Abstract
The revised international staging system (R-ISS) in multiple myeloma (MM) was recently updated as the second R-ISS (R2-ISS) and refined prognostication in clinical trial populations. By including 2929 Danish patients with MM and complete data on R2-ISS registered from 2005 through 2019, we validated the R2-ISS for overall survival (OS) in a population-based cohort; however, only partly among younger patients. We thus developed a real-world international staging system (RW-ISS) from a 75% training cohort. Feature selection and weighted scores of high-risk variables from a Cox regression model of OS included age >70 years (2 points), performance status (PS) > 1 (2 points), PS 1 (1 point), t(14;16) (1 point), ISS III (1 point), ISS II (0.5 points), high lactate dehydrogenase (0.5 points), and del(17p) (0.5 points). In the test set, patients with RW-ISS I (0–2.0 points, 38.2%), II (2.5–3.0 points, 19.8%), III (3.5–4.5 points, 27.1%), and IV (5.0–7.0 points, 15.0%) demonstrated a median OS of 9.5, 5.5, 3.4, and 1.1 years, respectively (P < 0.0001) and the C-index was superior for RW-ISS as compared to both R2-ISS and R-ISS (0.708 vs 0.604 vs 0.595, respectively). RW-ISS was in part externally validated. We thus recommend using RW-ISS in routine clinical care of NDMM.
Similar content being viewed by others
Introduction
Prognostication is key in patients with multiple myeloma (MM) who demonstrate highly heterogenous clinical outcomes from time of diagnosis. Since 2015, the revised international staging system (R-ISS) has been recommended as the gold standard for prognostication in patients with newly diagnosed MM (NDMM) [1]. On top of the former international staging system (decreased albumin and increased beta-2-microglobulin [B2M] levels), the R-ISS included lactate dehydrogenase (LDH) levels and adverse cytogenetic aberrations (CA) defined as t(4;14), t(14;16) and del(17p) detected by fluorescence in situ hybridization (FISH). However, only 3–5% of patients with NDMM harbor t(14;16), and its independent prognostic value has been questioned [2, 3]. Larger studies of patients with t(14;16) have been conducted without questioning the prognostic relevance of t(14;16) [4, 5]. Further, the distribution of patients into R-ISS I, II and III is uneven, which has led to inconclusive subgroup analyses due to small numbers [6, 7].
Based on these observations, the second R-ISS (R2-ISS) was recently developed to improve prediction of overall survival (OS) [8]. Developed as a prognostic index from a multivariable analysis in patients from randomized clinical trials, the R2-ISS score is calculated based on ISS III (1.5 point), ISS II (1 point), elevated LDH (1 point), presence of del(17p) (1 point), t(4;14) (1 point) and +1q (0.5 points), and patients are subsequently grouped into low (0 points), low-intermediate (0.5 to 1 points), intermediate-high (1.5 to 2.5 points) and high risk (≥3 points). Both the training and validation cohort consisted exclusively of patients enrolled in randomized clinical trials [8]. However, the differences between patients from clinical trials and those in real-world populations are significant [9, 10]. In general, real-world populations tend to be older patients enriched with high-risk features and clinical outcomes are worse as compared to clinical trial populations – especially for transplant-ineligible patients [9, 10]. Importantly, most patients in real-world populations do not fulfill inclusion criteria for clinical trials of NDMM, mainly due to kidney failure, comorbidity and poor Eastern Cooperative Oncology Group (ECOG) performance status (PS) [10]. At the same time, the prognostic role of +1q aberrations remain conflicting, likely because of the importance of copy numbers which was not available in the R2-ISS dataset [8, 11].
In this study, we aimed to validate R2-ISS in a population-based nationwide cohort in subgroups of transplant-eligible and transplant-ineligible MM patients, and to improve prognostication in real-world populations.
