, Yu R, Huang X, et al. The functional connectome predicts feeling of stress on regular days and during the COVID-19 pandemic. Neurobiol Stress. 2021;14:100285.
Dickey L, West M, Pegg S, Green H, Kujawa A. Neurophysiological responses to interpersonal emotional images prospectively predict the impact of COVID-19 pandemic-related stress on internalizing symptoms. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:887–97.
Moher D, Liberati A, Tetzlaff J, Altman DG, P. Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097.
Dimanova P, Borbás R, Schnider CB, Fehlbaum LV, Raschle NM. Prefrontal cortical thickness, emotion regulation strategy use and COVID-19 mental health. Soc Cogn Affect Neurosci. 2022;17:877–89.
Liu X, Zhao Y, Li J, Suo X, Gong Q, Wang S. Brain structure and functional connectivity linking childhood cumulative trauma to COVID-19 vicarious traumatization. J Child Psychol Psychiatry. 2024;65:1407–18.
Borbás R, Fehlbaum LV, Dimanova P, Negri A, Arudchelvam J, Schnider CB, et al. Mental well-being during the first months of Covid-19 in adults and children: behavioral evidence and neural precursors. Sci Rep. 2021;11:17595.
Zhang P, Piao Y, Chen Y, Ren J, Zhang L, Qiu B, et al. Outbreak of COVID-19 altered the relationship between memory bias and depressive degree in nonclinical depression. iScience. 2021;24:102081.
Abe K, Tei S, Takahashi H, Fujino J. Structural brain correlates of burnout severity in medical professionals: a voxel-based morphometric study. Neurosci Lett. 2022;772:136484.
Lan H, Suo X, Zuo C, Pan N, Zhang X, Kemp GJ, et al. Distinct pre-COVID brain structural signatures in COVID-19-related post-traumatic stress symptoms and post-traumatic growth. Cereb Cortex. 2023;33:11373–83.
Li T, Du X, Zhang X, Dong A, Yuan X, Yu T, et al. From study abroad to study at home: spontaneous neuronal activity predicts depressive symptoms in overseas students during the COVID-19 pandemic. Front Neurosci. 2023;17:1078119.
Li Q, Zhang X, Yang X, Pan N, Li X, Kemp GJ, et al. Pre-COVID brain network topology prospectively predicts social anxiety alterations during the COVID-19 pandemic. Neurobiol Stress. 2023;27:100578.
He L, Wei D, Yang F, Zhang J, Cheng W, Feng J, et al. Functional connectome prediction of anxiety related to the COVID-19 pandemic. Am J Psychiatry. 2021;178:530–40.
Mao Y, Chen Q, Wei D, Yang W, Sun J, Yu Y, et al. Resting-state functional connectome predicts individual differences in depression during COVID-19 pandemic. Am Psychol. 2022;77:760–9.
Chahal R, Ho TC, Miller JG, Borchers LR, Gotlib IH. Sex-specific vulnerability to depressive symptoms across adolescence and during the COVID-19 pandemic: The role of the cingulum bundle. JCPP Adv. 2022;2:e12061.
Lai H, Zhao Y, Li J, Gong Q, Wang S. Neuroanatomical signatures associated with dispositional optimism predict COVID-19-related posttraumatic stress symptoms. Cereb Cortex. 2023;33:9387–98.
Hardi FA, Goetschius LG, McLoyd V, Lopez-Duran NL, Mitchell C, Hyde LW, et al. Adolescent functional network connectivity prospectively predicts adult anxiety symptoms related to perceived COVID-19 economic adversity. J Child Psychol Psychiatry. 2023;64:918–29.
Sequeira SL, Silk JS, Hutchinson E, Jones NP, Ladouceur CD. Neural responses to social reward predict depressive symptoms in adolescent girls during the COVID-19 pandemic. J Pediatr Psychol. 2021;46:915–26.
