Abstract
MRD2STOP is a pragmatic trial evaluating maintenance therapy cessation guided by measurable residual disease (MRD) negativity in multiple myeloma (MM). Eligible patients had previous MRD < 10−5, received ≥1 year of maintenance, and were prospectively confirmed to have undetectable disease by positron emission tomography, bone marrow (BM) flow cytometry (limit of detection [LoD] 10−5), and BM clonoSEQ (LoD 10−6). BM aspirates enriched for CD138+ cells were analyzed by clonoSEQ to achieve MRD 10−7 sensitivity. We evaluated the incidence of disease resurgence and progression-free survival (PFS), stratified by 10−7 status. Forty-seven patients discontinued maintenance after a median of 36 months. Baseline MRD ≥ 10−7 was observed in 19% (9/47). The median follow-up post-discontinuation was 30 months. Disease resurgence (MRD 10 ≥ −6) occurred in 11 patients, including 5 disease progressions. One patient died from a second cancer. The estimated 3-year cumulative incidence of disease resurgence was 20% for patients with baseline MRD < 10−7 compared to 75% for MRD ≥ 10−7 (HR 7.8, 95% CI 2.2-27.6, p = 0.001). Baseline MRD ≥ 10−7 was associated with inferior PFS compared to MRD < 10−7 (HR 10.1, 95% CI 1.6–62.3; 3-year PFS 49% vs 92%). Maintenance discontinuation in patients with MM and MRD < 10−6 led to low rates of disease resurgence. MRD < 10−7 may be a superior cessation threshold, requiring further validation.

Similar content being viewed by others
Introduction
Multiple myeloma (MM) has long been thought to be an incurable disease; contemporary MM therapy involving prolonged maintenance therapy has challenged this assertion by leading to more exceptional responders, though the indefinite nature of maintenance makes identifying a cure even more challenging. Measurable residual disease (MRD), referring to low levels of cancer cells only detectable by advanced assays, serves as an important prognostic marker for progression-free survival (PFS) and overall survival (OS) in MM, with each increase in MRD sensitivity threshold leading to improved prognostication [1]. The depth of MRD testing is not the only factor. While a single instance of MRD negativity may be prognostic, sustained MRD negativity—defined by the International Myeloma Working Group (IMWG) as two consecutive MRD negative results at the 10−5 threshold performed at least one year apart—carries even greater significance with respect to outcomes [2,3,4].
Maintenance therapy in MM – typically with lenalidomide – can deepen responses after completion of induction and/or consolidation with autologous stem cell transplantation (ASCT), including converting patients with MRD positivity to MRD negativity [5,6,7]. Meta-analyses have shown that lenalidomide maintenance is associated with an OS benefit [8, 9], though some of these studies pre-date widespread use of triplet induction with a proteasome inhibitor and an immunomodulatory imide drug and all pre-date the incorporation of anti-CD38 monoclonal antibodies into frontline triplet or quadruplet therapies. With further improvements in the depth and duration of response using contemporary MM agents, should indefinite maintenance still be the standard of care? As of now, maintenance therapy has no established end date, may impact health-related quality of life (HRQoL) due to ongoing treatment-related side effects, may increase the risk of second cancers [10], and carries significant financial burden for patients and payors. For these reasons, there is emerging interest in discovering if patients can undergo maintenance cessation without excess risk of disease re-emergence based on the attainment of (sustained) MRD negativity.
In this prospective intervention study called MRD2STOP (NCT04108624), we evaluated the outcomes of patients with MM with sustained multimodal MRD negativity who underwent discontinuation of maintenance therapy.
Methods
Study design and participants
This was a prospective, pragmatic, single-institution trial that enrolled patients aged 18 or older with MM. Eligibility criteria for discontinuation included patients with MM who had received at least one year of maintenance, who were previously known to be in at least a complete response (CR) by IMWG criteria with no detectable disease by positron emission tomography (PET), and MRD negative by multiparametric flow cytometry (MFC) or next generation sequencing (NGS) at a sensitivity of at least 10−5 in the bone marrow (BM). Patients had to be receiving only single-agent maintenance therapy at the time of screening, though the 1-year duration of maintenance therapy could include time spent receiving multi-agent maintenance prior to de-escalation to single-agent maintenance therapy. Given the intentional pragmatic nature of this study, there were no stipulations regarding the type, duration, or intensity of induction or consolidation.
