Abstract
Fluorescence in situ hybridization (FISH) remains the gold-standard clinical assay to detect genetic abnormalities in multiple myeloma (MM). However, FISH panel design, use of conventional chromosome banding analysis and reporting practices have been reported to vary among laboratories. Therefore, standardization in FISH testing and reporting practices is needed to improve report clarity and avoid misinterpretation. The recommendations in this paper represent a consensus of our Cancer Genomics Consortium Plasma Cell Neoplasm Working Group, comprising a joint panel of cytogenetic laboratory directors and clinical investigators with expertise in the diagnosis, risk stratification, and treatment of multiple myeloma. Prior to developing these consensus recommendations, we performed a full literature review and conducted a survey of 102 oncologists to assess current variations and challenges in MM cytogenetic/FISH testing and reporting. Our guidelines establish best practices for the optimization of FISH panel selection, and recommendations for standardized reporting of cytogenetic results to align with the 2025 International Myeloma Society (IMS)/International Myeloma Working Group (IMWG) Updated Risk Stratification.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a plasma cell (PC) neoplasm representing ~10% of all blood-related cancers [1]. Nearly all cases of MM can be characterized by either recurrent immunoglobulin rearrangements (IGH-r) and/or hyperdiploidy defined by gains of odd-numbered chromosomes (trisomies) [1]. Approximately 40% of MM can be defined by five generally mutually exclusive IGH-r including t(4;14)(p16;q32), t(14;16)(q32;q23), t(14;20)(q32;q12), t(11;14)(q13;q32) and t(6;14)(p21.1;q32). Approximately 50% can be characterized by hyperdiploidy with or without a primary IGH-r [2,3,4]. These recurring acquired cytogenetic abnormalities within the PC clone represent known biomarkers of disease prognosis and response to therapy [3]. Given the prognostic and therapeutic value, these cytogenetic data have been incorporated into risk stratification guidelines including 1) the International Myeloma Society/International Myeloma Working Group (IMWG) [5]; 2) the National Comprehensive Cancer Network (NCCN) [6]; and 3) the Mayo Stratification for Myeloma and Risk-Adapted Therapy (mSMART) [7]. All guidelines consider deletion and/or mutation of TP53 as a high-risk cytogenetic entity [8, 9]. Most guidelines now consider either t(4;14), t(14;16) and t(14;20) in combination with gains or amplifications of 1q21 or deletions of 1p32 as high-risk. All other abnormalities such as hyperdiploidy, t(11;14) or t(6;14) when occurring without a TP53 deletion or mutation or biallelic 1p32 deletion are considered standard risk.
Risk-defining cytogenetic abnormalities are currently detected using fluorescence in situ hybridization (FISH). Although these abnormalities can also be identified by conventional chromosome banding analysis, chromosomal microarray analysis (CMA) or next-generation sequencing (NGS), FISH remains the current gold-standard clinical assay in the genetic evaluation of MM. However, MM clinical workup is heterogeneous among numerous clinical laboratories worldwide, often with variations in FISH panel design, PC enrichment methodologies, use of conventional chromosome banding analysis and reporting practices [10, 11]. This lack of standardization has resulted in confusion and may increase the probability of incorrect integration of cytogenetic results in risk stratification [12]. To improve the standardization of cytogenetic testing in MM, we formed the Cancer Genomics Consortium (CGC) Plasma Cell Neoplasm Working Group composed of board-certified cytogenetic laboratory directors from a variety of clinical laboratory settings from the United States and Canada to propose clear solutions to improve standardization and establish best MM FISH panel design and reporting practices aimed to improve the care of patients with MM.
Cancer Genomics Consortium Plasma Cell Neoplasm Working Group
The CGC Plasma Cell Neoplasm Working Group was formed by a professional group of 12 clinical cytogenetic laboratory directors from the CGC, an organization formed in 2009 with the goal of promoting best practices in clinical laboratory cancer genomics. The workgroup members represent small to medium academic laboratories and large reference commercial laboratories within the United States and Canada. The workgroup convened monthly for 1-hour via teleconference for 1.5 years. We also included three clinical MM oncologists from Mayo Clinic (SK and RF) and U of Washington (RB). We collected peer-reviewed literature of large case series or clinical trials concentrating on the clinical significance of cytogenetic abnormalities in MM. We searched the National Institute of Health National Library of Medicine’s “PubMed” database for studies in humans published in English between 2013 to 2024 with an emphasis on publications focusing on cytogenetics within the last 5 years. The role of each abnormality in diagnosis, prognosis, and therapy, and methods for detection was discussed. The primary literature was also evaluated to identify best practices for the cytogenetic evaluation of MM including the value of conventional chromosome banding analysis, optimization of FISH panel selection, and standardization of clinical reporting of cytogenetic results. Articles which focused on pre-malignant conditions such as monoclonal gammopathy of undetermined significance or smoldering MM were excluded as the clinical significance of different abnormalities in these contexts may vary from MM. To identify the status and aid the development of our recommendations, we conducted a survey interrogating numerous aspects of clinical MM FISH testing and reporting. We also ensured that our recommendations for testing and reporting are fully aligned with the 2025 IMS/IMWG Updated Risk Stratification [5].
Consensus recommendations for standard FISH panel design and testing algorithm
Newly diagnosed MM (NDMM) are often characterized by two major primary genomic events including IGH rearrangement at chromosomal level (IGH-r) which accounts for ~40% of NDMM cases [3, 13] and hyperdiploidy, which is often defined as gain of at least two or more odd-numbered chromosomes including chromosomes 3, 5, 7, 9, 11, 15, 19 and 21, and accounts for ~50% of the NDMM cases [14,15,16].
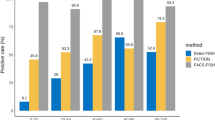
Our recommendations are based on a literature review of data from existing original research papers as well as current risk-stratification guidelines (Fig. 1) to ensure that we have evidence to support the clinical significance of each recommended FISH probe. We propose two standard FISH panels, an initial diagnostic panel, and a relapsed MM panel (Fig. 2). For all newly diagnosed MM (NDMM), a minimal evaluation for the following primary IGH-r, is recommended: t(4;14), t(14;16), t(14;20), t(11;14) if an IGH-r has been detected in the initial screen. Detection of an IGH-r occurs when the IGH break-apart (BAP) FISH probe is abnormal. Both the diagnostic and relapsed MM panels should include evaluation for the following abnormalities: 17p deletion including the TP53 gene, 1p deletion and 1q gain or amplification.
FISH panels incorporated into the major risk stratification guidelines (NCCN, IMWG and mSMART). * While not on the recommended diagnostic minimal panel, the NCCN lists MYC-r as a factor considered high-risk for progression/relapse. ** Hyperdiploidy defined by multiple trisomies can be detected by FISH or an equivalent method like flow cytometry. *** Consider implementing a reflex strategy. Many laboratories use an IGH BAP probe to determine rearrangement status. If an IGH BAP signal pattern is detected, laboratories will perform a reflex panel including pertinent IGH partners. However, rare IGH translocations may occur resulting in a “false-negative” using IGH BA; therefore, the decision to perform sequential testing is at the discretion of the individual laboratory. If a TP53 deletion is identified, reflex to evaluate for TP53 mutation can be considered, but is not required.
