Abstract
Double-hit (DHL) and double expressor (DEL) DLBCL have poor prognosis with standard therapy but CART may overcome this poor prognostic impact. In this multicenter retrospective study, we sought to confirm this observation by evaluating survival outcomes among patients with relapsed/refractory DHL and DEL treated with CART and evaluate outcomes of relapse post-CART. A total of 408 adult patients with relapsed/refractory DLBCL from 13 academic centers were included based on the availability of DHL and DEL. All 408 patients were included in the DHL (n = 80) vs non-DHL (n = 328) analysis, while 333 patients were included in the analysis of DHL (n = 80) vs DEL (n = 74) vs non (n = 179). On MVA, there were no differences for PFS for DHL vs non-DHL (HR 0.8, 95%CI 0.5–1.3, p = 0.35) or DHL vs DEL vs other (three-way p value, p = 0.5). Response rates and toxicities were similar among groups. Patients with DEL had the highest relapse rates post-CART, while DHL had the worst overall survival after CART relapse. In sum, our data support the notion that CART cell therapy can overcome the poor prognostic impact of DHL and DEL DLBCL in the relapsed/refractory setting. Additionally, patients with DHL that relapse after CART have a very poor prognosis.
Similar content being viewed by others
Introduction
Diffuse Large B Cell Lymphoma (DLBCL) is an aggressive subtype of non-Hodgkin lymphoma (NHL), making up about 25–30% of NHL cases worldwide. Treatment with anthracycline-based therapy can cure the majority of patients. However, ~30% of patients will have relapsed or refractory disease [1, 2]. Patients with DLBCL with dual expression of MYC and BCL-2 proteins not related to underlying chromosomal rearrangements, termed double expressor lymphoma (DEL), or high-grade B-cell lymphoma with dual rearrangements of MYC and BCL-2 or/and BCL-6, synonymous with “double-hit” (DHL) and “triple-hit” (THL) lymphoma respectively according to the World Health Organization (WHO) 2016 classification [3], are more likely to relapse after standard frontline chemo-immunotherapy [4,5,6]. This is despite the recent reclassification of high-grade B-cell lymphomas (HGBCL), use of novel therapeutics, and/or dose intensification of frontline chemo-immunotherapy [7,8,9,10]. Moreover, relapses in these subsets of patients tend to be early, within 12 months of frontline therapy [5]. Consequently, there is an urgent need to identify effective treatments for these subgroups.
Several studies have demonstrated high efficacy with CD19-directed autologous chimeric antigen receptor T-cell (CART) therapy for DHL/THL patients as defined by WHO 2016. In the third-line setting, axicabtagene ciloleucel (axi-cel), lisocabtagene maraleucel (liso-cel) and tisagenlecleucel (tisa-cel), all demonstrated similar overall response rates (ORR) for DHL and non-DHL patients [11,12,13]. In the second line setting, both axi-cel and liso-cel showed improvements in EFS for DHL patients compared to standard-of-care high-dose chemotherapy (HR 0.28 95% CI, 0.14–0.59 and HR 0.456 95%CI:0.226–0.921, respectively) [14, 15] In addition, axi-cel showed a similar improvement for a small cohort of DEL patients (HR 0.42 95% CI 0.27–0.67) [16, 17].
However, for the aforementioned CART trials collectively, there are obvious limitations to the generalizability of CART efficacy in patients with DHL/THL or DEL. One limitation is that these cohorts were small in number, and subset analyses evaluating outcomes were, in some cases, ad hoc and/or not powered to provide clear direction on the efficacy of CART [11,12,13,14,15,16,17]. It is also unclear whether the durability of responses and survival outcomes in DHL/THL and DEL truly mirror those of patients with DLBCL without these high-risk features. Additionally, with the increasing employment of CART in second-line therapy, it is imperative to better estimate expected survival with CART and establish a benchmark for future studies targeting these high-risk patient populations.
Thus, we performed a multicenter retrospective analysis to address these gaps in knowledge. Specifically, we evaluated the efficacy of CART and practice patterns post-CART relapse in large cohorts of DHL and DEL patients to better characterize the outcomes for these high-risk subsets treated with CART.
