Abstract
Aim
The aim of this study was to study the effect of Molar Incisor Hypomineralisation (MIH) on Oral Health-Related Quality of Life (OHRQoL) in children at the mixed dentition stage and correlate it with their caries experience.
Subjects and methods
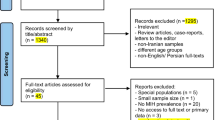
One hundred two children aged from 8 to 10 years were recruited, 51 with MIH and 51 as control. Caries experience was recorded using DMFT/deft and ICDAS II. MIH-TNI index was used for classifying MIH severity. CPQ8–10 with its Arabic version was used to evaluate OHRQoL. Mann–Whitney U test and Kruskal–Wallis test were used for comparisons (p ≤ 0.05).
Results
The mean value for CPQ8–10 in MIH group was 24.67 (±11.84; median 23; range 6–55) in comparison to 21.04 (±12.3; median 18; range 2–54) for the control group, with no significant difference between groups (p = 0.109). A significantly higher value (p = 0.011) was recorded in patients with MIH-TNI 4 mean 32.16 (±13.9; median 35; range from 7 to 55) in comparison to other categories of MIH.
Conclusion
Children with and without MIH, with similar caries experience showed no difference in OHRQoL. However, the presence of the severe form of MIH including hypersensitivity and enamel disintegration negatively impacted those children’s OHRQoL.
Similar content being viewed by others
Introduction
Molar Incisor Hypomineralisation (MIH) is defined as “hypomineralisation of systemic origin of one to four permanent first molars frequently associated with affected incisors” [1]. This qualitative developmental defect of enamel is characterized by demarcated opacities, soft and porous enamel that could be easily broken down and chipped after eruption exposing the underlying dentin and also reported hypersensitivities related to some of these affected teeth [2]. This phenomenon was first introduced with this terminology in 2001 [3].
The etiology of MIH is believed to be due to some systemic and genetic factors [4]. The genetic predisposition of MIH was proposed as some studies showed certain variants in amelogenesis related genes in MIH children and greater concordance of MIH in monozygotic twins [5, 6]. The systemic etiological hypotheses were related to prenatal exposures as maternal medications during pregnancy or perinatal exposures as premature birth, cesarean delivery, and hypoxia or postnatal exposures as early childhood illnesses in the first four years of life as asthma, pneumonia, bronchitis, ear or urinary tract infections and also medications as antibiotics [7, 8].
The worldwide prevalence rates of MIH had shown a wide range that varied from 2.4% to 40.2% [9, 10]. A recent national study reported a prevalence rate of 14.2% [11], and this coincides with the recent global mean prevalence rates of 14.2% and 12.9% [4].
Oral health-related quality of life (OHRQoL) is “a multidimensional construct that reflects among other things people’s comfort when eating, sleeping, and engaging in social interaction; their self-esteem; and their satisfaction with respect to their oral health” [12]. The quality of life of children with oral diseases, who are undergoing physical, mental, and social growth could be negatively affected, in contrast to children who do not have any oral pathology [13].
Children affected by MIH are more susceptible to caries affection and progression that can lead to pulpal inflammation [14]. Moreover, children tend to avoid tooth brushing because of increased sensitivity [1]. This hypersensitivity is an another major symptom that is related to many MIH affected teeth [15]. The hypersensitivity varies in severity from a mild response to an external stimulus to spontaneous hypersensitivity, with reported difficulty in achieving profound analgesia during restorative procedures [16]. Such factors can affect the daily lives of children, leading to negative social and esthetic effects as well as pain [17, 18], which in return negatively impact both the children’s oral self-perception [19], and the perception of their families towards their OHRQoL [20].
The European Academy of Pediatric Dentistry (EAPD) suggests MIH should be assessed in cross-sectional studies in 8-year-old children [17]. MIH presents a notable range of clinical manifestations that are subject to age-related influences [21]. Consequently, the assessment of MIH’s effect on OHRQoL in younger individuals is warranted, as it allows for the early detection of perceived needs in the disease’s initial phases. The Child Perceptions Questionnaire (CPQ8–10) is commonly utilized to assess OHRQoL in children aged 8–10 years, it is a generic questionnaire designed to cover different oral conditions including caries, malocclusion and craniofacial anomalies [22, 23].
Although MIH has been known for more than two decades now but no prior studies have examined MIH and OHRQoL in Egypt and to our knowledge there is lack of enough data about the relationship between them regionally in the Middle east, in addition to only one study has been previously reported in Africa [24].