Consensus recommendation for minimum FISH panel design includes detection of TP53 deletion using a probe targeting 17p13, 1q gain or amplification using a probe targeting 1q21 (typically CKS1B), 1p deletion using a probe tageting 1p32 (typically CDKN2C) and IGH-r for all NDMM. * If an IGH-r is identified, reflex to DC-DF probes targeting t(4;14), t(14;16), t(14;20) and t(11;14) should be performed. Detection of an IGH-r occurs when the IGH break-apart (BAP) FISH probe is abnormal. For RRMM, a minimal FISH panel that includes assessment for TP53 deletion, 1p deletion, 1q gain or amplification, and at least one probe targeting the primary abnormality observed at diagnosis is recommended. Inclusion of a previous primary abnormality serves as a positive control for detection of the patient’s previously described MM clone.
Translocation t(4;14) is present in ~15% of NDMM and results in overexpression of FGFR3 and/or NSD2 [17]. The t(14;16) is present in 3–5% of NDMM and leads to increased expression of MAF [18] while the t(14;20) is present in 1–2% of NDMM and leads to increased expression of MAFB [3, 19]. These subtypes are often associated with other high-risk secondary abnormalities [18, 20], a high mutation burden and hyper-APOBEC activity characterized by single base substitution (SBS2 and SBS13) signatures [21,22,23,24]. The t(11;14) involves IGH and CCND1 resulting in increased CCND1 expression, is present in 15–20% of NDMM and in 50% primary plasma cell leukemia, representing the most common primary IGH-r in MM [25, 26]. Patients with t(11;14) have been reported to be more sensitive to BCL2 inhibition [27,28,29].
Detection of each of these IGH-r can be achieved using specific dual-color, dual-fusion (DC-DF) probes. Laboratories often use an IGH break-apart (BAP) probe as an initial screen. If abnormal, including deletions of either 5’ or 3’ IGH, the laboratory typically performs reflex testing with t(4;14), t(14;16), t(14;20) and t(11;14) DC-DF probes (Fig. 2) in a labor and cost-conscious approach enabling the judicious use of limited enriched PC samples. The approach is supported by evidence indicating that nearly all recurrent IGH-r result in an abnormal IGH BAP result [30] and primary IGH-r are generally mutually exclusive [3, 13]. Of those cases with an abnormal IGH BAP result, approximately 80% have a recurrent IGH-r, while the remaining 20% have an IGH rearrangement not involving CCND1, CCND3, FGFR3, MAF, MAFB or have deletions of either 5’ or 3’ IGH [3]. While the specific reflex design or ordering may vary between cytogenetic laboratories, all laboratories must have a system to identify all recurrent IGH-r.
Deletion of TP53, located at 17p, is present in 7–10% of NDMM [31] and up to 80% of patients with relapsed and/or refractory multiple myeloma (RRMM) and in secondary plasma cell leukemia, [32]. TP53 biallelic inactivation can be observed as a biallelic deletion, or a heterozygous deletion with concurrent mutations detected by sequencing, sometimes resulting in aberrant splicing [33, 34]. TP53 deletion can be detected by FISH using enumeration and locus-specific probes targeting the centromere of chromosome 17 and 17p (TP53).
Chromosome 1 abnormalities and their associated clinical implications in MM have been historically difficult to define due to the use of different FISH probe targets and variability in reporting of copy states of chromosome 1. Deletion of 1p is present in 8–12% of NDMM [35,36,37] and the most significant region of interest is reported to be 1p32.3 (CDKN2C, FAF1) [11, 38, 39]. 1p deletion can be detected using FISH probes targeting CDKN2C. Gain or amplification of 1q is present in 30–45% of NDMM [37, 40] and in 55–70% of MM patients at relapse [37, 40]. Gain of 1q is defined as 3 total copies of 1q and amplification is defined as 4 or more total copies of 1q (relative to a diploid genome). Standardization of reporting practices of 1q have been particularly challenging in the cytogenetics community [12]. Although gain/amplification of 1q is typically extensive and involves multiple genes in large regions of chromosome 1 [11, 38, 39, 41], it is typically detected using FISH probes targeting CKS1B. Probes targeting 1p and 1q are often combined.
For RRMM, a minimal FISH panel that includes assessment for TP53 deletion, 1p deletion, 1q gain or amplification, and at least one probe targeting the primary abnormality observed at diagnosis is recommended (Fig. 2). Including a previously abnormal probe allows for confirmation that abnormal PCs have been identified minimizing the risk of a “false-negative” FISH study. Prioritization of FISH probes associated with high-risk disease, such as TP53, t(4;14) and 1p/1q can be performed in cases with limited PCs. Following treatment, FISH testing is not recommended to evaluate for minimum residual disease. In cases where the initial FISH test at diagnosis was incomplete or insufficient, a comprehensive diagnostic panel may be warranted.
Optional FISH probes for multiple myeloma
For all NDMM, additional probes to evaluate for ploidy including hyperdiploidy or hyperhaploidy, t(6;14), MYC-r, or 13q deletion may be considered. Hyperdiploidy is found in approximately 50% of NDMM and is typically associated with 47–57 chromosome count [14,15,16]. As the classic definition of hyperdiploidy was derived from a genome-wide chromosome perspective, the identification of hyperdiploidy is challenging when using a limited FISH panel. However, many clinical studies have evaluated the prognostic significance of FISH-based hyperdiploidy considering ≥2 odd-numbered chromosomes 3, 5, 7, 9, 11, 15, 19 and 21 [42]. If ploidy assessment is desired, FISH targeting odd-numbered chromosomes using tricolor probe sets of chromosomes can be utilized. Enumeration of chromosome 15 may have reduced sensitivity in association with African ancestry [43]. Flow cytometry [44] or CMA can also be used to assess hyperdiploidy.
Hyperhaploidy is an infrequent subtype associated with a genome wide loss of numerous chromosomes typically with a 24–34 chromosome count. The disomic chromosomes retained in hyperhaploidy are the same odd-numbered chromosomes found in hyperdiploidy. IGH-r are infrequently observed, but mutations of TP53 are common and often biallelic [45, 46]. Although hyperhaploidy is not a specific entity in risk stratification guidelines, TP53 deletion and mutation status is included. Use of probes targeting t(4;14), t(14;16), and TP53 allows detection of loss of chromosomes 4, 14, 16, and 17 enabling identification of potential hyperhaploidy.
Another rare IGH-r that can be considered for evaluation includes the t(6;14), present in 1–2% of NDMM leading to increased expression of CCND3 [3, 21, 47]. Using gene expression analysis, the profile of PCs with t(6;14) is similar to t(11;14) [48,49,50]. Both t(6;14) and t(11;14) can be represented by 2–3 distinct expression groups (termed CD-1, CD-2a and CD2b) with CD-1 having increased expression of KLHL4 and INHBE and CD-2 having increased expression of CD20, VPREB and PAX-5) [48,49,50]. Similar to t(11;14), patients with t(6;14) may also be sensitive to BCL2 inhibition [51]. The t(6;14), detected using DC-DF FISH probes for IGH and CCND3, can be considered reflex IGH testing.
Secondary rearrangements involving MYC (located at 8q24.21) are associated with increased MYC expression, and are present in 30–45% of NDMM and 50% of RRMM when detected by genomic sequencing [52,53,54]. MYC-r have been associated with progression of MM [55, 56], can be complex and involve numerous genomic mechanisms and partner genes [57]. MYC-r have not yet been incorporated into many risk guidelines but are discussed in the current 2024 NCCN guidelines [6]. Detection of MYC-r can be achieved using a MYC BAP or specific DC-DF probe sets, although only about half of MYC-r can be identified by FISH [53, 58].