Materials/subjects and methods
Study design and participants
Data were collected from adult patients with R/R aggressive B-NHL treated with CART from 2015–2021 across 13 academic institutions in the United States (n = 536). We excluded histologic subtypes other than de novo DLBCL and transformed follicular lymphoma (n = 59) and patients with missing MYC status by fluorescence in situ hybridization (FISH; n = 69); accordingly, a total of 408 patients were analyzed. Two separate comparative analyses were performed. First, DHL was compared to non-DHL. Second, a three-way comparison was made between DHL, DEL, and others. Due to limitations from missing data, separate analyses allowed more robust evaluation of DHL, which is thought to have a more significant prognostic impact on DLBCL outcomes. DHL was defined as patients with rearrangements of MYC and BCL-2 and/or BCL-6 irrespective of MYC or BCL-2 expression [3]. Patients with DEL were defined as having increased expression of MYC (>40%) and BCL-2 (>70%) by immunohistochemistry without chromosomal rearrangements involving MYC or BCL-2 by FISH. Patients with missing DEL status were excluded only from the DHL vs DEL vs other analysis (n = 75).
Statistical analysis
Baseline characteristics were compared between cohorts with Pearson Chi-squared test and included: age, gender, histology, cell of origin (COO), international prognostic index score (IPI), LDH level at apheresis, prior autoHCT, presence of bulky disease, number of lines of therapy prior to apheresis, use of bridging therapy (BT), time from diagnosis to CART infusion, time from apheresis to CART infusion, rates of utilization of CART on the clinical trial, type of CART product utilized, rates and grades of cytokine release syndrome (CRS) and immune effector cell associated neurotoxicity syndrome (ICANS). Median progression-free survival (mPFS) and median overall survival (mOS) were estimated via the Kaplan–Meier method. PFS was defined as time from CART infusion to date of progression or death, while OS was defined as time from CART infusion to date of death from any cause. Clinical variables associated with PFS on univariate analysis were incorporated into the Cox multivariable regression analysis (MVA) to determine the impact of clinical variables on CART PFS. A p value <0.05 was significant.
Results
Patient characteristics
A total of 408 patients were included in the DHL vs non-DHL analysis. There were 80 patients with DHL and 328 patients with non-DHL. The DHL group included a small subset of six patients with MYC/BCL-6 rearrangements. Patients with DHL had similar rates of BT use, time from apheresis to CART, CART utilization on clinical trials, and CAR-T product compared to non-DHL. Not surprisingly, DHL were enriched for germinal center COO (GCB; 87.2 vs 44.5%, p < 0.001), elevated LDH (80.4 vs 62.8%, p < 0.02), and CART as second-line therapy rather than later line therapy (20.0 vs 10.4%, p < 0.02) compared to non-DHL, in keeping with the known pathobiology of DHL.
For DHL vs DEL vs other, a total of 333 patients were included in this analysis. There were 80 patients with DHL, 74 patients with DEL, and 179 non-DHL/DEL patients (patients with missing DEL status were excluded, n = 75; Table 1). All groups had similar time from apheresis to CART infusion, rates of utilization of CART on clinical trials, and type of CART product. As expected, patients with DHL were more likely to have GCB COO (87.2 vs 58.1% vs 54.7%, p < 0.001). DHL and DEL appeared to have more frequent elevations of LDH (80.4 vs 74.6 vs 58.4%, p < 0.006). This trend was correlated to some degree with tumor bulk as patients with DEL and DHL were more likely to have bulky disease at diagnosis (39.7% with DEL vs 31.2% with DHL and 21.2% with other, p < 0.01), although DEL had the highest proportion of bulky disease overall. Patients with DEL also had the highest use of BT (60.6%), while DHL surprisingly had the lowest rate of BT utilization at 34.2 and 44.7% in others (p < 0.02).
Toxicity
Rates of CRS overall were numerically higher among patients in the DEL group (72.7%) compared to the DHL group (66.3%) and the non-DHL group (68.3%), although this did not approach statistical significance (p = 0.664). Rates of high-grade CRS (grade 3 or 4), on the other hand, were highest among the DHL group (17.5%) vs 13.0% in DEL and 10.0% in the non-DHL group (p = 0.192). As a surrogate for tumor burden, which can be predictive of toxicities, groups were well balanced for high LDH with 66.7, 66.7, and 68.0% of patients having elevated LDH, respectively. Rates of any grade ICANS (53.2%) and severe ICANS (22.1%) were slightly higher among patients in the DEL group compared to DHL (46.8% any grade, 18.8% high-grade) and non-DHL (45.9% any grade, 17.8% high grade), without reaching significance (p = 0.526 for any grade ICANS and p = 0.696 for high-grade). This trend was not explained by high LDH, as only 43.8% of DEL patients with high-grade ICANS had an elevated LDH compared to 71.4% of DHL patients and 60% of non-DHL patients (p = 0.295).