It was also recommended in epidemiological studies on enamel hypominerlaization to use the International Caries Detection and Assessment System II (ICDAS II) for caries recording [25]. This is distinctively featured in this study, so that the relationship between MIH and caries is determined more accurately. The aim of this study is to investigate the effect of MIH on OHRQoL in children at their mixed dentition stage and correlate it with their caries experience.
Methods
Study design and setting
This was an analytical observational study of matched pairs. Patients were recruited between May 2023 and December 2023, from those who were seeking dental care at the Outpatient clinic of the Pediatric Dentistry Department in the Faculty of Dentistry and aged from 8 to 10 years.
Exclusion criteria included children with systemic diseases, any physical or mental disability, severe malocclusion, or any developmental defects other than MIH. Recruitment of patients continued until the total sample of 102 Egyptian children were collected as required where Group I consisted of 51 children suffering from MIH, and Group II included 51 children as controls without MIH.
Sample size calculation was performed using G power statistical power Analysis program (version 3.1.9.4) for sample size determination [26]. A total sample size n = 102; (subdivided into 51 in each group) was sufficient to detect a large effect size (d) = 0.69, with an actual power (1-β error) of 0.95 (95%) and a significance level (α error) 0.05 (5%) for two-sided hypothesis test, based on the results of a previous study by Velandia et al. [2], where MIH-affected children were significantly higher than control children in Total CPQ8-10 score showing MIH Median (interquartile range IQR) [12.5 (17)] versus [4 (3.5)].
Clinical examination
All the participants were examined by two examiners. Before the clinical examination, the children were asked to brush their teeth under the examiner’s supervision. The children were examined on a dental chair. A plain dental mirror and the ball-ended explorer (WHO periodontal probe) were used with an air-water syringe and under artificial lighting of the dental unit. The examination proceeded in a clockwise direction starting from the upper right quadrant and ending by the lower right one.
Dental caries detection methods
The caries experience of the children was recorded using two methods. The first one was DMFT [decayed (D), missing (M), and filled (F) permanent teeth] and deft [decayed (d), tooth indicated for extraction due to caries (e) and filled (f) primary teeth] caries indices [27, 28]. The second one was the ICDAS II caries index [29].
The examiners received training for caries recording and were calibrated. For ICDAS II recording, theoretical sessions and discussions for about six hours were held and the examiners were further trained using the ICDAS training online flashcards (https://quizlet.com).
Ten patients were examined firstly by the examiners and the results were checked with the senior and experienced examiner and inter-examiner reliability was statistically analyzed with Kappa coefficient [30].
DMFT & deft recording indices
Caries experience was diagnosed through guidelines established by the World Health Organization (WHO) [31]. Assessment of dental caries in permanent teeth was done according to the DMFT index. Teeth with carious lesions that are frankly cavitated with detectably softened floor or wall or teeth with carious lesions adjacent to restorations were recorded as “D”. Any tooth with a temporary filling was also recorded as “D”. Missing teeth due to caries were recorded as “M”. Teeth with permanent fillings or with defective fillings but not decayed was counted as “F”.
Dental caries evaluation in primary teeth was done according to the deft index [27, 28].
ICDAS II recording system
Following the ICDAS guidelines, all the teeth were examined wet first and then dried by the air-water syringe of the dental chair for 5 s each [30].
Each surface took a two-digit code where the first digit is for sealant and restoration and it ranges from 0 to 9, while the second digit is for coronal caries recording and it ranges from 0 to 6, it records caries related to pit and fissure, smooth surface (mesial and distal), free smooth surface (buccal, lingual or proximal surfaces without adjacent) and caries associated with restorations and sealants CARS [29]. Taking into consideration that surfaces with developmental defects as demarcated opacities were recorded as sound [32].
MIH diagnostic criteria
The diagnosis of MIH was according to the criteria proposed by the EAPD [17, 33]. This includes (a) Well-demarcated opacities greater than 1 mm, which can be white, yellow, or brown in color; (b) Post-eruptive enamel breakdown where there is deficiency and surface loss of enamel after eruption; (c) Atypical restorations that are not conforming to the typical caries picture, they are extending to the buccal or lingual smooth surfaces and at the margins of the restorations frequently an opacity can be noticed; (d) Extracted first permanent molars whether with opacities, breakdowns or atypical restorations in the other first permanent molars or in dentitions with low caries activity in combination with demarcated opacities on the incisors, and (e) Failure of eruption of a molar or an incisor at 8 years of age.
The MIH treatment need index (MIH-TNI)
The MIH-TNI was recorded according to the Würzburg MIH concept [34]. This classification is founded upon the two most important clinical features: hypersensitivity and destruction (disintegration). The recording is by visual means using a mirror and with tactile means using a probe and on drying with an air syringe.