Deletion of 13q or monosomy 13 is present in approximately half of NDMM [38, 59,60,61,62] and is frequently associated with other MM subtypes t(4;14) and deletion of TP53 [60, 62,63,64]. The prognostic significance of del(13q) has been debated and may be a surrogate marker or a weak contributor to disease risk. Thus, del(13q) is not currently included in most risk stratification guidelines. Del(13q) is most often detected by FISH using probe sets targeting the RB1 locus at 13q14.2 or DLEU1/MIR15A/MIR16-1 (D13S319 or D13S25) at 13q14.2q14.3, with a control locus in distal 13q34, allowing differentiation of interstitial deletions from presumed monosomies [11].
Interpretation of abnormal FISH results
The most common FISH patterns are indicated in Supplementary Table 1. Hyperdiploidy is suggested when ≥2 odd-numbered chromosomes are identified, however identification of hyperdiploidy can be a challenge to precisely define with limited FISH panels. Distinguishing between hyperdiploidy or near-tetraploidy may not be possible. Tetraploidy or near-tetraploidy, which typically refers to the doubling or endoreduplication of a diploid genome, can be found between 5–10% of MM cases, an estimate dependent on the method of ascertainment. Near-tetraploidy can be present as a secondary clone, sometimes at low level [65, 66]. Overall, ascertainment of the ploidy status of a clone by FISH presents a challenge.
Caution should be taken when interpreting gains and amplifications of 1q and deletion of TP53 in the context of a tetraploid/near-tetraploid genome. When 2 copies of TP53 are observed in the context of a tetraploid (four copy) genomic state, interpretation of a deletion of 17p may be appropriate if there is evidence of a diploid clone with a TP53 deletion. However, in the context of limited ploidy assessment, minimization of the term “relative deletion” is advised and inclusion of a statement indicating that it is unclear if TP53 function is impacted could be helpful to underscore the uncertainty of the finding. Correlating with TP53 mutation status is recommended. Similarly, when 6 copies of 1q are observed in the context of a near-tetraploid genomic state, interpretation of a relative gain of 1q (not amplification) may be appropriate if there is evidence of a diploid clone with a 1q gain.
Our survey showed that clarity of FISH testing and interpretation is needed (Supplementary Results and Supplementary Fig. 1A–E). Only 60–65% of respondents were satisfied with the clarity, summary, and interpretation, respectively, of the FISH reports they currently receive (Supplementary Table 2). When clinicians were challenged with a difficult-to-interpret FISH result (Supplementary Material-Survey question 11) where an IGH-r with an unknown partner was listed as “atypical positive” for all listed FISH probes, 22% interpreted the report correctly with the remaining unsure of the interpretation (25%) or misinterpreted the report (53%) demonstrating a need for improved FISH report clarity.
Consensus recommendations for reporting FISH results for risk stratification of myeloma
In addition to the general FISH result reporting recommendations from the American College of Medical Genetics and Genomics (ACMG) Technical Standards for Clinical Genetics Laboratories (2021 revision) and in the College of American Pathologists (CAP) Cytogenetics Checklist we suggest the inclusion of the following additional elements.
-
Highlighting critical results. This may include a concise summary sentence at the top of the report in bold. For example, “Gain of 1q (CKS1B) detected”, “Deletion of TP53 detected”, “t(11;14)/IGH::CCND1 rearrangement detected”, “t(14;20)/IGH::MAFB rearrangement not detected”.
-
Table of results. A table of results can be included to document FISH probes being tested, the laboratory’s established cut-off value for each probe and the abnormality being detected or not detected. However, we urge caution regarding the interpretation of the percent positivity particularly regarding secondary abnormalities, as this percentage will depend on the PC burden and enrichment. Historic results can also be included for comparison for specific abnormal signal patterns in follow-up studies.
-
The use of plain language. Some may recognize cytogenetic abnormalities by the chromosomal aberrations while others may recognize them by their gene names. It is recommended to include both gene names and the associated chromosomal aberration in the report. For example, “t(11;14)/IGH::CCND1 rearrangement detected”.
-
The use of standardized language. The use of standardized language beyond the use of the international system for human cytogenomic nomenclature (ISCN) is critically important to improve clarity of result. We further recommend:
-
○
Use of “rearrangement” to describe for example, a t(11;14)/IGH::CCND1
-
○
Use of “gain” to describe an additional copy number signal and “amplification” to describe gain of two or more signals.
-
○
Use of “deletion” to describe a copy number loss (heterozygous or biallelic).
-
○
Avoid the term “atypical abnormal” when a FISH signal pattern displays a technically abnormal result but does not detect an expected abnormality. For example, a gain of an additional IGH signal may be observed in the context of a t(4;14)-r when using the t(11;14) FISH probe set. Rather, “not detected” for t(11;14) and “detected” for t(4;14) is suggested to avoid confusion.
-
○
Clearly defined methods. It is important to indicate whether PC enrichment was performed with the following comment: “Interphase FISH analysis was performed on cultured or uncultured bone marrow cells” or “Interphase FISH analysis was performed on plasma cells enriched from the bone marrow sample”.
-
○
Clear language that interprets the FISH results and accurately classifies patients into standard-risk and high-risk based on the 2025 IMS/IMWG Risk Stratification guidelines [5] (Figs. 3–4).
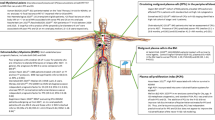
Fig. 3: Cytogenetic risk assessment and reporting for MM according to the 2025 IMS/IMWG risk stratification. Following FISH detection, laboratories should provide a report using clear language that interprets the FISH results with accurate classification into standard-risk and high-risk based on the 2025 IMS/IMWG Risk Stratification guidelines. Cytogenetic high-risk includes the presence of at least one of the following cytogenetic abnormalities: TP53 deletion or TP53 mutation, 1p biallelic deletion, t(4;14) plus 1q gain or amplification or 1p deletion, t(14;16) plus 1q gain or amplification or 1p deletion, t(14;20) plus 1q gain or amplification or 1p deletion, 1q gain or amplification plus 1p deletion. 17p deletion should have clonality of ≥20%. Standard-risk includes the absense of a high-risk cytogenetic abnormality and can include isolated hyperdiploidy, t(11;14) or t(6;14). Other features such as β2 microglobulin and creatinine also impact the overall IMS/IMWG risk stratification-please refer to Avet-Loiseau, et al. [5] for a complete risk stratification incorporating these variables along with the cytogenetics.
Fig. 4: Recommended format and components of sample report to conform to the new 2025 IMS/IMWG Risk Stratification of Myeloma. Sample of a FISH report reflecting the critical results highlighted in bold at the top of the report under “result summary” (example in blue shading). In this case, there is a t(11;14)/IGH::CCND1 rearrangement and hyperdiploidy detected. Also indicated are the results for cytogenetic abnormalities not detected in this sample. An interpretation written in plain and standardized language is provided which indicates that FISH analysis was performed on enriched plasma cells and identifies specifically which abnormalities were detected and not detected (example in purple shading). A comment about whether the FISH findings represent a standard or high-risk abnormality according to the 2025 IMS/IMWG risk stratification is also indicated. A table of results is provided (example in green shading), which indicates the FISH probes being tested, the laboratory’s established cut-off values for each probe and the abnormality being detected or not detected. Finally, additional technical details including previous FISH results if available, the ISCN nomenclature and the methods are also included (example in grey shading).