Response rates
Although not statistically significant, there was a trend toward an improved response to CART for DHL vs non-DHL (ORR 69 vs 66%, p = 0.7; CR 49 vs 48%, p = 0.8). This difference was more pronounced when we evaluated response rates separately for de novo HGBCL and for transformed follicular lymphoma (tFL). In the de novo HGBCL subgroup, the trend toward improved response rates for DHL (n = 51 DHL vs n = 266 for non-DHL) was still present with ORR rates of 64 vs 53% (p = 0.2) and CR rates of 48 vs 35% (p = 0.1). In the tFL subgroup, the same trend was preserved as well for ORR [tFL DHL (n = 19) vs tFL non-DHL (n = 62)] with 84% for DHL vs 74% for non-DHL (p = 0.5) while the CR rates were equal at 53% (p > 0.99).
CART response rates were similar for DHL vs DEL vs other (ORR 69 vs 64 vs 66%, p = 0.8; CR rate 49 vs 42 vs 48%, p = 0.6), with a non-significant trend toward DEL having the poorest response.
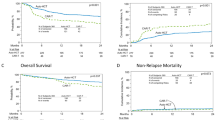
Progression-free and overall survival
The median follow-up post-CART infusion was 17.7 months. The mPFS was similar for DHL vs non-DHL (mPFS 7.5 vs 6.2 months, p = 0.2 [Fig. 1A]). The mOS, on the other hand, numerically trended in favor of non-DHL with mOS 21 months for DHL vs NR for others, but this did not reach statistical significance (p = 0.6 [Fig. 1C]). Interestingly, the trend shifted toward improved survival in favor of DHL when evaluating mOS in the tFL subgroup (NR vs 29 months, p = 0.07). When comparing DHL vs DEL vs other, the median follow-up time post-CART was 18.7 months in surviving patients. The mPFS and mOS were similar (mPFS 7.5 vs 6.2 vs 9.0 months, p = 0.35; Fig. 1B; mOS NR vs 19.1 vs 25.7 months, p = 0.8, Fig. 1D). Of note, patients with CR post-CART had similar PFS and OS regardless of DHL vs DEL vs other status (Fig. 2). The same was true for patients with PR; however, outcomes in patients with PR in response to CART were poor across all cohorts (Fig. 2).
PFS after CART exposure in DHL vs non-DHL (A) and DHL vs DEL vs other (B). OS after CART exposure in DHL vs non-DHL (C) and DHL vs DEL vs other (D). CART chimeric antigen receptor T-cell therapy, DEL double expressor lymphoma, DHL double hit lymphoma, Mon months, No number, OS overall survival, PFS progression- free survival.
On multivariate analysis (MVA) for PFS and OS, variables included elevated LDH, COO, number of prior lines of therapy, treatment with CART on a clinical trial, use of BT, and time from apheresis to CART infusion. On MVA for PFS for DHL vs non-DHL (n = 408), there was a non-significant PFS advantage for the DHL group (HR 0.8, 95% CI 0.5–1.3, p = 0.35). However, greater than two lines of therapy pre-apheresis (HR 1.6, 95% CI 1.2–2.2, p = 0.003), use of BT (HR 1.7, 95% CI 1.3–2.4, p < 0.001), and elevated LDH at time of apheresis (HR 1.5, 95% CI 1.1–2.1, p = 0.009) were predictive of inferior PFS on MVA for all patients regardless of DHL status. On MVA for OS in these cohorts, these variables also predicted reliably for inferior OS, each with an HR 1.7 (95% CI 1.2–2.4, p = 0.003–0.008). Of note, when we excluded DHL patients with MYC and BCL-6 translocations to match the WHO 2022 reclassification of HGBCL, there were no significant differences in the MVA results (Supplementary Tables 2 PFS, 3 OS).