The whole dentition is divided into sextants, recording starts in a clockwise direction, starting from the maxillary right sextant (distal to/with 14/54) then the maxillary front (with 13–23/53–63) then the maxillary left sextant (distal to/with 24/54), then the mandibular left sextant (distally to/with 34/74), then the mandibular front sextant (with 33–43/73–83), and ending by the mandibular right sextant (distal to/with 44/84) using a sextant recording diagram.
The essential parameters of the MIH including opacity, enamel fractures, and hypersensitivity are taken into consideration. The index values are 0 for no MIH and from 1 to 4 for the presence of MIH with further grading as shown in Table 1.
Evaluation of OHRQoL
OHRQoL was measured using the validated Arabic version of CPQ8–10 [35]. The CPQ8–10 questionnaire comprises 25 items categorized into four distinct domains: oral symptoms, functional limitations, emotional well-being (five items each), and social well-being (ten items). The questions evaluate the frequency of occurrences throughout the last month. The ratings are evaluated using a five-point Likert scale that ranges from 0 to 4 for each item, with 0 meaning “never,” 1 representing “once or twice,” 2 indicating “sometimes,” 3 for “often,” and 4 denoting “every day or almost every day”. Hence, total scores range from 0 to 100. A total score of zero indicates the absence of any problem, the higher the score, the worse OHRQoL. The CPQ8–10 includes two items for child identification (sex and age) and includes two global questions with a four-point Likert scales ranging from 0 to 3, the first assesses the child’s oral health where 0 is for “very good,” while 3 is for “poor” and the second evaluates the extent that his oral or facial condition affects his overall well-being, where 0 means “not at all” to 3 that means “a lot” [35, 36].
Statistical analysis
Data management and statistical analysis were conducted utilizing the Statistical Package for Social Sciences version 20. Summary statistics for numerical data included measures such as mean, standard deviation, confidence intervals, median and range. The normality of data was assessed through examination of data distribution using Kolmogorov–Smirnov and Shapiro–Wilk tests.
Based on the non-parametric distribution of most data, groups were compared using the Mann–Whitney U test, while the Kruskal–Wallis test was used for comparisons based on the MIH grade. All p-values are two-sided. P-values ≤ 0.05 were considered significant.
Results
Study population
A total of 102 subjects aged from 8 to 10 years were included in this study (51 per each group). The mean age in the MIH group was 8.94 ± 1.45 years in comparison to 8.8 ± 1.55 years in the control group, with no significant difference between the two groups (p = 0.602). The MIH group included 19 males (37.3%) and 32 females (62.7%) while the control group included 24 males (47.1%) and 27 females (52.9%); with no significant difference between groups (p = 0.316).
Caries recordings
The caries recordings for both DMFT/deft and ICDAS II indices were presented in Table 2.
The DMFT score for caries index of permanent teeth was significantly (p = 0.000) higher in MIH group (mean 1.55 ± 1.39, median 1, range 0–4) in comparison to control group (mean 0.59 ± 0.94, median 0, range 0–4). The D score was significantly (p = 0.001) higher in MIH group in comparison to the control group, and the F score was significantly (p = 0.044) higher in the MIH group) in comparison to control group while there was no significant difference in M score (p = 0.155). However, there was no significant difference in deft score for primary teeth between MIH and control groups (p = 0.245).
The DMFT + deft score recorded mean 4.76 (±2.84, median 5, range 0–13) in MIH group, in comparison to mean 4.51 (±3.12, median 4, range 0–13) in control group. This difference was not statistically significant (p = 0.452).
The analysis for ICDAS II data was done at two levels concerning the second digit of coronal caries recording, the first level is that score 0 is for sound surfaces and scores (1–6) is for caries [37], the other level is that only scores (4–6) is for caries, and considered for evaluation as those scores are equivalent to the WHO definition of caries [30]. Each tooth received the worst second digit code for one of its five surfaces for caries recording [37].
ICDAS II (1–6) scores for both non cavitated and cavitated lesions recorded mean 9.16 (±3.86, median 9, range 3–20) in the MIH group, in comparison to mean 8.22 (±3.59, median 8, range 1–18) in the control group. This difference was not statistically significant (p = 0.205).
ICDAS II (4–6) scores of cavitated lesions recorded mean 4.41 (±2.62, median 4, range 0–12) in the MIH group, in comparison to mean 4.24 (±3.16, median 3, range 0–14) in the control group. This difference was not statistically significant (p = 0.469) as shown in Fig. 1.
The analysis for both the DMFT/deft and ICDAS II scoring systems was done at the tooth level.
Kappa coefficient showed a good level of agreement between the examiners of 0.89.