-
○
A sample report incorporating improvements highlighted above can be found in (Fig. 4). When we enhanced the clarity and improved the result summary and interpretation implementing the recommendations described above, about 80% of the clinicians were now satisfied with the improved reporting format and interpretation (Supplementary Table 3).
Optional inclusion of TP53 mutation testing
The IMS/IMWG Risk Stratification guidelines now recognize TP53 mutation as a high-risk entity [5]. Mutation in TP53 occurs in approximately 6% of NDMM [67]. Notably, TP53 mutations are predominantly associated with TP53 deletions, with studies indicating that about 37% of patients with a TP53 deletion harbor a TP53 mutation while patients without a TP53 deletion were not reported to have a TP53 mutation [68]. Thus, if sample is available, evaluation for TP53 mutation may be considered particularly in cases without a TP53 deletion, but it may not be feasible to perform mutation testing in most laboratories globally. Although bi-allelic TP53 inactivation (double hit) has been recognized as an important driver of prognosis when compared to mono-allelic TP53 inactivation [67], the IMS/IMWG considers TP53 deletion or TP53 mutation as high risk. Thus, testing for TP53 mutation in the context of a TP53 deletion is not currently necessary for the IMS/IMWG risk stratification. If TP53 mutation testing is desired, such testing can be performed by NGS using DNA extracted from a PC-enriched sample using an MM-targeted sequencing panel designed, as described by others [69,70,71,72]. Caution is advised when interpreting TP53 mutation status from NGS performed on non-PC-enriched samples, as admixture with non-MM cells may affect accuracy. Over time, we anticipate these capture-based NGS tests, or even WGS or other technologies, when performed on PC-enriched samples will eventually replace FISH, as discussed by Akkari, et al. [73].
Technical recommendations
Special requirement or consideration for FISH studies for multiple myeloma
PC enrichment
A challenge in performing FISH on PCs is the generally low proportions of PCs in bone marrow aspirates, in comparison to other malignancies such as acute leukemias. Therefore, it is recommended that all samples undergo PC enrichment to minimize the potential for “false-negative” test results. Of interest, about 20% of the surveyed MM clinicians were unaware of (12.9%) or did not use (5.9%) PC enrichment by their FISH laboratory (Supplementary Fig. 1F). Enrichment of PCs is typically achieved using several technologies, typically utilizing antibodies that are relatively specific for PCs, i.e. CD138. The majority of laboratories utilize CD138 magnetic beads for enrichment [10], while some laboratories enrich PCs using a combination of antibodies including CD138, CD38, CD319, or CD229 by flow sorting [74,75,76,77,78,79,80]. However, flow cytometry may be less efficient at PC recovery in comparison to magnetic-based enrichment [76, 81]. Enrichment is subject to a variety of factors including sample volume, PC concentration and time to processing (where CD138 and other cell surface markers can be internalized over time) [82]. When possible, 1–2 ml of bone marrow aspirate from the first or second draw should be used. Samples should be processed within 24 h, but no more than 120 h after collection, depending on each laboratory’s validation of sample stability [82]. Sodium heparin and EDTA are acceptable anticoagulants. Bone marrow is preferred for PC enrichment, though peripheral blood can be used in cases of blood involvement such as in plasma cell leukemia. Confirmation of adequate enrichment is necessary to ensure an appreciable increase of PCs during validation [77, 83]. Samples with differing PC levels should be included in the verification process to evaluate the effectiveness of enrichment relative to PC burden [84]. Additionally, multiple samples with known aberrations should be tested with standard MM probes to ensure that the enrichment process did not affect the ability of cells to produce correlative FISH results. Each laboratory must establish its own cutoff value for MM FISH using the ACMG technical standards [85]. The preferred number of enriched PCs assessed by FISH should be 50–100 [75, 86]. If PC enrichment is not possible, FISH on direct bone marrow aspirate or cultured sample when flow supports >10–20% abnormal PCs may be possible.
Bone marrow smear and touch preparation utilization for FISH
Bone marrow smears and touch preparation slides can be utilized for FISH testing, when the aspirate has low cell count with patchy PCs by morphology [87]. Communication with the hematopathologist and evaluation of smears or touch preps should be performed prior to FISH to ensure the presence of adequate abnormal PCs. When FISH is performed, 200 cells should be assessed, but 50–100 cells may be evaluated in cases with low cellularity. We recommend the following disclaimer is included: “The sensitivity of FISH analysis of unstained smears is lower as compared to the analysis of CD138+ enriched plasma cells, and the negative FISH results do not preclude the presence of abnormalities associated with plasma cell neoplasms. If clinically indicated, a repeat FISH study on CD138+ enriched PCs is recommended.” Occasionally, FISH studies can be performed on paraffin-embedded tissue, if appropriate validation studies are in place.
G-banded karyotype studies in multiple myeloma
Except for the cryptic t(4;14), nearly all cytogenetic subtypes of MM can be identified by conventional chromosome banding analysis when there is an abnormally dividing PC clone in cell culture. However, due to the low-proliferative nature of PCs, only about 20% of karyotypes in MM are abnormal, even following IL-4 stimulation [88, 89]. Therefore, some laboratories do not perform conventional chromosome banding analysis, instead assessing proliferative capacity with S-phase by flow cytometry [90]. ACMG guidelines continue to recommend karyotyping [84, 90], since a complex karyotype ( ≥ 3 clonal abnormalities) indicates poor risk [4, 91] and often reflects high PC proliferation associated with an aggressive PC clone [2, 4, 90]. The IL-4 stimulated cell pellet can be used for FISH if needed. Conventional chromosome banding analysis in unstimulated cultures may detect concurrent therapy-related myeloid neoplasms, particularly when a monosomy 5 or monosomy 7 (or del(5q) or del(7q)) is identified [89]. The addition of myelodysplastic syndrome (MDS) FISH panels could also be considered in scenarios of cytopenias unexplained by MM or in the context of transplant or T-cell redirecting therapy. The value of conventional chromosome banding analysis was further reflected in the MM clinician survey where conventional chromosome banding analysis was always utilized by 59.8% of clinicians, never utilized in 17.6% and utilized depending on the clinical context (concern for MDS) in 22.5% of clinicians (Supplementary Fig. 1G). We recommend laboratories validate a workflow which prioritizes PC enrichment for FISH. If needed, the remaining sample can be used for conventional chromosome banding analysis after 24 hr and/or 72 hr stimulated culture. Correlation of conventional chromosome banding analysis and FISH results is recommended.
Summary
FISH testing on enriched PCs has long been recognized as the standard-of-care assay to detect recurrent cytogenetic aberrations that can be used to incorporate into risk stratification algorithms. Here, we summarize the clinical value of recurrent chromosomal abnormalities, recommend optimal MM FISH panel design, analysis, interpretation, and clear reporting practices with the goal to provide solutions that can be implemented by other laboratories to improve the quality of their MM FISH testing practices.