When comparing DHL vs DEL vs other on MVA (n = 333), there was no difference in CART PFS between cohorts (three-way p value, p = 0.5). However, once again, two lines of therapy pre-apheresis was predictive for PFS (HR 1.6, 95% CI 1.2–2.2, p = 0.003) and OS (HR 1.7, 95% CI 1.2–2.4, p = 0.003), and use of BT impacted PFS (HR 1.7, 95% CI 1.2–2.3, p = 0.001) and OS (HR 1.7, 95% CI 1.2–2.4, p = 0.004) for all patients. Elevated LDH at the time of apheresis also predicted for inferior PFS (HR 1.5, 95% CI 1.1–2.0, p = 0.01) and OS (HR 1.7, 95% CI 1.2–2.5, p = 0.003) for all patients.
Practice patterns and outcomes post-CART failure
For DHL vs non-DHL analyses: Patients with non-DHL were more likely to relapse after CART at 58.3% compared to DHL with only 50% relapse with a trend nearly reaching statistical significance (p = 0.083) Median time to progression post-CART was 89 days in both DHL and non-DHL groups. Rates of receipt of lymphoma-directed therapy after progression were numerically higher in the non-DHL group (54% in DHL vs 67% in non-DHL; p = 0.2). As the first-subsequent treatment after CART progression/relapse, patients with DHL were more likely to receive radiation alone (37%) as compared to patients with non-DHL (15%; p = 0.045) and less likely to be enrolled on a clinical trial (0 vs 26%; p = 0.007). Radiation was utilized most commonly (n = 7) followed by lenalidomide based therapy (n = 6 including two patients who received tafasitamab and lenalidomide), and ibrutinib (n = 2).
Patients with DHL had inferior response rates with first-subsequent therapy post-CART with ORR of 11% and CR of 0% compared to 43% (p = 0.01) and 19% (p = 0.04) for non-DHL. In addition to inferior response rates, patients in the DHL group had inferior progression-free survival with subsequent therapy post-CART failure (mPFS was 21 vs 70 days for DHL vs non-DHL patients who received post-CART failure therapy, p < 0.0001). The DHL group had an inferior OS post-CART progression as compared to non-DHL (2.7 vs 6.0 months; p = 0.02).
For DHL vs DEL vs other analyses: Relapse rates were highest among those with DEL (67.5%) compared to DHL (50%) and non-DHL patients (58.3%). After CART relapse, patients had similar rates of receiving further treatment regardless of subgroup (54.2 vs 72.7 vs 67.4%, p = 0.2) with a non-significant trend for less utilization in DHL. Although there were no differences noted in rates of relapse post-CART, patients with DHL had significantly inferior mOS (2.7 months) after progression vs 6 months for DEL and 5.8 months for other (DHL n = 35; DEL n = 46; other n = 92, p = 0.04; Fig. 3). The difference in mOS post-CAR-T progression for DEL and other was not significant (p = 0.99). Although the cause of death was not consistently collected in all patients, all but three patients had disease progression at last follow-up in the DHL cohort.
Discussion
CD19-directed CART therapy has been a groundbreaking advance in the management of aggressive large B-cell lymphoma (LBCL). It is curative in 30–40% of patients based on long-term follow-up of prospective trials evaluating CART in the second and third line and beyond [11,12,13, 15, 16]. However, whether this benefit extends to patients with high-risk features such as DHL/THL and DEL was not clear, given the small numbers of such patients included in these trials.
In our large multicenter retrospective study of patients with LBCL undergoing CD19-directed autologous CART, we identified sizeable cohorts of patients with DHL/THL and DEL. Our real-world dataset across 13 academic institutions included a higher incidence of patients with DHL than historically included on any prospective CART trial and highlighted the ability of CART to level the playing field regardless of DHL or DEL status. In particular, patients with DHL arising from the transformation of FL derived substantial benefits.
In addition, our study describes and compares outcomes for these subgroups after CART failure. In our cohort as a whole, we previously reported mPFS and mOS of 7.6 months and 25.6 months, respectively, post-CAR T failure, consistent with results seen in prospective studies [18]. In this analysis, however, we demonstrate that patients with DHL have dismal outcomes with a mOS of less than 3 months following CART progression. Although cause of death was not collected, all but 3 patients who died had disease progression at last follow-up. Since mPFS for DHL/THL vs DEL vs other were comparable with CART, the poor OS outcomes in DHL are likely secondary to a shorter mPFS2 after CART failure. Non-responders with DHL were more likely to be salvaged with radiation rather than systemic therapy, which may have led to inadequate systemic control. Reasons for these practices are unclear and may reflect concern for patient frailty and/or cytopenias post-CART progression.
