Abstract
Adolescent Self-Injurious Behavior (SIB) is a significant global public health issue, with a lifetime prevalence rate of approximately 13.7%. As awareness of SIB rises, there is an urgent need for effective prediction mechanisms to enable early identification and intervention, reducing the risk of suicide and self-harm attempts. This study, grounded in Psychopathological Network Theory, uses machine learning and network analysis to explore the multidimensional structure of risk factors for adolescent SIB. A survey of 2047 adolescents aged 11 to 17 years in China analyzed 19 variables across physiological, psychological, and social domains. The Entropy Weight Method (EWM) was applied to combine network analysis and machine learning outcomes for a comprehensive risk evaluation. The study identified key risk factors for SIB, including loneliness, ADHD symptoms, Internet addiction, anxiety, depression, affinity for solitude, autistic traits, being bullied. These factors interact within a complex network structure, influencing the occurrence of SIB both directly and indirectly. The integration of EWM, network analysis, and machine learning provides a more precise risk assessment approach for adolescent SIB. The findings offer valuable insights into the causal mechanisms of SIB and emphasize the importance of targeted prevention and intervention strategies.
Similar content being viewed by others
Introduction
Self-injurious behavior (SIB) refers to intentional actions in which individuals cause harm to their own bodies, including suicide preparation, suicide attempts, and self-inflicted injuries. It specifically excludes mere thoughts, intentions, or inclinations toward self-harm that individuals may experience without acting upon them [1, 2]. As societal awareness of SIB increases, it is now recognized as a complex public health issue of global significance, its prevalence worldwide underscoring its intricate nature and urgent need for attention as a public health challenge [3,4,5]. SIB manifests globally at substantial rates, a meta-analysis reported that among 686,672 children and adolescents, the lifetime prevalence rates were 6% for suicide attempts, 22.1% for non-suicidal self-injury, and 13.7% for deliberate self-harm [6]. Besides, SIB can be highly treatment-resistant and the cost of care is burdensome [7]. According to the “Economic Cost of Injury — United States 2019” report [8], self-harm incidents in the United States incurred an economic cost of approximately $0.058 million per incident, whereas the cost attributed to suicide was significantly higher, averaging $9.74 million per individual. Therefore, establishing a multimodal prediction mechanism for early identification and prediction of SIB in adolescents is crucial to reduce the risk of future suicide and self-injury attempts and ensure that adolescents can achieve positive developmental outcomes, while also significantly reducing the macroeconomic burden.
In recent years, psychopathological theory has been applied to explain psychological behavior problems such as SIB. This theory conceptualizes mental disorders as dynamic networks composed of various symptoms and factors, where individual elements interact in a non-linear manner, collectively contributing to the development and persistence of SIB. Individual aspects, such as psychological health [9], emotional regulation capabilities [10,11,12], intertwine with familial environmental factors like perceived family functioning [13], domestic conflicts, parent-child relationship quality, and peer influences, as well as broader socio-cultural, social isolation, and trauma experiences, institutional, and environmental impacts exemplified by events like the COVID-19 pandemic [14,15,16], which directly or indirectly impact the likelihood of SIB. Additionally, pivotal nodes or mediating factors play an even more crucial role within the network of suicide risk, such as mental health issues, social isolation, and trauma experiences, which impact the likelihood of suicidal behavior. This theory underscores the importance of multi-factorial interaction, revealing the multi-dimensional relationships underlying suicidal behavior [17].
Combined with previous studies, we selected some representative factors affecting SIB in a biopsychosocial framework [18, 19]. Physiological factors, such as gender, age, autistic traits, and Attention-Deficit/Hyperactivity Disorder(ADHD) symptoms, significantly influence an individual’s susceptibility to SIB [20,21,22]. Psychological variables, including childhood happiness, loneliness, affinity for solitude, mind wandering, depression, generalized anxiety, and internet addiction, offer insights into the internal emotional and cognitive states that may contribute to SIB [23,24,25]. Additionally, social factors, such as subjective socioeconomic status, childhood economic conditions, nuclear family status, association with deviant peers, experiences of being bullied, co-positive experiences between teachers and students, teacher management of bullying, and childhood trauma, provide an understanding of the external environment and interpersonal relationships affecting behavior [26,27,28,29]. Integrating these variables through a biopsychosocial framework allows for a more comprehensive assessment of the multi-faceted risk factors associated with SIB. This holistic approach not only aligns with the theoretical foundations discussed but also enhances the accuracy of predictions and supports the development of more effective prevention and intervention strategies for SIB [30] (Table 1).