Methods
We included all Danish patients registered with MM in the Danish Multiple Myeloma Register from 2005 through 2019 [12]. We excluded patients without an indication for treatment (according to CRAB criteria) and patients who had not started anti-myeloma therapy three months after diagnosis: these patients were defined as having smoldering MM. To calculate R-ISS and R2-ISS, we retrieved information on ISS, LDH levels, and adverse CA by FISH (i.e., t[4;14], t[14;16], del[17p], and amp/gain[1q]). LDH levels above 205 U/L were considered elevated regardless of age and geographical region. CAs were registered as either present or absent despite varying lower detection levels at different laboratories: a cutoff of 10% is recommended for FISH analyses in Denmark. We calculated overall survival (OS) from time of diagnosis until death with censoring at end of follow-up. Patients were grouped according to R-ISS and R2-ISS risk to compare median OS and Harrell’s C-index in order to assess discrimination capabilities. Subgroup analyses of OS stratified on R2-ISS and R-ISS were performed in three populations: (1) patients undergoing high-dose therapy (HDT), (2) younger transplant ineligible patients up to 70 years of age, and (3) transplant ineligible patients older than 70 years.
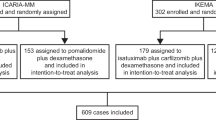
To develop a real-world ISS (RW-ISS), we replicated the methods as published by D’Agostino and colleagues [8]. In brief, we split patients with NDMM into a 75% training set and 25% test set, and performed a multivariable Cox regression analysis for OS on the training set including the variables as used to develop R2-ISS: I.e. age, ECOG PS, ISS, IgA isotype, kidney failure, elevated LDH, del(17p), t(4;14), t(14;16), and amp(1q) [8]. In contrast to R2-ISS, age was dichotomized (≤70 years vs >70 years) and ECOG PS was grouped according to the tertile distribution (0 vs 1 vs >1) (Table 1). Kidney failure was defined as a creatinine level above 2 mg/dL (>177 µM) regardless of age, sex and baseline creatinine [13]. Next, we selected the top 6 features with the highest significant hazard ratios (HR) from the multivariable model to develop RW-ISS. Features with HR above 2 weighted 2 points, HR between 1.5 and 2.0 weighted 1 point, and HR below 1.5 weighted 0.5 points. Cumulative RW-ISS scores were calculated in order to assign patients to RW-ISS I, II, III, and IV based on the quartile distribution of scores in the training set. The test set and the Norwegian external cohort were used to internally and externally validate RW-ISS, respectively. We requested external validation of the RW-ISS from all collaborators within the Nordic Myeloma Study Group, however, only one center could participate and retrieve data on all RW-ISS variables. The data for external validation was thus acquired from The Myeloma Registry of Central Norway (MRCN) including myeloma patients from hospitals in Central Norway [14]. All living patients included in the MRCN have signed an informed consent for the use of their clinical data in medical research. We received an exemption from informed consent for patients, who were dead at the time of inclusion in the MRCN.
The study was approved by the Danish National Ethics Committee (1804410) and Data Protection Agency (P-2020-561). The use of Norwegian data was approved by the Regional Committee for Medical and Health Research Ethics (714399) and the scientific committee of the MRCN. All methods were performed in accordance with the relevant guidelines and regulations.
Results
Among 5492 patients with NDMM, FISH was registered in 2929 patients (53.3%) for whom R2-ISS could be calculated. Baseline characteristics are summarized in Table 1. Adverse CAs were identified in 188 (6.4%) patients with t(4;14), 238 (8.1%) patients with del(17p), and 546 (18.6%) patients with +1q, while t(14;16) was identified in only 77 (2.6%) patients. Overall, adverse CAs included in R2-ISS were detected in 800 (27.3%) patients as compared with 452 (15.4%) for R-ISS related adverse CAs. Single, double, and triple hit adverse cytogenetics was identified in 635 (21.7%), 187 (6.4%), and 17 (0.6%) patients, respectively [15]. R2-ISS was low, low-intermediate, intermediate-high, and high-risk in 397 (13.6%), 830 (26.7%), 1484 (50.7%), and 264 (9.0%) patients, respectively.
