Abstract
Quality of life of patients who undergo allogeneic hematopoietic stem cell transplantation (HSCT) temporally deteriorates and recovers over several years. We retrospectively evaluate the impact of chronic graft-versus-host disease (GVHD) and glucocorticoid on physical recovery. We included 162 patients who underwent their first allogeneic HSCT between October 2010 and December 2015 in a single hospital. All patients are planned to undergo physical function tests before and 1, 3, 12 months after allogeneic HSCT. Scores of knee extension strength and distance covered in the 6-min walk test (6MWT) recovered at the 12-month assessment. Both chronic GVHD and high dose glucocorticoid were associated with delayed recovery of body mass index (BMI), hand grip strength, knee extension strength, and duration of standing on one foot. Lung GVHD and high dose glucocorticoid had negative impact on the distance covered in the 6MWT. A multivariate analysis revealed that chronic GVHD and glucocorticoid was an independent risk factor for decreased BMI and delayed recovery of muscle strength, respectively. Our results suggest that high-risk patients who have chronic GVHD or who receive glucocorticoid therapy may require reduced dose of glucocorticoid and long-term physical support to recover physical function after transplantation.
Similar content being viewed by others
Introduction
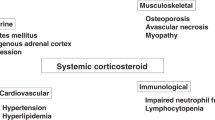
Allogeneic hematopoietic stem cell transplantation (HSCT) has achieved long-term disease remission and survival for patients with hematologic diseases. However, the quality of life (QOL) of long-term survivors who have undergone allogeneic HSCT is sometimes deteriorated because of comorbidities. Graft-versus-host disease (GVHD), infectious diseases, organ failure, disease relapse, and secondary malignancy are major causes of mortality after allogeneic HSCT. Even if patients survive these comorbidities, both their physical and psychological function are often impaired [1, 2]. Although physical function is temporarily impaired for several months after allogeneic HSCT, many survivors eventually recover from any major physical limitations by about 1 year after the procedure [1, 3]. Physical intervention is considered to be important for promoting physical recovery in allogeneic HSCT recipients [4, 5]. However, a significant percentage of patients with comorbidities suffer from persistent physical limitations. Chronic GVHD is a major factor that reduces physical QOL [6] and physical functional capacity [7]. Moreover, patients with chronic GVHD sometimes require long-term glucocorticoid administration, which reduces muscle strength [8,9,10,11]. Several studies showed that hand grip strength, 2-min walk test, range of motion correlated with chronic GVHD symptoms [12]. In this study, we evaluated association of physical recovery after HSCT with chronic GVHD quantitatively from physical function tests in our institution.
In our institution, we started routine rehabilitation in 2010, which was usual physical rehabilitation therapy during hospitalization followed by ongoing physical assessment by physical trainers for all allogeneic HSCT recipients. In this study, we retrospectively analyzed the changes in physical function in allogeneic HSCT recipients based on medical records at our hospital. Particularly, we focused on the associations of chronic GVHD and glucocorticoid administration with delayed recovery of physical function.
Methods
Study patients
We retrospectively analyzed the records of 162 consecutive patients who underwent their first allogeneic HSCT at our institution between October 1, 2010 and December 31, 2015. Eligible participants were at least 16 years old at allogeneic HSCT. Allogeneic HSCT recipients underwent physical function assessments according to the programmed schedule. Changes in physical assessment scores after HSCT were evaluated. Chronic GVHD status and cumulative dose of glucocorticoid were investigated along with other factors associated with the patient and disease backgrounds, transplantation procedures and clinical course after allogeneic HSCT. Based on these data, the associations between changes in physical function and chronic GVHD status or cumulative dose of glucocorticoid were assessed.
According to the Japanese ethics guidelines for clinical studies, informed consent was not obtained from each participant. Instead, we provided information regarding this retrospective observational study online and allowed patients to exclude themselves from the study if they did not want for us to use their data. This study was approved by the Institutional Review Board of Saitama Medical Center, Jichi Medical University.