OHRQoL in MIH and control groups
The mean value for CPQ8–10 in the MIH group was 24.67 (±11.84; median 23; range 6–55) in comparison to 21.04 (±12.3; median 18; range 2–54) for the control group, with no significant difference between groups (p = 0.109). Regarding the scores of the subdomains, there was no significant difference between groups for oral symptoms (p = 0.33), emotional well-being (p = 0.236), and social well-being (p = 0.676), only for the functional limitations, MIH group recorded mean 6.69 (±3.76; median 7; range 0–16), in comparison to mean 4.43 (±3.83; median 4; range 0–14) in the control group, with a statistically significant difference between groups (p = 0.003) as shown in Table 3.
As for emotional well-being only question no.11 “ How often have you had been upset because of your teeth or mouth?”, MIH group recorded mean 1.67 (±1.52; median 2; range 0–4), in comparison to mean 1.04 (±1.34; median 0; range 0–4) in the control group, with a statistically significant difference between groups (p = 0.038)
OHRQoL related to the severity of MIH
Regarding CPQ8–10 scores, a significantly higher value (p = 0.011) was recorded in patients with MIH-TNI 4 mean 32.16 (±13.9; median 35; range from 7 to 55) in comparison to MIH-TNI 3 mean 23 (±9.97; median 21; range from 13 to 36), MIH-TNI 2 mean 19.65 (±8.09; median 18; range from 6 to 33) and MIH-TNI 1 mean 20.6 (±3.65; median 22; range from 15 to 24) as shown in Fig. 2. CPQ8–10 scores for each domain for MIH-TNI different grades were presented in Table 4. Clinical pictures for MIH cases classified according to MIH-TNI index were shown in Fig. 3.
(a) Index 1(without hypersensitivity, without defect) in upper central incisors, (b) Index 2b (without hypersensitivity, with defect extension ≥1/3 ≤2/3) in lower left first permanent molar, (c) Index 3 (with hypersensitivity without defect) in lower right first permanent molar, (d) Index 4c (with hypersensitivity, with defect extension ≥2/3) in lower right first permanent molar.
OHRQoL between male and female patients
For the MIH group, CPQ8–10 scores showed no significant difference between genders (p = 0.992), only in Question no. 13 ”How often have you had been shy because of your teeth or mouth?” a significantly higher value (p = 0.044) was recorded in females (mean 1.22 ± 1.48, median 0, range 0–4), in comparison to males (mean 0.42 ± 1.02, median 0, range 0–3) and in question no 15” How often have you had worried that you are not as good-looking as others because of your teeth or mouth?”, a significantly higher value (p = 0.019) was recorded in females (mean 0.75 ± 1.37, median 0, range 0–4), in comparison to males who recorded score 0 in all cases.
Also, for the control group, CPQ8–10 scores showed no significant difference between genders (p = 0.148).
OHRQoL between different age groups
CPQ8–10 scores at 8 years showed a statistically significantly (p = 0.039) greater value (median = 34.5) in MIH group, in comparison to control group (median = 18), while no statistically significant difference was recorded between MIH and control group at 9 years (p = 0.808) and 10 years (p = 0.077).
Discussion
The concern for MIH is increasing worldwide among clinicians and also among patients in relation to their impact on oral health [38]. The main objective of the current study was to study the effect of MIH on OHRQoL in children at the mixed dentition stage and correlate it with the caries experience of these children. The CPQ8–10 with its validated Arabic version was used in this study as a widely used instrument to evaluate the OHRQoL [35]. The mean age in the MIH group was 8.94 ± 1.45 years in comparison to 8.8 ± 1.55 years in the control group, which is consistent with the EAPD guidelines, given that first permanent molars and permanent incisors usually erupt at that age and the risk of enamel defects concealment by carious cavities or restorations is restricted [39]. In addition, according to a systematic review published in 2021, the most common age of children examined in MIH studies was 8–10 years [40]. The understanding of the connection between MIH and caries and the overlap between the two conditions represents a clinical challenge and reflects the complexity of diagnosing MIH lesions and carious lesions [41].
Many investigations assessing dental caries in individuals with MIH commonly employ the DMFT index, as suggested by the WHO [20, 42,43,44]. Although, many studies opt for the DMFT index for assessing caries, yet it has limitations, including its failure to consider the stage of the carious lesion [36, 43, 45]. The ICDAS II index is effective in identifying caries at various stages, encompassing both cavitated and non-cavitated lesions. Furthermore, ICDAS II streamlines the diagnostic process, enhancing its accuracy and standardization in detecting caries [46]. Hence, the ICDAS II system for caries diagnosis with its detailed description was also used in this study as it allows for a more accurate picture of MIH and dental caries relationship [47].
