Abstract
The COVID-19 pandemic and its associated lockdowns were an unprecedented source of stress, with striking adverse effects on adolescents’ mental health but relatively unknown effects on important aspects of neurobiological functioning. Using data from 154 adolescents (age M ± SD = 16.2 ± 1.1 years; range = 13.9–19.4) drawn from an ongoing longitudinal study and assessed either before or after the pandemic, we compared the pre-pandemic and post-pandemic groups on three key stress-sensitive biological systems: the hypothalamic-pituitary-adrenal (HPA) axis, immune response, and neural responses to affective stimuli. We found that compared to those assessed before the pandemic, adolescents assessed post-lockdown had significantly lower total cortisol production, elevated levels of systemic inflammation, and reduced neural activation in the prefrontal cortex during affective processing (pseudo-F(1,3250) = 7.43, p = 0.006). These findings suggest that, for adolescents, the experience of the pandemic was associated with significant disruptions in multiple biological systems that are sensitive to stress that might have enduring adverse developmental effects.
Similar content being viewed by others
Introduction
Chronic stress profoundly affects both physical and mental health, increasing individuals’ risk for developing a range of diseases and reducing overall well-being [1]. The body’s response to chronic stress is complex and multifaceted, involving several physiological systems, including the hypothalamic-pituitary-adrenal (HPA) axis, inflammation, and brain function. Each of these systems plays a significant role in determining whether and how chronic stress can have long-lasting detrimental consequences.
The HPA axis, a primary component of the body’s stress response system, produces cortisol, which has widespread effects on biological functioning. Cortisol helps maintain homeostasis by supporting metabolism via gluconeogenesis, regulating blood pressure, and suppressing inflammation [2]. Chronic stress, however, can lead to prolonged cortisol secretion and impair biological functioning over time, including disrupting HPA axis homeostasis [3, 4]. This dysregulation has been linked to poor health [5], in part through its documented impact on the inflammatory response [6]. Psychological stress can trigger inflammation in the same way a physical pathogen does; further, chronic stress is associated with persistently elevated levels of systemic inflammation [7, 8], which have been linked to a range of chronic illnesses [9]. Finally, these disruptions are associated with altered brain function, including communication between the brain and the endocrine and immune systems. Indeed, glucocorticoids have been found to affect brain areas critical for executive function, memory, and emotion processing, including the prefrontal cortex (PFC), hippocampus, and amygdala [10]. These alterations have been linked to various forms of psychopathology, such as depression [11].
In addition to examining the biological effects of chronic stress, researchers have recently highlighted the importance of the timing of stress exposure. Sensitive periods, characterized by heightened plasticity in developmental processes, can increase individuals’ vulnerability to the effects of stress [12, 13]. Adolescence, which spans from the onset of puberty to young adulthood, is one such sensitive period, during which significant physiological changes across the endocrine, immune, and neural systems occur [14, 15]. In the endocrine system, basal levels of cortisol increase with the onset of puberty [16]. Similarly, sex hormones can directly influence immune cells like lymphocytes and macrophages [17]. Further, findings from animal models indicate that pro-inflammatory activity can alter neurodevelopmental processes like synaptic pruning and dendritic remodeling by affecting glial cells in the brain [18]. There is also significant development during adolescence in executive and limbic brain regions; the PFC, in particular, undergoes changes that facilitate higher-order cognition [19]. In fact, the PFC is also especially sensitive to stress, expressing more glucocorticoid receptor mRNA during adolescence than at any other developmental stage [20]. Importantly, these changes in the brain [21, 22] may be related to an increased susceptibility to the effects of elevated levels of inflammation. Together, these processes not only highlight the significant neurobiological growth that occurs during adolescence but also reveal the increased susceptibility of adolescents to the effects of stress. It is not surprising, therefore, that mental health difficulties often peak during adolescence [23].
In this context, the COVID-19 pandemic and the subsequent lockdowns caused unprecedented societal disruptions, and the resulting stress had a particularly strong impact on young people [24, 25]. Emotional difficulties among adolescents increased sharply, with meta-analyses showing that rates of stress-related conditions such as anxiety and depression doubled worldwide [26]. While researchers have begun to examine the effects of pandemic-related stress on various aspects of psychological functioning in adolescents, we know much less about its impact on neurobiological functioning [27]. Although some studies have identified neurobiological characteristics that predict levels of functioning during the pandemic [28, 29], the lockdown restrictions limited opportunities to obtain data addressing precisely how the pandemic affected or changed the neurobiology of youth.
Longitudinal studies examining within-person changes through the pandemic and studies comparing independent, matched pre- and post-COVID groups have linked aspects of the pandemic to disruptions in endocrine and immune function, as well as structural neurodevelopment. For example, Fung et al. [30] and Taylor et al. [31] reported that adolescent levels of hair cortisol increased over the initial months of the pandemic and predicted subsequent increases in negative affect. A study of adults also indicated that pandemic-related stress affects immune function. Brusaferri et al. [32] found that adults with chronic lower back pain who provided blood samples and participated in PET/MR scans during the pandemic had higher levels of the proinflammatory cytokine interleukin-6 and increased markers of neuroinflammation than did adults who were assessed before the pandemic.
