Abstract
Routine genetic profiling of acute myeloid leukemia (AML) at initial diagnosis has allowed subgroup specific prognostication, drug development, and clinical management strategies. The optimal approach for treatment response assessment for AML subgroups has not yet however been determined. A nationwide cohort of 257 adult patients in first remission (CR1) from AML associated with an IDH2 mutation (IDH2m) undergoing allogeneic transplant during the period 2013–2019 in the United States had rates of relapse and survival three years after transplantation of 24% and 71%, respectively. Pre-transplant clinical flow cytometry assessment was not useful in stratifying patients based on risk of post-transplant relapse or death. DNA-sequencing was performed on CR1 blood collected within 100 days before transplant. Persistent detection of IDH2m was common (51%) and associated with increased relapse and death compared to testing negative. Co-mutation at initial diagnosis with mutated NPM1 and/or FLT3-ITD was common in this cohort (41%) and use of these validated MRD markers provided superior stratification compared to IDH2m testing. Patients testing negative for IDH2m prior to transplant had low relapse-related death, regardless of conditioning intensity. Post-transplant relapse rates for those with persistently detectable IDH2m in pre-transplant remission were lower after the FDA approval of enasidenib in August 2017.
Similar content being viewed by others
Introduction
Acute myeloid leukemia (AML) is a type of rare but fatal blood cancer with around 20,000 new cases in the United States per year and an overall survival (OS) of 32% [1]. Mutational sub-classification of AML has created opportunities for specific prognostication, management, and development of targeted therapies [2,3,4]. Mutations in isocitrate dehydrogenase (IDH) genes are commonly observed in patients with AML, with IDH2 mutations detected at around 10–15% of all patients at AML diagnosis [5, 6]. Two specific IDH2 mutations, R140 and R172, compose around 80% and 20% of all IDH2-mutated cases, respectively [7]. Enasidenib, a targeted inhibitor of IDH2 mutations, was approved by the United States Food and Drug Administration to treat relapsed or refractory AML in August 2017 and is under study for other indications [8,9,10,11]. Allogeneic hematopoietic cell transplant (alloHCT) is an important, potentially curative, therapy for many patients with IDH2 mutated AML.
Measurable residual disease (MRD) test positivity in patients with AML during first complete remission (CR1) is associated with adverse clinical outcomes after alloHCT [12,13,14,15,16,17,18,19,20,21,22,23]. While a variety of AML MRD testing methods are possible, a molecular approach is typically preferred when both a validated target and test are available [12, 24,25,26]. The most common AML-specific somatic mutations, mutated NPM1 and FLT3 internal tandem duplication (ITD), are well-validated molecular targets for AML MRD testing [17, 27,28,29,30,31]. While other mutations are commonly detected at initial diagnosis, the prognostic significance of detecting individual, or combinations of, AML-associated mutations in remission have not been fully determined. Selecting and validating additional targets for molecular MRD monitoring will assist relapse prediction and facilitate early intervention, especially for disease subgroups with targeted therapies available [32,33,34,35,36,37]. While MRD in IDH-mutated AML has been studied previously, cohort sample size has limited conclusions [6, 38, 39], and large studies examining the significance of IDH2 as a potential AML MRD target are of particular interest due to the possibility of targeted clinical intervention.
The Pre-MEASURE project was designed to assess, in a nation-wide retrospective cohort of adults with AML in CR1 prior to first alloHCT, the association of pre-transplant remission blood testing by DNA-sequencing with post-transplant clinical outcomes. We present here the findings associated with persistent IDH2 mutation (IDH2m) detection.