The results of caries screening using the DMFT index showed a significantly higher difference for the MIH group compared to the control group regarding the mean DMF scores for permanent teeth, where both D and F scores were significantly higher in the MIH group. This can be explained by the fact that the hypomineralized enamel surface exhibits higher porosity compared to intact enamel, which facilitates increased biofilm buildup, consequently promoting demineralization [45].
Moreover, concerning that the differential diagnosis between dental caries and post-eruptive enamel breakdowns is quiet challenging, it was previously reported that the scores of DMFT caries index for MIH patients will probably be overestimated where score D can be given for post-eruptive enamel breakdowns not only dental caries and score Fand M is given for restorations or extractions treating dental caries, post-eruptive enamel breakdowns or combinations of both [43].
A systematic review published in 2017 concluded that the DMF index was higher in children with MIH than in children without MIH, but it is worth noting that none of the studies included were classified as high-quality studies [38].
Combining both DMFT index for permanent teeth and deft for primary teeth showed a mean score of 4.76 (±2.84) in the MIH group, in comparison to mean 4.51 (± 3.12) in the control group with a non-statistically significant difference. Similarly, a previous study recorded dmft/DMFT mean score of 5.04 (±3.73) for the MIH group in comparison to 5.49 (±3.84) for the control one showing a comparable caries experience [42].
In this study, the ICDAS II index was employed, which takes into account both the stages of the lesion and the child’s caries history [46].
The ICDAS II (1–6) scores including the non-cavitated lesions showed no difference between MIH patients and control ones as the early signs of dental caries as white spot lesions usually occur in areas of plaque stagnation in the cervical areas of smooth surfaces where enamel hypomineralization rarely occurs [48]. So, no overestimation of the ICDAS scores of 1 and 2 in MIH patients was presented.
Regarding the ICDAS II (4–6) scores of cavitated lesions with dentinal involvement in both primary and permanent teeth collectively, there were no statistically significance difference between the MIH and control groups. To our knowledge, there was only one study conducted before for comparisons of the ICDAS II scores in our same age group, their results showed that caries is far greater in surfaces with severe MIH than in surfaces with mild MIH or no MIH, as they explained that creamy and brownish opacities are more porous and susceptible to post-eruptive enamel breakdowns that in return worsen caries, however, there were two differences than our study where there was subgrouping of MIH to two forms, mild and severe one and MIH and caries was assessed by two different examiners [49]. Another study compared caries experience in children aged 3–5 years with and without hypomineralized second primary molars, there was no significant difference in ICDAS II codes (2–6) or (4–6) at their tooth surface level or in the overall caries experience [50].
The comparable ICDAS II (4–6) scores in the two groups in our study which represents the more severe form of caries involvement may reflect their similar impact on oral symptoms.
Regarding the effect of MIH on the OHRQoL, the impact of MIH only on the domain of functional limitations was manifested. In a systematic review published in 2021 [40], only two articles showed a significant impact of MIH on all domains of OHRQoL, Gutiérrez et al. [51] in 2019 and Velandia et al. [2] in 2018.
On the other hand, in agreement with our results, other studies evaluated the effect of MIH on OHRQoL in children and concluded that the presence of MIH had no significant impact on the OHRQoL according to children’s self-reported perceptions, these studies was conducted in developing countries similar to our study [24, 52].
Demographic and socioeconomic factors, along with the organization of children’s dental services, vary significantly worldwide which may explain these differences between studies. This controversy in the results of previous studies also prompts inquiry into potential cultural variances in esthetic perception and the psychological impact of esthetics on self-well-being [53].
Regarding the functional limitations caused by MIH, previous studies explained this impact as a result of hypersensitivity, which is the main issue that appeared to stem from challenges with eating and maintaining oral hygiene [54].
Meanwhile, when considering the clinical severity of MIH, significantly higher CPQ8–10 scores were recorded in patients with MIH-TNI 4 in comparison to other categories of MIH and to the control group. Patients with MIH-TNI 4 show the two most important clinical symptoms of MIH which is hypersensitivity and disintegration. Joshi et al. study showed increased CPQ8–10 scores with increasing severity reflecting a more impaired OHRQoL, their findings demonstrated statistically significant variances between the control group and the MIH-TNI groups of index 2, 3, and 4, but no statistically significant difference was recorded between the control group and MIH-TNI 1 [42]. Other studies also showed that the more severe the MIH, the greater the impact on OHRQoL where hypersensitivity, enamel fractures, atypical cavities adversely affected the OHRQoL [20, 41].