Transplantation procedures
Patients received a myeloablative or reduced-intensity conditioning regimen [13] before transplantation. Continuous infusion of calcineurin inhibitor (CNI) (cyclosporine or tacrolimus) and short-term methotrexate were used as GVHD prophylaxis [14]. Anti-thymocyte globulin or alemtuzumab was added as in vivo T-cell depletion before transplantation from a human leukocyte-antigen mismatched donor [15, 16].
Rehabilitation and physical assessment
All recipients participated in the routine rehabilitation unless they declined. Physical function was assessed before and 1, 3, and 12 months after allogeneic HSCT. Assessments at 1 month were performed after engraftment. After patients were discharged, assessments were conducted at the time of outpatient visits. Physical function assessments were delayed or skipped when the patient was in a poor medical condition.
Assessment of physical function
In the physical function test, body height, body weight, hand grip strength, knee extension strength, duration of standing on one foot, length of body anteflexion, and distance covered in a 6-min walk test (6MWT) were recorded. Body mass index (BMI) was calculated as body weight (kg) divided by squared body height (m). Hand grip strength and knee extension strength were recorded as indicators of muscle strength. Hand grip strength was recorded by a digital grip dynamometer (T.K.K.5401 GRIP D, TAKEI, Japan) as the patient stood upright and gripped the dynamometer. Knee extension strength was recorded as isometric strength by a hand-held dynamometer (μTas F-1, Anima, Japan): the patient sat with their feet off the ground and their knee joint at a 90-degree angle. The dynamometer was fixed at their ankle, and the patient then extended their knee joint. The highest of two measurements was recorded as the score for each hand and foot. Standing on one foot is a balance test that is associated with injurious falls [17]. It was recorded as the amount of time that the patient could continue to stand on one foot on a flat floor with their eyes open. The test was ended at a maximum of 60 s, which has been shown to be sufficient for detecting a change in physical capacity [18]. Length of body anteflexion was used as an indicator of flexibility: it was recorded as the distance that the patient, from a sitting position with their hip joint at a 90-degree angle and knees extended, could move their fingertips while they held their hands forward and bent their torso forward [19]. 6MWT was conducted around a square with 5-m sides in our rehabilitation center, otherwise it was conducted as described in the literature [20]. The distance walked in 6 min was recorded.
GVHD assessment and cumulative glucocorticoid dose
Acute GVHD, chronic GVHD and cumulative glucocorticoid dose were evaluated. The severities of the worst chronic GVHD symptoms were graded according to National Institutes of Health (NIH) severity criteria [21]. Organ response was evaluated by chronic GVHD symptoms at 12-month assessment. Then, overall response was assessed according to the NIH therapeutic response criteria [22]. Complete response (CR) was defined as resolution of all manifestations in each organ or site, and partial response (PR) was defined as improvement in at least 1 organ or site without progression in any other organ or site. Patients were classified into three groups according to chronic GVHD status and response to the treatment: A: without chronic GVHD, B: with chronic GVHD who had CR or PR to the treatment, and C: with chronic GVHD who had no response to the treatment. The reason for glucocorticoid administration and the daily glucocorticoid dose were extracted from the records. The glucocorticoid dose was adjusted to units of milligrams of prednisolone per patient’s body weight (kg) under the assumption that the relative potencies of hydrocortisone, prednisolone, methylprednisolone, and dexamethasone are 1:4:5:30. The cumulative dose of glucocorticoid was calculated between day 0 and the day of the 12-month physical assessment.