Materials and methods
Study cohort
Patients 18 years or older with AML reported as associated with an IDH2m at diagnosis, who achieved CR1 and underwent alloHCT at one of 112 sites from the Center for International Blood and Marrow Transplant Research (CIBMTR) from 2013–2019, registered to participate in the CIBMTR database (NCT01166009) and repository (NCT04920474) protocols, and with a remission blood sample collected within 100 days of alloHCT were included in the study (median: 8.5 days, range 0–71). All patients gave written informed consent in accordance with the Declaration of Helsinki. Clinical outcome data were provided by CIBMTR including time to death or censoring, time to relapse, and graft-versus-host disease (GvHD, acute or chronic) when available. Other baseline characteristics were also extracted from the database including age, sex, race, ethnicity, hematopoietic cell transplant specific comorbidity (HCT-CI), Karnofsky performance status (KPS), secondary AML, European LeukemiaNet (ELN) 2017 risk group, baseline IDH2 mutational status, conditioning regimen, graft type, donor group, anti-thymocyte globulin (ATG) usage, site reported flow cytometry MRD status, and month/year transplanted.
Residual variant detection by next generation sequencing
Genomic DNA was extracted from remission blood obtained from the CIBMTR repository and sequenced as described previously [17]. In short, ultrasensitive error-corrected next generation sequencing (NGS) targeting mutational hotspot regions of the IDH2, NPM1, and FLT3 genes was performed utilizing an automated workflow with pre- and post-PCR separation. The assay was validated to detect IDH2 variants down to at least 0.1% variant allele fraction (VAF) by performing serial dilutions of AML patient DNA containing known IDH2 R140Q, R172K, or R132H mutations into normal DNA at a range of 5% to 0.005%. NPM1 and FLT3-ITD variants were called down to 0.01% VAF. NGS libraries were sequencing on a NovaSeq 6000 (Illumina) with unique dual indices. Bioinformatic pipelines were used to perform error-corrected variant calling followed by filtering to identify residual disease. Raw FASTQ files are available at the NCBI Sequence Read Archive (SRA) (Accession: PRJNA834073 and PRJNA1051602).
Digital droplet PCR (ddPCR)
A subset of 127 IDH2 variants identified by NGS were orthogonally validated using ddPCR on the Bio-Rad QX200 or QX600 system as described previously [17].
Statistical analysis
The primary outcomes were OS and cumulative incidence of relapse with non-relapse related mortality (NRM) as a competing risk. The day of transplant was considered as time 0, and the median follow-up time was calculated for censored patients. Kaplan–Meier (KM) estimation and log rank tests were used to calculate OS and relapse-free survival endpoints. Cox proportional hazards models were fitted, with forward selection by analysis of variance or Lasso penalty for variable selection, and the proportional hazards assumptions were validated. Fine-Gray regression models were used to examine the cumulative incidence of relapse with NRM as a competing risk, and Bayesian information criterion (BIC) was used for model selection. Potential interactions between NGS IDH2 MRD status and clinical characteristics were tested. KM curves were visualized up to 3 years based on the number of patients at risk, but the p-values included were obtained using full data. Two-sided p-values less than or equal 0.05 were considered as statistically significant. R version 4.3.0 was used to perform statistical analysis, generate figures and tables.
Results
Clinical characteristics and post-transplant clinical outcomes
A total of 257 adults with IDH2-mutated AML undergoing alloHCT in CR1 at a CIBMTR reporting site between 2013 and 2019 were included in this study (Table 1). The median age was 60.1 (range 19.8–79.3), 84% were Caucasian, 50% were female, 57% had a Karnofsky performance score of 90 or above, and 48% had an HCT-CI comorbidity index of 3 or greater. In addition to IDH2 mutations in all patients, NPM1 and/or FLT3-ITD mutations were reported at initial diagnosis in 41%. Transplants were from peripheral blood 75% of the time, 49% had myeloablative conditioning, and 60% were from matched unrelated donors.
Overall, the 1-year and 3-year cumulative incidence of relapse in this cohort was estimated as 16% and 24%, respectively (Fig. 1a, Supplementary Fig. 1). Of 57 relapses recorded, 41 (72%) occurred within 12 months following transplantation. For all baseline characteristics studied (Table 1), using univariable competing risk regression considering NRM as the competing risk event, only cord blood compared to peripheral blood as a graft type (HR: 2.3, 95% CI 1.2–4.5; Supplementary Fig. 2A) was related with higher relapse risk.