From the perspective of research methods, while research on the risk factors for SIB among adolescents has been extensive, many studies have employed deductive methods, such as mediation and moderation models [31]. Although valuable, these approaches often rely on pre-established hypotheses for verification, which may lead to confirmation bias. To address the limitations of hypothesis testing, we attempt to integrate deductive reasoning with inductive inference. That is, we make hypotheses based on existing literature, guess which risk factors might be associated with SIB, and arrive at results based on data-driven inductive reasoning [32, 33]. This study employs a combination of machine learning and network analysis, methodologies that not only can discover patterns and associations within the data but also avoid the constraints of analysis based on preset hypotheses. Machine learning can handle large datasets, identifying complex, nonlinear, and dynamic relationships, which is particularly advantageous when dealing with multivariate and high-dimensional data. Moreover, network analysis offers a novel perspective for understanding the complex interactions between SIB risk factors, revealing the direct and indirect connections between variables and their roles within the entire network [17, 34]. This approach can provide a more comprehensive and accurate map of risk factors and also help to uncover previously overlooked or deemed insignificant factors. However, both methods have their strengths and limitations. While machine learning is powerful, its “black-box” nature makes the results difficult to interpret. On the other hand, network analysis provides an intuitive visualization of the relationships between variables but may fall short in capturing complex nonlinear interactions. In response, we propose the incorporation of the entropy weight method (EWM) to conduct integrated analysis [35]. The strength of EWM lies in its ability to quantify system uncertainty and effectively merge information from different analytical methods, thereby providing a more comprehensive and reliable assessment of risk factors. In this study, we use EWM to combine with network analysis and machine learning outcomes. By quantifying system uncertainty, EWM synthesizes insights from diverse methodologies, resulting in a more robust risk factor evaluation [36]. While centrality measures in network analysis (such as degree centrality, betweenness centrality, and closeness centrality) reveal the relative importance of risk factors within the network, they often fail to capture the complex nonlinear interactions between variables. By integrating the predictive capabilities of machine learning, EWM assigns dynamic weights to these centrality measures, reflecting not only structural characteristics but also potential nonlinear interactions within the data. This approach highlights the most influential risk factors and enhances the interpretability of machine learning models while preserving the strengths of network analysis. Moreover, this method can identify potential key nodes and edges that traditional approaches might overlook, offering new perspectives for research. For example, by combining factor weight analysis from machine learning models with network centrality, EWM can uncover variables that may have low centrality but high predictive power, thus providing stronger scientific support for a comprehensive understanding of SIB risk factors [19].
In conclusion, investigating SIB of adolescents is essential to understand and improve their mental health. Based on the bio-psycho-social model, entropy method was used to fuse the results of machine learning and network analysis. This study aimed to explore the network structure of risk factors associated with SIB in adolescents, find high-risk nodes, and prioritize their significance. The aim of this study is to provide a more comprehensive and accurate theoretical basis and practical application for the development of targeted and effective prevention and intervention strategies for SIB in adolescents.
Methods
Participants
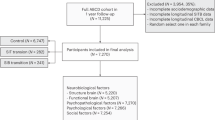
In the investigation, questionnaires were systematically distributed among various secondary educational institutions in Hunan Province, China. We obtained the consent of the school administration, teachers and parents before issuing the questionnaire, and informed the students that they had the right to withdraw and refuse to answer the questionnaire at any time during the process of issuing the questionnaire. To ensure the uniformity and dependability of the gathered data, the principal investigator provided comprehensive training to classroom instructors on a uniform questionnaire administration protocol. This training aimed to minimize instructional disruption, with questionnaires being filled out during designated study periods. Subsequently, instructors collected and forwarded the completed surveys to the research team, adhering to a structured process.To ensure the validity and relevance of the data, specific inclusion and exclusion criteria were applied. Participants were eligible if they were enrolled as full-time students in secondary educational institutions within Hunan Province and were aged between 11 and 17 years. Exclusion criteria included students with cognitive or physical impairments that would hinder their ability to complete the questionnaire accurately, as well as students who had been absent during the survey administration. Additionally, students who declined to provide informed consent or withdrew from the study at any point during the process were also excluded from the final dataset. This ensured that the sample was representative of the target population while maintaining ethical standards in participant selection.
This rigorous approach to data collection resulted in the acquisition of 2047 legitimate responses from a demographic of students aged between 11 and 17 years, boasting an average age of 13.69 years (SD = 1.55). The gender distribution of the participants was 1088 males and 959 females, including 1259 junior high and 788 senior high students, providing a representative cross-section of adolescents within the specified age range. Ethical approval for this study was granted by the Ethics Committee of the National Clinical Research Center, Xiangya Second Hospital, Central South University (Approval No. (2023) Guo Lun Shen [Ke] No.036), ensuring compliance with ethical standards.
Measurement
Adolescent SIB, based on aggregated items related to self-harm, suicide attempts, and suicide preparation, is a concise and effective tool for assessing the frequency of SIB in adolescents. This tool includes items such as “Have you ever engaged in self-harm or attempted suicide?” to evaluate the risk of self-harm and suicidal behaviors among adolescents. In this study, responses were scored on a five-point scale according to frequency, with binary scoring applied during data processing. The study reports a Cronbach’s alpha of 0.85 for the simple scale composed of three items. Information on the measurement of other variables can be found in the Supplementary Materials.
Sample size estimation
According to the rule of thumb in machine learning, the sample size should be at least 10 times the number of features to ensure the stability and effectiveness of the model. In this study, the machine learning model has 19 features, so the required minimum sample size is:
In network analysis, a minimum sample size of 500 is generally recommended to ensure the stability and significance of network structure analysis. Considering 19 nodes in the network analysis, the following formula is used to calculate the minimum sample size:
By substituting the significance level (α = 0.05, z_(α/2) = 1.96), the expected effect size (0.15), and the assumed network variance (1), the calculated minimum sample size is approximately 342 samples. The sample size in this study is 2047, which is sufficient to support stable machine learning and network analysis, ensuring the reliability and accuracy of the results.
Statistical process
Firstly, before machine learning, we preprocessed data involves cleaning the raw data, standardizing it, and dividing the dataset. The data cleaning process includes removing samples with significant missing values, handling outliers and duplicates, and imputing missing values. Continuous variables are standardized to ensure that their mean is 0 and their standard deviation is 1, allowing for comparability across different scales in subsequent analyses. Categorical variables are encoded into numerical formats. The dataset was then split into training and testing subsets in a 7:3 ratio to enable robust model training and evaluation. We applied six machine learning algorithms—Random Forest (RF), HistGradientBoosting (HGB), Support Vector Machine (SVM), Multi-Layer Perceptron (MLP), LightGBM (LGBM), and K-Nearest Neighbors (KNN)—to predict SIB. Each model’s performance was assessed using several metrics: accuracy, AUC (Area Under the ROC Curve), sensitivity, positive predictive value (PPV), and Brier Score. Additional details are provided in the Supplementary Materials. This entire process was carried out using Python 3.11.7 and the “Scikit-learn” package.