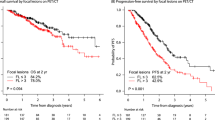
With a median follow-up of 5.2 years (interquartile range [IQR], 3.1–7.8), R2-ISS clearly stratified patients demonstrating a median OS for low, low-intermediate, intermediate-high, and high-risk of 8.4, 6.2, 4.1, and 2.6 years, respectively (Fig. 1A; P < 0.0001; C-index 0.604). We next analyzed OS stratified on R2-ISS in three different subgroups: patients undergoing HDT, younger and older transplant ineligible patients. First, R2-ISS barely stratified OS in 875 patients from time of HDT (Fig. 1B; P = 0.0078), and we were unable to demonstrate a pairwise OS difference between R2-ISS low, low-intermediate, intermediate-high, and high (P ≤ 0.28; pairwise log-rank). Second, among the 2054 patients (70.1%), who could not undergo HDT, 618 (30.1%) patients were younger and 1436 (69.9%) patients were older than 70 years of age. Among these transplant-ineligible patients, R2-ISS could not clearly stratify OS in younger patients (Fig. 1C; P ≤ 0.38; pairwise log-rank), whereas OS in elderly patients stratified well based on R2-ISS (Fig. 1D; P ≤ 0.0042; pairwise log-rank). Furthermore, patients with single, double, and triple hit demonstrated an incremental shorter OS with a hazard ratio of 1.18 (95% confince interval 1.09 to 1.28; P < 0.0001) per additional high risk CA hit.
To compare R2-ISS and R-ISS, we repeated the OS analyses for the same subgroups stratified on R-ISS. R-ISS was I, II and III in 442 (15.1%), 1883 (64.3) and 604 (20.6%) patients, respectively, with a median OS of 8.5, 5.1, and 2.8 years, respectively (supplemental Fig. S1A; P < 0.0001; C-index 0.595). R-ISS clearly stratified all subgroups although C-indices were generally lower as compared with R2-ISS (Fig. 1 and Supplemental Fig. S1).
As R2-ISS could not be fully validated in this Danish real-world population, we noticed that age was not selected as feature in R2-ISS as the multivariate model, from which it was developed, was adjusted for age using 1-year intervals. Further, ECOG PS was presumably markedly lower in the clinical trials populations used to develop R2-ISS as compared to this real-world population (median [IQR]; Not published vs 1 [1;2]) [10].
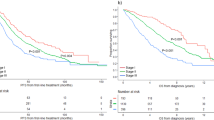
To create a real-world international staging system (RW-ISS), we thus performed multivariable analysis, feature selection and weighted scoring of hazard ratios similar to the methods applied by D’Agostino and colleagues (see Methods) [8]. However, we divided patients into categorical age groups based on a cutoff of 70 years (≤70 vs. >70 years) and ECOG PS into three groups based the tertile distribution (0 vs 1 vs >1; Table 1). We randomly split patients with available R2-ISS (n = 2 929) into a 75% training set and a 25% test set with an even distribution of baseline characteristics (Table 1). Multivariable analysis on the training set demonstrated an independent association with shorter OS for age, ECOG PS, t(14;16), ISS, LDH, del(17p), IgA isotype, renal insufficiens, and sex, whereas t(4;14) and +1q were not significantly associated with shorter OS (Fig. 2). Selecting the top 6 significant features, we assigned 2 points to patients above 70 years and with an ECOG PS > 1 (HR > 2), 1 point to patients with an ECOG PS 1, t(14;16) and ISS III (HR 1.5–1.9), and 0.5 points to patients with ISS II, elevated LDH and del(17p) (Table 2). In the test set, 278 (38.2%), 144 (19.8%), 197 (27.1%), and 109 (15.0%) patients were RW-ISS I (0 to 2 points), II (2.5 to 3 points), II (3.5 to 4.5 points), and IV (5 to 8 points), respectively, and the median OS was 9.5, 5.5, 3.4 and 1.1 years, respectively (Fig. 3A; P < 0.0001; C-index 0.708). In comparison, C-indices for R2-ISS and R-ISS were only 0.604 vs 0.595, respectively (Fig. 1A and supplemental Fig. S1A). These results were partly validated externally in Norwegian data (Fig. 3B) as the NDMM patients with RW-ISS stage II (n = 28) seemed to fare worse as compared to those with stage III (n = 25; P = 0.37; pairwise log-rank). A full validation could be demonstrated when combining RW-ISS stage II and III (Supplemental Fig. S2; P = 0.0004; C-index = 0.679).