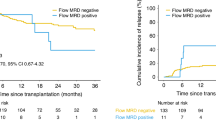
Cumulative incidence of relapse (left) and overall survival (right) are shown for IDH2 mutated patients (a) for the entire cohort (b) based on the presence (Flow MRDpos) or absence (Flow MRDneg) of reported clinical flow cytometry measurable residual disease (MRD), and (c) based on the presence (IDH2 NGS MRDpos) or absence (IDH2 NGS MRD neg) of residual IDH2 variants by next generation sequencing (NGS) MRD assay.
Overall, the 1-year and 3-year OS in this cohort were estimated as 81% and 71%, respectively (Fig. 1a). Median follow-up time among censored patients was 25 months. Two baseline characteristics identified by univariable Cox regression analysis as associated with differences in OS were HCT-CI (3+ vs. 0, HR: 2.8, 95% CI: 1.3–5.9) and AML group (transformed from myelodysplastic syndrome/myeloproliferative neoplasm vs. de novo HR: 2.1, 95% CI: 1.1–4.3; Supplementary Fig. 2B).
Pre-transplant flow cytometry and residual IDH2m detection
Flow cytometry is commonly performed for patients with AML in remission prior to transplant as a test of MRD to estimate post-transplant relapse risk [12], although the clinical utility of such testing as currently performed has been questioned [17, 40]. 247 of the 257 (96%) patients in this cohort had pre-transplant remission flow cytometry results reported to the CIBMTR registry, of which 25 (10%) tested positive. Testing positive by flow cytometry pre-transplant did not predict any differences in relapse or OS compared with those testing negative (Fig. 1a).
Testing for IDH2m persistence for patients with AML in remission prior to transplant is not routinely performed clinically. A custom error-corrected NGS assay was validated to detect IDH2 mutations down to a variant allele fraction (VAF) of at least 0.1% (Supplementary Fig. 3A). NGS analysis detected residual IDH2m in CR1 pre-transplant blood samples from 130 patients (51%) with VAFs ranging from 0.05 to 56% (median: 3%; Supplementary Fig. 3, Supplementary Table 1). Those with IDH2m detected (IDH2 NGS MRDpos) had increased relapse (3 yrs: 29% vs. 18%, +11%, 95% CI: 0.2% to 22%; overall p = 0.03), decreased OS (3 yrs: 58% vs. 83%, −25%, 95% CI: −13% to −38%; overall p < 0.001), and decreased relapse-free survival (RFS 3 yrs: 53% vs. 70%, −17%, 95% CI: −4% to −30%; overall p = 0.002) compared to those testing negative (IDH2 NGS MRDneg, Fig. 1c). The OS for IDH2 NGS MRDneg patients was estimated to be 83% (95% CI: 75% to 89%, p < 0.001) at 3 years and only 6 of the 21 deaths in this group were relapse related.
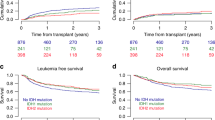
Association of age, residual IDH2m burden and type with clinical outcome
To study the association of IDH2m detection in pre-transplant CR1 and clinical outcomes in younger and older patients, subgroups were created by using 60 years of age as a cutoff (≥60 vs. <60). For both age groups, decreased OS was observed for those testing positive for IDH2m compared to those testing negative (<60 yrs, 3 yrs: 62% vs. 90%, −28%, 95% CI: −12% to −43%, overall p < 0.001; ≥60 yrs, 3 yrs: 54% vs. 73%, −19%, 95% CI: −1% to −40%, overall p = 0.04; Fig. 2a, b; Supplementary Fig. 4). OS for the younger group testing negative for persistent IDH2m was 90% (95% CI: 81% to 95%, p < 0.001); among 9 patients who died in this group only 3 experienced relapse. Older patients had an increased rate of relapse when testing positive for persistent IDH2m compared to those testing negative (3 yrs: 33% vs. 12%, +21%, 95% CI: 6% to 36%, overall p = 0.007). Interestingly, the level of IDH2m persistence was significantly higher in older versus younger patients (median VAFs: 5.4% vs. 1.4%, ≥60 yrs vs. <60 yrs, p = 0.01). To examine a potential dose effect of IDH2m persistence, patients were divided into two VAF subgroups with 2.5% as the cutoff, but the risk of relapse was not significantly different between the VAF groups (Fig. 2c). Among patients with residual IDH2m detected, 13% (n = 17) had R172 variants and the remaining had R140 variants. The type of residual IDH2m did not further stratify the risks of clinical outcomes (Fig. 2d).