Patients meeting these criteria were screened with peripheral blood (PB) testing for paraproteins, a PET scan, and a BM biopsy and aspiration with MRD evaluation by MFC (limit of detection [LoD] 10−5) and by NGS using clonoSEQ (Adaptive Biotechnologies, LoD of 6.8 × 10−7 and limit of quantitation of 1.76 × 10−6 with 20 μg [~3 million cells] input). Discontinuation of therapy was permitted only for those who were MRD negative by PET, MFC, and NGS at the 10−6 threshold.
After discontinuation of therapy, patients underwent PB testing every 3 months (serum protein electrophoresis, immunofixation, and serum-free light chains), BM MRD testing by MFC and NGS every year, and PET imaging every year for 3 years.
All patients provided written informed consent; the study was conducted in accordance with the US Food and Drug Administration, the International Conference on Harmonization Guidelines for Good Clinical Practice, and the Declaration of Helsinki. The study was approved by the University of Chicago institutional review board (#19-0339) and was registered at ClinicalTrials.gov (NCT04108624).
Additional evaluations
Additional assessments were performed in the BM. At screening and at each timepoint, BM aspirate samples were also collected for CD138+ immunomagnetic enrichment using EasySep (Stem Cell Technologies, Vancouver, Canada) for the performance of clonoSEQ to achieve an approximate sensitivity of 10−7. A first-pull aspirate of 10 cc was divided into 2 cc for clonoSEQ and 8 cc for CD138+ selection. A fraction of the CD138+-selected sample was analyzed to target 10−7 sensitivity. To validate the results, the remaining fraction was also analyzed. Investigators and patients were blinded to individual 10−7 results at screening. HRQoL was assessed serially every 6 months for a subset of patients using the validated patient-reported outcome (PRO) survey tools EORTC QLQ-C30 and EORTC QLQ-MY20.
Study endpoints
The endpoints of interest in this study included the rate of MRD 10−6 resurgence (including progression) and PFS among those MRD negative by the standard non-enriched NGS assay (10−6) and the CD138+ enriched NGS assay (10−7). MRD resurgence was defined as MRD detectable at the 10−6 threshold. If a serial sample was indeterminate at the 10−6 threshold due to insufficient sample, it was not considered MRD resurgence. We also followed patients for overall survival. Secondary endpoints included the feasibility of the CD138+ enrichment method and the differences in MRD detection by NGS using both methods. Longitudinal changes in PRO scores, including global health status and within specific functional and symptom HRQoL domains, were an exploratory endpoint.
MRD sensitivity thresholds
MRD by NGS using the standard clonoSEQ assay carries an LoD of 6.8 × 10−7 and LoQ of 1.76 × 10−6 with an input of 20 µg DNA. For the CD138+ enriched sample processed using the clonoSEQ assay, feasibility was defined as at least 80% of samples having at least 20 million nucleated cells in the raw aspirate sample.
Statistical analysis
The study was powered to assess MRD resurgence and PFS stratified by MRD 10−7. Based on the results of the IFM-2009 trial, we hypothesized that the 3-year progression-free survival (PFS) from maintenance cessation for patients who were MRD negative at the 10−6 threshold would be 75% [5]; as was the case for lower MRD sensitivity thresholds, we surmised that PFS could be further stratified based on 10−7 status. Assuming 40% of enrolled patients would be 10−7 positive, calculations suggested that if the 3-year PFS was 52% for patients with 10−6 negativity but 10−7 positivity and 90% for patients with double (10−6/10−7) negativity (for a 3-year PFS of 75% overall), a sample size of 45 patients would yield 80% power with a two-sided alpha of 0.05 to detect a difference of this magnitude. Interim analyses were prespecified to limit undue harm to enrolled patients in the event of excess relapse; if the 2-year PFS was significantly less than 85% at a one-sided 0.05 alpha level, the study would be terminated. The Kaplan–Meier method was used to analyze PFS and OS.