We recommend close communication with the clinical management team including MM oncologists/providers, cytogeneticists, molecular geneticists and pathologists to ensure maximal diagnostic benefit. We observed increased utilization of in-house FISH testing among providers within the academic setting in comparison to the community setting. This suggests additional challenges may exist among the community providers, who are more likely to utilize reference laboratories, for their FISH testing. Ease and frequency of communication with the cytogeneticist at the reference laboratory may differ in comparison to in-house cytogenetics laboratories. Reduced access to the reference laboratory may be reflected by the increased frequency of providers who reported a lack of knowledge of PC enrichment practices among their reference laboratory services. Further, the impact of increased transit times of the PC specimen when evaluated by the reference laboratory is unknown. A direct comparison of PC FISH failure rates between reference and in-house FISH laboratory could be of value.
MM FISH interpretations remain a challenge even among the cytogeneticists within the workgroup. Identification of hyperdiploidy or even overall ploidy status in the context of small FISH panels and whether optimal quantification of 1q gain should be determined relative to the overall ploidy of the clone or determined based on total copies of 1q independent of clonal ploidy status can be a challenge. Implementation of MM risk stratification systems based on FISH data is imperfect as cases can harbor multiple high-risk and standard-risk factors [92]. Studies have shown a synergistic negative impact of high-risk abnormalities including TP53 deletion in combination with other high-risk IGH-r such as in cases with “double hit” high-risk abnormalities [67]. Some evidence suggests that the combination of trisomies may reduce the risk of high-risk abnormalities [88]. Thus, a comprehensive genomic scoring system, ideally genome-wide assessment of cytogenetic aberrations, genomic mutations, and PC proliferation index may improve risk stratification in the future.
A limitation to FISH is the interrogation (albeit on a single-cell level) of only a limited region where FISH probes are applied and, in some instances, low sensitivity to detect copy number abnormalities. CMA has shown clinical utility in detecting recurrent copy number aberrations across the entire genome and to potentially replace FISH testing for 1p and 17p deletions, 1q gain and for the assessment of trisomies, when PC content is >20% PC [10, 93], if not enriched. However, since CMA cannot detect balanced rearrangements and cannot distinguish mixed ploidy populations, this testing modality cannot be used to replace all FISH testing. CMA-based copy number detection is often less sensitive for copy number detection than FISH and in addition having adequate specimen to perform all this testing is often challenging. NGS could be implemented to detect all recurrent genetic abnormalities in MM, which may replace FISH in the future [73]. While still within the research domain, a combination of genome sequencing-based testing for the identification of recurrent rearrangements and gene expression of enriched PC using RNA-sequencing may be performed in the future clinically [94, 95]. A limitation of this study is the relatively small sample size of the survey respondents primarily representing a North American perspective, which may impact the generalizability of the findings globally. Overall, FISH remains a vital standard-of-care assay in the evaluation of patients with MM. We propose improvements in FISH testing and reporting with the goal to reduce variability and increase clarity to benefit patient care in MM.
Data availability
Raw survey data are provided in supplemental results.
References
Kumar SK, Rajkumar SV. The multiple myelomas - current concepts in cytogenetic classification and therapy. Nat Rev Clin Oncol. 2018;15:409–21.
Saxe D, Seo EJ, Bergeron MB, Han JY. Recent advances in cytogenetic characterization of multiple myeloma. Int J Lab Hematol. 2019;41:5–14.
Abdallah N, Rajkumar SV, Greipp P, Kapoor P, Gertz MA, Dispenzieri A, et al. Cytogenetic abnormalities in multiple myeloma: association with disease characteristics and treatment response. Blood Cancer J. 2020;10:82.
Rajan AM, Rajkumar SV. Interpretation of cytogenetic results in multiple myeloma for clinical practice. Blood Cancer J. 2015;5:e365.
Avet-Loiseau H, Davies FE, Samur MK, Corre J, D’Agostino M, Kaiser MF, et al. International Myeloma Society/International Myeloma Working Group Consensus Recommendations on the Definition of High-Risk Multiple Myeloma. J Clin Oncol. 2025; In Press. https://healthtree.org/myeloma/community/articles/ims-2024-high-risk-mm-report.
Network NCC. Multiple Myeloma (Version 4.2024). [cited September 11, 2024]. https://www.nccn.org/professionals/physician_gls/pdf/myeloma.pdf.
Dispenzieri A, Rajkumar SV, Gertz MA, Fonseca R, Lacy MQ, Bergsagel PL, et al. Treatment of newly diagnosed multiple myeloma based on Mayo Stratification of Myeloma and Risk-adapted Therapy (mSMART): consensus statement. Mayo Clin Proc. 2007;82:323–41.
Palumbo A, Avet-Loiseau H, Oliva S, Lokhorst HM, Goldschmidt H, Rosinol L, et al. Revised International Staging System for Multiple Myeloma: A Report From International Myeloma Working Group. J Clin Oncol. 2015;33:2863–9.
Mikhael JR, Dingli D, Roy V, Reeder CB, Buadi FK, Hayman SR, et al. Management of newly diagnosed symptomatic multiple myeloma: updated Mayo Stratification of Myeloma and Risk-Adapted Therapy (mSMART) consensus guidelines 2013. Mayo Clin Proc. 2013;88:360–76.
Pugh TJ, Fink JM, Lu X, Mathew S, Murata-Collins J, Willem P, et al. Assessing genome-wide copy number aberrations and copy-neutral loss-of-heterozygosity as best practice: An evidence-based review from the Cancer Genomics Consortium working group for plasma cell disorders. Cancer Genet. 2018;228-229:184–96.
Yu Y, Brown Wade N, Hwang AE, Nooka AK, Fiala MA, Mohrbacher A, et al. Variability in Cytogenetic Testing for Multiple Myeloma: A Comprehensive Analysis From Across the United States. JCO Oncol Pr. 2020;16:e1169–80.
Neupane K, Fortuna GG, Dahal R, Schmidt T, Fonseca R, Chakraborty R, et al. Alterations in chromosome 1q in multiple myeloma randomized clinical trials: a systematic review. Blood Cancer J. 2024;14:20.
Ravindran A, Greipp PT, Wongchaowart N, Smadbeck JB, Peterson JF, Ketterling RP, et al. Dual Primary IGH Translocations in Multiple Myeloma: A Novel Finding. Clin Lymphoma Myeloma Leuk. 2021;21:e710–3.
Smadja NV, Fruchart C, Isnard F, Louvet C, Dutel JL, Cheron N, et al. Chromosomal analysis in multiple myeloma: cytogenetic evidence of two different diseases. Leukemia. 1998;12:960–9.
Debes-Marun CS, Dewald GW, Bryant S, Picken E, Santana-Davila R, Gonzalez-Paz N, et al. Chromosome abnormalities clustering and its implications for pathogenesis and prognosis in myeloma. Leukemia. 2003;17:427–36.
Barila G, Bonaldi L, Grassi A, Martines A, Lico A, Macri N, et al. Identification of the true hyperdiploid multiple myeloma subset by combining conventional karyotyping and FISH analysis. Blood Cancer J. 2020;10:18.
Keats JJ, Reiman T, Belch AR, Pilarski LM. Ten years and counting: so what do we know about t(4;14)(p16;q32) multiple myeloma. Leuk Lymphoma. 2006;47:2289–2300.
Schavgoulidze A, Perrot A, Cazaubiel T, Leleu X, Montes L, Jacquet C, et al. Prognostic impact of translocation t(14;16) in multiple myeloma according to the presence of additional genetic lesions. Blood Cancer J. 2023;13:160.