Khorrami KJ, Manzler CA, Kreutzer KA, Gorka SM. Neural and self-report measures of sensitivity to uncertainty as predictors of COVID-related negative affect. Psychiatry Res Neuroimaging. 2022;319:111414.
Zhang X, Li Q, Yang X, Pan N, Suo X, He M, et al. Pre-coronavirus disease 2019 brain structure might be associated with social anxiety alterations during the pandemic. Chin Med J (Engl). 2023;136:1621–3.
Li Q, Zhang X, Yang X, Pan N, He M, Suo X, et al. Pre-COVID resting-state brain activity in the fusiform gyrus prospectively predicts social anxiety alterations during the pandemic. J Affect Disord. 2024;344:380–8.
Suo X, Zuo C, Lan H, Pan N, Zhang X, Kemp GJ, et al. COVID-19 vicarious traumatization links functional connectome to general distress. Neuroimage. 2022;255:119185.
Weissman DG, Rodman AM, Rosen ML, Kasparek S, Mayes M, Sheridan MA, et al. Contributions of emotion regulation and brain structure and function to adolescent internalizing problems and stress vulnerability during the COVID-19 pandemic: a longitudinal study. Biol Psychiatry Glob Open Sci. 2021;1:272–82.
Pan N, Qin K, Yu Y, Long Y, Zhang X, He M, et al. Pre-COVID brain functional connectome features prospectively predict emergence of distress symptoms after onset of the COVID-19 pandemic. Psychol Med. 2023;53:5155–66.
Sacu S, Dubois M, Hezemans FH, Aggensteiner PM, Monninger M, Brandeis D, et al. Early-life adversities are associated with lower expected value signaling in the adult brain. Biol Psychiatry. 2024;96:948–58.
Perica MI, Ravindranath O, Calabro FJ, Foran W, Luna B. Hippocampal-prefrontal connectivity prior to the COVID-19 pandemic predicts stress reactivity. Biol Psychiatry Glob Open Sci. 2021;1:283–90.
Pan N, Wang S, Lan H, Zhang X, Qin K, Kemp GJ, et al. Multivariate patterns of brain functional connectome associated with COVID-19-related negative affect symptoms. Transl Psychiatry. 2024;14:49.
Chan MY, Park DC, Savalia NK, Petersen SE, Wig GS. Decreased segregation of brain systems across the healthy adult lifespan. Proc Natl Acad Sci USA. 2014;111:E4997–5006.
Cabello-Toscano M, Vaqué-Alcázar L, Cattaneo G, Solana-Sánchez J, Bayes-Marin I, Abellaneda-Pérez K, et al. Functional brain connectivity prior to the COVID-19 Outbreak moderates the effects of coping and perceived stress on mental health changes: a first year of COVID-19 pandemic follow-up study. Biol Psychiatry Cogn Neurosci Neuroimaging. 2023;8:200–9.
Feng P, Chen Z, Becker B, Liu X, Zhou F, He Q, et al. Predisposing variations in fear-related brain networks prospectively predict fearful feelings during the 2019 coronavirus (COVID-19) pandemic. Cereb Cortex. 2022;32:540–53.
Zhang S, Cui J, Zhang Z, Wang Y, Liu R, Chen X, et al. Functional connectivity of amygdala subregions predicts vulnerability to depression following the COVID-19 pandemic. J Affect Disord. 2022;297:421–9.
Miller JG, Ho TC, Kirshenbaum JS, Chahal R, Gifuni AJ, Gotlib IH. Testing a developmental model of positive parenting, amygdala-subgenual anterior cingulate cortex connectivity, and depressive symptoms in adolescents before and during the COVID-19 pandemic. Biol Psychiatry Glob Open Sci. 2021;1:291–9.
Holt-Gosselin B, Cohodes EM, McCauley S, Foster JC, Odriozola P, Zacharek SJ, et al. Lack of robust associations between prepandemic coping strategies and frontolimbic circuitry with depression and anxiety symptoms during the COVID-19 pandemic: a preregistered longitudinal study. Behav Neurosci. 2022;136:528–40.