Secondly, we conduct the network analysis in R Statistical Software [37]. The qgraph and bootnet R packages [38, 39] were utilized to estimate the network structure of SIB-related variables and the calculation of network centrality indicators. The EBICglasso estimator (tuning = 0.5) is used to generate a sparse network model, simplifying the network structure and highlighting the most important connections between variables. Centrality indicators such as degree centrality, betweenness centrality, and closeness centrality are used to evaluate the relative importance of each variable within the network. A Network Comparison Test was conducted with the NetworkComparisonTest R package [40], examining structural invariance, global strength, and edge invariance.
Thirdly, following the machine learning and network analysis, we use EWM to integrate the importance scores from the machine learning model with the centrality indicators from the network analysis. By calculating the entropy values for each variable in these two sets of results and combining them using a weighted sum approach, a composite ranking is generated. This allows for the identification of key variables that are both strong predictors and central to the network. EWM is a commonly used method for calculating weights in multi-indicator comprehensive evaluations (Fig. 1). The detailed steps and formulas of the EWM are provided in the Supplementary Materials.
Ethics approval and consent to participate
All procedures involving human participants were conducted in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Ethical approval for this study was granted by the Ethics Committee of the National Clinical Research Center, Xiangya Second Hospital, Central South University (Approval No. (2023) Guo Lun Shen [Ke] No.036). Informed consent was obtained from all participants prior to their inclusion in the study, and the term “informed consent” was explicitly communicated and confirmed during the data collection process. For underage participants, written informed consent was obtained from their legal guardians through coordination with the respective schools and educational authorities.
Results
Demographic variables
The participants in the study ranged in age from 11 to 17 years, with an average age of 13.69 years (SD = 1.55). The sample consisted of 1088 males, accounting for 53.15%, and 959 females, representing 46.85%. High school students made up 61.50%, numbering 1259, while junior high school students constituted 38.50%, totaling 788 individuals. There were 728 only children, comprising 35.56%, whereas 1319, or 64.44%, had siblings. Ethnic minorities were represented by 133 individuals or 6.49%. The majority resided in urban areas, with 1843 people, or 90.03%, followed by those living in villages, at 7.77% with 159 individuals, and lastly, those from urban-rural fringe areas, at 2.20%, amounting to 45 people (see Table 2).
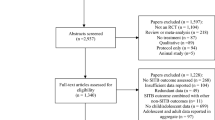
Machine learning
Based on the selected variables, six suitable machine learning algorithms were used to train the machine learning model. All models demonstrated commendable predictive capabilities for SIB (Table 3). Among them, the Random Forest algorithm emerged to be the most effective one, achieving an accuracy of 0.748 and an AUC of 0.814. The KNN algorithm, despite being relatively less effective, still achieved an accuracy of 0.728 and an AUC value of 0.757, indicating that all six models exhibited good overall fitting performance.
Given the outstanding performance of the Random Forest (RF) algorithm, we utilized it to evaluate the feature importance. This method enables a more detailed investigation into the key factors that predict SIB (Table 4). Figure 2 presents the ranked order of feature importance obtained from applying the RF algorithm to the classification task of predicting SIB within our study. In the figure, feelings of loneliness (L), ADHD, and being bullied (BB) are identified as the top three most important factors to predict SIB.
Network analysis
Figure 3 shows the network structure of non-SIB and SIB groups. Both groups consist of 19 nodes, each with 81 non-zero edges out of a possible 171, resulting in a sparsity of 0.530. This indicates that approximately 53% of potential connections between variables are absent in both groups, reflecting a moderate level of network sparsity. While the overall network structures are similar, the specific connections and the strength of associations between variables may differ, warranting further analysis.
By examining the edge weight matrix, we identified notable differences in variable interactions between the non-SIB and SIB groups. In the SIB group, strong positive correlations were observed between autistic traits and ADHD symptoms (0.272 and 0.177, respectively), as well as between mind wandering and ADHD symptoms (0.243), and depression and anxiety (0.439). The SIB group also showed significant associations between internet addiction and anxiety (0.301), and loneliness and internet addiction (0.171), indicating their importance in the SIB risk network. Positive teacher-student interactions were also relevant, with a weight of 0.195 between these interactions and ADHD symptoms, suggesting their potential role in mitigating SIB. Negative connections included the inverse relationship between gender and deviant peer association (−0.148), and gender and bullying (−0.128).
Comparative analysis of network centrality (Fig. 4) revealed that ADHD symptoms exhibited high centrality in both groups, particularly in the SIB group (1.852), indicating its strong predictive value. Loneliness (1.585), autistic traits (0.877), and depression (0.971) also had high centrality in the SIB group, highlighting their critical roles in SIB. Mind wandering had a centrality of 0.749, suggesting its influence. In contrast, variables like Nuclear Family Status (−1.155), Objective Economic Status (−0.970), and Childhood Happiness (−0.997) showed low centrality, indicating a more peripheral role in the SIB network. Positive teacher-student experiences had a centrality of 0.286, hinting at its emerging importance in the SIB context.
To further validate the robustness of our network analysis results, we conducted a bootstrap analysis with 1000 resamples, assessing the stability of edge weights and centrality values for each node. The bootstrap method, by repeatedly sampling from the original dataset and recalculating the edge weights and centrality metrics, allowed us to evaluate the stability and reliability of the observed relationships and centralities across the network (Figure S1 and S2).