Discussion
To our knowledge, this is the first validation of the R2-ISS in a population-based, nationwide cohort of patients with NDMM. However, R2-ISS could only be fully validated in elderly transplant ineligible patients as stratification according to R2-ISS in younger patients was unclear - regardless of transplant eligibility. As a result, we here developed the real-world ISS (RW-ISS) based on selection of high-risk features from a multivariable model (age, ECOG PS, t[14;16], ISS, high LDH and del[17p]). We further demonstrate stratification and discriminatory capabibilities in a test set and in part externally validate RW-ISS in an independent real-world population.
Overall, we demonstrated that the R2-ISS had superior discriminatory capabilities benchmarked against R-ISS. Similar to the findings by D’Agostino and colleagues [8], R2-ISS primarily refined the prognosis for the nearly two-thirds of patients previously classified as R-ISS II, while the prognosis for patients with R-ISS I and III was largely similar to those with R2-ISS low and high risk, respectively. Although a more even distribution of patients according to R2-ISS may be an advantage in a clinical trial setting, where statistical analyses become better balanced, we are concerned that R2-ISS could not clearly stratify younger patients whether transplant eligible or ineligble in a real world setting. Another limitation of the R2-ISS is the scoring system, which is certainly feasible to handle, but more laborious as compared to calculating R-ISS. Because R2-ISS was only partly validated and without clear implications of R2-ISS for the clinical management of patients, we believe that R2-ISS may only be considered in elderly patients and in clinical trials as validated by others [16]. As R-ISS on the other hand clearly stratified all subgroups, we will thus continue to recommend the use of R-ISS for routine clinical management of patients with NDMM outside clinical trials.
In this study, we used a smaller yet large real-world cohort (5492 vs 10843 patients, respectively) with a higher proportion of evaluable patients with complete FISH data (2929 [53.3%] vs 3440 [31.7%], respectively) as compared to the original study published by D’Agostino and colleagues [8]. Replicating the methods applied in their original study [8], we here selected the top 6 features with the highest hazard ratios from the multivariable model to develop RW-ISS: Age >70 years (2 points), ECOG PS 1 and >1 (1 point and 2 points), ISS II and III (1 point and 2 points), t(14;16) (1 point), high LDH (0.5 points), and del(17p) (0.5 points) were used to calculate RW-ISS score and assign patients to RW-ISS I (0–2 points), II (2.5–3 points), III (3.5–4.5 points), and IV (5–8 points). In this study, t(14;16) was indeed rare and identified in only 2.6% of patients, while +1q was the most common CA identified in 18.6% of patients; information on the number of 1q aberrations was not available in Danish data. Further, t(14;16) was a strong prognostic marker of OS [8], whereas +1q was not at all prognostic of OS in our statistically well-powered multivariable analysis. While only one large study has not been able to confirm the prognostic value of t(14;16) [2], others have demonstrated longer OS for patients with sole t(14;16) as compared with additional cytogenetic aberration and a high occurrence of renal failure at time of diagnosis in pure t(14;16) populations [4, 5]. Thus, the argument for R2-ISS to replace a rare biomarker for a common one seems invalid in the setting of real-world populations. To overcome this obstacle, future studies considering single, double and triple hit MM are warranted [13]. It is important to stress that neither RW-ISS nor R2-ISS evaluated multi-hit high risk cytogenetics. Considering the missing effect of +1q in our population-based cohort, R2-ISS seems to favor addition of FISH analyses over obvious confounders such as age and comorbidity. Although D’Agostino and colleagues adjusted for age and sex, using age as continuous variable, it seems that age was deliberately excluded as only features with the highest hazard ratios were selected for R2-ISS. Even so, age is prognostic of OS in almost every aspect of general medicine, and most international prognostic indices in lymphoid cancers include age [17,18,19,20,21,22]. The rationale for using age as a part of the prognostication is further confirmed by results from the Myeloma XI cohort demonstrating that the relative contribution of molecular risk to survival varied by age group, with a larger effect on OS in the younger