Chahal R, Kirshenbaum JS, Miller JG, Ho TC, Gotlib IH. Higher executive control network coherence buffers against puberty-related increases in internalizing symptoms during the COVID-19 pandemic. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:79–88.
Liu X, Zhao Y, Suo X, Zhang X, Pan N, Kemp GJ, et al. Psychological resilience mediates the protective role of default-mode network functional connectivity against COVID-19 vicarious traumatization. Transl Psychiatry. 2023;13:231.
Zhang Y, Guo L, Gu Z, Yang Q, Han S, Zhang H. Short-term restriction of physical and social activities effects on brain structure and connectivity. Brain Sci. 2024;15:7.
Xiao M, Chen X, Yi H, Luo Y, Yan Q, Feng T, et al. Stronger functional network connectivity and social support buffer against negative affect during the COVID-19 outbreak and after the pandemic peak. Neurobiol Stress. 2021;15:100418.
Hu L, Stamoulis C. Strength and resilience of developing brain circuits predict adolescent emotional and stress responses during the COVID-19 pandemic. Cereb Cortex. 2024;34:bhae164.
Rogala J, Dreszer J, Malinowska U, Waligóra M, Pluta A, Antonova I, et al. Stronger connectivity and higher extraversion protect against stress-related deterioration of cognitive functions. Sci Rep. 2021;11:17452.
LoMauro A, Molisso MT, Mameli F, Ruggiero F, Ferrucci R, Dellarosa C, et al. EEG evaluation of stress exposure on healthcare workers during COVID-19 emergency: not just an impression. Front Syst Neurosci. 2022;16:923576.
Dell’Acqua C, Moretta T, Dal Bò E, Messerotti Benvenuti S, Palomba D. Emotional processing prospectively modulates the impact of anxiety on COVID-19 pandemic-related post-traumatic stress symptoms: an ERP study. J Affect Disord. 2022;303:245–54.
Morales S, Zeytinoglu S, Buzzell GA, Valadez EA, Troller-Renfree SV, Bowers ME, et al. Neurocognitive profiles in adolescence predict subsequent anxiety trajectories during the COVID-19 pandemic. Biol Psychiatry Cogn Neurosci Neuroimaging. 2022;7:192–200.
Riesel A, Härpfer K, Kathmann N, Klawohn J. In the face of potential harm: the predictive validity of neural correlates of performance monitoring for perceived risk, stress, and internalizing psychopathology during the COVID-19 pandemic. Biol Psychiatry Glob Open Sci. 2021;1:300–9.
Perellón-Alfonso R, Redondo-Camós M, Abellaneda-Pérez K, Cattaneo G, Delgado-Gallén S, España-Irla G, et al. Prefrontal reactivity to TMS perturbation as a toy model of mental health outcomes during the COVID-19 pandemic. Heliyon. 2022;8:e10208.
Luo L, Shan M, Zu Y, Chen Y, Bu L, Wang L, et al. Effects of long-term COVID-19 confinement and music stimulation on mental state and brain activity of young people. Neurosci Lett. 2022;791:136922.
Pessoa L. Emotion and cognition and the amygdala: from “what is it?” to “what’s to be done?”. Neuropsychologia. 2010;48:3416–29.
Kim MJ, Loucks RA, Palmer AL, Brown AC, Solomon KM, Marchante AN, et al. The structural and functional connectivity of the amygdala: from normal emotion to pathological anxiety. Behav Brain Res. 2011;223:403–10.
Coccaro EF, McCloskey MS, Fitzgerald DA, Phan KL. Amygdala and orbitofrontal reactivity to social threat in individuals with impulsive aggression. Biol Psychiatry. 2007;62:168–78.
Buckholtz JW, Callicott JH, Kolachana B, Hariri AR, Goldberg TE, Genderson M, et al. Genetic variation in MAOA modulates ventromedial prefrontal circuitry mediating individual differences in human personality. Mol Psychiatry. 2008;13:313–24.