Ross FM, Chiecchio L, Dagrada G, Protheroe RK, Stockley DM, Harrison CJ, et al. The t(14;20) is a poor prognostic factor in myeloma but is associated with long-term stable disease in monoclonal gammopathies of undetermined significance. Haematologica. 2010;95:1221–5.
Mina R, Joseph NS, Gay F, Kastritis E, Petrucci MT, Kaufman JL, et al. Clinical features and survival of multiple myeloma patients harboring t(14;16) in the era of novel agents. Blood Cancer J. 2020;10:40.
Walker BA, Wardell CP, Murison A, Boyle EM, Begum DB, Dahir NM, et al. APOBEC family mutational signatures are associated with poor prognosis translocations in multiple myeloma. Nat Commun. 2015;6:6997.
Rustad EH, Yellapantula V, Leongamornlert D, Bolli N, Ledergor G, Nadeu F, et al. Timing the initiation of multiple myeloma. Nat Commun. 2020;11:1917.
Maura F, Petljak M, Lionetti M, Cifola I, Liang W, Pinatel E, et al. Biological and prognostic impact of APOBEC-induced mutations in the spectrum of plasma cell dyscrasias and multiple myeloma cell lines. Leukemia. 2018;32:1044–8.
Samur MK, Aktas Samur A, Fulciniti M, Szalat R, Han T, Shammas M, et al. Genome-Wide Somatic Alterations in Multiple Myeloma Reveal a Superior Outcome Group. J Clin Oncol. 2020;38:3107–18.
Fonseca R, Blood EA, Oken MM, Kyle RA, Dewald GW, Bailey RJ, et al. Myeloma and the t(11;14)(q13;q32); evidence for a biologically defined unique subset of patients. Blood. 2002;99:3735–41.
Moreau P, Facon T, Leleu X, Morineau N, Huyghe P, Harousseau JL, et al. Recurrent 14q32 translocations determine the prognosis of multiple myeloma, especially in patients receiving intensive chemotherapy. Blood. 2002;100:1579–83.
Cleynen A, Samur M, Perrot A, Buisson L, Maheo S, Fulciniti M, et al. Variable BCL2/BCL2L1 ratio in multiple myeloma with t(11;14). Blood. 2018;132:2778–80.
Touzeau C, Maciag P, Amiot M, Moreau P. Targeting Bcl-2 for the treatment of multiple myeloma. Leukemia. 2018;32:1899–907.
Kumar S, Kaufman JL, Gasparetto C, Mikhael J, Vij R, Pegourie B, et al. Efficacy of venetoclax as targeted therapy for relapsed/refractory t(11;14) multiple myeloma. Blood. 2017;130:2401–9.
Bonolo De Campos C, Smadbeck JB, Arribas M, Sharma N, Ahmann GJ, Kumar SK, et al. A Single Next Generation Sequencing Assay for Detection of Driver Mutations, Translocations and Copy Number Alterations in Patients with Multiple Myeloma. Blood. 2022;140:7180–1.
Hao S, Lin P, Medeiros LJ, Fang L, Carballo-Zarate AA, Konoplev SN, et al. Clinical implications of cytogenetic heterogeneity in multiple myeloma patients with TP53 deletion. Mod Pathol. 2017;30:1378–86.
Marcon C, Simeon V, Deias P, Facchin G, Corso A, Derudas D, et al. Experts’ consensus on the definition and management of high risk multiple myeloma. Front Oncol. 2022;12:1096852.
Thanendrarajan S, Tian E, Qu P, Mathur P, Schinke C, van Rhee F, et al. The level of deletion 17p and bi-allelic inactivation of TP53 has a significant impact on clinical outcome in multiple myeloma. Haematologica. 2017;102:e364–67.
Liu E, Sudha P, Becker N, Jaouadi O, Suvannasankha A, Lee K, et al. Identifying novel mechanisms of biallelic TP53 loss refines poor outcome for patients with multiple myeloma. Blood Cancer J. 2023;13:144.
Schavgoulidze A, Talbot A, Perrot A, Cazaubiel T, Leleu X, Manier S, et al. Biallelic deletion of 1p32 defines ultra-high-risk myeloma, but monoallelic del(1p32) remains a strong prognostic factor. Blood. 2023;141:1308–15.
Wang H, Meng H, Wang J, Lou Y, Zhou Y, Lin P, et al. Clinical characteristics and prognostic values of 1p32.3 deletion detected through fluorescence in situ hybridization in patients with newly diagnosed multiple myeloma: a single-center study in China. Front Med. 2020;14:327–34.
Croft J, Ellis S, Sherborne AL, Sharp K, Price A, Jenner MW, et al. Copy number evolution and its relationship with patient outcome-an analysis of 178 matched presentation-relapse tumor pairs from the Myeloma XI trial. Leukemia. 2021;35:2043–53.
Walker BA, Leone PE, Chiecchio L, Dickens NJ, Jenner MW, Boyd KD, et al. A compendium of myeloma-associated chromosomal copy number abnormalities and their prognostic value. Blood. 2010;116:e56–65.
Ross FM, Avet-Loiseau H, Ameye G, Gutierrez NC, Liebisch P, O’Connor S, et al. Report from the European Myeloma Network on interphase FISH in multiple myeloma and related disorders. Haematologica. 2012;97:1272–7.
Abdallah N, Greipp P, Kapoor P, Gertz MA, Dispenzieri A, Baughn LB, et al. Clinical characteristics and treatment outcomes of newly diagnosed multiple myeloma with chromosome 1q abnormalities. Blood Adv. 2020;4:3509–19.
Schmidt TM, Fonseca R, Usmani SZ. Chromosome 1q21 abnormalities in multiple myeloma. Blood Cancer J. 2021;11:83.
Fonseca R, Debes-Marun CS, Picken EB, Dewald GW, Bryant SC, Winkler JM, et al. The recurrent IgH translocations are highly associated with nonhyperdiploid variant multiple myeloma. Blood. 2003;102:2562–7.
Koleilat A, Tang H, Sharma N, Yan H, Tian S, Smadbeck J, et al. Disparity in the detection of chromosome 15 centromere in patients of African ancestry with a plasma cell neoplasm. Genet Med Open. 2023;1:100816.
Sidana S, Jevremovic D, Ketterling RP, Tandon N, Dispenzieri A, Gertz MA, et al. Rapid assessment of hyperdiploidy in plasma cell disorders using a novel multi-parametric flow cytometry method. Am J Hematol. 2019;94:424–30.
Peterson JF, Rowsey RA, Marcou CA, Pearce KE, Williamson CM, Frederick LA, et al. Hyperhaploid plasma cell myeloma characterized by poor outcome and monosomy 17 with frequently co-occurring TP53 mutations. Blood Cancer J. 2019;9:20.
Ashby C, Tytarenko RG, Wang Y, Weinhold N, Johnson SK, Bauer M, et al. Poor overall survival in hyperhaploid multiple myeloma is defined by double-hit bi-allelic inactivation of TP53. Oncotarget. 2019;10:732–7.
Tian E, Sawyer JR, Heuck CJ, Zhang Q, van Rhee F, Barlogie B, et al. In multiple myeloma, 14q32 translocations are nonrandom chromosomal fusions driving high expression levels of the respective partner genes. Genes Chromosomes Cancer. 2014;53:549–57.