Conversion from MRD 10−6 negativity to positivity (MRD resurgence rate) within the first two years from the achievement of MRD negativity was 27% in one study, which has been confirmed in more recent analyses [11,12,13]. We posited that if patients with MRD 10−7 negativity had a 2-year MRD 10−6 resurgence rate of ≤10%, it would be considered clinically meaningful. A sample size of 45 patients would provide 84% power with a two-sided alpha of 0.05 to detect a reduction of this magnitude using the historical control of 27%. The cumulative incidence rate of progression or MRD 10−6 resurgence was calculated by the Fine-Gray method, with death without MRD resurgence considered a competing event. We also calculated MRD-free survival (MRD-FS)—defined as the absence of MRD resurgence, progression, or death—using the Kaplan–Meier method.
Longitudinal changes in PRO scores between baseline and 6, 12, and 18 months were analyzed by one-way repeated-measures ANOVA and were visualized as mean score changes from baseline (Supplement page 7). Absolute score changes of 8 for the EORTC QLQ-C30 [14] and 9–13 for the EORTQ QLQ-MY20 (10 for disease symptoms, 10 for side effects of treatment, 13 for body image, and 9 for future perspective) [15] were considered minimally important differences (MID), as previously validated in patients with MM. All statistical analyses were performed in STATA 17.0 (College Station, TX). The data cutoff for this report is January 21, 2024.
Results
Patient characteristics
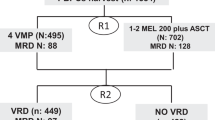
A total of 83 patients signed consent and underwent screening, of which 47 patients met protocol eligibility criteria and discontinued maintenance therapy. A total of 9/47 (19%) patients had MRD ≥ 10−7 at baseline. The median age of enrolled patients was 66 years (range, 39–84) (Table 1). At least one high-risk disease feature was present in 17 (36%) patients at diagnosis, and 2 (4%) had 2+ HRCAs. Nearly all patients (45/47, 96%) were still in their first line of therapy at the time of treatment discontinuation; 26 (55%) received a triplet induction regimen, 20 (43%) received a quadruplet, and 1 (2%) received doublet therapy. Thirty (64%) received an ASCT, and 36 (77%) received multi-drug consolidation prior to single-agent maintenance therapy. Nearly all patients (45/47, 96%) received lenalidomide as their single-agent maintenance therapy. The median duration of post-induction/ASCT therapy prior to discontinuation was 36 months (range, 12–95); 14 (30%) patients received 2 years or less of consolidation/maintenance. There were no significant differences in patient characteristics based on baseline MRD 10−7 status, though numerically a higher percentage of patients received quadruplet induction therapy in the MRD < 10−7 group, and the median duration of consolidation/maintenance therapy was numerically longer for the MRD ≥ 10−7 group (Table 1).
During screening, sustained MRD < 10−6 was confirmed in 22/47 (47%); the remaining patients had MRD < 10−6 during screening, and IMWG-defined sustained MRD < 10−5 but with indeterminate prior 10−6 status. There was a numerically higher percentage of patients with baseline MRD ≥ 10−7 in those with indeterminate sustained MRD < 10−6 (6/25) vs those with confirmed sustained MRD < 10−6 (3/22, p = 0.3).
The median follow-up was 30 months (range, 8–46). Of the 47 enrolled patients, 1 (2%) patient withdrew from the study due to geographic relocation and restarted maintenance (no evidence of disease resurgence), and 1 (2%) patient could not be followed for MRD surveillance due to insurance coverage issues; both were alive and free of disease progression at the data cutoff and were included in PFS and OS analyses. Because MRD status could not be ascertained, these two patients were not included in the MRD-FS analysis. An additional two patients were enrolled to account for these withdrawals and are included in this analysis (Fig. 1).
Feasibility of CD138+ selection
BM samples evaluated for MRD by NGS at 10−7 sensitivity passed quality control in 134/136 (99%) cases. The median estimated unselected nucleated cell count prior to CD138+ enrichment was 57 × 106 (interquartile range, 38 × 106–72 × 106) cells; only 6 (4%) samples had fewer than 20 × 106 cells. The median CD138+ cell count analyzed was 216,469 (range 1291–2,857,681) cells across both runs. The feasibility endpoint of ≥80% of samples having ≥20 million nucleated cells in the unselected aspirate sample, along with ≥80% evaluable 10−7 results, was met.