Etkin A, Prater KE, Schatzberg AF, Menon V, Greicius MD. Disrupted amygdalar subregion functional connectivity and evidence of a compensatory network in generalized anxiety disorder. Arch Gen Psychiatry. 2009;66:1361–72.
Marsh AA, Finger EC, Mitchell DG, Reid ME, Sims C, Kosson DS, et al. Reduced amygdala response to fearful expressions in children and adolescents with callous-unemotional traits and disruptive behavior disorders. Am J Psychiatry. 2008;165:712–20.
Erk S, Mikschl A, Stier S, Ciaramidaro A, Gapp V, Weber B, et al. Acute and sustained effects of cognitive emotion regulation in major depression. J Neurosci. 2010;30:15726–34.
Baxter MG, Murray EA. The amygdala and reward. Nat Rev Neurosci. 2002;3:563–73.
Ressler KJ. Amygdala activity, fear, and anxiety: modulation by stress. Biol Psychiatry. 2010;67:1117–9.
Suarez-Jimenez B, Albajes-Eizagirre A, Lazarov A, Zhu X, Harrison BJ, Radua J, et al. Neural signatures of conditioning, extinction learning, and extinction recall in posttraumatic stress disorder: a meta-analysis of functional magnetic resonance imaging studies. Psychol Med. 2020;50:1442–51.
Peterson A, Thome J, Frewen P, Lanius RA. Resting-state neuroimaging studies: a new way of identifying differences and similarities among the anxiety disorders? Can J Psychiatry. 2014;59:294–300.
Mulders PC, van Eijndhoven PF, Schene AH, Beckmann CF, Tendolkar I. Resting-state functional connectivity in major depressive disorder: a review. Neurosci Biobehav Rev. 2015;56:330–44.
Nicholson AA, Rabellino D, Densmore M, Frewen PA, Paret C, Kluetsch R, et al. The neurobiology of emotion regulation in posttraumatic stress disorder: Amygdala downregulation via real-time fMRI neurofeedback. Hum Brain Mapp. 2017;38:541–60.
Seeley WW, Menon V, Schatzberg AF, Keller J, Glover GH, Kenna H, et al. Dissociable intrinsic connectivity networks for salience processing and executive control. J Neurosci. 2007;27:2349–56.
Turner BM, Rodriguez CA, Liu Q, Molloy MF, Hoogendijk M, McClure SM. On the neural and mechanistic bases of self-control. Cereb Cortex. 2019;29:732–50.
Gagnepain P, Hulbert J, Anderson MC. Parallel regulation of memory and emotion supports the suppression of intrusive memories. J Neurosci. 2017;37:6423–41.
Wessing I, Rehbein MA, Postert C, Fürniss T, Junghöfer M. The neural basis of cognitive change: reappraisal of emotional faces modulates neural source activity in a frontoparietal attention network. Neuroimage. 2013;81:15–25.
Brewin CR, Gregory JD, Lipton M, Burgess N. Intrusive images in psychological disorders: characteristics, neural mechanisms, and treatment implications. Psychol Rev. 2010;117:210–32.
Banich MT, Mackiewicz KL, Depue BE, Whitmer AJ, Miller GA, Heller W. Cognitive control mechanisms, emotion and memory: a neural perspective with implications for psychopathology. Neurosci Biobehav Rev. 2009;33:613–30.
Forbes NF, Carrick LA, McIntosh AM, Lawrie SM. Working memory in schizophrenia: a meta-analysis. Psychol Med. 2009;39:889–905.
Niendam TA, Laird AR, Ray KL, Dean YM, Glahn DC, Carter CS. Meta-analytic evidence for a superordinate cognitive control network subserving diverse executive functions. Cogn Affect Behav Neurosci. 2012;12:241–68.
Leyman L, De Raedt R, Vanderhasselt MA, Baeken C. Influence of high-frequency repetitive transcranial magnetic stimulation over the dorsolateral prefrontal cortex on the inhibition of emotional information in healthy volunteers. Psychol Med. 2009;39:1019–28.