Bergsagel PL, Kuehl WM, Zhan FH, Sawyer J, Barlogie B, Shaughnessy J. Cyclin D dysregulation: an early and unifying pathogenic event in multiple myeloma. Blood. 2005;106:296–303.
Zhan F, Huang Y, Colla S, Stewart JP, Hanamura I, Gupta S, et al. The molecular classification of multiple myeloma. Blood. 2006;108:2020–8.
Skerget S, Penaherrera D, Chari A, Jagannath S, Siegel DS, Vij R, et al. Comprehensive molecular profiling of multiple myeloma identifies refined copy number and expression subtypes. Nat Genet. 2024;56:1878–89.
Cegledi A, Csukly Z, Fekete M, Kozma A, Szemlaky Z, Andrikovics H, et al. Effective venetoclax-based treatment in relapsed/refractory multiple myeloma patients with translocation t(6;14). Pathol Oncol Res. 2023;29:1611375.
Mikulasova A, Ashby C, Tytarenko RG, Qu P, Rosenthal A, Dent JA, et al. Microhomology-mediated end joining drives complex rearrangements and overexpression of MYC and PVT1 in multiple myeloma. Haematologica. 2020;105:1055–66.
Sharma N, Smadbeck JB, Abdallah N, Zepeda-Mendoza C, Binder M, Pearce KE, et al. The Prognostic Role of MYC Structural Variants Identified by NGS and FISH in Multiple Myeloma. Clin Cancer Res. 2021;27:5430–9.
Walker BA, Wardell CP, Brioli A, Boyle E, Kaiser MF, Begum DB, et al. Translocations at 8q24 juxtapose MYC with genes that harbor superenhancers resulting in overexpression and poor prognosis in myeloma patients. Blood Cancer J. 2014;4:e191.
Misund K, Keane N, Stein CK, Asmann YW, Day G, Welsh S, et al. MYC dysregulation in the progression of multiple myeloma. Leukemia. 2020;34:322–6.
Boyle EM, Deshpande S, Tytarenko R, Ashby C, Wang Y, Bauer MA, et al. The molecular make up of smoldering myeloma highlights the evolutionary pathways leading to multiple myeloma. Nat Commun. 2021;12:293.
Affer M, Chesi M, Chen WG, Keats JJ, Demchenko YN, Roschke AV, et al. Promiscuous MYC locus rearrangements hijack enhancers but mostly super-enhancers to dysregulate MYC expression in multiple myeloma. Leukemia. 2014;28:1725–35.
Barwick BG, Neri P, Bahlis NJ, Nooka AK, Dhodapkar MV, Jaye DL, et al. Multiple myeloma immunoglobulin lambda translocations portend poor prognosis. Nat Commun. 2019;10:1911.
Fonseca R, Bergsagel PL, Drach J, Shaughnessy J, Gutierrez N, Stewart AK, et al. International Myeloma Working Group molecular classification of multiple myeloma: spotlight review. Leukemia. 2009;23:2210–21.
Avet-Loiseau H, Facon T, Grosbois B, Magrangeas F, Rapp MJ, Harousseau JL, et al. Oncogenesis of multiple myeloma: 14q32 and 13q chromosomal abnormalities are not randomly distributed, but correlate with natural history, immunological features, and clinical presentation. Blood. 2002;99:2185–91.
Fonseca R, Harrington D, Oken MM, Dewald GW, Bailey RJ, Van Wier SA, et al. Biological and prognostic significance of interphase fluorescence in situ hybridization detection of chromosome 13 abnormalities (delta13) in multiple myeloma: an eastern cooperative oncology group study. Cancer Res. 2002;62:715–20.
Chiecchio L, Protheroe RK, Ibrahim AH, Cheung KL, Rudduck C, Dagrada GP, et al. Deletion of chromosome 13 detected by conventional cytogenetics is a critical prognostic factor in myeloma. Leukemia. 2006;20:1610–7.
Avet-Loiseau H, Attal M, Moreau P, Charbonnel C, Garban F, Hulin C, et al. Genetic abnormalities and survival in multiple myeloma: the experience of the Intergroupe Francophone du Myelome. Blood. 2007;109:3489–95.
Rajkumar SV, Gupta V, Fonseca R, Dispenzieri A, Gonsalves WI, Larson D, et al. Impact of primary molecular cytogenetic abnormalities and risk of progression in smoldering multiple myeloma. Leukemia. 2013;27:1738–44.
Locher M, Jukic E, Vogi V, Keller MA, Kroll T, Schwendinger S, et al. Amp(1q) and tetraploidy are commonly acquired chromosomal abnormalities in relapsed multiple myeloma. Eur J Haematol. 2023;110:296–304.
Sidana S, Jevremovic D, Ketterling RP, Tandon N, Greipp PT, Baughn LB, et al. Tetraploidy is associated with poor prognosis at diagnosis in multiple myeloma. Am J Hematol. 2019;94:E117–E120.
Walker BA, Mavrommatis K, Wardell CP, Ashby TC, Bauer M, Davies F, et al. A high-risk, Double-Hit, group of newly diagnosed myeloma identified by genomic analysis. Leukemia. 2019;33:159–70.
Lode L, Eveillard M, Trichet V, Soussi T, Wuilleme S, Richebourg S, et al. Mutations in TP53 are exclusively associated with del(17p) in multiple myeloma. Haematologica. 2010;95:1973–6.
Sudha P, Ahsan A, Ashby C, Kausar T, Khera A, Kazeroun MH, et al. Myeloma Genome Project Panel is a Comprehensive Targeted Genomics Panel for Molecular Profiling of Patients with Multiple Myeloma. Clin Cancer Res. 2022;28:2854–64.
Bolli N, Li Y, Sathiaseelan V, Raine K, Jones D, Ganly P, et al. A DNA target-enrichment approach to detect mutations, copy number changes and immunoglobulin translocations in multiple myeloma. Blood Cancer J. 2016;6:e467.
White BS, Lanc I, O’Neal J, Gupta H, Fulton RS, Schmidt H, et al. A multiple myeloma-specific capture sequencing platform discovers novel translocations and frequent, risk-associated point mutations in IGLL5. Blood Cancer J. 2018;8:35.
Yellapantula V, Hultcrantz M, Rustad EH, Wasserman E, Londono D, Cimera R, et al. Comprehensive detection of recurring genomic abnormalities: a targeted sequencing approach for multiple myeloma. Blood Cancer J. 2019;9:101.
Akkari YMN, Baughn LB, Dubuc AM, Smith AC, Mallo M, Dal Cin P, et al. Guiding the global evolution of cytogenetic testing for hematologic malignancies. Blood. 2022;139:2273–84.
Draube A, Pfister R, Vockerodt M, Schuster S, Kube D, Diehl V, et al. Immunomagnetic enrichment of CD138 positive cells from weakly infiltrated myeloma patients samples enables the determination of the tumor clone specific IgH rearrangement. Ann Hematol. 2001;80:83–89.
Gagnon MF, Midthun SM, Fangel JA, Schuh CM, Luoma IM, Pearce KE, et al. Superior detection rate of plasma cell FISH using FACS-FISH. Am J Clin Pathol. 2024;161:60–70.
Hartmann L, Biggerstaff JS, Chapman DB, Scott JM, Johnson KR, Ghirardelli KM, et al. Detection of genomic abnormalities in multiple myeloma: the application of FISH analysis in combination with various plasma cell enrichment techniques. Am J Clin Pathol. 2011;136:712–20.