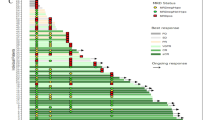
MRD resurgence
Among the 45 MRD evaluable patients, MRD resurgence at the 10−6 threshold was identified in 11 (24%) patients, which included 5 (11%) patients with disease progression. Characteristics of patients with disease progression or MRD 10−6 resurgence can be found in Table S1. Consolidation before maintenance was received by 8/11 (73%) and 6/11 (54%) had a known high-risk cytogenetic abnormality (1q gain n = 4, t(4;14) n = 1, and TP53 deletion n = 1). Among the 11 patients with progression or MRD resurgence, 5 (45%) had detectable MRD by the 10−7 assay at baseline, and an additional 3 (27%) had MRD 10−7 detectable at least one year prior to MRD 10−6 resurgence; the other 3 (27%) patients had MRD resurgence at 10−6 at the same time as MRD resurgence at 10−7. MRD 10−6 resurgence during follow-up preceded disease progression in 3/5 (60%) patients. MRD 10−7 positivity at baseline preceded disease progression in 3/5 (60%) patients by a median of 18 months (12–24 months), and MRD 10−7 resurgence during follow-up preceded disease progression in 1 (20%) other patient (Table S1).
Of the 9 patients with MRD positivity at 10−7 at baseline, 5 (56%) experienced progression (n = 3) or MRD resurgence at the 10−6 threshold (n = 2) (Fig. S1).
At 30 months of median follow-up, MRD 10−7 positivity at baseline was associated with inferior MRD-FS (HR 6.3, 95% CI 1.9–21.5, p = 0.003). The estimated 3-year MRD-FS in all patients was 68% (95% CI 49–81%) (Fig. 2): 77% (95% CI 55–89%) for MRD 10−7 negative patients and 25% (95% CI 1–63%) for MRD 10−7 positive patients (Fig. 3A). Univariate analyses found no differences in MRD-FS when stratifying patients by confirmed sustained MRD < 10−6 status, receipt of quadruplet induction, ASCT, or consolidation, or duration of consolidation and/or maintenance. The presence of a high-risk cytogenetic abnormality at baseline was associated with inferior MRD-FS (HR 3.7, 95% CI 1.2–11.7, p = 0.02).
The 3-year cumulative incidence rate of progression or MRD 10−6 resurgence for all patients was 30%, including a 16% rate of MRD 10−6 resurgence without progression. The cumulative incidence rate was higher for patients with MRD 10−7 positivity compared to 10−7 negativity at baseline (subdistribution hazard ratio [SHR] 7.8, 95% CI 2.2–27.6, p = 0.001); the 3-year cumulative incidence of progression or MRD resurgence was 20% for patients with MRD 10−7 negativity at baseline and 75% for patients with MRD 10−7 positivity at baseline (Fig. S2)
Progression-free survival and overall survival
With a median follow-up of 30 months, MRD 10−7 positivity at baseline was associated with inferior PFS compared to MRD 10−7 negativity (HR 10.1, 95% CI 1.6–62.3, p = 0.01). The estimated 3-year PFS for the whole cohort was 85% (95% CI 67–94%) (Fig. 2): 92% (95% CI 72–98%) for MRD 10−7 negative patients and 49% (95% CI 8–82%) for MRD 10−7 positive patients (Fig. 3B). Univariate analyses found no differences in PFS when stratifying patients by high-risk cytogenetics at baseline, confirmed sustained MRD < 10−6 status, receipt of quadruplet induction, ASCT, or consolidation, or duration of consolidation and/or maintenance.
Cumulative incidence of progression was higher for patients with MRD 10−7 positivity compared to 10−7 negativity at baseline (SHR 21.5, 95% CI 2.8–166.7, p = 0.003). The 3-year cumulative incidence rate of progression was 12%; 4% for patients with MRD 10−7 negativity and 51% for patients with MRD 10−7 positivity at baseline (Fig. S3).
Of the 5 progression events, 2 (40%) had biochemical progression alone, and 3 (60%) had hypermetabolic osseous lesions identified on PET scans. None of the 5 patients had a history of extramedullary disease at diagnosis. All five patients successfully underwent retreatment, and three again reached MRD < 10−6.