Entropy analysis
In this study, we used EWM to calculate the Comprehensive Scores for various features to assess their relative importance and centrality within the feature network for predicting SIB (Fig. 5). The results showed that Loneliness (L) had the highest Comprehensive Score of 0.856, underscoring its critical importance in SIB prediction. ADHD Symptoms and Internet Addiction (IA) followed with scores of 0.825 and 0.692, indicating a key role in predicting SIB. Additionally, Depression(DEP), Anxiety (ANX), Affinity for Solitude (AS), Autistic Traits(AT), and Being Bullied(BB) had scores of 0.523, 0.510, 0.471, 0.464, and 0.438, respectively, which also showed their influence in SIB prediction. Variables with Comprehensive Scores lower than 0.4 were considered relatively less important, meaning they had a smaller influence in predicting SIB.
Discussion
The current study investigates the complex and multifaceted nature of SIB among adolescents, emphasizing the interconnectedness of psychological, physiological, and social factors. Understanding these risk factors is essential for developing more effective prevention and intervention strategies. This section explores the key findings regarding the central psychological, physiological, and social elements contributing to adolescent SIB, and reflects on the research methods used to capture the intricate dynamics of these risk factors. Through an integrated approach combining machine learning, network analysis, and entropy weighting, we offer a comprehensive view of the factors influencing SIB and discuss their implications for both theory and practice.
Psychological factors and SIB
Loneliness, depression, and anxiety are central psychological factors driving adolescent SIB. Across all analyses, loneliness exhibited exceptionally high centrality, indicating its dominant role within the SIB risk network. Loneliness is not merely a perceived sense of social isolation but is also linked to significant neurological changes in brain regions responsible for social processing, such as the superior temporal sulcus and anterior cingulate cortex [41]. These neurological changes may impair emotional regulation, leading to social cognitive biases and gradually accumulating as chronic psychological stress [42]. Over time, this chronic stress and the buildup of negative emotions can exacerbate internal distress, ultimately making SIB a means of escaping or alleviating emotional turmoil.Affinity for solitude may lead to SIB because individuals are more likely to confront negative emotions when alone and lack external support to effectively regulate these emotions [43]. Although solitude does not equate to loneliness, prolonged solitude may cause individuals to become immersed in self-criticism and negative feelings, which can lead to self-harm as a way of coping with emotional distress [44]. Depression and anxiety symptoms are typically accompanied by persistent negative emotions [45], such as profound sadness and intense anxiety, which may drive individuals to engage in SIB as an attempt to regulate or distract from these overwhelming feelings [46]. Additionally, depression and anxiety can lead to cognitive distortions, such as negative self-evaluation, extreme pessimism about the future, and underestimating one’s problem-solving abilities, further amplifying psychological distress and increasing the risk of SIB [47]. Therefore, these psychological factors do not operate in isolation but interact in complex ways to collectively drive the occurrence of SIB.
Physiological factors and SIB
In the analysis of physiological factors, symptoms of ADHD and autistic traits are key to understanding adolescent SIB. ADHD, as a neurodevelopmental disorder, profoundly impacts self-control, particularly in regulating impulses and maintaining attention, often attributed to frontal lobe dysfunction [48, 49]. This impulsivity may lead adolescents to resort to SIB as a quick means to relieve internal emotional fluctuations and conflicts [50]. Although ADHD symptoms in this study are treated as behavioral traits rather than clinical diagnoses, their significant influence on SIB aligns with extensive literature identifying ADHD as a risk factor for SIB [51]. On the other hand, autistic traits primarily affect adolescents’ social and communication skills, making them more prone to misunderstanding and rejection, which can result in severe psychological distress [52]. Particularly in the context of intense loneliness, these social impairments render autistic adolescents more vulnerable, potentially leading them to use SIB as an extreme coping mechanism to deal with complex emotions [53]. More concerning is that adolescents may encounter online content that encourages self-injury, such as the “Blue Whale Game,” which normalizes and even promotes SIB behavior, making it easier for adolescents to perceive self-harm as a way to resolve their distress [54]. These physiological factors reveal how neurodevelopmental characteristics can influence psychological and behavioral processes, ultimately contributing to the occurrence of SIB.
Social factors and SIB
Social factors also play a crucial role within the SIB risk network, particularly experiences of bullying significantly increase the risk of developing SIB in adolescents. Among adolescents experiencing various forms of bullying victimization (physical, verbal, and relational), the risk of engaging in self-injurious behavior is significantly elevated. This increased vulnerability is often compounded by additional challenges such as depression and a lack of social support, which further exacerbate the impact of these negative experiences and contribute to the development of unhealthy coping mechanisms like self-harm [55]. This social factor illustrates how environmental and experiential elements can alter an individual’s psychological state, ultimately leading to SIB.
Reflection on research methods
Many studies exploring SIB risk factors in the existing literature rely on traditional statistical methods, such as regression analysis or mediation/moderation models. While these methods effectively reveal direct relationships between variables, they are significantly limited in capturing the complex nonlinear and dynamic interactions between variables [56]. Moreover, traditional approaches often assume the independence of risk factors, overlooking the intricate network structure of interactions across social, psychological, and physiological dimensions [57]. Although some studies have attempted to apply single machine learning methods [58] or text analysis methods [59] to detect suicide risk, the lack of interpretability and systematic integration often hampers the ability to provide actionable intervention recommendations. Additionally, existing research has rarely considered how to effectively combine results from various analytical methods to enhance the robustness and accuracy of conclusions [60]. This study addresses these gaps by integrating multiple data analysis tools to reveal the complex risk structure of adolescent SIB. First, machine learning techniques are employed to identify and predict key risk factors for SIB, offering the advantage of handling multidimensional and high-complexity datasets and capturing nonlinear and dynamic relationships [61]. However, the “black-box” nature of machine learning [62] poses challenges for model interpretability, which is why this study also introduces network analysis to construct a relational network among variables, visually displaying the interactions and centrality of various factors within the risk network. By incorporating the EWM, the study integrates results from both machine learning and network analysis, assigning dynamic weights to variables to derive a more comprehensive and reliable ranking of key risk factors [63, 64].