The pandemic has also been found to affect brain structure in stress-sensitive regions. Gotlib et al. [33] and Van Drunen et al. [34] compared youth assessed before the COVID-19 pandemic with youth assessed after the lockdown restrictions ended using magnetic resonance imaging (MRI). Gotlib et al. found that adolescents in the post-lockdown group had reduced bilateral cortical thickness and larger gray matter volumes in the bilateral hippocampus and amygdala, and more advanced brain age, compared to their age- and sex-matched peers who were assessed before the pandemic. In a similar analysis of youth 9–13 years of age, Van Drunen et al. reported that youth assessed post-lockdown had a greater decrease in cortical thickness in the medial PFC and a larger increase in hippocampal volume than did youth assessed before the pandemic. Finally, a recent study suggests that the adverse effects of the pandemic on adolescents’ brain structure are sex-specific. Corrigan et al. [35] reported that female adolescents assessed after pandemic restrictions ended experienced more widespread cortical thinning compared to those assessed before the pandemic; in male adolescents this effect was limited to only two occipital lobe regions.
Overall, the COVID-19 pandemic has been linked to higher levels of hair cortisol in adolescents, elevated levels of inflammation in adults, and altered brain structure in the PFC and limbic regions in adolescents; however, it is not clear whether the pandemic has also led to changes in levels of inflammation and brain function in youth. In fact, no study to date has comprehensively examined the effects of the pandemic and its associated lockdowns on multiple biological systems of stress in a single sample of participants. The purpose of this study was to advance our understanding of how the pandemic and its associated lockdowns has affected stress-sensitive biological systems during a sensitive developmental period. Specifically, we examined whether adolescents assessed after the pandemic lockdowns ended differ from their age- and sex-matched peers who were assessed before the pandemic in their diurnal patterns of cortisol secretion, their levels of systemic inflammation, and their PFC responses to affective stimuli.
Methods and materials
Participants
Participants were drawn from a larger sample of 220 adolescents from the San Francisco Bay Area community in California who were participating in an ongoing longitudinal study of the psychobiological effects of early life stress (ELS) across adolescence. The adolescents in the current sample are a subset of those assessed in Gotlib et al. [33]. Participants were 9–13 years of age at entry to the study in 2013 and were matched at that time on pubertal stage, assessed using self-reported Tanner Staging, as described below. They completed follow-up assessments approximately every two years. At all assessments we collected a wide range of data, including structural and functional neuroimaging, biological samples, and self-report measures of psychosocial functioning. Exclusion criteria included nonfluency in English, standard MRI contraindications, and history of neurological disorder or major medical or psychiatric illness. This study was approved by the Stanford University Institutional Review Board, and participants were compensated for their time. Research staff obtained informed consent and assent from parents and their adolescent children, respectively.
We constructed two matched groups of adolescents from the larger sample using data collected before the pandemic (pre-COVID group; n = 76; November 2016 to November 2019) and data collected after the COVID-19 pandemic lockdown restrictions ended in the Bay Area (post-COVID group; n = 78; October 2020 to March 2022; total n = 154; 89 F/65 M; age M ± SD = 16.2 ± 1.1years; range = 13.9–19.4). On average, adolescents in the post-COVID group were assessed approximately one year after the March 2020 lockdown restrictions began (M ± SD = 1.08 ± 0.36years; range = 0.43–2.06). We prioritized matching the two groups on age and sex; further the groups did not differ significantly in race, puberty, socioeconomic status (SES), or early life stress (ELS). The only exception was that post-COVID adolescents had a higher body mass index (BMI), described below. Only one participant reported having been infected with COVID-19; supplemental sensitivity analyses excluding this participant yielded the same pattern of results reported here.
Demographic characteristics
Pubertal stage & body mass index
To assess pubertal status at study onset and at the follow-up assessments, participants reported their Tanner Staging, for which pubertal development is rated on a scale from 1–5 based on illustrations of pubic hair and breast/testes growth [36]. We averaged these scores to compute an overall pubertal stage and treated this score as a continuous variable. We calculated BMI from participants’ height and weight [37] as it relates to pubertal development and other biological measures assessed in the current study.
Socioeconomic status
We obtained two indicators of SES: highest parental education and income-to-needs ratio (INR) [38, 39]. Parents of participants provided their highest education, coded ordinally (1 = no GED/high school diploma; 2 = GED/high school diploma; 3 = some college; 4 = two-year college degree; 5 = four-year college degree; 6 = master’s degree; 7 = professional degree [MD/JD/DDS]; 8 = PhD). INR was calculated by dividing parent-reported income by the 2017 low-income limit for the county of residence, as defined by the Department of Housing and Urban Development as 80% of the median income and adjusted for the number of household members (https://www.huduser.gov/portal/datasets/il).
Early life stress
Participants completed a structured interview assessing early life stress, the Traumatic Events Screening Inventory for Children (TESI-C) at the first timepoint of the study (mean age of 11.5 years) to assess exposure to over 30 types of stressors (e.g., domestic violence, emotional abuse, neglect). For each event endorsed, participants described and rated the severity of the event. An external panel of three coders blind to the participants’ subjective ratings then rated the objective severity of each event on a scale ranging from 0 (non-event) to 4 (high severity), in half-point increments, using a modified version of the UCLA Life Stress Interview coding system [40]. A cumulative ELS severity score was computed for each participant by summing the maximum objective severity scores from each category of stressful experience that the participant endorsed [41, 42].