Statistical analysis
Physical assessment scores after transplantation were compared to scores before transplantation by a paired t-test or Wilcoxon signed-rank test. Scores of patients who survived and underwent a 12-month assessment were included in the analysis of the impact of chronic GVHD and glucocorticoid. Multivariate linear regression was used to assess the effects of various factors on the physical assessment score. Objective variables are expressed as the ratios of scores at the 12-month assessment to scores before transplantation. Factors with borderline significance (p < 0.15) in a univariate analysis were assessed by a multivariate linear regression analysis. Multicollinearity was evaluated. The impact of chronic GVHD was assessed by a t-test or Wilcoxon signed-rank test, which compared the percentage changes in scores between assessments before and 12 months after HSCT for patients with or without GVHD. Analysis of variance (ANOVA) or the Kruskal–Wallis rank sum test was performed to compare the scores of three groups. When a significant difference was detected, the Bonferroni correction was applied. The correlation between the cumulative glucocorticoid dose and physical assessment scores was evaluated by Pearson’s correlation coefficient or Spearman’s test. Subsequently, the association between the cumulative dose of glucocorticoid and physical assessment scores was estimated by a linear regression analysis. In these analyses, the percentage changes in physical assessment scores from baseline to 12 months were analyzed. The impact of lung GVHD on the 6-min walking distance was evaluated by a paired t-test. The cut-off p value was set at .05. All statistical analyses were performed with R version 3.3.2 (The R Foundation for Statistical Computing, Vienna, Austria) and EZR version 1.3.3. (Saitama Medical Center, Jichi Medical University, Saitama, Japan; http://www.jichi.ac.jp/saitama-sct/SaitamaHP.files/statmedEN.html) [23]. EZR is a graphical user interface for R. More precisely, it is a modified version of R commander designed to add statistical functions frequently used in biostatistics.
Results
Patient characteristics
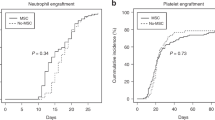
A total of 162 patients underwent allogeneic HSCT at our institute during the study period. Among them, 93 patients (57.4%) survived at least 1 year after HSCT and continued to visit our hospital. Baseline patient, disease, and treatment characteristics are shown in Table 1.
Incidence of GVHD
Chronic GVHD was diagnosed in 48 (51.6%, 95% confidence interval: 41.0–62.1%) survivors. Thirteen (14.0%, 7.7–22.7%), 19 (20.4%, 12.8–30.1%), and 16 (17.2%, 10.2–26.4%) were diagnosed as mild, moderate, and severe chronic GVHD, respectively. Organ specific chronic GVHD score was shown in the Table 2. Only few patients developed joint or sclerodermic involvement, and thus, it was difficult to separately analyze joint or sclerodermic involvement. Some patients developed joint involvement after 12-month follow up. Among 48 patients with chronic GVHD, 22, 19, 1, and 6 patients were treated by systemic glucocorticoid + CNI, CNI only, systemic glucocorticoid only, topical therapy only, and the response rate was 67% in total. When 8 patients who had chronic GVHD and died before 12-month assessment were included, the response rate was 66%. Thirty-two of 48 patients had PR or CR to the treatment. Eleven of 13 patients with chronic lung GVHD were treated by systemic glucocorticoid. Acute GVHD was diagnosed in 72 (77.4%, 67.6–85.4%) survivors. Cumulative incidence of acute GVHD grade II-IV, and grade III-IV were 34.1% and 12.5%, respectively. The frequency of skin, liver, and gastrointestinal tract acute GVHD was 68 (73.1%), 3 (3.22%), and 16 (17.2%), and organ stage is shown in the Table 3. Unfortunately, we could not precisely identify patients with late acute or overlap GVHD due to retrospective nature of this study.
Glucocorticoid treatment
Twenty-two (45.8%) of 48 patients with chronic GVHD and 26 (36.1%) of 72 patients with acute GVHD were treated with systemic glucocorticoid equivalent to prednisolone at 0.5 mg/kg/day or more. Seven patients received glucocorticoid for reasons other than GVHD. The cumulative glucocorticoid dose was evaluated in 84 patients who underwent a physical assessment at 12 months. The median cumulative glucocorticoid dose in all patients and in 62 patients who received glucocorticoid at least once after HSCT was 3.6 mg/kg (range, 0–241.4) and 25.79 mg/kg (range, 0.29–241.4), respectively. The median cumulative glucocorticoid dose in patients with chronic GVHD was 25.96 mg/kg (0–174.6).