Lyoo IK, Kim JE, Yoon SJ, Hwang J, Bae S, Kim DJ. The neurobiological role of the dorsolateral prefrontal cortex in recovery from trauma. Longitudinal brain imaging study among survivors of the South Korean subway disaster. Arch Gen Psychiatry. 2011;68:701–13.
Campbell-Sills L, Simmons AN, Lovero KL, Rochlin AA, Paulus MP, Stein MB. Functioning of neural systems supporting emotion regulation in anxiety-prone individuals. Neuroimage. 2011;54:689–96.
Kaiser RH, Andrews-Hanna JR, Wager TD, Pizzagalli DA. Large-scale network dysfunction in major depressive disorder: a meta-analysis of resting-state functional connectivity. JAMA Psychiatry. 2015;72:603–11.
Woodward ND, Rogers B, Heckers S. Functional resting-state networks are differentially affected in schizophrenia. Schizophr Res. 2011;130:86–93.
Menon V, Anagnoson RT, Mathalon DH, Glover GH, Pfefferbaum A. Functional neuroanatomy of auditory working memory in schizophrenia: relation to positive and negative symptoms. Neuroimage. 2001;13:433–46.
Joshi SA, Duval ER, Kubat B, Liberzon I. A review of hippocampal activation in post-traumatic stress disorder. Psychophysiology. 2020;57:e13357.
van Ettinger-Veenstra H, Boehme R, Ghafouri B, Olausson H, Wicksell RK, Gerdle B. Exploration of functional connectivity changes previously reported in fibromyalgia and their relation to psychological distress and pain measures. J Clin Med. 2020;9:3560.
Boyd JE, Lanius RA, McKinnon MC. Mindfulness-based treatments for posttraumatic stress disorder: a review of the treatment literature and neurobiological evidence. J Psychiatry Neurosci. 2018;43:7–25.
Sylvester CM, Corbetta M, Raichle ME, Rodebaugh TL, Schlaggar BL, Sheline YI, et al. Functional network dysfunction in anxiety and anxiety disorders. Trends Neurosci. 2012;35:527–35.
Whitfield-Gabrieli S, Thermenos HW, Milanovic S, Tsuang MT, Faraone SV, McCarley RW, et al. Hyperactivity and hyperconnectivity of the default network in schizophrenia and in first-degree relatives of persons with schizophrenia. Proc Natl Acad Sci USA. 2009;106:1279–84.
Suo X, Chen L, Kemp GJ, Wu D, Wang S. Aberrant structural-functional coupling of large-scale brain networks in older women with subthreshold depression. J Gerontol B Psychol Sci Soc Sci. 2025;80:gbaf013.
Giustino TF, Maren S. The role of the medial prefrontal cortex in the conditioning and extinction of fear. Front Behav Neurosci. 2015;9:298.
Frith U, Frith CD. Development and neurophysiology of mentalizing. Philos Trans R Soc Lond B Biol Sci. 2003;358:459–73.
Burkhouse KL, Jacobs RH, Peters AT, Ajilore O, Watkins ER, Langenecker SA. Neural correlates of rumination in adolescents with remitted major depressive disorder and healthy controls. Cogn Affect Behav Neurosci. 2017;17:394–405.
Fanselow MS, Dong HW. Are the dorsal and ventral hippocampus functionally distinct structures? Neuron. 2010;65:7–19.
McHugh SB, Fillenz M, Lowry JP, Rawlins JN, Bannerman DM. Brain tissue oxygen amperometry in behaving rats demonstrates functional dissociation of dorsal and ventral hippocampus during spatial processing and anxiety. Eur J Neurosci. 2011;33:322–37.
Ressler KJ, Berretta S, Bolshakov VY, Rosso IM, Meloni EG, Rauch SL, et al. Post-traumatic stress disorder: clinical and translational neuroscience from cells to circuits. Nat Rev Neurol. 2022;18:273–88.