Biological indicators
We examined differences between the two groups of adolescents in their stress physiology and immune functioning using metrics of their daily diurnal cortisol secretion and levels of the inflammatory marker C-reactive protein (CRP), respectively. Both variables were analyzed across different assay batches, which we controlled for in all statistical analyses. We describe measures of these variables briefly below and present more detail in the Supplement.
Stress physiology – diurnal cortisol
Stress physiology was assessed by measuring participants’ levels of diurnal cortisol, as described in Berens et al. [43]. Within a week of the scan session, participants provided saliva samples at four time points across two consecutive weekdays: upon waking while still in bed, 30 min after waking, midafternoon (at 3 p.m.), and in the evening two hours after dinner. Participants reported the actual time of saliva collection, which was used when calculating the cortisol metrics. The samples were stored in participants’ freezers until they could be transferred to Stanford University, where they were stored at −20 °C. Samples were assayed at Salimetrics’ SalivaLab (Carlsbad, CA) using the Salimetrics Salivary Cortisol Assay Kit (Cat. No. 1-3002), without modifications to the manufacturer’s protocol; the intra- and inter-assay coefficient of variation (CV) were 4.6% and 6.0%, respectively. We measured two commonly used characteristics of diurnal cortisol secretion: cortisol awakening response (CAR) slope (waking to 30 min post-waking) and area under the curve with respect to ground (AUCg), indexing total cortisol produced throughout the day [44]. Outlying values were winsorized using a 5% threshold. See the Supplement for more information about cortisol collection and analysis.
Systemic inflammation – C-reactive protein
Systemic inflammation was assessed using a dried blood spot protocol in which CRP levels were obtained from finger-prick blood samples collected after participants’ scan (see the Supplement for more details). The samples were frozen and stored before being analyzed using Luminex FlexMap3D at the Stanford Human Immune Monitoring Center. Inflammation concentrations are reported as log-transformed median fluorescence intensity (MFI) values, with higher values indicating higher inflammation. We used MFI instead of concentration units given its advantage for low-abundant analytes [45]. Participants had generally low CRP levels (M ± SD = 105.5 ± 268.7; range = 0.3–1301.6 ng/mL), which are typical for healthy adolescents.
Neural function
Participants completed a neuroimaging session consisting of structural and functional MRI (fMRI) sequences at the Stanford Center for Cognitive and Neurobiological Imaging. As Gotlib et al. [33] described previously, all pre-COVID participants were scanned using a GE 3T Discovery MR750 that was upgraded to the GE UltraHigh Performance (UHP) system during the pandemic shutdown (see Gotlib et al., [33] for a description of procedures implemented to ensure that scanner differences did not introduce bias that might explain group differences in MRI-based measures). For the current study, we examined neural activation in the stress-sensitive PFC during two fMRI tasks designed to elicit responses in this region during the processing of affective stimuli. All fMRI data were preprocessed using fMRIPrep [46] (v.20.2.1), an automated pipeline based on empirically optimized processing procedures, following surface-based registration of anatomical images using FreeSurfer [47] (v.6.0.1). Individual-level modeling of fMRI timeseries data was conducted in FSL [48, 49] (v.6.0.6.2) and parameter estimates of activation were extracted from a priori defined regions previously shown to be engaged with the tasks using binarized masks, described below.
Monetary reward processing
Adolescents completed a child-modified version of the Monetary Incentive Delay (MID) task, which reliably engages frontostriatal brain regions associated with reward processing [50, 51]. In each of 72 trials, participants (1) viewed the incentive cue indicating the condition (gain, nongain, loss, nonloss); (2) anticipated the target; (3) viewed and responded to a triangular target before it disappeared (adaptive timing); (4) fixated for a delay period; and (5) viewed an outcome message. We extracted parameter estimates of neural activation using bilateral anatomical masks derived from the Brainnetome and Harvard-Oxford atlases during the following contrasts: (1) medial PFC (mPFC) during outcome of gain > nongain, 50% threshold; and (2) the nucleus accumbens (NAcc) during anticipation of gain > nongain, 50% threshold, respectively, as has been previously done in studies using the MID task [51, 52].
Implicit emotion regulation
Participants also completed an affect labeling task in the scanner. Affect labeling (i.e. putting feelings into words) is a form of implicit emotion regulation in which linguistic processing of stimuli attenuates emotion reactivity [53,54,55]. In the affect labeling task, participants were asked to match options to a target facial expression displaying negatively-valenced (fear, anger, sadness) or positively-valenced (happy, excited, calm) emotions. In the Label condition, participants matched word labels to a target emotional face stimulus; in the Match condition, they matched images of facial expressions to the target facial expression. Overall, there were five blocks for a single run of the task: Negative Label, Negative Match, Positive Label, Positive Match, and a sensorimotor control (Shape Match). We extracted estimates of neural activation from the contrast of Negative Label > Match using a bilateral ventrolateral prefrontal cortex (vlPFC) mask that was defined using 5 mm spherical ROI masks centered on peak activation coordinates from prior work using this task from our group [56].