In 2023, two CD20-CD3 bispecific antibodies—epcoritamab and glofitamab were granted accelerated approval by the United States Food and Drug Administration (FDA) for treatment of LBCL in the third line and beyond. However, it is important to note that fewer than 15% of patients enrolled in prospective trials for these agents had DHL/THL. Our dataset is limited in providing further information on bispecific antibodies efficacy post-CART failure as it predates approval of these agents. Thus, it remains ambiguous whether these agents offer benefits in DHL/THL as salvage after CART failure. Additionally, since early relapse appears to predict poor response to bispecifics, it is possible these agents will offer less benefit to patients with DHL, as the majority of DHL patients in our study relapsed within 90 days of CART infusion [19,20,21,22]. As DHL remains a population of high unmet need and should be targeted for the investigation of novel therapies post-CART failure.
Despite the promising findings in terms of CART efficacy in patients with DHL and DEL, our study does come with the inherent biases of retrospective studies, including selection bias. In addition, although the current WHO classification has removed patients with MYC and BCL-6 translocations from the DHL category, we included them in our analyses as the pivotal CD19 CART trials included these patients and were the foundation of our study. Of note, the MVA analysis for survival outcomes was not influenced by the removal of this subgroup (Supplementary Tables 2, 3). Finally, there were a large number of patients that were excluded from our analysis due to missing data on DHL and DEL status. Survival outcomes of this group of patients with missing data were not different from the other groups analyzed suggesting that exclusion of these patients did likely not introduce significant bias in the survival analyses (Supplementary Fig. 1).
Despite these limitations, we present the largest analysis characterizing CART survival outcomes in R/R DHL and DEL to date and demonstrate that mPFS and mOS mirrors that of DLBCL patients without these high-risk features. In fact, there were non-significant trends toward improved outcomes in the DHL group, which in other treatment settings is considered the highest risk. This trend appeared most significant for DHL arising in tFL patients. Overall, our data support the use of CART in these high-risk patients. Patients with DHL progressing after CART have the most dismal survival, reflecting an urgent need for effective therapies post-CART failure. Trials exploring novel therapies post-CART could be specifically designed to enrich this population with more directed inclusion criteria to address this unmet need in the future.
Data availability
Data were available upon request of the corresponding author.
References
Coiffier B, Thieblemont C, Van Den Neste E, Lepeu G, Plantier I, Castaigne S, et al. Long-term outcome of patients in the LNH-98.5 trial, the first randomized study comparing rituximab-CHOP to standard CHOP chemotherapy in DLBCL patients: a study by the Groupe d’Etudes des Lymphomes de l’Adulte. Blood. 2010;116:2040–5.
Pfreundschuh M, Kuhnt E, Trumper L, Osterborg A, Trneny M, Shepherd L, et al. CHOP-like chemotherapy with or without rituximab in young patients with good-prognosis diffuse large-B-cell lymphoma: 6-year results of an open-label randomised study of the MabThera International Trial (MInT) Group. Lancet Oncol. 2011;12:1013–22.
Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127:2375–90.
Johnson NA, Savage KJ, Ludkovski O, Ben-Neriah S, Woods R, Steidl C, et al. Lymphomas with concurrent BCL2 and MYC translocations: the critical factors associated with survival. Blood. 2009;114:2273–9.
Petrich AM, Gandhi M, Jovanovic B, Castillo JJ, Rajguru S, Yang DT, et al. Impact of induction regimen and stem cell transplantation on outcomes in double-hit lymphoma: a multicenter retrospective analysis. Blood. 2014;124:2354–61.
Hu S, Xu-Monette ZY, Tzankov A, Green T, Wu L, Balasubramanyam A, et al. MYC/BCL2 protein coexpression contributes to the inferior survival of activated B-cell subtype of diffuse large B-cell lymphoma and demonstrates high-risk gene expression signatures: a report from The International DLBCL Rituximab-CHOP Consortium Program. Blood. 2013;121:4021–31.
Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, Araujo IBO, Berti E, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia. 2022;36:1720–48.
Godfrey JK, Nabhan C, Karrison T, Kline JP, Cohen KS, Bishop MR, et al. Phase 1 study of lenalidomide plus dose-adjusted EPOCH-R in patients with aggressive B-cell lymphomas with deregulated MYC and BCL2. Cancer. 2019;125:1830–6.
Pillai RK, Sathanoori M, Van Oss SB, Swerdlow SH. Double-hit B-cell lymphomas with BCL6 and MYC translocations are aggressive, frequently extranodal lymphomas distinct from BCL2 double-hit B-cell lymphomas. Am J Surg Pathol. 2013;37:323–32.
Staiger AM, Ziepert M, Horn H, Scott DW, Barth TFE, Bernd HW, et al. Clinical impact of the cell-of-origin classification and the MYC/ BCL2 dual expresser status in diffuse large B-cell lymphoma treated within prospective clinical trials of the German High-Grade Non-Hodgkin’s Lymphoma Study Group. J Clin Oncol. 2017;35:2515–26.
Abramson JS, Palomba ML, Gordon LI, Lunning MA, Wang M, Arnason J, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet. 2020;396:839–52.
Schuster SJ, Svoboda J, Chong EA, Nasta SD, Mato AR, Anak Ö, et al. Chimeric antigen receptor T cells in refractory B-cell lymphomas. N Engl J Med. 2017;377:2545–54.
Neelapu SS, Jacobson CA, Ghobadi A, Miklos DB, Lekakis LJ, Oluwole OO, et al. Five-year follow-up of ZUMA-1 supports the curative potential of axicabtagene ciloleucel in refractory large B-cell lymphoma. Blood. 2023;141:2307–15.
Locke FL, Miklos DB, Jacobson CA, Perales M-A, Kersten M-J, Oluwole OO, et al. Axicabtagene ciloleucel as second-line therapy for large B-cell lymphoma. N Engl J Med. 2021;386:640–54.
Kamdar M, Solomon SR, Arnason J, Johnston PB, Glass B, Bachanova V, et al. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet. 2022;399:2294–308.
Westin JR, Oluwole OO, Kersten MJ, Miklos DB, Perales MA, Ghobadi A, et al. Survival with axicabtagene ciloleucel in large B-cell lymphoma. N Engl J Med. 2023;389:148–57.
Locke FL, Ghobadi A, Jacobson CA, Miklos DB, Lekakis LJ, Oluwole OO, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large B-cell lymphoma (ZUMA-1): a single-arm, multicentre, phase 1-2 trial. Lancet Oncol. 2019;20:31–42.
Zurko J, Nizamuddin I, Epperla N, David K, Cohen JB, Moyo TK, et al. Peri-CAR-T practice patterns and survival predictors for all CAR-T patients and post-CAR-T failure in aggressive B-NHL. Blood Adv. 2023;7:2657–69.
Hutchings M, Morschhauser F, Iacoboni G, Carlo-Stella C, Offner FC, Sureda A, et al. Glofitamab, a novel, bivalent CD20-targeting T-cell–engaging bispecific antibody, induces durable complete remissions in relapsed or refractory B-cell lymphoma: a phase I trial. J Clin Oncol. 2021;39:1959–70
Hutchings M, Mous R, Clausen MR, Johnson P, Linton KM, Chamuleau MED, et al. Subcutaneous epcoritamab induces complete responses with an encouraging safety profile across relapsed/refractory B-cell non-Hodgkin lymphoma subtypes, including patients with prior CAR-T therapy: updated dose escalation data. Blood. 2020;136:45–46.
Dickinson MJ, Carlo-Stella C, Morschhauser F, Bachy E, Corradini P, Iacoboni G, et al. Glofitamab for relapsed or refractory diffuse large B-cell lymphoma. N Engl J Med. 2022;387:2220–31.
Thieblemont C, Phillips T, Ghesquieres H, Cheah CY, Clausen MR, Cunningham D, et al. Epcoritamab, a novel, subcutaneous CD3xCD20 bispecific T-cell-engaging antibody, in relapsed or refractory large B-cell lymphoma: dose expansion in a phase I/II trial. J Clin Oncol. 2023;41:2238–47.