One patient died due to complications related to a second hematologic malignancy. Overall survival (OS) is immature; the estimated 3-year OS was 97% (Fig. S4).
Health-related quality of life
There were 18 and 16 patients with available QLQ-C30 and QLQ-MY20 data, respectively. Survey completion rates were 55% and 50% at 18 months post-discontinuation for the QLQ-C30 and QLQ-MY20, respectively.
There were statistically significant improvements in role functioning, insomnia, diarrhea, pain, and financial difficulties after lenalidomide discontinuation (all p < 0.05, Fig. 4), all of which exceeded the MID threshold. These improvements were sustained up to 18 months after maintenance discontinuation. There were no significant changes in other QLQ-C30 or QLQ-M20 domains (Figs. S5–S7).
Adverse events
Adverse events of interest included second cancers, including second hematologic malignancies, that occurred during the study period. Three patients were diagnosed with second cancers during the study: one patient was diagnosed with Hodgkin lymphoma after 14 months (in complete remission), one patient was diagnosed with B-cell acute lymphoblastic leukemia after 24 months (achieved complete remission but died due to an infectious complication), and one patient was diagnosed with melanoma. All three patients had received high-dose melphalan and had received 68, 48, and 23 months of maintenance therapy, respectively. All three patients had remained MRD negative with respect to MM.
Discussion
In this pragmatic prospective study of patients with MM with multimodal MRD < 10−6 who underwent discontinuation of maintenance therapy regardless of induction regimen, receipt of ASCT, or maintenance therapy, the estimated 3-year PFS was 85% and even higher (92%) for those with MRD < 10−7 using a CD138+-selected assay. The cumulative incidence of MRD 10−6 resurgence or disease progression at 3 years following maintenance discontinuation was 30%, though this was driven mainly by patients with MRD 10−7 positivity at baseline (20% for MRD < 10−7 vs 75% for MRD ≥ 10−7). The presence of an HRCA was associated with worse MRD-FS but not PFS. HRQoL improved among a subset of patients following maintenance cessation, specifically role functioning, insomnia, diarrhea, pain, and financial difficulties.
MRD is not a binary marker but exists on a continuous spectrum, and naturally, MRD negativity at deeper thresholds will be associated with better outcomes. However, there are practical constraints to the amount of sample that can be obtained owing to limitations with DNA/cell input, expense of evaluation, and potential harm to the patient. No MRD assay is currently validated to provide 10−7 sensitivity, but we show that the CD138+-selected NGS 10−7 assay was feasible and detected MRD when the standard 10−6 assay did not. Four out of five progression events were preceded by MRD 10−7 positivity at baseline (n = 3) or at least one year prior to progression (n = 1). CD138+ immunomagnetic separation is already performed in cytogenetic laboratories as part of the routine fluorescent in situ hybridization workflow, but efforts to increase its use are needed [16]. CD138+-selection to achieve a higher level of sensitivity was demonstrated in conjunction with next-generation flow cytometry (NGF) in PB of patients with MM but required substantially higher volumes (50 mL) and did not demonstrate superior sensitivity to bone marrow methods [17].
The results from our study build upon previously published data. In the IFM-2009 trial, patients received a fixed duration of one year of lenalidomide maintenance therapy. Patients with MRD 10−6 negativity following one year of maintenance lenalidomide had a 3-year PFS of approximately 75% from the time of maintenance discontinuation [5]. In the GEM2014MAIN trial of lenalidomide, dexamethasone, ±ixazomib maintenance following triplet induction and ASCT, patients with MRD < 10−6 by NGF after two years of maintenance underwent cessation of treatment; the 4-year PFS from treatment discontinuation was 82.8%, similar to our results [18]. These two studies examined the impact of cessation of maintenance therapy in patients who received triplet induction therapy. Our study included 40% of patients who received quadruplet induction and 36% who did not receive ASCT, along with variable durations of consolidation and maintenance therapy. This reflects a contemporary patient population that may be more generalizable to the current treatment landscape. Our results support the use of MRD < 10−6 as a minimum threshold for prompting a patient-centered discussion around treatment discontinuation. Notably, the MASTER trial employed a rapid MRD-guided discontinuation in patients who received quadruplet therapy and ASCT and found that sustained MRD 10−6 negativity was associated with improved PFS but sustained MRD 10−5 negativity was not [19].