Statistical analysis
All statistical analyses were conducted using R [57] (v. 4.4.2). Because Shapiro-Wilk tests for normality indicated that demographic and neurobiological indicators were not normally distributed, we conducted nonparametric tests. We used an α = 0.05 level given the exploratory nature of the analyses. Code available upon request to the corresponding author.
Demographic characteristics
To test for differences between the pre-COVID and post-COVID groups, we conducted nonparametric Wilcoxon rank sum tests comparing the two groups on median values of each of the following demographic characteristics: age, SES, ELS exposure, and BMI. Group differences in categorical variables were assessed using Χ2 tests.
Analysis of neurobiological functioning
To test whether the pre-COVID adolescents differed significantly from the post-COVID adolescents with respect to their neurobiological functioning, we first conducted a permutational multivariate analysis of covariance (MANCOVA) using distance matrices [58, 59]. This nonparametric technique assumes no explicit distributions and yields a pseudo-F test statistic, modeled after the F-statistic from the standard analysis of variance (ANOVA) and MANCOVA. Before running the analyses, we used multiple imputation for the permutational analyses, a robust statistical technique that leverages the distribution of observed data to generate plausible estimates for missing values [60, 61]. Specifically, we conducted multiple imputation by chained equations (MICE) via the mice R package [62], implementing predictive mean matching to impute 100 datasets. The resulting datasets were analyzed separately, and the results were subsequently pooled using the D2 method for combining ANOVA results [63]. See the Supplement for more details.
Using a permutational MANCOVA, we tested whether the two groups differed significantly in the following outcomes: diurnal CAR slope, diurnal AUCg, peripheral concentration of CRP, mPFC activation during the MID outcome of gain contrast, NAcc activation during the MID anticipation of gain contrast, and vlPFC activation during the affect label negative implicit emotion regulation contrast. We controlled for the following variables known to affect these outcomes: BMI, cortisol and inflammation assay batch, waking time for morning saliva/cortisol collection, and ELS. MANCOVAs were conducted with 1000 permutations using the adonis2 function from the vegan package [64] in R. Additional sensitivity analyses are reported in the Supplement.
Finally, because the MANOVA yielded a significant effect of group status, we followed up this analysis with permutational analyses of covariance (ANCOVAs) for each dependent variable to identify which outcomes contributed to the overall significant multivariate effect. We controlled for the same covariates as we did in the permutational MANCOVA and used the same parameters with the adonis2 function.
Results
Demographic characteristics
The two groups did not significantly differ across all demographic variables tested except that the Post-COVID group displayed higher BMI (W = 1968.5; p = 0.025). Detailed results are reported in Table 1.
Overall group differences
The permutation MANCOVA yielded a statistically significant effect of COVID-19 group on the measures of endocrine, immune, and neural functioning (pseudo-F(1,3250) = 7.43, p = 0.006).
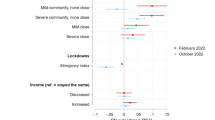
HPA axis function
Post-COVID youth had significantly lower AUCg values than did pre-COVID youth (Fig. 1A; pseudo-F(1,625) = 9.52, p = 0.002); the two groups did not differ significantly in CAR slope (Fig. 1B; pseudo-F(1,2782) = 0.33, p = 0.568).
A Average cortisol production over two days (AUCg). B CAR slope (the change from waking to 30 min post-waking). C Systemic inflammation assessed using CRP levels from blood. Analyses used imputed values; only raw values are plotted in the figure for ease of visualization, with the sample size indicated. Diamond mean, * significant, CRP C-reactive protein, CAR cortisol awakening response, AUCg area under the curve with respect to ground.
Systemic inflammation
Post-Covid youth had significantly higher levels of peripheral CRP than did pre-COVID youth (Fig. 1C; pseudo-F(1989) = 48.79, p < 0.001).
Neural function
Post-COVID youth had significantly lower neural activation in the mPFC while receiving monetary rewards (Fig. 2A; pseudo-F(1,1204) = 7.99, p = 0.005) and vlPFC during negative implicit emotion regulation (Fig. 2C; pseudo-F(1,1901) = 8.38, p = 0.004). The two groups did not differ in neural activation in the NAcc while anticipating monetary rewards (Fig. 2B; pseudo-F(1,2365) = 0.90, p = 0.343).
Panels A and B show neural activation during the monetary incentive delay task. A mPFC during the outcome of gain contrast; and B NAcc during anticipation of gain contrast. C Activation in the vlPFC during negative implicit emotion regulation in the Affect Label task. Analyses used imputed values; only raw values are plotted in the figure for ease of visualization, with the sample size indicated. Diamond mean; * significant, mPFC medial prefrontal cortex, NAcc nucleus accumbens, vlPFC ventrolateral prefrontal cortex, Neg. Emotion Reg. negative implicit emotion regulation contrast.
