Abstract
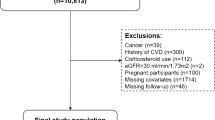
Patients with chronic graft-versus-host disease (cGVHD) are at heightened risk for components of metabolic syndrome (MetS), yet the prevalence and impact of MetS in the cGVHD patient population remain unknown. Adult patients (n = 229) with cGVHD enrolled in the cross-sectional NIH cGVHD Natural History Study (NCT00092235) were evaluated for MetS at enrollment and for variables associated with MetS. A majority (54.1%, 124/229) of the cohort met the diagnostic criteria for MetS. Patients with higher body mass index and lower performance status scores were more likely to have MetS (P < 0.0001; P = 0.026; respectively). Higher circulating erythrocyte sedimentation rate, C-reactive protein, and creatinine concentrations, along with lower estimated glomerular filtration rate, were associated with MetS (P < 0.001; P < 0.004; P = 0.02; P = 0.002; respectively). Patients with MetS compared to patients without MetS had no statistical differences in survival or NRM (5-year OS: 64% [95% CI: 54.8–71.8%] vs. 75.1% [95% CI: 65.6–82.3%]; respectively; overall P = 0.20; 5-year NRM: 21.7% [95% CI: 13.6–30.9%] vs. 10.1% [95% CI: 4.4–18.7%]; respectively; overall P = 0.12). Additionally, there was no difference in cGVHD severity between the two groups. Given the high prevalence of MetS in this cohort, clinicians should screen for its presence before it develops into comorbidities that complicate the course of cGVHD treatment.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Alberti KG, Zimmet P, Shaw J, Group IDFETFC. The metabolic syndrome-a new worldwide definition. Lancet. 2005;366:1059–62.
Expert Panel on Detection E, Treatment of High Blood Cholesterol in A. Executive summary of the third report of The National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001;285:2486–97.
Samson SL, Garber AJ. Metabolic syndrome. Endocrinol Metab Clin North Am. 2014;43:1–23.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–52.
Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–9.
Hirode G, Wong RJ. Trends in the prevalence of metabolic syndrome in the United States, 2011-2016. JAMA. 2020;323:2526–8.
Liang XP, Or CY, Tsoi MF, Cheung CL, Cheung BMY, Pharmacology DOC, et al. Prevalence of metabolic syndrome in the United States National Health and Nutrition Examination Survey (nhanes) 2011–2018. Eur Heart J. 2021;42:2420.
Moore JX, Chaudhary N, Akinyemiju T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988-2012. Prev Chronic Dis. 2017;14:E24.
Sherling DH, Perumareddi P, Hennekens CH. Metabolic syndrome. J Cardiovasc Pharm Ther. 2017;22:365–7.
Noubiap JJ, Nansseu JR, Lontchi-Yimagou E, Nkeck JR, Nyaga UF, Ngouo AT, et al. Geographic distribution of metabolic syndrome and its components in the general adult population: a meta-analysis of global data from 28 million individuals. Diabetes Res Clin Pract. 2022;188:109924.
Chew NWS, Ng CH, Tan DJH, Kong G, Lin C, Chin YH, et al. The global burden of metabolic disease: data from 2000 to 2019. Cell Metab 2023;35:414–28.e3.
Dalla Via V, Halter JP, Gerull S, Arranto C, Tichelli A, Heim D, et al. New-onset post-transplant diabetes and therapy in long-term survivors after allogeneic hematopoietic stem cell transplantation. Vivo. 2020;34:3545–9.
Griffith ML, Jagasia M, Jagasia SM. Diabetes mellitus after hematopoietic stem cell transplantation. Endocr Pract. 2010;16:699–706.
Annaloro C, Usardi P, Airaghi L, Giunta V, Forti S, Orsatti A, et al. Prevalence of metabolic syndrome in long-term survivors of hematopoietic stem cell transplantation. Bone Marrow Transpl. 2008;41:797–804.