Physical assessment
In 162 patients who received allogeneic HSCT, 159 (98%), 123 (76%), 106 (65%), and 84 (52%) patients underwent physical assessment before and 1, 3, and 12 months after transplantation, respectively (Fig. 1). The percentages of survivors who completed all four assessments at each physical test were between 62 and 74% (Supplementary Table 1). Figure 2 shows boxplots of the time-dependent changes in physical scores. Generally, muscle strength scores tended to decrease at the 1-month and 3-month assessments and recover at the 12-month assessment. Scores of BMI, hand grip strength, knee extension strength, duration of standing on one foot, and distance covered in the 6MWT significantly decreased at the 1-month assessment. Scores of knee extension strength and distance covered in the 6MWT recovered to the respective levels before HSCT at the 3-month and 12-month assessments, respectively (Supplementary Table 1).
Time-dependent changes in physical assessment scores. Each boxplot shows the median score, first quartile, and third quartile as a bold line, upper hinge, and lower hinge. Outlier values that exceed 1.5 × interquartile ranges are shown as dot plots. kgf: kilogram-force (1 kgf = 9.8 N). Pre assessment before HSCT, 1 mo assessment 1 month after HSCT, 3 mo assessment 3 months after HSCT, 12 mo assessment 12 months after HSCT, BMI body mass index, HSCT hematopoietic stem cell transplantation
Impact of chronic GVHD on physical function
Changes in scores between the assessment before transplantation and the assessment at 12 months in patients with or without chronic GVHD are shown in Fig. 3a. BMI (p < 0.001), right hand grip strength (p = 0.02), knee extension strength (Right: p < 0.01, Left: p < 0.001), and duration of standing on the left foot (p = 0.02) decreased more in patients with chronic GVHD. Although there were no significant differences in left hand grip strength or duration of standing on the right foot, the scores decreased more in patients with chronic GVHD (Fig. 3a).
a Changes in physical assessment scores of patients with or without cGVHD. b Changes in distance covered in the 6-min walk test for patients with or without lung GVHD. Circles and triangles represents mean scores. Error bars represent standard deviation. P values are the result of comparing percentage changes between assessments before and 12 months after HSCT in patients with or without GVHD symptoms. kgf: kilogram-force (1 kgf = 9.8 N). Pre assessment before HSCT, 1 mo assessment 1 month after HSCT, 3 mo assessment 3 months after HSCT, 12 mo assessment 12 months after HSCT, BMI body mass index, HSCT hematopoietic stem cell transplantation, GVHD graft-versus-host disease, cGVHD chronic graft-versus-host disease
Relative changes in BMI and knee extension strength between the assessment before transplantation and the assessment at 12 months were significantly different among the three groups classified according to the chronic GVHD status by both ANOVA and the Kruskal–Wallis rank sum test (Supplementary Table 2). The changes in BMI and left knee extension strength were greater in groups B (p < 0.001 and p < 0.01) than in group A by the Bonferroni method, respectively.
Chronic lung GVHD had a negative impact on the distance covered in the 6MWT at the 12-month physical assessment in comparison with assessment before transplantation (11.6% vs. −5.93%, p = 0.023) (Fig. 3b).
Impact of glucocorticoid dose on physical function
The cumulative glucocorticoid dose was negatively correlated with changes in BMI (r = −0.38, 95% confidence interval: −0.56 to −0.18, p < 0.001), hand grip strength (Right: r = -0.37, −0.53 to −0.16, p < 0.001; Left: r = −0.31, −0.49 to −0.10, p < 0.01), knee extension strength (Right: r = −0.49, −0.64 to −0.30, p < 0.001; Left: r = -0.34, −0.53 to −0.12, p < 0.01), duration of standing on one foot (Right: r = −0.31, −0.36 to −0.07, p < 0.01, Left: r = −0.32, −0.40 to −0.02, p < 0.01), and distance covered in the 6MWT (r = −0.38, −0.56 to −0.17, p < 0.001) by both the Pearson method and Spearman’s method (Fig. 4).