Discussion
The primary aim of this study was to examine changes across multiple biological and neural systems in adolescents following the COVID-19 pandemic and lockdown restrictions. By comparing two independent age- and sex-matched groups drawn from a larger longitudinal study, we were able to assess pandemic-related differences in neurobiological indicators of endocrine, immune, and neural function. We found significant differences between adolescents who were assessed pre-pandemic and adolescents who were assessed post-pandemic in three stress-sensitive systems — HPA-axis function, inflammation, and prefrontal neural activation to affective stimuli. Specifically, adolescents who were assessed after the COVID-19 lockdowns ended had significantly lower AUCg, higher levels of CRP, and less PFC activation while receiving monetary rewards and during implicit emotion regulation of negative emotions.
Our findings of COVID-19-related changes in all three of the biological systems examined in this study demonstrate the pervasiveness of the effects of the pandemic on adolescents’ psychobiological functioning. These three interacting systems (endocrine, immune, and neural) influence and regulate each other to maintain homeostasis. Their dynamic interplay reflects the concept of allostatic load, in which chronic stress results in cumulative “wear and tear” across bodily systems, reducing their ability to adapt and function effectively [65]. In particular, the lower AUCg exhibited by post-COVID youth suggests a dysregulated HPA-axis response, consistent both with prior studies of cortisol production in adolescents [30, 31] and with extensive research linking chronic stress to HPA-axis dysregulation [2]. Interestingly, we did not find a significant difference between the pre- and post-COVID adolescents in their cortisol awakening response, suggesting that pandemic-related stress had differential effects on the HPA response system. Given that cortisol is a potent anti-inflammatory agent, and that its prolonged reduction due to chronic stress can lead to altered pro-inflammatory states [66], it is not surprising that we also found elevated levels of CRP in adolescents post-lockdowns. Documenting this heightened pro-inflammatory state in typically developing youth suggests that the impact of the pandemic-related stress on immune function was widespread, extending beyond populations with clinical conditions (e.g. adult patients as reported in Brusaferri et al., [32]) and, further, is concerning in light of findings that chronically elevated levels of inflammation are associated with the development of poor physical and mental health [67].
Finally, the post-COVID adolescents in our study also demonstrated reduced neural activation in PFC regions during both reward processing and implicit emotion regulation tasks. These changes are consistent with previous reports that the experience of stress can impair the development and function of these processes [68]. It is noteworthy that these alterations in neural activation involved the PFC, which contributes to the processing of threatening stimuli, making it a central mediator of the stress response [69]. This COVID-19-related difference also has developmental significance, as the PFC continues to develop through late adolescence into young adulthood [70, 71], perhaps rendering this structure particularly susceptible to the stresses of the pandemic. Indeed, the broad multi-system effects documented here are concerning for adolescent development, given the cumulative effects of allostatic load in increasing risk for chronic health difficulties [72].
While we focused in this study on the impact of a recent and enduring stressor, the COVID-19 pandemic, it is noteworthy that exposure to ELS, a well-documented risk factor for a range of adverse outcomes, often leads to neurobiological changes in adolescents that closely mirror those reported here and in other studies examining the impact of COVID-19 on youth [30, 31, 33,34,35]. ELS has been found to be associated with serious long-term health consequences, including heightened risk for cancer, diabetes, stroke, and depression, as well as poorer socioeconomic outcomes in adulthood [73,74,75]. These outcomes have been attributed to disruptions in the same interconnected systems examined in the current study: endocrine dysregulation [4]; a pro-inflammatory immune response [76]; and altered neural functioning [77]. It appears that in a relatively short timeframe, the COVID-19 pandemic has led to changes in adolescents’ psychobiological functioning that previously were delineated following years of exposure to adversity.
We should note three limitations of this study. First, to address missing data, we used multiple imputation, a recommended method for handling missing data that appropriately reflects uncertainty and does not introduce bias compared to other methods [78]. Importantly, however, supplementary group-level analyses using only complete cases yielded results consistent with the findings reported here. Second, our sample was primarily White and came from higher income households. Given that young people from racial and ethnic minorities and lower-SES backgrounds have been found to face compounding challenges during the pandemic lockdowns [27], it will be important to extend our findings to these populations. Third, our sample, while unique and important, is relatively small, particularly for a neuroimaging study. Thus, our findings should be replicated in a larger sample.
Overall, the findings of this study indicate that adolescents who were assessed after the COVID-19 pandemic and its associated lockdowns exhibit significant indicators of allostatic “wear and tear” compared to similar adolescents who were assessed before the pandemic. This is particularly concerning because these differences have been found to be associated with poorer health outcomes and, further, are occurring during a sensitive period of development. As a result of the pandemic, adolescents may now be at elevated risk for negative outcomes. While speculative, an important implication of these findings is that the developmental trajectories of adolescents following the COVID-19 pandemic may have diverged from the normative trajectories before the pandemic. This possibility is strengthened by the phenotypic similarity between post-COVID adolescents and youth who experienced significant stressors early in development. Understanding this “new normal” will be essential for developing targeted strategies to mitigate the impact of pandemic and its associated lockdowns on adolescents’ health and well-being.
Data availability
Data and code are available upon reasonable request to the corresponding author.
References
O’Connor DB, Thayer JF, Vedhara K. Stress and health: a review of psychobiological processes. Annu. Rev. Psychol. 2021;72:663–88.