Entropy weighting has been widely used across disciplines like economics and environmental studies to integrate weights from multiple criteria, making it suitable for complex datasets. It assigns importance to variables based on their distribution, ensuring an objective combination of results from machine learning and network analysis. This method provides a more reliable ranking of risk factors by considering each factor’s contribution proportionately.Future studies should consider the quality and consistency of data, as inaccurate data can lead to biased results. Researchers should also be cautious of overfitting in machine learning models, using cross-validation techniques to improve generalizability. Lastly, while this approach improves accuracy, enhancing model interpretability will be crucial for deriving practical, actionable insights.
Implications
Psychological implications
At the psychological level, loneliness, and symptoms of depression and anxiety have been identified as core risk factors for adolescent SIB. Loneliness is one of the most significant predictors [65, 66], reflecting not only emotional isolation but also the accompanying psychological stress and emotional distress, which significantly increase the risk of SIB [67, 68]. Schools and communities can mitigate the negative impact of loneliness on adolescents’ mental health by organizing social activities and establishing supportive groups. For example, the “Circle of Friends” program has demonstrated significant improvements in participants’ social integration and mental health through peer support and group interaction [69]. Additionally, depression and anxiety symptoms are closely linked to SIB, often manifesting as persistent negative emotions and cognitive distortions, such as pessimism about the future and negative self-evaluation [23]. A combination of cognitive-behavioral therapy (CBT) and pharmacotherapy has been widely proven to effectively alleviate these symptoms, thereby reducing the risk of SIB [70].
Physiological implications
On the physiological front, symptoms of ADHD and autistic traits have a pronounced impact on SIB. ADHD symptoms, characterized by impulsivity and inattention, are often associated with frontal lobe dysfunction, making adolescents more prone to impulsive, often self-destructive behaviors to cope with emotional fluctuations [48]. Interventions combining behavioral therapy, pharmacotherapy, and CBT have proven effective in reducing ADHD symptoms, thereby lowering the incidence of SIB [71]. For instance, the “Family Training Program” has shown significant efficacy in reducing behavioral problems in children with ADHD, improving both impulse control and emotional management [72]. Autistic traits primarily affect social and communication skills, leading to greater social exclusion and misunderstanding, which exacerbates psychological distress [52]. Particularly in cases of intense loneliness, these social impairments make autistic adolescents more likely to adopt SIB as a coping mechanism [73]. Interventions for this issue should focus on social skills training and personalized support plans, such as Applied Behavior Analysis (ABA) and social stories [74], which have been effective in improving social interaction and reducing social exclusion in autistic adolescents [75].
Social implications
Social factors also play a critical role in SIB risk, with the impact of bullying and childhood abuse being particularly significant. Bullying, especially during childhood, has profound effects on adolescent mental health. Studies indicate that adolescents who experience early bullying face a higher risk of SIB [76]. The sustained psychological stress and social rejection caused by bullying severely damage the victims’ self-esteem and self-efficacy [77], increasing their negative emotions and depressive symptoms, which often drive them to seek emotional relief through SIB. Schools should actively create supportive environments and implement comprehensive anti-bullying programs, such as Finland’s “KiVa” anti-bullying program, which has significantly reduced bullying incidents and improved overall school climate through counseling services and peer support [78]. For adolescents who have experienced childhood abuse, trauma-informed care, such as Trauma-Focused Cognitive Behavioral Therapy (TF-CBT), is a crucial intervention, helping them process and overcome trauma, thereby reducing the incidence of SIB [79].
Limitations and future directions
Despite uncovering the complex risk structure of adolescent SIB through the integration of multiple data analysis tools, this study has several limitations. First, the reliance on cross-sectional data means that we can only observe associations between variables at a single point in time, without establishing causality or tracking their dynamic changes over time. Future research should consider longitudinal designs to explore the causal relationships between risk factors and SIB more deeply. Second, much of the data in this study is based on self-reporting, which may introduce social desirability bias or memory distortion, potentially affecting the accuracy of the results. Future studies could incorporate physiological measurements or third-party assessments to provide more objective data. Additionally, while we employed advanced analytical tools such as machine learning and network analysis, the complexity of these methods may limit their interpretability and practical application in clinical settings. Although the development of Explainable AI (XAI) can partially address this issue, further efforts are needed to make these methods more practical and user-friendly in clinical practice [80].
Future research should address current limitations and enhance understanding of SIB through longitudinal studies, which can clarify causal links and developmental paths related to risk factors. To enhance the accuracy and reliability, future research should attempt to integrate multiple data sources, including physiological data, behavioral observations, and third-party reports, to offer a more comprehensive perspective on SIB. Additionally, methodologically, further exploration of Explainable AI (XAI) could help us better understand the outputs of complex models, making the research findings more accessible and applicable to clinicians and policymakers. Ultimately, these efforts will provide a solid scientific foundation for developing more precise and personalized intervention strategies, helping to more effectively prevent and mitigate adolescent SIB and improve their mental health and social adaptability.
Conclusion
This study, through the comprehensive application of machine learning, network analysis, and the Entropy Weight Method, has revealed the complex risk structure of adolescent SIB, highlighting the multidimensional interactions of psychological, physiological, and social factors. The findings indicate that loneliness, ADHD symptoms, Internet addiction, anxiety, depression, affinity for solitude, autistic traits, being bullied play crucial roles in the occurrence of SIB. Although this study provides important theoretical and empirical support for understanding the complex etiology of SIB, challenges remain in establishing causality, addressing the limitations of self-report data, and improving the interpretability of models. Future research should deepen the understanding of SIB through longitudinal designs, multi-source data integration, and the application of Explainable AI techniques, providing a more robust scientific basis for developing personalized intervention strategies. Through these efforts, we hope to offer stronger support for the mental health and social adaptation of adolescents, thereby effectively reducing the incidence of SIB.