Lu G, Muddasani R, Orlowski RZ, Abruzzo LV, Qazilbash MH, You MJ, et al. Plasma cell enrichment enhances detection of high-risk cytogenomic abnormalities by fluorescence in situ hybridization and improves risk stratification of patients with plasma cell neoplasms. Arch Pathol Lab Med. 2013;137:625–31.
Lu G, Zhang XX, You MJ, Chen W. Correlation of assessment of plasma cells by flow cytometry and detection of cytogenomic abnormalities by fluorescence in situ hybridization in plasma cell neoplasms. Int J Lab Hematol. 2011;33:545–50.
Pozdnyakova O, Crowley-Larsen P, Zota V, Wang SA, Miron PM. Interphase FISH in plasma cell dyscrasia: increase in abnormality detection with plasma cell enrichment. Cancer Genet Cytogenet. 2009;189:112–7.
Tembhare PR, Ghogale S, Tauro W, Badrinath Y, Deshpande N, Kedia S, et al. Evaluation of CD229 as a new alternative plasma cell gating marker in the flow cytometric immunophenotyping of monoclonal gammopathies. Cytom B Clin Cytom. 2018;94:509–19.
Paiva B, Almeida J, Perez-Andres M, Mateo G, Lopez A, Rasillo A, et al. Utility of flow cytometry immunophenotyping in multiple myeloma and other clonal plasma cell-related disorders. Cytom B Clin Cytom. 2010;78:239–52.
Ahmann GJ, Chng WJ, Henderson KJ, Price-Troska TL, DeGoey RW, Timm MM, et al. Effect of tissue shipping on plasma cell isolation, viability, and RNA integrity in the context of a centralized good laboratory practice-certified tissue banking facility. Cancer Epidemiol Biomark Prev. 2008;17:666–73.
Christensen JH, Abildgaard N, Plesner T, Nibe A, Nielsen O, Sørensen AG, et al. Interphase fluorescence in situ hybridization in multiple myeloma and monoclonal gammopathy of undetermined significance without and with positive plasma cell identification: analysis of 192 cases from the Region of Southern Denmark. Cancer Genet Cytogenet. 2007;174:89–99.
Akkari Y, Baughn LB, Kim A, Karaca E, Raca G, Shao L, et al. Section E6.1-6.6 of the American College of Medical Genetics and Genomics (ACMG) Technical Laboratory Standards: Cytogenomic studies of acquired chromosomal abnormalities in neoplastic blood, bone marrow, and lymph nodes. Genet Med. 2024;26:101054.
Mascarello JT, Hirsch B, Kearney HM, Ketterling RP, Olson SB, Quigley DI, et al. Section E9 of the American College of Medical Genetics technical standards and guidelines: fluorescence in situ hybridization. Genet Med. 2011;13:667–75.
Stevens-Kroef M, Weghuis DO, Croockewit S, Derksen L, Hooijer J, Elidrissi-Zaynoun N, et al. High detection rate of clinically relevant genomic abnormalities in plasma cells enriched from patients with multiple myeloma. Genes Chromosomes Cancer. 2012;51:997–1006.
Yu Y, Shen H, Liu L, Luo P, Wu S, He J, et al. Interphase Fluorescence in situ Hybridization of Bone Marrow Smears of Multiple Myeloma. J Vis Exp. 2022. https://doi.org/10.3791/63083.
Kumar S, Fonseca R, Ketterling RP, Dispenzieri A, Lacy MQ, Gertz MA, et al. Trisomies in multiple myeloma: impact on survival in patients with high-risk cytogenetics. Blood. 2012;119:2100–5.
Sawyer JR. The prognostic significance of cytogenetics and molecular profiling in multiple myeloma. Cancer Genet. 2011;204:3–12.
Mellors PW, Binder M, Ketterling RP, Greipp PT, Baughn LB, Peterson JF, et al. Metaphase cytogenetics and plasma cell proliferation index for risk stratification in newly diagnosed multiple myeloma. Blood Adv. 2020;4:2236–44.
Dewald GW, Kyle RA, Hicks GA, Greipp PR. The clinical significance of cytogenetic studies in 100 patients with multiple myeloma, plasma cell leukemia, or amyloidosis. Blood. 1985;66:380–90.
Carballo-Zarate AA, Medeiros LJ, Fang LH, Shah JJ, Weber DM, Thomas SK, et al. Additional-structural-chromosomal aberrations are associated with inferior clinical outcome in patients with hyperdiploid multiple myeloma: a single-institution experience. Mod Pathol. 2017;30:843–53.
Clarke SE, Fuller KA, Erber WN. Chromosomal defects in multiple myeloma. Blood Rev. 2024;64:101168.
Cohen YC, Zada M, Wang SY, Bornstein C, David E, Moshe A, et al. Identification of resistance pathways and therapeutic targets in relapsed multiple myeloma patients through single-cell sequencing. Nat Med. 2021;27:491-+.
Tirier SM, Mallm JP, Steiger S, Poos AM, Awwad MHS, Giesen N. Subclone-specific microenvironmental impact and drug response in refractory multiple myeloma revealed by single-cell transcriptomics. Nat Commun. 2021;12:6960.
Acknowledgements
We thank the survey respondents, the members of the Cancer Genomics Consortium board of directors and members of the community for reviewing the manuscript.
Author information
Authors and Affiliations
Contributions
XL, EFA, CCE, PRG, AML, PMM, TP, FQR, VCT, DJW, JZ, LBB contributed to survey creation, literature data review, survey data analysis, and manuscript preparation and approved the final content. XL and LBB wrote the original manuscript draft. RB, SK, RF reviewed survey data, reviewed the manuscript and approved the final content.
Corresponding author
Ethics declarations
Competing interests
EA reports consultancy AbbVie. RB reports consultancy Adaptive Biotech, BMS, Caribou Biosciences, Genentech, Janssen, Karyopharm, Legend Biotech, Pfizer, Sanofi, SparkCures; Research: Novartis, Pack Health. RF reports consultancy for AbbVie, Adaptive Biotechnologies, AMGEN, AZeneca, Bayer, Binding Site, BMS (Celgene), Millenium Takeda, Jansen, Juno, Kite, Merck, Pfizer, Pharmacyclics, Regeneron, Sanofi; scientific advisory boards for Adaptive Biotechnologies, Caris Life Sciences, Oncotracker; board of directors for Antegene, AZBio; and patents for FISH in myeloma. SK reports consultancy from BMS/Celgene, Takeda and Janssen and research funding from BMS (Celgene), Takeda, Novartis, AbbVie, Janssen and Amgen. LBB reports consultancy Genentech. The remaining authors have no interests to disclose.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lu, X., Andersen, E.F., Banerjee, R. et al. Guidelines for the testing and reporting of cytogenetic results for risk stratification of multiple myeloma: a report of the Cancer Genomics Consortium Plasma Cell Neoplasm Working Group. Blood Cancer J. 15, 86 (2025). https://doi.org/10.1038/s41408-025-01286-w
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41408-025-01286-w
This article is cited by
-
Regulation of stress tolerance by CREB1 sustains multiple myeloma cell survival
Cell Death & Disease (2026)
-
Characterization of cytogenetic abnormalities in Lebanese multiple myeloma patients
BMC Cancer (2025)
-
Genomic Alterations in Multiple Myeloma: A Comprehensive Landscape
Indian Journal of Hematology and Blood Transfusion (2025)