Cost savings from the discontinuation of maintenance therapy could be substantial, which can be validated by a formal cost savings analysis. Second hematologic cancers occurred despite maintenance discontinuation; whether this risk can be reduced by earlier cessation of maintenance following exposure to high-dose melphalan is unknown.
There are several limitations to this study. This was a single institution, single-arm trial; the lack of randomization precludes our ability to determine if continuing lenalidomide would have led to better outcomes. There was a preponderance of patients who received multi-drug consolidation (77%), which is not universally done; the overrepresentation may be explained by multi-drug therapy being associated with superior PFS and sustained MRD negativity versus single agent maintenance [2, 12, 20, 21]. Few patients with two or more HRCAs were included in this study, which is reflective of the recalcitrant nature of this disease subset [12]. Our results are most applicable to patients in their first line of therapy without ultra-high-risk disease. It is possible hemodilution could have accounted for false negative NGS results; however, this is unlikely as we used first-pull aspirate for all NGS analyses, and the estimated quantity of cells in the CD138+-selected samples was much higher than what has been reported in PB in healthy individuals [22].
While patients could meet the criteria for death or progression at any point, MRD resurgence could have occurred earlier than the annual assessment. HRQoL surveys could have been biased as they were completed by a subset of patients. Lastly, 19% of patients had MRD positivity at 10−7, lower than the anticipated 40%; we have since expanded the study to enroll additional patients.
Our results suggest that MRD 10−7 status further informs on the risk of disease resurgence among patients discontinuing therapy. Decreasing the risk of disease resurgence may be important to patients. As such, this study identifies the need to further validate MRD < 10−7 as a potential guide for treatment discontinuation, performed both before and/or during maintenance therapy in the era of quadruplet induction which is responsible for exceptionally deep responses. We propose that MRD < 10−7 might further improve upon existing assays to guide earlier discontinuation of maintenance therapy or provide justification to forgo maintenance entirely. Considering that three patients had osseous lesions at relapse, incorporating optimal imaging and PB techniques to better characterize spatial heterogeneity [23] and its impact on disease re-emergence is another area for further study. Encouragingly, all five patients with relapse were successfully retreated, and three had again achieved MRD < 10−6.
If a cure is defined by the absence of disease in patients who have stopped treatment and with mortality similar to an age-matched population [24], patients with sustained MRD < 10−6 following discontinuation may ultimately fulfill this definition and prove that a cure is indeed possible in MM. Incorporation of MRD 10−7 testing, complementary imaging, and peripheral blood assays such as mass spectrometry using the intact light chain or clonotypic peptide approaches may help to further enhance our understanding of a cure.
In conclusion, discontinuation of maintenance therapy in patients with MM and multimodal MRD < 10−6 resulted in a low rate of disease progression or MRD resurgence. MRD-guided maintenance cessation may also improve HRQoL and could result in substantial cost savings. The results to date indicate that MRD assessed using the clonoSEQ assay with CD138+-enrichment to achieve 10−7 sensitivity may anticipate disease progression or conventional MRD resurgence, and consequently may help to better identify patients who can more confidently discontinue maintenance therapy with improved chances for a cure. Longer follow-up is needed to validate these preliminary results.
References
Munshi NC, Avet-Loiseau H, Anderson KC, Neri P, Paiva B, Samur M, et al. A large meta-analysis establishes the role of MRD negativity in long-term survival outcomes in patients with multiple myeloma. Blood Adv. 2020;4:5988–99.
Gay F, Musto P, Rota-Scalabrini D, Bertamini L, Belotti A, Galli M, et al. Carfilzomib with cyclophosphamide and dexamethasone or lenalidomide and dexamethasone plus autologous transplantation or carfilzomib plus lenalidomide and dexamethasone, followed by maintenance with carfilzomib plus lenalidomide or lenalidomide alone for patients with newly diagnosed multiple myeloma (FORTE): a randomised, open-label, phase 2 trial. Lancet Oncol. 2021;22:1705–20.