patients [23]. Further, rather than depending on randomization, the selection of patients for duplet, triplet or quadruplet therapy outside clinical trials largely relies on myeloma frailty [24, 25]. The simplest model of myeloma frailty is probably the Mayo Clinic frailty score which includes dichotomized age, ECOG PS and high N-terminal natriuretic peptide type B (NT-ProBNP) underscoring the importance of age, fitness and cardiac comorbidity [26, 27]. Here, we demonstrate that age (≤70 vs >70 years) and ECOG PS (0 vs 1 vs >1) were better prognosticactors of OS in NDMM as compared to any other factor included in the R-ISS and R2-ISS (Fig. 2), probably reflecting that elderly, frail patients are likely to receive limited therapy in the real-world setting. As the sole purpose of prognostic tools in NDMM is to inform on prognosis (rather than treatment selection), we firmly believe that it is reasonable to include both age and ECOG PS in RW-ISS. This still leaves room for frailty scores such as the international myeloma working group (IMWG) frailty score including activities of daily living (ADL) and Charlson comorbidity index (CCI) to help evaluating the expected tolerable therapy intensity [24, 27]. We further notice a fairly even distribution of patients in the test set with RW-ISS I (38.2%), II (19.8%), III (27.1%) and IV (15.0%), which may be argued as an advantage when comparing suvival differences in smaller cohorts [8]. Lastly, we externally validated the RW-ISS in part from Norwegian real-world data. We believe that the small external cohort likely explains why R2-ISS was only partly validated.
Limitations to this study include dichotomization of age, which likely holds more prognostic value in smaller age intervals as exemplified in diffuse large B-cell lymphoma [28]. Further, FISH data were retrieved from a large nationwide register rather than from laboratories directly. Thus, in some cases, amp(1q) may in fact represent gain(1q) rather than multiple 1q copies, which to some extent may explain the absent effect on OS of this cytogenetic aberration. We also recognize that the six variables used in RW-ISS may limit its daily practical use. However, we underscore that both age and PS are freely available for practicing hematologists in all countries, while deployment of electronic clinical support tools with automated calculations may overcome this obstacle [29]. Lastly, we underscore that we were only able to retrieve a validation cohort with available baseline variables from a single center, despite requesting such data from collaborators in all Nordic countries. The small number of patients in the external validation cohort may likely explain that RW-ISS could only be externally validated in part. The RW-ISS thus needs further external validation in larger real-world cohorts.
In conclusion, RW-ISS may refine the prognosis in real-world, routine clinical care of patient with NDMM, which in addition to R-ISS risk factors also considers clinical factors age and performance status. RW-ISS may be calulcated online (https://rwiss.shinyapps.io/RWISS/). Although R2-ISS could be validated in Danish real-world data, we believe that R2-ISS should be reserved for patients enrolled in clinical trials.
Data availability
According to Danish legislation, register data may not be shared publicly. Data may be shared on a collaborative basis within the DALY-CARE data resource based on data processing agreement [30]. Danish quality register data may also be accessed by request. Statistical analyses were performed in R software. The base code is available at github.
Code availability
According to Danish legislation, register data may not be shared publicly. Data may be shared on a collaborative basis within the DALY-CARE data resource based on data processing agreement [30]. Danish quality register data may also be accessed by request. Statistical analyses were performed in R software. The base code is available at github.
References
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, et al. Revised international staging system for multiple myeloma: a report from international myeloma working group. J Clin Oncol. 2015;33:2863–9.
Avet-Loiseau H, Malard F, Campion L, Magrangeas F, Sebban C, Lioure B, et al. Translocation t(14;16) and multiple myeloma: is it really an independent prognostic factor? Blood. 2011;117:2009–11.
Schavgoulidze A, Perrot A, Cazaubiel T, Leleu X, Montes L, Jacquet C, et al. Prognostic impact of translocation t(14;16) in multiple myeloma according to the presence of additional genetic lesions. Blood Cancer J. 2023;13:160.