Knezevic E, Nenic K, Milanovic V, Knezevic NN. The role of cortisol in chronic stress, neurodegenerative diseases, and psychological disorders. Cells. 2023;12:2726.
Gunnar M, Quevedo K. The neurobiology of stress and development. Annual Review of Psychology. 2007;58:145–73.
Koss KJ, Gunnar MR. Annual research review: early adversity, the hypothalamic–pituitary–adrenocortical axis, and child psychopathology. Journal of Child Psychology and Psychiatry. 2018;59:327–46.
Agorastos A, Chrousos GP. The neuroendocrinology of stress: the stress-related continuum of chronic disease development. Mol Psychiatry. 2022;27:502–13.
Kotas ME, Medzhitov R. Homeostasis, inflammation, and disease susceptibility. Cell. 2015;160:816–27.
Lumertz FS, Kestering-Ferreira E, Orso R, Creutzberg KC, Tractenberg SG, Stocchero BA, et al. Effects of early life stress on brain cytokines: a systematic review and meta-analysis of rodent studies. Neuroscience & Biobehavioral Reviews. 2022;139:104746.
Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychological Bulletin. 2004;130:601–30.
Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, et al. Chronic inflammation in the etiology of disease across the life span. Nat Med. 2019;25:1822–32.
Lupien SJ, Juster R-P, Raymond C, Marin M-F. The effects of chronic stress on the human brain: from neurotoxicity, to vulnerability, to opportunity. Frontiers in Neuroendocrinology. 2018;49:91–105.
Auerbach RP, Admon R, Pizzagalli DA. Adolescent depression: stress and reward dysfunction. Harv Rev Psychiatry. 2014;22:139–48.
Cheng TW, Mills KL, Pfeifer JH. Revisiting adolescence as a sensitive period for sociocultural processing. Neuroscience & Biobehavioral Reviews. 2024;164:105820.
Lupien SJ, McEwen BS, Gunnar MR, Heim C. Effects of stress throughout the lifespan on the brain, behaviour and cognition. Nat Rev Neurosci. 2009;10:434–45.
Dahl RE, Allen NB, Wilbrecht L, Suleiman AB. Importance of investing in adolescence from a developmental science perspective. Nature. 2018;554:441–50.
Sisk LM, Gee DG. Stress and adolescence: vulnerability and opportunity during a sensitive window of development. Current Opinion in Psychology. 2022;44:286–92.
Engel, ML & Gunnar, MR Chapter three - the development of stress reactivity and regulation during human development. In: Clow, A & Smyth, N, editors. International review of neurobiology. 150. Academic Press, 2020. pp. 41–76.
Shames RS. Gender differences in the development and function of the immune system. Journal of Adolescent Health. 2002;30:59–70.
Andersen SL. Neuroinflammation, early-life adversity, and brain development. Harvard Review of Psychiatry. 2022;30:24.
Larsen B, Luna B. Adolescence as a neurobiological critical period for the development of higher-order cognition. Neuroscience & Biobehavioral Reviews. 2018;94:179–95.
Sheth C, McGlade E, Yurgelun-Todd D. Chronic stress in adolescents and its neurobiological and psychopathological consequences: an RDoC perspective. Chronic Stress. 2017;1:247054701771564.
Giedd JN, Blumenthal J, Jeffries NO, Castellanos FX, Liu H, Zijdenbos A, et al. Brain development during childhood and adolescence: a longitudinal MRI study. Nat Neurosci. 1999;2:861–3.
Norbom LB, Ferschmann L, Parker N, Agartz I, Andreassen OA, Paus T, et al. New insights into the dynamic development of the cerebral cortex in childhood and adolescence: integrating macro- and microstructural MRI findings. Progress in Neurobiology. 2021;204:102109.
Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. 2022;27:281–95.
Gotlib IH, Borchers LR, Chahal R, Gifuni AJ, Teresi GI, Ho TC. Early life stress predicts depressive symptoms in adolescents during the COVID-19 pandemic: the mediating role of perceived stress. Front. Psychol. 2021;11:603748.
McLaughlin KA, Rosen ML, Kasparek SW, Rodman AM. Stress-related psychopathology during the COVID-19 pandemic. Behaviour Research and Therapy. 2022;154:104121.
Racine N, McArthur BA, Cooke JE, Eirich R, Zhu J, Madigan S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: a meta-analysis. JAMA Pediatr. 2021;175:1142.
Hostinar CE, Velez G. Generation COVID: coming of age amid the pandemic. Current Opinion in Psychology. 2024;55:101725.
Borchers LR, Gifuni AJ, Ho TC, Kirshenbaum JS, Gotlib IH. Threat- and reward-related brain circuitry, perceived stress, and anxiety in adolescents during the COVID-19 pandemic: a longitudinal investigation. Social Cognitive and Affective Neuroscience. 2024;19:nsae040.
Machlin L, McLaughlin KA. Pre-pandemic brain structure and function and adolescent psychopathology during the COVID-19 pandemic. Current Opinion in Psychology. 2023;52:101647.
Fung MH, Taylor BK, Embury CM, Spooner RK, Johnson HJ, Willett MP, et al. Cortisol changes in healthy children and adolescents during the COVID-19 pandemic. Stress. 2022;25:323–30.