Factors that influenced physical function
A univariate analysis was performed to identify factors that influenced physical function at the 12-month assessment. The effects of patient age, sex, Eastern Cooperative Oncology Group (ECOG) performance status (PS), Karnofsky PS, Hematopoietic Cell Transplantation-Comorbidity Index (HCT-CI), donor source, conditioning intensity, disease risk, severity of acute GVHD, chronic GVHD, cumulative glucocorticoid dose, duration of hospitalization after HSCT, and relapse on changes in physical function were assessed. The results of this univariate analysis suggested that severe acute GVHD, chronic GVHD, and administration of glucocorticoid affected BMI, muscle strength, and distance covered in the 6MWT. Multivariate models that included variables with p values less than 0.15 in the univariate analysis were used to assess the effects of chronic GVHD and glucocorticoid (Supplementary table 3).
A multivariate analysis revealed that chronic GVHD was an independent risk factor for decreased BMI. Glucocorticoid administration was an independent risk factor for decreased hand grip strength and knee extension strength (Table 4). Statistical significance of the results about sex, age, Karnofsky PS, and relapse was inconsistent on left and right. Good PS (ECOG PS 0 and 1) was associated with earlier recovery of both hand grip strength. Acute GVHD grade III-IV and poor HCT-CI (HCT-CI > 0) were associated with decreased BMI and recovery of body anteflexion.
Discussion
This study retrospectively investigated physical performance in patients who underwent allogeneic HSCT by repeated tests of physical function. The results of this study showed that physical function worsened after allogeneic HSCT and tended to recover within 1 year, consistent with previous studies [1, 6, 8]. However, the pattern of recovery seemed to differ depending on the test used to assess physical function. Knee extension strength and 6MWT recover to the pre-transplantation levels in our study. Knee extension strength and distance covered in the 6MWT may show relatively good recovery due to frequent use of muscles in the lower extremities and a good response to lower extremity muscle training as described previously [4]. On the other hand, muscles of the upper extremities may be less likely to be trained actively. With respect to the impact of glucocorticoid, muscle weakness at 12-month assessment was greater in the lower limbs than in the upper limbs among patients who received glucocorticoid. Previous reviews have reported that glucocorticoid-induced myopathy strongly affected muscles of the lower extremities in allogeneic HSCT recipients [9,10,11].
Both chronic GVHD [12, 24,25,26,27] and glucocorticoid [8] were associated with impaired physical function. The success rate of systemic glucocorticoid treatment with or without CNIs for the treatment of chronic GVHD has been reported to be approximately 40 to 50%, which is consistent with the results of our study [28]. From the results of this study, glucocorticoid therapy, in addition to chronic GHVD, was considered to strongly influence performance in the physical function test. Our results suggest that the dose of glucocorticoid during chronic GVHD treatment should be gradually tapered to reduce the deterioration of physical function, as described previously [29], as long as the symptoms of chronic GVHD are controlled.
A previous study showed that patients with resolved chronic GVHD had less severe adverse health conditions than patients with active chronic GVHD in terms of patient-reported general health, mental health, functional impairment, activity limitation, and pain [30, 31]. In contrast to these previous studies, the changes in most of the physical function scores in this study were not significantly different among those with active chronic GVHD, those with improved chronic GVHD, and those who did not experience chronic GVHD. This might reflect the fact that chronic GVHD had a different impact on physical function tests depending on the involved organs. Especially, skin, joint/fascia, and lung involvement may have the greatest negative impact on physical function and QOL [25]. In fact, lung chronic GVHD had a negative impact on 6MWT, which reflects not only muscle strength but also cardio-pulmonary function, at the 12-month assessment in our study, similar to the results of previous studies [7, 25, 32]. Another plausible explanation is that patients with improved chronic GVHD in our study included those with improving but still active chronic GVHD. Furthermore, the number of such patients was limited. Therefore, it is still important to control chronic GVHD, even though an improvement of chronic GVHD was not directly associated with an improvement of objective scores of physical function in our study.