Avet-Loiseau H, San-Miguel J, Casneuf T, Iida S, Lonial S, Usmani SZ, et al. Evaluation of sustained minimal residual disease negativity with daratumumab-combination regimens in relapsed and/or refractory multiple myeloma: analysis of POLLUX and CASTOR. J Clin Oncol. 2021;39:1139–49.
San-Miguel J, Avet-Loiseau H, Paiva B, Kumar S, Dimopoulos MA, Facon T, et al. Sustained minimal residual disease negativity in newly diagnosed multiple myeloma and the impact of daratumumab in MAIA and ALCYONE. Blood. 2022;139:492–501.
Perrot A, Lauwers-Cances V, Corre J, Robillard N, Hulin C, Chretien M-L, et al. Minimal residual disease negativity using deep sequencing is a major prognostic factor in multiple myeloma. Blood. 2018;132:2456–64.
Diamond B, Korde N, Lesokhin AM, Smith EL, Shah U, Mailankody S, et al. Dynamics of minimal residual disease in patients with multiple myeloma on continuous lenalidomide maintenance: a single-arm, single-centre, phase 2 trial. Lancet Haematol. 2021;8:e422–e432.
Paiva B, Puig N, Cedena M-T, Rosiñol L, Cordón L, Vidriales M-B et al. Measurable residual disease by next-generation flow cytometry in multiple myeloma. JCO. 2019.
McCarthy PL, Holstein SA, Petrucci MT, Richardson PG, Hulin C, Tosi P, et al. Lenalidomide maintenance after autologous stem-cell transplantation in newly diagnosed multiple myeloma: a meta-analysis. J Clin Oncol. 2017;35:3279–89.
Jackson GH, Davies FE, Pawlyn C, Cairns DA, Striha A, Collett C, et al. Lenalidomide maintenance versus observation for patients with newly diagnosed multiple myeloma (Myeloma XI): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2019;20:57–73.
Richardson PG, Jacobus SJ, Weller EA, Hassoun H, Lonial S, Raje NS, et al. Triplet therapy, transplantation, and maintenance until progression in myeloma. N. Engl J Med. 2022;387:132–47.
Jasielec J, Kubicki T, Raje N, Vij R, Reece D, Berdeja JG et al. Carfilzomib, lenalidomide, and dexamethasone plus transplant in newly diagnosed multiple myeloma. Blood. 2020. https://doi.org/10.1182/blood.2020007522.
D’Agostino M, Bertuglia G, Rota-Scalabrini D, Belotti A, Morè S, Corradini P, et al. Predictors of unsustained measurable residual disease negativity in patients with multiple myeloma. Blood. 2024;143:592–6.
Guerrero C, Puig N, Cedena M-T, Calasanz M-J, Gutierrez NC, Fernandez M, et al. Predictors of unsustained measurable residual disease negativity in transplant-eligible patients with multiple myeloma. Blood. 2024;143:597–603.
Kvam AK, Fayers PM, Wisloff F. Responsiveness and minimal important score differences in quality-of-life questionnaires: a comparison of the EORTC QLQ-C30 cancer-specific questionnaire to the generic utility questionnaires EQ-5D and 15D in patients with multiple myeloma. Eur J Haematol. 2011;87:330–7.
Sully K, Trigg A, Bonner N, Moreno-Koehler A, Trennery C, Shah N, et al. Estimation of minimally important differences and responder definitions for EORTC QLQ-MY20 scores in multiple myeloma patients. Eur J Haematol. 2019;103:500–9.
Yu Y, Brown Wade N, Hwang AE, Nooka AK, Fiala MA, Mohrbacher A, et al. Variability in cytogenetic testing for multiple myeloma: a comprehensive analysis from across the United States. JCO Oncol Pract. 2020;16:e1169–e1180.
Notarfranchi L, Zherniakova A, Lasa M, Puig N, Cedena MT, Martinez-Lopez J, et al. Ultra-sensitive assessment of measurable residual disease (MRD) in peripheral blood (PB) of multiple myeloma (MM) patients using bloodflow. Blood. 2022;140:2095–7.
Rosiñol L, Oriol A, Ríos R, Blanchard MJ, Jarque I, Bargay J, et al. Lenalidomide and dexamethasone maintenance with or without ixazomib, tailored by residual disease status in myeloma. Blood. 2023;142:1518–28.