Taylor BK, Fung MH, Frenzel MR, Johnson HJ, Willett MP, Badura-Brack AS, et al. Increases in circulating cortisol during the COVID-19 pandemic are associated with changes in perceived positive and negative affect among adolescents. Res Child Adolesc Psychopathol. 2022;50:1543–55.
Brusaferri L, Alshelh Z, Schnieders JH, Sandström A, Mohammadian M, Morrissey EJ, et al. Neuroimmune activation and increased brain aging in chronic pain patients after the COVID-19 pandemic onset. Brain, Behavior, and Immunity. 2024;116:259–66.
Gotlib IH, Miller JG, Borchers LR, Coury SM, Costello LA, Garcia JM, et al. Effects of the COVID-19 pandemic on mental health and brain maturation in adolescents: implications for analyzing longitudinal data. Biological Psychiatry Global Open Science. 2023;3:912–8.
Van Drunen L, Toenders YJ, Wierenga LM, Crone EA. Effects of COVID-19 pandemic on structural brain development in early adolescence. Sci Rep. 2023;13:5600.
Corrigan NM, Rokem A, Kuhl PK. COVID–19 lockdown effects on adolescent brain structure suggest accelerated maturation that is more pronounced in females than in males. Proc Natl Acad Sci USA. 2024;121:e2403200121.
Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969;44:291–303.
He Q, Karlberg J. Bmi in childhood and its association with height gain, timing of puberty, and final height. Pediatr Res. 2001;49:244–51.
King LS, Humphreys KL, Camacho MC, Gotlib IH. A person-centered approach to the assessment of early life stress: associations with the volume of stress-sensitive brain regions in early adolescence. Dev Psychopathol. 2019;31:643–55.
Yuan JP, Jaeger EL, Coury SM, Uy JP, Buthmann JL, Ho TC, et al. Socioeconomic disadvantage moderates the association of systemic inflammation with amygdala volume in adolescents over a two-year interval: an exploratory study. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. 2024;9:896–904. https://doi.org/10.1016/j.bpsc.2024.05.002.
Rudolph KD, Hammen C, Burge D, Lindberg N, Herzberg D, Daley SE. Toward an interpersonal life-stress model of depression: the developmental context of stress generation. Development and Psychopathology. 2000;12:215–34.
King LS, Colich NL, LeMoult J, Humphreys KL, Ordaz SJ, Price AN, et al. The impact of the severity of early life stress on diurnal cortisol: The role of puberty. Psychoneuroendocrinology. 2017;77:68–74.
King LS, Graber MG, Colich NL, Gotlib IH. Associations of waking cortisol with DHEA and testosterone across the pubertal transition: effects of threat-related early life stress. Psychoneuroendocrinology. 2020;115:104651.
Berens A, LeMoult J, Kircanski K, Gotlib IH. ADHD symptoms and diurnal cortisol in adolescents: the importance of comorbidities. Psychoneuroendocrinology. 2023;148:105990.
Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–31.
Breen EJ, Tan W, Khan A. The statistical value of raw fluorescence signal in luminex xMAP based multiplex immunoassays. Sci Rep. 2016;6:26996.
Esteban O, Markiewicz CJ, Blair RW, Moodie CA, Isik AI, Erramuzpe A, et al. fMRIPrep: a robust preprocessing pipeline for functional MRI. Nature Methods. 2019;16:111–6.
Dale AM, Fischl B, Sereno MI. Cortical surface-based analysis: I. Segmentation and surface reconstruction. NeuroImage. 1999;9:179–94.
Smith SM, Jenkinson M, Woolrich MW, Beckmann CF, Behrens TEJ, Johansen-Berg H, et al. Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage. 2004;23:S208–19.
Woolrich MW, Ripley BD, Brady M, Smith SM. Temporal autocorrelation in univariate linear modeling of FMRI data. NeuroImage. 2001;14:1370–86.
Knutson B, Adams CM, Fong GW, Hommer D. Anticipation of increasing monetary reward selectively recruits nucleus accumbens. J. Neurosci. 2001;21:RC159.
Knutson B, Greer SM. Anticipatory affect: neural correlates and consequences for choice. Phil. Trans. R. Soc. B. 2008;363:3771–86.
Yuan JP, Coury SM, Ho TC, Gotlib IH. Early life stress moderates the relation between systemic inflammation and neural activation to reward in adolescents both cross-sectionally and longitudinally. Neuropsychopharmacol. 2024;49:532–40.
Colich NL, Williams ES, Ho TC, King LS, Humphreys KL, Price AN, et al. The association between early life stress and prefrontal cortex activation during implicit emotion regulation is moderated by sex in early adolescence. Development and Psychopathology. 2017;29:1851–64.
Lieberman MD, Eisenberger NI, Crockett MJ, Tom SM, Pfeifer JH, Way BM. Putting feelings into words. Psychol Sci. 2007;18:421–8.
Torre JB, Lieberman MD. Putting feelings into words: affect labeling as implicit emotion regulation. Emotion Review. 2018;10:116–24.
Yuan JP, Ho TC, Coury SM, Chahal R, Colich NL, Gotlib IH. Early life stress, systemic inflammation, and neural correlates of implicit emotion regulation in adolescents. Brain, Behavior, and Immunity. 2022;105:169–79.