Koch SB, van Zuiden M, Nawijn L, Frijling JL, Veltman DJ, Olff M. ABERRANT RESTING-STATE BRAIN ACTIVITY IN POSTTRAUMATIC STRESS DISORDER: A META-ANALYSIS AND SYSTEMATIC REVIEW. Depress Anxiety. 2016;33:592–605.
Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research–past, present, and future. Biol Psychiatry. 2006;60:376–82.
Ballmaier M, Toga AW, Blanton RE, Sowell ER, Lavretsky H, Peterson J, et al. Anterior cingulate, gyrus rectus, and orbitofrontal abnormalities in elderly depressed patients: an MRI-based parcellation of the prefrontal cortex. Am J Psychiatry. 2004;161:99–108.
Thomaes K, Dorrepaal E, Draijer N, de Ruiter MB, Elzinga BM, Sjoerds Z, et al. Increased anterior cingulate cortex and hippocampus activation in Complex PTSD during encoding of negative words. Soc Cogn Affect Neurosci. 2013;8:190–200.
Etkin A, Egner T, Kalisch R. Emotional processing in anterior cingulate and medial prefrontal cortex. Trends Cogn Sci. 2011;15:85–93.
Rive MM, van Rooijen G, Veltman DJ, Phillips ML, Schene AH, Ruhé HG. Neural correlates of dysfunctional emotion regulation in major depressive disorder. A systematic review of neuroimaging studies. Neurosci Biobehav Rev. 2013;37:2529–53.
Robinson OJ, Krimsky M, Lieberman L, Allen P, Vytal K, Grillon C. Towards a mechanistic understanding of pathological anxiety: the dorsal medial prefrontal-amygdala ‘aversive amplification’ circuit in unmedicated generalized and social anxiety disorders. Lancet Psychiatry. 2014;1:294–302.
Schiller D, Delgado MR. Overlapping neural systems mediating extinction, reversal and regulation of fear. Trends Cogn Sci. 2010;14:268–76.
Li L, Xu Z, Chen L, Suo X, Fu S, Wang S, et al. Dysconnectivity of the amygdala and dorsal anterior cingulate cortex in drug-naive post-traumatic stress disorder. Eur Neuropsychopharmacol. 2021;52:84–93.
Ibañez A, Gleichgerrcht E, Manes F. Clinical effects of insular damage in humans. Brain Struct Funct. 2010;214:397–410.
Paulus MP, Stein MB. An insular view of anxiety. Biol Psychiatry. 2006;60:383–7.
Nitschke JB, Sarinopoulos I, Mackiewicz KL, Schaefer HS, Davidson RJ. Functional neuroanatomy of aversion and its anticipation. Neuroimage. 2006;29:106–16.
Hoehn-Saric R, Schlund MW, Wong SH. Effects of citalopram on worry and brain activation in patients with generalized anxiety disorder. Psychiatry Res. 2004;131:11–21.
Schimmelpfennig J, Topczewski J, Zajkowski W, Jankowiak-Siuda K. The role of the salience network in cognitive and affective deficits. Front Hum Neurosci. 2023;17:1133367.
Ehrhardt NM, Fietz J, Kopf-Beck J, Kappelmann N, Brem AK. Separating EEG correlates of stress: cognitive effort, time pressure, and social-evaluative threat. Eur J Neurosci. 2022;55:2464–73.
Marshall AC, Cooper NR. The association between high levels of cumulative life stress and aberrant resting state EEG dynamics in old age. Biol Psychol. 2017;127:64–73.
Müller-Putz GR. Electroencephalography. Handb Clin Neurol. 2020;168:249–62.
Lian J, Xu L, Song T, Peng Z, Zhang Z, An X, et al. Reduced resting-state EEG power spectra and functional connectivity after 24 and 36 h of sleep deprivation. Brain Sci. 2023;13:949.