CPQ8–10 scores for male and female patients showed no significant difference between them in the MIH group, however only two questions concerning dental esthetics and their social influence showed a significantly higher value in females compared to males. It is reported that females are more concerned with dental esthetics and smile satisfaction than males [55]. Interestingly, among facial esthetics, the smile appears to be critical for adolescents as well as for children younger than 10 years of age and influence their social perception [56]. Concerning the OHRQoL between different age groups, CPQ8–10 scores only at 8 years showed a statistically significantly greater value in the MIH group, in comparison to the control group, this could be attributed to hypersensitivity where a previous study conducted on MIH patients between 6 and 18 years of age with a mean of 10.9 (±2.9) years showed that the degree of hypersensitivity is significantly higher in individuals aged ≤8 years [15].
Among the limitations of the current study, the collected data represent the individual’s perception at the time of assessment. Therefore, a longitudinal study design is necessary to examine the influence of MIH on OHRQoL over time with respect to different socioeconomic and cultural differences.
Conclusion
Children with and without MIH showing similar overall caries experience recorded by ICDAS II showed no difference in their OHRQoL evaluation except for functional limitations. However, the presence of the severe form of MIH including hypersensitivity and enamel disintegration negatively impacted those children’s OHRQoL.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Weerheijm KL. Molar incisor hypomineralisation (MIH). Eur J Paediatr Dent. 2003;4:114–20.
Velandia LM, Álvarez LV, Mejía LP, Rodríguez MJ. Oral health-related quality of life in Colombian children with molar-incisor hypomineralization. Acta Odontol Latinoam. 2018;31:38–44.
Weerheijm KL, Jälevik B, Alaluusua S. Molar-incisor hypomineralisation. Caries Res. 2001;35:390–1.
Lygidakis NA, Garot E, Somani C, Taylor GD, Rouas P, Wong FSL. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): an updated European Academy of Paediatric Dentistry policy document. Eur Arch Paediatr Dent. 2022;23:3–21.
Jeremias F, et al. Family-based genetic association for molar-incisor hypomineralization. Caries Res. 2016;50:310–8.
Teixeira RJPB, et al. Exploring the association between genetic and environmental factors and molar incisor hypomineralization: evidence from a twin study. Int J Paediatr Dent. 2018;28:198–206.
Silva MJ, Scurrah KJ, Craig JM, Manton DJ, Kilpatrick N. Etiology of molar incisor hypomineralization - a systematic review. Community Dent Oral Epidemiol. 2016;44:342–53.
Garot E, Rouas P, Somani C, Taylor GD, Wong F, Lygidakis NA. An update of the aetiological factors involved in molar incisor hypomineralisation (MIH): a systematic review and meta-analysis. Eur Arch Paediatr Dent 2022;23:23–38.
Cho S-Y, Ki Y, Chu V. Molar incisor hypomineralization in Hong Kong Chinese children. Int J Paediatr Dent. 2008;18:348–52.
Soviero V, Haubek D, Trindade C, Da Matta T, Poulsen S. Prevalence and distribution of demarcated opacities and their sequelae in permanent 1st molars and incisors in 7 to 13-year-old Brazilian children. Acta Odontol Scand. 2009;67:170–5.
Osman S, Elmasry E, Abd Al Gawad R. Prevalence of molar incisor hypominerlization among a group of egyptian children: a cross sectional study. Egypt Dent J. 2020;66:2021–8.
Bennadi D, Reddy CVK. Oral health related quality of life. J Int Soc Prev Community Dent. 2013;3:1–6.
Barbosa TS, Gavião MBD. Oral health-related quality of life in children: part II. Effects of clinical oral health status. A systematic review. Int J Dent Hyg. 2008;6:100–7.
Fagrell TG, Lingström P, Olsson S, Steiniger F, Norén JG. Bacterial invasion of dentinal tubules beneath apparently intact but hypomineralized enamel in molar teeth with molar incisor hypomineralization. Int J Paediatr Dent. 2008;18:333–40.
Linner T, Khazaei Y, Bücher K, Pfisterer J, Hickel R, Kühnisch J. Hypersensitivity in teeth affected by molar-incisor hypomineralization (MIH). Sci Rep. 2021;11:17922.
Lygidakis NA, Garot E, Somani C, Taylor GD, Rouas P, Wong FSL. Best clinical practice guidance for clinicians dealing with children presenting with molar-incisor-hypomineralisation (MIH): an updated European Academy of Paediatric Dentistry policy document. Eur. Arch. Paediatr. Dent. 2022; 23. https://doi.org/10.1007/s40368-021-00668-5.