R Core Team. R: A language and environment for statistical computing. 2022. https://www.r-project.org/
Anderson MJ. A new method for non-parametric multivariate analysis of variance. Austral Ecology. 2001;26:32–46.
Anderson, MJ Permutational multivariate analysis of variance (PERMANOVA). In Wiley StatsRef: Statistics reference online pp. 1–15. John Wiley & Sons, Ltd; 2017. https://doi.org/10.1002/9781118445112.stat07841.
Rubin, DB Multiple imputation for nonresponse in surveys. John Wiley & Sons, Ltd; 1987. https://doi.org/10.1002/9780470316696.
Rubin DB. Multiple imputation after 18+ years. Journal of the American Statistical Association. 1996;91:473–89.
van Buuren S, Groothuis-Oudshoorn K. mice: Multivariate imputation by chained equations in R. Journal of Statistical Software. 2011;45:1–67.
Grund S, Lüdtke O, Robitzsch A. Pooling ANOVA results from multiply imputed datasets: a simulation study. Methodology. 2016;12:75–88.
Oksanen, J, Simpson, G, Blanchet, F, Kindt, R, Legendre, P, Minchin, P, et al. vegan: Community ecology package. R package version 2.8-0, (2025). https://vegandevs.github.io/vegan/.
McEwen BS, Stellar E. Stress and the individual: mechanisms leading to disease. Archives of Internal Medicine. 1993;153:2093–101.
Fries E, Hesse J, Hellhammer J, Hellhammer DH. A new view on hypocortisolism. Psychoneuroendocrinology. 2005;30:1010–6.
Nusslock R, Miller GE. Early-life adversity and physical and emotional health across the lifespan: a neuroimmune network hypothesis. Biological Psychiatry. 2016;80:23–32.
Lo Iacono L, Carola V. The impact of adolescent stress experiences on neurobiological development. Seminars in Cell & Developmental Biology. 2018;77:93–103.
McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiological Reviews. 2007;87:873–904.
Casey BJ, Heller AS, Gee DG, Cohen AO. Development of the emotional brain. Neuroscience Letters. 2019;693:29–34.
Galván A. Adolescent brain development and contextual influences: a decade in review. Journal of Research on Adolescence. 2021;31:843–69.
Juster R-P, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience & Biobehavioral Reviews. 2010;35:2–16.
Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield CH, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. Eur Arch Psychiatry Clin Neurosci. 2006;256:174–86.
Hughes K, Bellis MA, Hardcastle KA, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health. 2017;2:56–e366.
Merrick MT. Vital signs: estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention — 25 states, 2015–2017. MMWR Morb Mortal Wkly Rep. 2019;68:999–1005.
Reid B, Danese A. Challenges in researching the immune pathways between early life adversity and psychopathology. Development and Psychopathology. 2020;32:1597–624.
Teicher MH, Samson JA, Anderson CM, Ohashi K. The effects of childhood maltreatment on brain structure, function and connectivity. Nature Reviews Neuroscience. 2016;17:652–66.
Newman DA. Missing data: five practical guidelines. Organizational Research Methods. 2014;17:372–411.
Acknowledgements
We thank Anna Cichocki, Lauren Costello, Miranda Edwards, Jordan Garcia, Abigail Graber, Madelaine Graber, Melissa Hansen, Vanessa Lopez, Amar Ojha, Holly Pham, Michelle Sanabria, Jill Segarra, Lucinda Sisk, Alexess Sosa, Megan Strickland, Giana Teresi, Johanna Walker and Rachel Weisenburger for their assistance in data collection and management. We thank Tran Nguyen, Yael Rosenberg-Hasson and Holden Maecker for their assistance with the dried blood spot protocol and to Joelle LeMoult and Anne Berens for their assistance with the diurnal cortisol measures. Finally, we thank all our participants and their families for participating in this research.
Funding
This study was supported by grants from the National Institute of Mental Health (R37MH101495 to IHG and K01MH117442 to TCH), the Stanford University Precision Health and Integrated Diagnostics Center (to IHG and TCH), the Stanford Maternal Health and Child Research Institute (to TCH), the Young Investigator Grant from the Brain and Behavior Research Foundation (to JLB), the Stanford Institute for Research in the Social Sciences, the Stanford Psychology Norman Anderson Fund and the National Science Foundation Graduate Research Fellowship Program (to JPY).
Author information
Authors and Affiliations
Contributions
JPY – conceptualization, study design, data processing, statistical analysis, data visualization and manuscript preparation; LRB – conceptualization and study design; YL – data processing and analysis; JLB – study design and analysis; SMC, JJ and ELJ – data collection and processing; TCH – interpretation and funding; IHG – conceptualization, study design, interpretation, funding and supervision. All authors contributed to reviewing and editing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
Study procedures were approved by the Stanford University Institutional Review Board and conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from legal guardians, and assent was obtained from adolescent participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yuan, J.P., Borchers, L.R., Lee, Y. et al. The effects of the COVID-19 pandemic on neurobiological functioning in adolescents. Transl Psychiatry 15, 276 (2025). https://doi.org/10.1038/s41398-025-03485-2
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03485-2