Code availability
All Python and R code used in our study is available at the following link: https://osf.io/6gceu.
References
Huisman S, Mulder P, Kuijk J, Kerstholt M, van Eeghen A, Leenders A, et al. Self-injurious behavior. Neuroscience & Biobehavioral Reviews. 2018;84:483–91.
Wen X, Qu D, Zhang X, Wang Y, Cui Z, Zhang X, et al. The transition trajectories of self-injurious thoughts and behaviours among children from a biopsychosocial perspective. Nat Mental Health. 2023;1:782–91.
Gillies D, Christou MA, Dixon AC, Featherston OJ, Rapti I, Garcia-Anguita A, et al. Prevalence and characteristics of self-harm in adolescents: Meta-analyses of community-based studies 1990–2015. J Am Acad Child Adolesc Psychiatry. 2018;57:733–41.
Lucena NL, Rossi TA, Azevedo LMG, Pereira M. Self-injury prevalence in adolescents: a global systematic review and meta-analysis. Child Youth Serv Rev. 2022;142:106634.
Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet (London, England). 2016;387:1227–39.
Lim K-S, Wong C, McIntyre R, Wang J, Zhang Z, Tran B, et al. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int J Environ Res Public Health. 2019;16:4581. https://doi.org/10.3390/ijerph16224581
Dimian AF, Symons FJ. A systematic review of risk for the development and persistence of self-injurious behavior in intellectual and developmental disabilities. Clin Psychol Rev. 2022;94:102158.
Peterson C, Miller GF, Barnett SBL, Florence C. Economic cost of injury — United States, 2019. Morbidity and Mortality Weekly Report. 2021;70:1655–9.
Lundberg J, Cars T, Lampa E, Ekholm Selling K, Leval A, Gannedahl A, et al. Determinants and outcomes of suicidal behavior among patients with major depressive disorder. JAMA Psychiatry. 2023;80:1218–25.
Calvete E, Royuela-Colomer E, Maruottolo C. Emotion dysregulation and mindfulness in non-suicidal self-injury. Psychiatry Res. 2022;314:114691.
Liu S, You J, Ying J, Li X, Shi Q. Emotion reactivity, nonsuicidal self-injury, and regulatory emotional self-efficacy: a moderated mediation model of suicide ideation. Journal of Affective Disorders. 2020;266:82–9.
Swee G, Shochet I, Cockshaw W, Hides L. Emotion regulation as a risk factor for suicide ideation among adolescents and young adults: the mediating role of belongingness. J Youth Adolescence. 2020;49:2265–74.
Lipschitz JM, Yen S, Weinstock LM, Spirito A. Adolescent and caregiver perception of family functioning: relation to suicide ideation and attempts. Psychiatry Research. 2012;200:400–3.
Farooq S, Tunmore J, Wajid Ali M, Ayub M. Suicide, self-harm and suicidal ideation during COVID-19: a systematic review. Psychiatry Res. 2021;306:114228.
Kapur N, Clements C, Appleby L, Hawton K, Steeg S, Waters K, et al. Effects of the COVID-19 pandemic on self-harm. The Lancet Psychiatry. 2021;8:e4.
Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nature Human Behaviour. 2021;5:229–38.
Kirtley OJ, Hussey I, Marzano L. Exposure to and experience of self-harm and self-harm related content: an exploratory network analysis. Psychiatry Res. 2021;295:113572.
Askew M, Byrne MW. Biopsychosocial approach to treating self-injurious behaviors: an adolescent case study. J Child Adolesc Psychiatr Nurs. 2009;22:115–9.
Chan L, Simmons C, Tillem S, Conley M, Brazil IA, Baskin-Sommers A. Classifying conduct disorder using a biopsychosocial model and machine learning method. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging. 2023;8:599–608.
Tang H, Zhang Z, Chen H, Chen H, Chen X, Li S, et al. Core items selection and psychometric properties of the adult attention-deficit hyperactivity disorder self-report scale-chinese short version (ASRS-CSV). Asian Journal of Psychiatry. 2024;99:104136.
Ye Y, Zhang Z, Tao Z, Liping C, Wang Y, Chen H, et al. Academic pressure and psychological imbalance in high school students: predictors of depression via polynomial regression and response surface analysis. Psychology Research and Behavior Management. 2025;18:15–23.
Zhang Z, Qiu A, Zhang X, Zhao Y, Yuan L, Yi J, et al. Gender differences in the mental symptom network of high school students in Shanghai, China: a network analysis. BMC Public Health. 2024;24:2719.
Ye C, Ye B, Zhang Z. The relationship between unpredictability in childhood and depression among college students: the mediating roles of coping style and resilience. BMC Psychol. 2024;12:333.
Zhang Z, Lin R, Qiu A, Wu H, Wu S, Zhang L, et al. Application of DASS-21 in Chinese students: invariance testing and network analysis. BMC Public Health. 2024;24:2934.
Zhang Z, Tang H, Li X, Chen H, Chen X, Liu J, et al. The influence of neuroticism on insomnia: the chain mediating effect of mind wandering and symptom rumination. Sleep Medicine. 2023;112:197–202.
Mangnall J, Yurkovich E. A literature review of deliberate self-harm. Perspect Psychiatr Care. 2008;44:175–84.
Rahman F, Webb RT, Wittkowski A. Risk factors for self-harm repetition in adolescents: a systematic review. Clin Psychol Rev. 2021;88:102048.