Li C, Liu P, Liu L, Zhang X, Yang P, Sheng H, et al. Metabolic syndrome in hematologic malignancies survivors: a meta-analysis. Med Oncol. 2015;32:422.
Majhail NS, Flowers ME, Ness KK, Jagasia M, Carpenter PA, Arora M, et al. High prevalence of metabolic syndrome after allogeneic hematopoietic cell transplantation. Bone Marrow Transpl. 2009;43:49–54.
Greenfield DM, Salooja N, Peczynski C, van der Werf S, Schoemans H, Hill K, et al. Metabolic syndrome and cardiovascular disease after haematopoietic cell transplantation (HCT) in adults: an EBMT cross-sectional non-interventional study. Bone Marrow Transpl. 2021;56:2820–5.
Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR, et al. Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med. 2012;367:1487–96.
Jagasia MH, Greinix HT, Arora M, Williams KM, Wolff D, Cowen EW, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 diagnosis and staging working group report. Biol Blood Marrow Transpl. 2015;21:389–401.e1.
Medina G, Vera-Lastra O, Peralta-Amaro AL, Jimenez-Arellano MP, Saavedra MA, Cruz-Dominguez MP, et al. Metabolic syndrome, autoimmunity and rheumatic diseases. Pharm Res. 2018;133:277–88.
Ruscitti P, Cipriani P, Masedu F, Romano S, Berardicurti O, Liakouli V, et al. Increased cardiovascular events and subclinical atherosclerosis in rheumatoid arthritis patients: 1 year prospective single centre study. PLoS One. 2017;12:e0170108.
Paschos P, Paletas K. Non alcoholic fatty liver disease and metabolic syndrome. Hippokratia. 2009;13:9–19.
Maung K, Ramalingam S, Chaudhry M, Ren Y, Jung SH, Romero K, et al. Pre-transplant hepatic steatosis (fatty liver) is associated with chronic graft-vs-host disease but not mortality. PLoS One. 2020;15:e0238824.
Filipovich AH, Weisdorf D, Pavletic S, Socie G, Wingard JR, Lee SJ, et al. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: I. Diagnosis and staging working group report. Biol Blood Marrow Transpl. 2005;11:945–56.
Ghazanfari Z, Haghdoost AA, Alizadeh SM, Atapour J, Zolala F. A comparison of HbA1c and fasting blood sugar tests in general population. Int J Prev Med. 2010;1:187–94.
Guo F, Moellering DR, Garvey WT. Use of HbA1c for diagnoses of diabetes and prediabetes: comparison with diagnoses based on fasting and 2-hr glucose values and effects of gender, race, and age. Metab Syndr Relat Disord. 2014;12:258–68.
Nam HK, Cho WK, Kim JH, Rhie YJ, Chung S, Lee KH, et al. HbA1c cutoff for prediabetes and diabetes based on oral glucose tolerance test in obese children and adolescents. J Korean Med Sci. 2018;33:e93.
Olson DE, Rhee MK, Herrick K, Ziemer DC, Twombly JG, Phillips LS. Screening for diabetes and pre-diabetes with proposed A1C-based diagnostic criteria. Diabetes Care. 2010;33:2184–9.
Agresti A Categorical data analysis: John Wiley & Sons; 2012.
Mehta CR, Patel NR. A network algorithm for performing fisher’s exact test in r × c contingency tables. J Am Stat Assoc. 1983;78:427–34.
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706.
Baird K, Steinberg SM, Grkovic L, Pulanic D, Cowen EW, Mitchell SA, et al. National Institutes of Health chronic graft-versus-host disease staging in severely affected patients: organ and global scoring correlate with established indicators of disease severity and prognosis. Biol Blood Marrow Transpl. 2013;19:632–9.
Grkovic L, Baird K, Steinberg SM, Williams KM, Pulanic D, Cowen EW, et al. Clinical laboratory markers of inflammation as determinants of chronic graft-versus-host disease activity and NIH global severity. Leukemia. 2012;26:633–43.