Mina R, Joseph NS, Gay F, Kastritis E, Petrucci MT, Kaufman JL, et al. Clinical features and survival of multiple myeloma patients harboring t(14;16) in the era of novel agents. Blood Cancer J. 2020;10:40.
Goldman-Mazur S, Jurczyszyn A, Castillo JJ, Waszczuk-Gajda A, Grząśko N, Radocha J, et al. A multicenter retrospective study of 223 patients with t(14;16) in multiple myeloma. Am J Hematol. 2020;95:503–9.
Radocha J, Maisnar V, Pour L, Špička I, Minařík J, Szeligová L, et al. Validation of multiple myeloma risk stratification indices in routine clinical practice: analysis of data from the Czech Myeloma Group Registry of Monoclonal Gammopathies. Cancer Med. 2018;7:4132–45.
Kastritis E, Terpos E, Roussou M, Gavriatopoulou M, Migkou M, Eleutherakis-Papaiakovou E, et al. Evaluation of the revised international staging system in an independent cohort of unselected patients with multiple myeloma. Haematologica. 2017;102:593–9.
D’Agostino M, Cairns DA, Lahuerta JJ, Wester R, Bertsch U, Waage A, et al. Second Revision of the International Staging System (R2-ISS) for overall survival in multiple myeloma: a European Myeloma Network (EMN) Report Within the HARMONY Project. J Clin Oncol. 2022;40:3406–18.
Blimark CH, Vangsted AJ, Klausen TW, Gregersen H, Szabo AG, Hermansen E, et al. Outcome data from >10 000 multiple myeloma patients in the Danish and Swedish national registries. Eur J Haematol. 2022;108:99–108.
Klausen TW, Gregersen H, Abildgaard N, Andersen NF, Frolund UC, Gimsing P, et al. The majority of newly diagnosed myeloma patients do not fulfill the inclusion criteria in clinical phase III trials. Leukemia. 2019;33:546–9.
Schmidt TM, Fonseca R, Usmani SZ. Chromosome 1q21 abnormalities in multiple myeloma. Blood Cancer J. 2021;11:83.
Gimsing P, Holmstrom MO, Klausen TW, Andersen NF, Gregersen H, Pedersen RS, et al. The Danish National Multiple Myeloma Registry. Clin Epidemiol. 2016;8:583–7.
Rajkumar SV. Multiple myeloma: 2024 update on diagnosis, risk-stratification, and management. Am J Hematol. 2024;99:1802–24.
Laugesen K, Ludvigsson JF, Schmidt M, Gissler M, Valdimarsdottir UA, Lunde A, et al. Nordic health registry-based research: a review of health care systems and key registries. Clin Epidemiol. 2021;13:533–54.
Panopoulou A, Easdale S, Ethell M, Nicholson E, Potter M, Giotas A, et al. Impact of ultra high-risk genetics on real-world outcomes of transplant-eligible multiple myeloma patients. Hemasphere. 2023;7:e831.
Richardson PG, Perrot A, Mikhael J, Martin T, Beksac M, Spicka I, et al. Allocation and validation of the second revision of the International Staging System in the ICARIA-MM and IKEMA studies. Blood Cancer J. 2024;14:209.
Bahlo J, Kutsch N, Bauer K, Bergmann MA, Byrd J, Chaffee KG, et al. An international prognostic index for patients with chronic lymphocytic leukaemia (CLL-IPI): a meta-analysis of individual patient data. Lancet Oncol. 2016;17:779–90.
Federico M, Bellei M, Marcheselli L, Luminari S, Lopez-Guillermo A, Vitolo U, et al. Follicular lymphoma international prognostic index 2: a new prognostic index for follicular lymphoma developed by the international follicular lymphoma prognostic factor project. J Clin Oncol. 2009;27:4555–62.
Sehn LH, Berry B, Chhanabhai M, Fitzgerald C, Gill K, Hoskins P, et al. The revised International Prognostic Index (R-IPI) is a better predictor of outcome than the standard IPI for patients with diffuse large B-cell lymphoma treated with R-CHOP. Blood. 2007;109:1857–61.
