Abstract
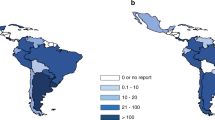
Hematopoietic cells transplants are technically complex and expensive imposing a huge burden on health care systems, especially those in developing countries and regions. In 2017 > 4500 transplants were done in 13 Latin American countries with established transplant programmes. We interrogated data on transplant rate, cost, funding source, hospital type, Gini coefficient and the United Nations Development Programme Inequality-Adjusted Human Development Index to determine co-variates associated with transplant development. Transplant rates varied almost 30-fold between the 13 countries from 345 in Uruguay to 12 in Venezuela with a regional transplant rate 7–8-fold lower compared with the US and EU. We found significant correlations between higher transplant cost, public funding, transplants in private hospitals with transplant rate. Low cost per transplant regardless of payor and transplants done in public hospitals were associated with low transplant rates. In contrast, high cost per transplant funded by the government and transplants done in private hospitals were associated with high transplant rates. Surprisingly, we found transplant rates were higher when transplants cost more, when they were done in private for-profit hospitals and payed for with public funds. These data give insights how to increase transplant rates in Latin America and other developing regions.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Ferreira E, Dulley FL, Morsoletto F, Pasquini R. Bone marrow transplantation in Brazil. Hum Immunol. 1985;14:324–32.
Khera N, Zeliadt S, Lee S. Economics of bone marrow transplantation. Blood. 2012;120:1545–51.
Broder M, Quock T, Chang E, Reddy S, Agarwal- Hashmi R, Arai S, et al. The cost of hematopoietic stem-cell transplantation in the United States. Am Health Drug Benefits. 2017;10:366–74.
Stranges E, Russo CA, Friedman B. Procedures with thE Most Rapidly Increasing Hospital Costs, 2004-7. Statistical Brief #82. US: Agency for Healthcare Research and Quality; 2006.
Jaimovich G, Martinez Rolon J, Baldomero H, Rivas M, Hanesman I, Bouzas L, et al. Latin America: the next region for haematopoietic transplant progress. Bone Marrow Transplant. 2017;52:671–7.
Gale R, Seber A, Bomfin C, Pasquini M. Haematopoietic cell transplants in Latin America. Bone Marrow Transplant. 2016;51:898–905.
Gratwohl A, Baldomero H, Schwendener A Gratwohl M, Apperley J, Frauendorfer K, et al. The EBMT activity survey 2008: impact of team size, team density and new trends. Bone Marrow Transplant. 2011;46:174–91.
Ortiz I, Cummins M. (PDF). Global Inequality: Beyond the bottom Billion. A Rapid Review of Income Distribution in 141 Countries. April 2011 UNICEF POLICY AND PRACTICE .UNICEF.
Báscolo E, Houghton N, Del Riego A. Lógicas de transformación de los sistemas de salud en América Latina y resultado en acceso y cobertura de salud (Types of health systems reforms in Latin America and results in health access and coverage). Rev Panam Salud Publica. 2018;42:e126 https://doi.org/10.26633/RPSP.2018.126.
Matus-López M. Thinking about long-term care policies for Latin America. Salud Colectiva. 2015;11:485–96. https://doi.org/10.18294/sc.2015.785.
Figueras J, Musgrove P, Carrin G, Duran A. Challenges to Latin-American health systems: what can be learned from the European experience? Gac Sanit. 2002;16:5–17.
Becerril-Montekio V, Belló M. Sistema De Salud De Argentina (The Health System of Argentina). Salud Pública de México. 2011;53:s96–s108.
Allen DM. Mean square error of prediction as a criterion for selecting variables. Technometrics. 1971;13:469–75.
Alves Sidney L, de Matos Lopes R, Gentilli L. Public and private in a high complexity medical procedure. Salus J Health Sci. 2016;3:87–90.
Seber A. The cost of hematopoietic stem cell transplantation in the real world. Hematology. 2012;17 sup1:s208–s211.
Jaime-Pérez J, Heredia-Salazar A, Cantú-Rodríguez O, Gutiérrez-Aguirre H, Villarreal-Villarreal C, Mancías-Guerra C, et al. Cost structure and clinical outcome of a stem cell transplantation program in a developing country: the experience in northeast Mexico. Oncologist 2015;20:386–92.
Gale RP, Lazarus HM. Liaisons Dangereuses? new drugs, physicians and the drug industry. Bone Marrow Transplant. 2021;56:299–302. https://doi.org/10.1038/s41409-020-0988-0.
Acknowledgements
Hellen Baldomero (WBMT) shared unpublished data. Profs. Navneet Majhail (Cleveland Clinic) and Marcelo Pasquini (CIBMTR) kindly reviewed the typescript. RPG acknowledges support from the National Institute of Health Research (NIHR) Biomedical Research Centre funding scheme. An overview of the conclusions of this study but not the supporting data was previously published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
RPG is a Consultant to BeiGene Ltd., CStone Pharmaceuticals and Kite Pharmma; a Consultant toFusion Pharma LLC, LaJolla NanoMedical Inc. and Mingsight Parmaceuticals Inc.; an Advisory Board member for Antegene Biotech LLC and StemRad Ltd; Medical Director at FFF Enterprises Inc; Partner in AZACA Inc; and a member of the Board of Directorsof the Russian Foundation for Cancer Research Support.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Jaimovich, G., Gale, R.P., Hanesman, I. et al. The paradox of haematopoietic cell transplant in Latin America. Bone Marrow Transplant 56, 2382–2388 (2021). https://doi.org/10.1038/s41409-021-01321-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-021-01321-x
This article is cited by
-
Results of the Latin American Bone Marrow Transplantation Society (LABMT) activity survey 2019-2022: the impact of the COVID-19 pandemic and the increase in related haploidentical donors
Bone Marrow Transplantation (2025)
-
Understanding factors limiting hematopoietic cell transplantation for acute myeloid leukemia patients in Mexico: a comprehensive analysis
Annals of Hematology (2024)
-
Increasing access to hematopoietic cell transplantation in Latin America: results of the 2018 LABMT activity survey and trends since 2012
Bone Marrow Transplantation (2022)