Fingelkurts AA, Fingelkurts AA, Kähkönen S. Functional connectivity in the brain–is it an elusive concept? Neurosci Biobehav Rev. 2005;28:827–36.
Hajcak G, MacNamara A, Olvet DM. Event-related potentials, emotion, and emotion regulation: an integrative review. Dev Neuropsychol. 2010;35:129–55.
Foti D, Olvet DM, Klein DN, Hajcak G. Reduced electrocortical response to threatening faces in major depressive disorder. Depress Anxiety. 2010;27:813–20.
Kujawa A, MacNamara A, Fitzgerald KD, Monk CS, Phan KL. Enhanced neural reactivity to threatening faces in anxious youth: evidence from event-related potentials. J Abnorm Child Psychol. 2015;43:1493–501.
MacNamara A, Jackson TB, Fitzgerald JM, Hajcak G, Phan KL. Working memory load and negative picture processing: neural and behavioral associations with panic, social anxiety, and positive affect. Biol Psychiatry Cogn Neurosci Neuroimaging. 2019;4:151–9.
Rocchi L, Ibáñez J, Benussi A, Hannah R, Rawji V, Casula E, et al. Variability and predictors of response to continuous theta burst stimulation: a TMS-EEG study. Front Neurosci. 2018;12:400.
Xia W, Dai R, Xu X, Huai B, Bai Z, Zhang J, et al. Cortical mapping of active and passive upper limb training in stroke patients and healthy people: a functional near-infrared spectroscopy study. Brain Res. 2022;1788:147935.
Mantini D, Marzetti L, Corbetta M, Romani GL, Del Gratta C. Multimodal integration of fMRI and EEG data for high spatial and temporal resolution analysis of brain networks. Brain Topogr. 2010;23:150–8.
Kaneta T. PET and SPECT imaging of the brain: a review on the current status of nuclear medicine in Japan. Jpn J Radiol. 2020;38:343–57.
Jamieson D, Kannis-Dymand L, Beaudequin DA, Schwenn P, Shan Z, McLoughlin LT, et al. Can measures of sleep quality or white matter structural integrity predict level of worry or rumination in adolescents facing stressful situations? Lessons from the COVID-19 pandemic. J Adolesc. 2021;91:110–18.
Zheng A, Chen X, Xiang G, Li Q, Du X, Liu X, et al. Association between negative affect and perceived mortality threat during the COVID-19 pandemic: the role of brain activity and connectivity. Neuroscience. 2023;535:63–74.
Funding
This work was supported by National Key R&D Program of China (Q.G., 2022YFC2009900) and the National Natural Science Foundation of China (Q.G., grants 82027808; N.P., grant 823B2041; S.W., grant 31800963). N.P. was also supported by the Young Elite Scientists Sponsorship Program for Graduate Students by China Association for Science and Technology.
Author information
Authors and Affiliations
Contributions
YG, NP, SW, and QG conceptualized the project. YG drafted the manuscript. YG, NP, SW, YL, and XZ contributed to literature search, data collection and analysis, as well as data interpretation. NP, YZ, MKS, QL, XS, SW, and QG critically revised the paper. All authors approved the final version of the paper.
Corresponding authors
Ethics declarations
Competing interests
Dr. Singh is on the advisory board for Sunovion and Skyland Trail, is a consultant for Johnson and Johnson, Alkermes, Neumora, AbbVie, Karuna Therapeutics, Inc., Boehringer Ingelheim, and Intra-Cellular Therapeutics, Inc. Dr. Singh receives honoraria from the American Academy of Child and Adolescent Psychiatry, and royalties from American Psychiatric Association Publishing and Thrive Global. All other authors declare that they have no competing interests. All other authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, Y., Pan, N., Zou, Y. et al. Neuroimaging insights into the psychosocial impact of the COVID-19 pandemic: a systematic review. Transl Psychiatry 15, 236 (2025). https://doi.org/10.1038/s41398-025-03423-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-025-03423-2