Lygidakis NA, Wong F, Jälevik B, Vierrou A-M, Alaluusua S, Espelid I. Best clinical practice guidance for clinicians dealing with children presenting with Molar-Incisor-Hypomineralisation (MIH): an EAPD policy document. Eur Arch Paediatr Dent. 2010;11:75–81.
Jälevik B, Klingberg GA. Dental treatment, dental fear and behaviour management problems in children with severe enamel hypomineralization of their permanent first molars. Int J Paediatr Dent. 2002;12:24–32.
Leal SC, Oliveira TRM, Ribeiro APD. Do parents and children perceive molar-incisor hypomineralization as an oral health problem? Int J Paediatr Dent. 2017;27:372–9.
Dantas-Neta NB, et al. Impact of molar-incisor hypomineralization on oral health-related quality of life in schoolchildren. Braz Oral Res. 2016;30:e117.
Da Costa-Silva CM, Ambrosano GMB, Jeremias F, De Souza JF, Mialhe FL. Increase in severity of molar-incisor hypomineralization and its relationship with the colour of enamel opacity: a prospective cohort study. Int J Paediatr Dent. 2011;21:333–41.
Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26:512–8.
Gilchrist F, Rodd H, Deery C, Marshman Z. Assessment of the quality of measures of child oral health-related quality of life. BMC Oral Health. 2014;14:40.
Folayan MO, et al. Developmental defects of the enamel and its impact on the oral health quality of life of children resident in Southwest Nigeria. BMC Oral Health. 2018;18:1–10.
Ghanim A, Elfrink M, Weerheijm K, Mariño R, Manton D. A practical method for use in epidemiological studies on enamel hypomineralisation. Eur Arch Paediatr Dent J Eur Acad Paediatr Dent. 2015;16:235–46.
Charan J, Biswas T. How to calculate sample size for different study designs in medical research? Indian J Psychol Med. 2013;35:121–6.
World Health Organization. Oral health surveys: basic methods. 3rd ed. Geneva: World Health Organization; 1987.
Gruebbel AO. A measurement of dental caries prevalence and treatment service for deciduous teeth. J Dent Res. 1944;23:163–8.
Dikmen B. Icdas II criteria (international caries detection and assessment system). J Istanb Univ Fac Dent. 2015;49:63–72.
Almerich-Silla J-M, Boronat-Ferrer T, Montiel-Company J-M, Iranzo-Cortés J-E. Caries prevalence in children from Valencia (Spain) using ICDAS II criteria, 2010. Med Oral Patol Oral Cir Bucal. 2014;19:e574–80.
World Health Organization. Oral health surveys. basic methods. 5th ed. Geneva: World Health Organization; 2013.
Ismail AI, et al. The international caries detection and assessment system (ICDAS): an integrated system for measuring dental caries. Community Dent Oral Epidemiol. 2007;35:170–8.
Weerheijm KL, et al. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: a summary of the European meeting on MIH held in Athens, 2003. Eur J Paediatr Dent. 2003;4:110–3.
Steffen R, Krämer N, Bekes K. The Würzburg MIH concept: the MIH treatment need index (MIH TNI): a new index to assess and plan treatment in patients with molar incisior hypomineralisation (MIH). Eur Arch Paediatr Dent. 2017;18:355–61.
Al-Blaihed D, El-Housseiny AA, Farsi NJ, Farsi NM. Validity and reliability of the Arabic version of the child perceptions questionnaire for 8-10-year-old children. Qual Life Res. 2020;29:3131–41.
Portella PD, Menoncin BLV, de Souza JF, de Menezes JVNB, Fraiz FC, da Assunção LRS. Impact of molar incisor hypomineralization on quality of life in children with early mixed dentition: a hierarchical approach. Int J Paediatr Dent. 2019;29:496–506.
Melgar RA, Pereira JT, Luz PB, Hugo FN, de Araujo FB. Differential impacts of caries classification in children and adults: a comparison of ICDAS and DMF-T. Braz Dent J. 2016;27:761–6.
Americano GCA, Jacobsen PE, Soviero VM, Haubek D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int J Paediatr Dent. 2017;27:11–21.
Ben Salem M, Chouchene F, Masmoudi F, Baaziz A, Maatouk F, Ghedira H. Are molar-incisor hypomineralization and hypomineralized second primary molars predictive of dental caries?: a systematic review. Eur J Dent. 2023;17:7–15.
Jälevik B, Sabel N, Robertson A. Can molar incisor hypomineralization cause dental fear and anxiety or influence the oral health-related quality of life in children and adolescents?—a systematic review. Eur Arch Paediatr Dent. 2022;23:65–78.