In a previous study, brief training and stress management did not improve the scores on a physical component summary scale in patients who underwent HSCT [33], whereas several studies on physical intervention during hospitalization and more than several weeks following hospital discharge showed improved physical function and fatigue several months after HSCT [4, 5, 34, 35]. These studies suggested that early intervention was effective, but these intervention programs were not designed for patients with chronic GVHD. Our rehabilitation program was not intense and was provided only during hospitalization. Although there is little evidence available regarding the effect of exercise for patients with chronic GVHD, long-term intervention might help physical function to recover in patients with chronic GVHD. Effective intervention methods for patients who require long-term support are needed, and that effective glucocorticoid sparing strategy for management of chronic GVHD is also warranted.
Multivariate analyses in this study revealed the possible risk factors for delayed physical recovery, and results of multivariate analyses suggested the necessity of supportive care for the patients with risk factors. However, the clinical importance of these results of multivariate analyses should be interpreted with caution and further analysis is warranted.
Our research has limitations. Previous studies reported that hand grip strength [36] and a 2-min walk test [7, 12, 20] could be used as standard physical functional capacity tests under chronic GVHD. Since our measurement procedure was somewhat different from those in other studies, the results of our research should be interpreted with caution, particularly when comparing them to the results of other studies. Second, only patients who survived at least 12 months after HSCT were included in this study. A previous study reported that patients who died or discontinued physical assessments during research had a lower physical QOL [6]. Since a significant number of patients with very severe chronic GVHD or poor functional status who died within 12 months after HSCT or skipped the assessments were not included in the statistical analysis in this study, there is a possibility that the deterioration of physical function in patients with life-threatening complications was underestimated. Finally, multiple testing is potentially a problem in our statistical results. Further study is warranted to confirm our study results.
In conclusion, the physical function in patients who underwent allogeneic HSCT tends to recover within 12 months after transplantation. Patients with chronic GVHD experienced delayed recovery of BMI and muscle strength. Those with lung GVHD experienced a delayed recovery of cardiopulmonary function. The cumulative dose of glucocorticoid was associated with a deterioration of muscle strength. In a multivariate analysis, systemic glucocorticoid administration was the sole independent risk factor for the delayed recovery of muscle strength. Our results suggest that patients who have chronic GVHD or who receive glucocorticoid therapy may require long-term physical support to recover physical function after transplantation.
References
Syrjala KL, Langer SL, Abrams JR, Storer B, Sanders JE, Flowers MED, et al. Recovery and long-term function after hematopoietic cell transplantation for leukemia or lymphoma. JAMA. 2004;291:2335–43.
Andrykowski MA, Bishop MM, Hahn EA, Cella DF, Beaumont JL, Brady MJ, et al. Long-term health-related quality of life, growth, and spiritual well-being after hematopoietic stem-cell transplantation. J Clin Oncol. 2005;23:599–608.
Morton LM, Saber W, Baker KS, Barrett AJ, Bhatia S, Engels EA, et al. National institutes of health hematopoietic cell transplantation late effects initiative: the subsequent neoplasms working group report. Biol Blood Marrow Transplant. 2017;23:367–78.
Wiskemann J, Dreger P, Schwerdtfeger R, Bondong A, Huber G, Kleindienst N, et al. Effects of a partly self-administered exercise program before, during, and after allogeneic stem cell transplantation. Blood. 2011;117:2604–13.
Hacker ED, Collins E, Park C, Peters T, Patel P, Rondelli D. Strength training to enhance early recovery after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2017;23:659–69.