Hoster E, Dreyling M, Klapper W, Gisselbrecht C, van Hoof A, Kluin-Nelemans HC, et al. A new prognostic index (MIPI) for patients with advanced-stage mantle cell lymphoma. Blood. 2008;111:558–65.
Kastritis E, Morel P, Duhamel A, Gavriatopoulou M, Kyrtsonis MC, Durot E, et al. A revised international prognostic score system for Waldenström’s macroglobulinemia. Leukemia. 2019;33:2654–61.
Hasenclever D, Diehl V. A prognostic score for advanced Hodgkin’s disease. International Prognostic Factors Project on Advanced Hodgkin’s Disease. N. Engl J Med. 1998;339:1506–14.
Pawlyn C, Cairns D, Kaiser M, Striha A, Jones J, Shah V, et al. The relative importance of factors predicting outcome for myeloma patients at different ages: results from 3894 patients in the Myeloma XI trial. Leukemia. 2020;34:604–12.
Cook G, Larocca A, Facon T, Zweegman S, Engelhardt M. Defining the vulnerable patient with myeloma-a frailty position paper of the European Myeloma Network. Leukemia. 2020;34:2285–94.
Larocca A, Dold SM, Zweegman S, Terpos E, Wäsch R, D’Agostino M, et al. Patient-centered practice in elderly myeloma patients: an overview and consensus from the European Myeloma Network (EMN). Leukemia. 2018;32:1697–712.
Milani P, Vincent Rajkumar S, Merlini G, Kumar S, Gertz MA, Palladini G, et al. N-terminal fragment of the type-B natriuretic peptide (NT-proBNP) contributes to a simple new frailty score in patients with newly diagnosed multiple myeloma. Am J Hematol. 2016;91:1129–34.
Mian H, Brouwers M, Kouroukis CT, Wildes TM. Comparison of frailty scores in newly diagnosed patients with multiple myeloma: a review. J Frailty Aging. 2019;8:215–21.
Jelicic J, Juul-Jensen K, Bukumiric Z, Roost Clausen M, Ludvigsen Al-Mashhadi A, Pedersen RS, et al. Prognostic indices in diffuse large B-cell lymphoma: a population-based comparison and validation study of multiple models. Blood Cancer J. 2023;13:157.
Agius R, Riis-Jensen AC, Wimmer B, da Cunha-Bang C, Murray DD, Poulsen CB, et al. Deployment and validation of the CLL treatment infection model adjoined to an EHR system. NPJ Digit Med. 2024;7:147.
Brieghel C, Werling M, Frederiksen CM, Parviz M, Lacoppidan T, Faitova T, et al. The Danish Lymphoid Cancer Research (DALY-CARE) Data Resource: the basis for developing data-driven hematology. Clin Epidemiol. 2025;17:131–45.
Author information
Authors and Affiliations
Contributions
CB conceived the study and analyzed the data. CUN gathered the Danish data. TSS gathered the Norwegian data. CB and ST wrote the draft manuscript. CB, TSS, NMA, AGS, CUN and ST interpreted the data. All authors made significant contributions to the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
CB received travel grants from AbbVie outside this study. TSS has received honoraria from Takeda, Celgene, Amgen, Janssen, AbbVie, Pfizer; Consultancy for Bristol Myers Squibb, GSK, Pfizer, Menarini Group, and advisory board consultancy from Sanofi, Bristol Myers Squibb, Sanofi, Amgen, Celgene, GSK, and Janssen outside this study. CUN received research funding and/or consultancy fees from AstraZeneca, Janssen, AbbVie, Beigene, Genmab, CSL Behring, Octapharma, Takeda, Eli Lily, MSD, and Novo Nordisk Foundation. ST has received honoraria for scientific talks from AbbVie and Thermo Fisher Scientific. All other authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Brieghel, C., Slørdahl, T.S., Andersen, M.N. et al. A Real-World International Staging System (RW-ISS) for patients with newly diagnosed multiple myeloma. Blood Cancer J. 15, 59 (2025). https://doi.org/10.1038/s41408-025-01268-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41408-025-01268-y