Song C, Zhang Z, Wei K, Xie H. Divergent school bullying experiences and mental health: the mediating role of self-stigma among Chinese LGB adolescents and young adults. Child Abuse & Neglect. 2025;161:107306.
Zhong Y, Lai S, Hu A, Liao Y, Li Y, Zhang Z, et al. Sex differences in prevalence and clinical correlates of internet addiction among Chinese adolescents with schizophrenia. BMC Psychiatry. 2024;24:258.
Hawton K, Saunders KE, O’Connor RC. Self-harm and suicide in adolescents. Lancet. 2012;379:2373–82. https://doi.org/10.1016/S0140-6736(12)60322-5.
Baker AC, Wallander JL, Elliott MN, Schuster MA. Non-suicidal self-injury among adolescents: a structural model with socioecological connectedness, bullying victimization, and depression. Child Psychiatry Hum Dev. 2023;54:1190–208.
Glenn CR, Kleiman EM, Kellerman J, Pollak O, Cha CB, Esposito EC, et al. Annual research review: a meta-analytic review of worldwide suicide rates in adolescents. Journal of Child Psychology and Psychiatry. 2020;61:294–308.
Robinson J, Bailey E, Witt K, Stefanac N, Milner A, Currier D, et al. What works in youth suicide prevention? A systematic review and meta-analysis. eClinicalMedicine. 2018;4:52–91.
Misiak B, Szewczuk-Bogusławska M, Samochowiec J, Moustafa AA, Gawęda Ł. Unraveling the complexity of associations between a history of childhood trauma, psychotic-like experiences, depression and non-suicidal self-injury: a network analysis. J Affect Disord. 2023;337:11–7.
Yuan W, Yang M, Liu D, Fu X, Yu L, Wang K. Evaluation of the applicability of hospital-affiliated green spaces to patient recovery using the entropy weight method and grey relational analysis. Front Public Health. 2024;12:1362884.
Dong F, Yin J, Xiang J, Chang Z, Gu T, Han F. EWM-FCE-ODM-based evaluation of smart community construction: from the perspective of residents’ sense of gain. Sustainability. 2023;15:6587.
R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing: Vienna, Austria, 2024 https://www.R-project.org/.
Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: network visualizations of relationships in psychometric data. Journal of Statistical Software. 2012;48:1–18.
Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: a tutorial paper. Behavior Research Methods. 2018;50:195–212.
Van Borkulo CD, Van Bork R, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, et al. Comparing network structures on three aspects: a permutation test. Psychological Methods. 2023;28:1273–85.
Markauskaite L, Marrone R, Poquet O, Knight S, Martinez-Maldonado R, Howard S, et al. Rethinking the entwinement between artificial intelligence and human learning: what capabilities do learners need for a world with AI? Computers and Education: Artificial Intelligence. 2022;3:100056. https://doi.org/10.1016/j.caeai.2022.100056.
Frieden TR, Lee CT, Lamorde M, Nielsen M, McClelland A, Tangcharoensathien V. The road to achieving epidemic-ready primary health care. The Lancet Public Health. 2023;8:e383–e390.
Kusnadi GA. Self injury in adolescents that may disturb the mental health. Psikoeduko: Jurnal Psikologi Edukasi dan Konseling. 2021;1:11–23.
Gandhi A, Luyckx K, Goossens L, Maitra S, Claes L. Association between non-suicidal self-injury, parents and peers related loneliness, and attitude towards aloneness in flemish adolescents: an empirical note. Psychol Belg. 2018;58:3–12.
Suveg C, Hoffman B, Zeman JL, Thomassin K. Common and specific emotion-related predictors of anxious and depressive symptoms in youth. Child Psychiatry Hum Dev. 2009;40:223–39.
Nixon MK, Cloutier PF, Aggarwal S. Affect regulation and addictive aspects of repetitive self-injury in hospitalized adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1333–41.
Yesilyaprak N, Batmaz S, Yildiz M, Songur E, Aslan EA. Automatic thoughts, cognitive distortions, dysfunctional attitudes, core beliefs, and ruminative response styles in unipolar major depressive disorder and bipolar disorder: a comparative study. Psychiatry and Clinical Psychopharmacology. 2019;29:854–63.
Allely CS. The association of ADHD symptoms to self-harm behaviours: a systematic PRISMA review. BMC Psychiatry. 2014;14:133.
Chen W, Taylor E Resilience and self-control impairment. In: Goldstein S, Brooks RB (editors). Handbook of Resilience in Children. Cham: Springer International Publishing; 2023. pp. 175–211.
Arens AM, Gaher RM, Simons JS. Child maltreatment and deliberate self‐harm among college students: testing mediation and moderation models for impulsivity. American Journal of Orthopsychiatry. 2012;82:328–37.
Jaisle EM, Groves NB, Black KE, Kofler MJ. Linking ADHD and ASD symptomatology with social impairment: the role of emotion dysregulation. Res Child Adolesc Psychopathol. 2023;51:3–16.
Moseley RL, Gregory NJ, Smith P, Allison C, Baron-Cohen S. Links between self-injury and suicidality in autism. Molecular Autism. 2020;11:14.
Rattaz C, Michelon C, Baghdadli A. Symptom severity as a risk factor for self-injurious behaviours in adolescents with autism spectrum disorders. Journal of Intellectual Disability Research. 2015;59:730–41.
Mukhra R, Baryah N, Krishan K, Kanchan T. Blue whale challenge’: a game or crime? Sci Eng Ethics. 2019;25:285–91.
Brunstein Klomek A, Snir A, Apter A, Carli V, Wasserman C, Hadlaczky G, et al. Association between victimization by bullying and direct self injurious behavior among adolescence in Europe: a ten-country study. Eur Child Adolesc Psychiatry. 2016;25:1183–93.
Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: observations, recommendations, and implementation. Behaviour Research and Therapy. 2017;98:39–57.
McNally RJ. Network analysis of psychopathology: controversies and challenges. Annual Review of Clinical Psychology. 2021;17:31–53.
Niu W, Feng Y, Xu S, Wilson A, Jin Y, Ma Z, et al. Revealing suicide risk of young adults based on comprehensive measurements using decision tree classification. Comput Hum Behav. 2024;158:108272.
Abdulsalam A, Alhothali A. Suicidal ideation detection on social media: a review of machine learning methods. Soc Netw Anal Min 2024; 14: 188.
Dai W, Wang H, Yang Z. Discovery of cybervictimization-associated factors among adolescents: using machine learning and network analysis. Comput Hum Behav. 2025;162:108469.
Rajendra P, Brahmajirao V. Modeling of dynamical systems through deep learning. Biophys Rev. 2020;12:1311–20.
Watson DS, Krutzinna J, Bruce IN, Griffiths CE, McInnes IB, Barnes MR, et al. Clinical applications of machine learning algorithms: beyond the black box. Br Med J. 2019;364:l886.
Li G, Zhang L, Wang Y, Kang Z. Critical node identification method of power grid based on the improved entropy weight method. Electronics. 2023;12:2439.
Xi H, Li Z, Han J, Shen D, Li N, Long Y, et al. Evaluating the capability of municipal solid waste separation in China based on AHP-EWM and BP neural network. Waste Management. 2022;139:208–16.
Li Y, Zhang Z, Cui L, Wang Y, Guo H, Wang J, et al. The role of mind wandering and anxiety in the association between internet addiction and hyperactivity-impulsivity: a serial mediation model. BMC Psychol. 2025;13:345.
Zhou J, Zhang Z, Li S, Chen H, Chen X, Tang H, et al. Childhood maltreatment influences coping in youths with major depression and bipolar depression through resilience and impulsivity. Sci Rep. 2025;15:11441.
Geulayov G, Mansfield K, Jindra C, Hawton K, Fazel M. Loneliness and self-harm in adolescents during the first national COVID-19 lockdown: results from a survey of 10,000 secondary school pupils in England. Curr Psychol. 2024;43:14063–74.
John A, Lee SC, Solomon S, Crepaz-Keay D, McDaid S, Morton A, et al. Loneliness, coping, suicidal thoughts and self-harm during the COVID-19 pandemic: a repeat cross-sectional UK population survey. BMJ Open. 2021;11:e048123.
Hassani S, Alves S, Avramidis E, Schwab S. The Circle of Friends intervention: a research synthesis. European Journal of Special Needs Education. 2022;37:535–53.
Sinyor M, Williams M, Mitchell R, Zaheer R, Bryan CJ, Schaffer A, et al. Cognitive behavioral therapy for suicide prevention in youth admitted to hospital following an episode of self-harm: a pilot randomized controlled trial. Journal of Affective Disorders. 2020;266:686–94.
Li Y, Zhang L. Efficacy of cognitive behavioral therapy combined with pharmacotherapy versus pharmacotherapy alone in adult ADHD: a systematic review and meta-analysis. J Atten Disord. 2024;28:279–92.
Vaziri S, Kashani FL, Sorati M. Effectiveness of family training in reduced symptoms of the children with attention deficit hyperactivity disorder. Procedia - Social and Behavioral Sciences. 2014;128:337–42.
Blanchard A, Chihuri S, DiGuiseppi CG, Li G. Risk of self-harm in children and adults with autism spectrum disorder: a systematic review and meta-analysis. JAMA Network Open. 2021;4:e2130272.
Kokina A, Kern L. Social StoryTM interventions for students with autism spectrum disorders: a meta-analysis. J Autism Dev Disord. 2010;40:812–26.
Nomi JS, Molnar-Szakacs I, Uddin LQ. Insular function in autism: update and future directions in neuroimaging and interventions. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2019;89:412–26.
Fisher HL, Moffitt TE, Houts RM, Belsky DW, Arseneault L, Caspi A. Bullying victimisation and risk of self harm in early adolescence: longitudinal cohort study. BMJ. 2012;344:e2683.
Cao Y, Yang F. Self-efficacy and problem behaviors of school bully victims: evidence from rural China. J Child Fam Stud. 2018;27:3241–9.
Garandeau CF, Lee IA, Salmivalli C. Differential effects of the KiVa anti-bullying program on popular and unpopular bullies. Journal of Applied Developmental Psychology. 2014;35:44–50.
Peters W, Rice S, Cohen J, Murray L, Schley C, Alvarez-Jimenez M, et al. Trauma-focused cognitive–behavioral therapy (TF-CBT) for interpersonal trauma in transitional-aged youth. Psychological Trauma: Theory, Research, Practice, and Policy. 2021;13:313–21.
Asgharian Rezaei A, Munoz J, Jalili M, Khayyam H. A machine learning-based approach for vital node identification in complex networks. Expert Systems with Applications. 2023;214:119086.
Funding
This study was supported by the STI2030-Major Projects (2021ZD0200700; XW and JZ, co-PIs), the National Natural Science Foundation of China (82471568), and the Postdoctoral Fellowship Program of CPSF (GZC20233170) for Huijuan Guo. The funding sources had no role in the study design, data collection, analysis, interpretation of data, the writing of the report, or the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
Ethics approval for this study was obtained from the Ethics Committee of the National Clinical Medical Research Center at the Second Xiangya Hospital, Central South University(LYF2022031).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Z., Chen, H., Ye, Y. et al. Entropy-based risk network identification in adolescent self-injurious behavior using machine learning and network analysis. Transl Psychiatry 15, 299 (2025). https://doi.org/10.1038/s41398-025-03511-3
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41398-025-03511-3