Shields S, Chen T, Crombie F, Manton DJ, Silva M. The impact of molar incisor hypomineralisation on children and adolescents: a narrative review. Healthc. 2024;12:1–11.
Joshi T, Rahman A, Rienhoff S, Rienhoff J, Stamm T, Bekes K. Impact of molar incisor hypomineralization on oral health-related quality of life in 8-10-year-old children. Clin Oral Investig. 2022;26:1753–9.
Vieira FG, Pintor AV, Silva F, Da, Neves ADA, Costa MD. Molar incisor hypomineralization-influence on dental caries experience indexes: a cross-sectional study. Int J Clin Pediatr Dent. 2022;15:65–68.
Opydo-Szymaczek J, Gerreth K. Developmental enamel defects of the permanent first molars and incisors and their association with dental caries in the region of Wielkopolska, Western Poland. Oral Health Prev Dent. 2015;13:461–9.
Al. B et. Molar-incisor hypomineralization and dental caries: a hierarchical approach in a populational-based study. Braz Dent J. 2021;32:74–82.
Al Dhubayb S, Al Sultan M, Al Sudairi S, Hakami F, Al Sweleh FS. Ability of dentists and students to detect caries by using the international caries detection and assessment system. Clin Cosmet Investig Dent. 2021;13:379–87.
Ghanim A, Elfrink M, Weerheijm K, Mariño R, Manton D. A practical method for use in epidemiological studies on enamel hypomineralisation. Eur Arch Paediatr Dent. 2015;16. https://doi.org/10.1007/s40368-015-0178-8.
Ghanim A, et al. Molar incisor hypomineralisation (MIH) training manual for clinical field surveys and practice. Eur Arch Paediatr Dent. 2017;18:225–42.
Negre-Barber A, Montiel-Company JM, Catalá-Pizarro M, Almerich-Silla JM. Degree of severity of molar incisor hypomineralization and its relation to dental caries. Sci Rep. 2018;8:1–7.
Owen ML, Ghanim A, Elsby D, Manton DJ. Hypomineralized second primary molars: prevalence, defect characteristics and relationship with dental caries in Melbourne preschool children. Aust Dent J. 2018;63:72–80.
Gutiérrez TV, Ortega CCB, Pérez NP, Pérez AG. Impact of molar incisor hypomineralization on oral health-related quality of life in mexican schoolchildren. J Clin Pediatr Dent. 2019;43:324–30.
Dias FMCS, Gradella CMF, Ferreira MC, Oliveira LB. Molar–incisor hypomineralization: parent’s and children’s impact perceptions on the oral health-related quality of life. Eur Arch Paediatr Dent. 2021;22:273–82.
Bandeira Lopes L, Machado V, Botelho J, Haubek D. Molar-incisor hypomineralization: an umbrella review. Acta Odontol Scand. 2021;79:359–69.
Sekundo C, Jung M, Muscholl C, Frese C. Oral health-related quality of life and survival analysis after preventive and restorative treatment of molar-incisor hypomineralisation. Sci Rep. 2024;14:1–9.
Ellakany P, Fouda SM, Alghamdi M, Bakhurji E. Factors affecting dental self-confidence and satisfaction with dental appearance among adolescents in Saudi Arabia: a cross sectional study. BMC Oral Health. 2021;21:149.
Rossini G, Parrini S, Castroflorio T, Fortini A, Deregibus A, Debernardi CL. Children’s perceptions of smile esthetics and their influence on social judgment. Angle Orthod. 2016;86:1050–5.
Funding
This work was self-funded. Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
LKG performed conceptualization, methodology, investigation, and writing-original draft, EK participated in methodology, data collection, and editing, RW participated in data collection, reviewing, and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests. This study was reviewed and approved by the Medical Research Ethics Committee (MREC) of the National Research Centre, with reference number (03470233). Prior to carrying out the research, written informed consents were signed by the parents or legal guardians of the participating children and verbal assents were also obtained from the children themselves.
Ethics
This study was reviewed and approved by the Medical Research Ethics Committee (MREC) of the National Research Centre, with reference number (03470233).
Prior to carrying out the research, written informed consents were signed by the parents or legal guardians of the participating children and verbal assents were also obtained from the children themselves.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gadallah, L.K., Korayem, E. & Wahby, R. Oral health-related quality of life in Egyptian children with Molar Incisor Hypomineralisation. An observational study. BDJ Open 10, 89 (2024). https://doi.org/10.1038/s41405-024-00272-x
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41405-024-00272-x
This article is cited by
-
Parental knowledge and perception of Molar Incisor Hypomineralisation (MIH)
European Archives of Paediatric Dentistry (2025)