Acknowledgements
We would like to acknowledge the patients who are stricken with this terrible disease, without whom we would not be able to perform this research.
Author information
Authors and Affiliations
Contributions
RK and GS wrote the manuscript, RK, GS, PT, TM, JR, SB, RB, JC, NS, JZ, VK, BH, DS, LF, TO, BT, IR, SM, JW, BP, JM, AD, KD, LG, and NE all contributed to manuscript preparation, data collection, and analysis.
Corresponding author
Ethics declarations
Competing interests
NE: Research funding: Beigene, Eli Lilly; Speakers Bureau for Beigene, Incyte, and Novartis; Honoraria/consulting/ad boards for Merck, ADC Therapeutics, Ipsen, Lilly, and Novartis. GS: Advisory boards: Kite, Beigene, AstraZeneca; Speakers Bureau: Kite, Beigene. JR: Research funding: Merck, Corvus Pharmaceuticals, Kymera Therapeutics; Consulting: Acrotech Biopharma, Kyowa Kirin. TKM: Advisory board for Seattle Genetics. TAO: Research support from ONO and LOXO. Consulting for ONO, ADC therapeutics. SM: Research funding: Abbvie, AstraZeneca, BeiGene, Janssen, Juno, Loxo, TG Therapeutics. Speakers Bureau: AstraZeneca, BeiGene, Lilly. Advisory boards: Abbvie, AstraZeneca, BMS, Genentech, Janssen. JNW: Research funding and honoraria from Merck. DMS: consulting fees from Abbvie, AstraZeneca, Beigene, BMS, Celgene, Eli Lilly, Genentech, and Janssen. Institutional research funding from AstraZeneca, Novartis. AVD: consulting fees from Abbvie, AstraZeneca, BeiGene, Bristol Meyers Squibb, Genentech, GenMab, Incyte, Janssen, Lilly Oncology, MEI Pharma, Merck, Nurix and Prelude and has ongoing research funding from Abbvie, AstraZeneca, Bayer Oncology, Beigene, Bristol Meyers Squibb, Cyclacel, GenMab, Lilly Oncology, MEI Pharma, Morphosys and Nurix. NNS: consultancy or advisory committee participation with Miltenyi Biotec, Lilly Oncology, BMS/Juno, Galapagos, Gilead/Kite, Abbvie, Incyte, Seattle Genetics. He has research funding from both Miltenyi Biotec and Lilly Oncology and is on the scientific advisory board for Tundra Therapeutics. SKB: Honoraria: Acrotech, Affimed, Daiichi Sankyo, Kyowa Kirin, Janssen, Seagen. MC: Advisory Board: ADC therapeutics, AstraZeneca, Cellectar, Synthekine; Consultancy: Abbvie: Speaker’s Bureau: Curio Life Sciences, Precision Oncology, Secura Bio. JBC: Consultant/Advisor: AstraZeneca, Abbvie, BeiGene, Janssen, Loxo/Lilly, Kite/Gilead, ADCT; Research Funding: LLS, Genentech, AstraZeneca, Novartis, Loxo/Lilly, BMS/Celgene. ASK: Research funding from AstraZeneca and BeiGene. Advisory boards for AstraZeneca, Abbvie, BeiGene, Bristol-Myers Squibb, Janssen, Kite a Gilead Company, Lox@Lilly. Speakers bureau for BeiGene. RK: Advisory Board: AstraZeneca, BMS, Morphosys/Incyte, Genentech/Roche, Abbvie, Lilly Oncology, Miltenyi; Speakers Bureau: BeiGene, AstraZeneca, Morphosys/Incyte. The remaining authors declare no competing interests.
Ethics
Our study was based on data collected from a retrospective chart review. As such, participants were not exposed to greater than minimal risk and, therefore not consented to the study. The protocol was IRB-approved at all participating institutions, including the Northwestern University Central Institutional Review Board (date of approval January 26, 2021) where the data was collated and analyzed. We confirm that all methods were performed in accordance with the relevant guidelines and regulations.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Karmali, R., Shouse, G., Torka, P. et al. Double hit & double expressor lymphomas: a multicenter analysis of survival outcomes with CD19-directed CAR T-cell therapy. Blood Cancer J. 15, 43 (2025). https://doi.org/10.1038/s41408-025-01250-8
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41408-025-01250-8