Costa LJ, Chhabra S, Medvedova E, Dholaria BR, Schmidt TM, Godby KN et al. Minimal residual disease response-adapted therapy in newly diagnosed multiple myeloma (MASTER): final report of the multicentre, single-arm, phase 2 trial. Lancet Haematol. 2023. https://doi.org/10.1016/S2352-3026(23)00236-3.
Dytfeld D, Wróbel T, Jamroziak K, Kubicki T, Robak P, Walter-Croneck A, et al. Carfilzomib, lenalidomide, and dexamethasone or lenalidomide alone as maintenance therapy after autologous stem-cell transplantation in patients with multiple myeloma (ATLAS): interim analysis of a randomised, open-label, phase 3 trial. Lancet Oncol. 2023;24:139–50.
Rodríguez-Otero P, Moreau P, Dimopoulos MA, Beksac M, Perrot A, Broijl A, et al. Daratumumab (DARA) + bortezomib/lenalidomide/dexamethasone (VRd) in transplant-eligible (TE) patients (pts) with newly diagnosed multiple myeloma (NDMM): analysis of minimal residual disease (MRD) in the PERSEUS trial. JCO. 2024;42:7502.
Caraux A, Klein B, Paiva B, Bret C, Schmitz A, Fuhler GM, et al. Circulating human B and plasma cells. Age-associated changes in counts and detailed characterization of circulating normal CD138− and CD138+ plasma cells. Haematologica. 2010;95:1016–20.
Rasche L, Chavan SS, Stephens OW, Patel PH, Tytarenko R, Ashby C, et al. Spatial genomic heterogeneity in multiple myeloma revealed by multi-region sequencing. Nat Commun. 2017;8:268.
Derman BA, Jakubowiak AJ. Moving toward a cure in multiple myeloma: eradication of measurable residual disease. Adv Oncol. 2022;2:159–69.
Acknowledgements
The authors thank: the patients and their families for participating in this study; Allison Jacob, Lanny Kirsch, Kayla Layng, and Heidi Simmons at Adaptive Biotechnologies for their assistance with MRD analyses; Luis Alcantar, Evangelia Andreatos, Karson Buckley, Camila Duarte, Martha Hodges, Bernadette Libao, Sarah Major, Allison Marthaler, Amanda McIver, Samrawit Melka, Megan Whelan, and Brittany Wolfe at the University of Chicago for their assistance in conducting this study.
Author information
Authors and Affiliations
Contributions
B.A.D., Th.K., and A.J.J. were responsible for designing the protocol, statistical design, and data analysis. Th.K. was responsible for statistical design and data analysis. K.J. and A.R. were responsible for processing patient samples. B.A.D. was responsible for data analysis and initial paper drafting. A.M. was responsible for initial quality-of-life data analysis. All authors were responsible for interpretation of results, and paper revisions and final approval.
Corresponding author
Ethics declarations
Competing interests
B.A.D. declares consultancy for Johnson & Johnson, Sanofi, Canopy, and Cota Inc.; independent clinical trial reviewer for BMS; research funding from GSK and Amgen. A.M., J.C., K.J., A.R., Th.K., and Ta.K. have nothing to disclose. A.J.J. declares honoraria and advisory board fees from Abbvie, Amgen, Bristol-Myers Squibb/Celgene, GlaxoSmithKline, Gracell, Janssen, and Sanofi.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Derman, B.A., Major, A., Cooperrider, J. et al. Discontinuation of maintenance therapy in multiple myeloma guided by multimodal measurable residual disease negativity (MRD2STOP). Blood Cancer J. 14, 170 (2024). https://doi.org/10.1038/s41408-024-01156-x
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-024-01156-x
This article is cited by
-
Evolution of clonal hematopoiesis on and off lenalidomide maintenance for multiple myeloma
Leukemia (2025)
-
Opportunities and challenges for MRD assessment in the clinical management of multiple myeloma
Nature Reviews Clinical Oncology (2025)
-
Attitudes and perspectives of oncologists about measurable residual disease testing in multiple myeloma: initiative for standardizing guidelines
Bone Marrow Transplantation (2025)
-
EHA–EMN Evidence-Based Guidelines for diagnosis, treatment and follow-up of patients with multiple myeloma
Nature Reviews Clinical Oncology (2025)