Wong FL, Francisco L, Togawa K, Bosworth A, Gonzales M, Hanby C, et al. Long-term recovery after hematopoietic cell transplantation: predictors of quality of life concerns. Blood. 2010;115:2508–20.
Pidala J, Chai X, Martin P, Inamoto Y, Cutler C, Palmer J, et al. Hand grip strength and 2-minute walk test in chronic graft-versus-host disease assessment: Analysis from the chronic GVHD consortium. Biol Blood Marrow Transplant. 2013;19:967–72.
Morishita S, Kaida K, Yamauchi S, Sota K, Ishii S, Ikegame K, et al. Relationship between corticosteroid dose and declines in physical function among allogeneic hematopoietic stem cell transplantation patients. Support Care Cancer. 2013;21:2161–9.
Gupta A, Gupta Y. Glucocorticoid-induced myopathy: pathophysiology, diagnosis, and treatment. Indian J Endocrinol Metab. 2013;17:913–6.
Pereira RMR, Freire de Carvalho J. Glucocorticoid-induced myopathy. Jt Bone Spine. 2011;78:41–44.
Guis S, Mattéi J-P, Lioté F. Drug-induced and toxic myopathies. Best Pract Res Clin Rheumatol. 2003;17:877–907.
Fiuza-Luces C, Simpson RJ, Ramírez M, Lucia A, Berger NA. Physical function and quality of life in patients with chronic GvHD: a summary of preclinical and clinical studies and a call for exercise intervention trials in patients. Bone Marrow Transplant. 2016;51:13–26.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33.
Kanda Y, Kobayashi T, Mori T, Tanaka M, Nakaseko C, Yokota A, et al. A randomized controlled trial of cyclosporine and tacrolimus with strict control of blood concentrations after unrelated bone marrow transplantation. Bone Marrow Transplant. 2016;51:103–9.
Kanda Y, Oshima K, Kako S, Fukuda T, Uchida N, Miyamura K, et al. In vivo T-cell depletion with alemtuzumab in allogeneic hematopoietic stem cell transplantation: Combined results of two studies on aplastic anemia and HLA-mismatched haploidentical transplantation. Am J Hematol. 2013;88:294–300.
Kako S, Akahoshi Y, Harada N, Nakano H, Kameda K, Ugai T, et al. HLA-mismatched haploidentical transplantation using low-dose anti-thymocyte globulin (ATG: thymoglobulin). Hematology. 2017;22:129–35.
Vellas BJ, Wayne SJ, Romero L, Baumgartner RN, Rubenstein LZ, Garry PJ. One-leg balance is an important predictor of injurious falls in older persons. J Am Geriatr Soc. 1997;45:735–8.
Springer BA, Marin R, Cyhan T, Roberts H, Gill NW. Normative values for the unipedal stance test with eyes open and closed. J Geriatr Phys Ther. 2007;30:8–15.
Narita T, Kaneoka K, Takemura M, Sakata Y, Nomura T, Miyakawa S. Critical factors for the prevention of low back pain in elite junior divers. Br J Sports Med. 2014;48:919–23.
Crapo RO, Casaburi R, Coates AL, Enright PL, MacIntyre NR, McKay RT, et al. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transplant. 2015;21:389–401.
Lee SJ, Wolff D, Kitko C, Koreth J, Inamoto Y, Jagasia M, et al. Measuring therapeutic response in chronic graft-versus-host disease. National institutes of health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: IV. The 2014 response criteria working group report. Biol Blood Marrow Transplant. 2015;21:984–99.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Mitchell SA, Leidy NK, Mooney KH, Dudley WN, Beck SL, LaStayo PC, et al. Determinants of functional performance in long-term survivors of allogeneic hematopoietic stem cell transplantation with chronic graft-versus-host disease (cGVHD). Bone Marrow Transplant. 2010;45:762–9.