Pavletic SZ, Smith LM, Bishop MR, Lynch JC, Tarantolo SR, Vose JM, et al. Prognostic factors of chronic graft-versus-host disease after allogeneic blood stem-cell transplantation. Am J Hematol. 2005;78:265–74.
Kitko CL, White ES, Baird K. Fibrotic and sclerotic manifestations of chronic graft-versus-host disease. Biol Blood Marrow Transpl. 2012;18:S46–52.
Johansen S, Blomberg B, Vo AK, Wendelbo O, Reikvam H. Weight gain during treatment course of allogenic hematopoietic stem cell transplantation in patients with hematological malignancies affects treatment outcome. Cytotherapy. 2022;24:1190–4.
López-Vilella R, Sánchez-Lázaro IJ, Martínez-Dolz L, Almenar-Bonet L, Marqués-Sulé E, Melero-Ferrer J, et al. Incidence of development of obesity after heart transplantation according to the calcineurin inhibitor. Transplant Proc. 2015;47:127–9.
Fuhrmann A, Lopes PC, Sereno J, Pedro J, Espinoza DO, Pereira MJ, et al. Molecular mechanisms underlying the effects of cyclosporin A and sirolimus on glucose and lipid metabolism in liver, skeletal muscle and adipose tissue in an in vivo rat model. Biochem Pharmacol. 2014;88:216–28.
Tokodai K, Amada N, Kikuchi H, Haga I, Takayama T, Nakamura A. Body fat percentage as a marker of new-onset diabetes mellitus after kidney transplantation. Transplant Proc. 2013;45:1544–7.
Sahinoz M, Luther JM, Mashayekhi M, Jung DK, Ikizler TA, Engelhardt BG. Hematologic malignancies magnify the effect of body mass index on insulin resistance in cancer survivors. Blood Adv. 2022;6:1981–90.
Asslan MA, Elsheikh E, Taha A, Abdelraouf YM, Kabbash I, Baker K, et al. High Body Mass Index (BMI) Is Associated with Lower Survival and Increased Chronic GVHD after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2019;25:S321–S2.
Doney K, McMillen K, Buono L, Deeg HJ, Gooley T. Impact of body mass index on outcomes of hematopoietic stem cell transplantation in adults. Biol Blood Marrow Transpl. 2019;25:613–20.
Nakasone H, Binh PN, Yamazaki R, Tanaka Y, Sakamoto K, Ashizawa M, et al. Association between serum high-molecular-weight adiponectin level and the severity of chronic graft-versus-host disease in allogeneic stem cell transplantation recipients. Blood. 2011;117:3469–72.
Voshtina E, Szabo A, Hamadani M, Fenske TS, D’Souza A, Chhabra S, et al. Impact of obesity on clinical outcomes of elderly patients undergoing allogeneic hematopoietic cell transplantation for myeloid malignancies. Biol Blood Marrow Transpl. 2019;25:e33–e8.
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–16.
Acknowledgements
The authors thank the patients and families for their participation in the NIH cGVHD Natural History Study. This research was supported [in part] by the Intramural Research Program of the NIH, Center for Cancer Research, the National Cancer Institute, the Clinical Center, the National Eye Institute, the National Institute for Dental and Craniofacial Research, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. The views expressed are not representative of the official views of the NIH or the US Government.
Author information
Authors and Affiliations
Contributions
ATZ: conceptualization, investigation, writing; FP: conceptualization, data curation and methodology; SMS: statistical analysis; NGH: conceptualization; ED: conceptualization; AM: conceptualization; SZP: conceptualization, investigation, supervision; all authors: review, editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhao, A.T., Pirsl, F., Steinberg, S.M. et al. Metabolic syndrome prevalence and impact on outcomes in patients with chronic graft-versus-host disease. Bone Marrow Transplant 58, 1377–1383 (2023). https://doi.org/10.1038/s41409-023-02097-y
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41409-023-02097-y