Baird K, Steinberg SM, Grkovic L, Pulanic D, Cowen EW, Mitchell SA, et al. National Institutes of Health chronic graft-versus-host disease staging in severely affected patients: organ and global scoring correlate with established indicators of disease severity and prognosis. Biol Blood Marrow Transplant. 2013;19:632–9.
Pidala J, Vogelsang G, Martin P, Chai X, Storer B, Pavletic S, et al. Overlap subtype of chronic graft-versus-host disease is associated with an adverse prognosis, functional impairment, and inferior patient-reported outcomes: A Chronic Graft-versus-Host Disease Consortium study. Haematologica. 2012;97:451–8.
El-Jawahri A, Pidala J, Inamoto Y, Chai X, Khera N, Wood WA, et al. Impact of age on quality of life, functional status, and survival in patients with chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2014;20:1341–8.
Inamoto Y, Flowers MED, Sandmaier BM, Aki SZ, Carpenter PA, Lee SJ, et al. Failure-free survival after initial systemic treatment of chronic graft-versus-host disease. Blood. 2014;124:1363–71.
Flowers MED, Martin PJ. How we treat chronic graft-versus-host disease. Blood. 2015;125:606–15.
Fraser CJ, Bhatia S, Ness K, Carter A, Francisco L, Arora M, et al. Impact of chronic graft-versus-host disease on the health status of hematopoietic cell transplantation survivors: a report from the Bone Marrow Transplant Survivor Study. Blood. 2006;108:2867–73.
Hudson MM. Health status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. JAMA J Am Med Assoc. 2003;290:1583–92.
Kurosawa S, Oshima K, Yamaguchi T, Yanagisawa A, Fukuda T, Kanamori H, et al. Quality of life after allogeneic hematopoietic cell transplantation according to affected organ and severity of chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2017. https://doi.org/10.1016/j.bbmt.2017.06.011.
Jacobsen PB, Le-Rademacher J, Jim H, Syrjala K, Wingard JR, Logan B, et al. Exercise and stress management training prior to hematopoietic cell transplantation: Blood and marrow transplant clinical trials network (BMT CTN) 0902. Biol Blood Marrow Transplant. 2014;20:1530–6.
Knols RH, de Bruin ED, Uebelhart D, Aufdemkampe G, Schanz U, Stenner-Liewen F, et al. Effects of an outpatient physical exercise program on hematopoietic stem-cell transplantation recipients: a randomized clinical trial. Bone Marrow Transplant. 2011;46:1245–55.
Persoon S, Kersten MJ, van der Weiden K, Buffart LM, Nollet F, Brug J, et al. Effects of exercise in patients treated with stem cell transplantation for a hematologic malignancy: a systematic review and meta-analysis. Cancer Treat Rev. 2013;39:682–90.
Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am. 1984;9:222–6.
Acknowledgements
We thank all the physical trainers at our institute who offered physical training and collected physical function data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Hayakawa, J., Miyamura, D., Kimura, Si. et al. Negative impact of chronic graft-versus-host disease and glucocorticoid on the recovery of physical function after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transplant 54, 994–1003 (2019). https://doi.org/10.1038/s41409-018-0365-4
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41409-018-0365-4
This article is cited by
-
Post-transplant changes in physical functioning and quality of life in patients undergoing two allogeneic hematopoietic stem cell transplants
International Journal of Hematology (2025)
-
Graft-Versus-Host Disease: an Update on Functional Implications and Rehabilitation Interventions
Current Oncology Reports (2023)
-
Psychological and physical function in allogeneic hematopoietic cell transplant survivors with chronic graft-versus-host disease
Journal of Cancer Survivorship (2023)
-
Changes in the health-related quality of life and social reintegration status after lung transplantation following hematopoietic stem cell transplantation
Supportive Care in Cancer (2022)
-
Functional capacity, pulmonary function, and quality of life in hematopoietic stem cell transplantation survivors
Supportive Care in Cancer (2021)