Cumulative incidence of relapse (left) and overall survival (right) are shown for IDH2 mutated patients by the presence (IDH2 NGS MRDpos) or absence (IDH2 NGS MRDneg) of residual IDH2 variants and by (a) age group below 60 years old, (b) age group 60 years or above, (c) different variant allele fraction (VAF) groups, and (d) by IDH2 mutation type.
Co-occurrence of mutated IDH2 with mutated NPM1 and FLT3-ITD
As IDH2 mutated AML often also has mutations in NPM1 and/or FLT3-ITD [2, 4], the cohort was separated into those with (n = 106, 41%) or without (n = 151, 59%) either of these two mutations reported at initial diagnosis. In the IDH2 mutated patients who did not also have mutated NPM1 and/or FLT3-ITD at baseline, IDH2m were commonly detected in pre-transplant remission blood (n = 80, 53%) and was associated with increased relapse and decreased OS compared with testing negative (relapse 3 yrs: 31% vs. 12%, +19%, 95% CI: 6% to 32%, overall p = 0.01; OS 3 yrs: 56% vs. 79%, −23%, 95% CI: −6% to −40%, overall p = 0.005; Fig. 3, Supplementary Fig. 5).
In contrast, for patients known to also have mutations in NPM1 and/or FLT3-ITD at initial diagnosis (n = 106), detection of persistent IDH2m pre-transplant was also common (N = 50, 47%) but was prognostic only for OS and not relapse (Fig. 4a, Supplementary Fig. 6). Since the persistence of NPM1 and/or FLT3-ITD variants in pre-transplant CR1 blood has already been shown to be strongly associated with worse post-transplant clinical outcomes [17], the utility of these markers was validated in this specific setting. As anticipated the detection of persistent NPM1 and/or FLT3-ITD variants (n = 20, 19%) was strongly associated with increased relapse, while those with only residual IDH2m detected (n = 35, 33%) had similar relapse risk as those testing negative (3 yrs: 65% vs. 12% vs. 16%; overall p < 0.001; p < 0.001 for NPM1/FLT3-ITD vs. negative, p = 0.8 for IDH2m only vs. negative; Fig. 4b). Both residual mutation positive groups had inferior OS compared to the negative group while patients with residual NPM1/FLT3-ITD had the worst estimated OS (3 yrs: 41% vs. 71% vs. 94%; overall p < 0.001). None of the patients testing negative (n = 51, 48%) experienced relapse-related mortality among the 4 reported death events.
Cumulative incidence of relapse on the left and overall survival on the right for patients based on (a) the presence (IDH2 NGS MRDpos) or absence (IDH2 NGS MRDneg) of residual IDH2 variants or (b) the presence of residual NPM1 and/or FLT3-ITD variants (NPM1/FLT3-ITD NGS MRDpos), the presence of only residual IDH2 variants (IDH2 NGS MRDpos), or the absence of residual variants (NGS MRDneg).
Modifying effects of other clinical characteristics on residual IDH2m detection
Given evidence that the intensity of the conditioning regimen used prior to transplant can impact clinical outcomes in MRD positive patients [22], we next examined the modifying effect of conditioning intensity and IDH2m persistence. Patients were grouped into low intensity (reduced intensity conditioning (RIC) and nonmyeloablative (NMA)) and high intensity (RIC with melphalan and myeloablative conditioning (MAC)) regimens. When considering all patients, those with IDH2m persistence who received RIC/NMA had the highest rate of relapse (3 yrs: 35%, 95% CI: 20–51%) and lowest OS (3 yrs: 51%, 95% CI: 34–66%; Fig. 5a, Supplementary Fig. 7), but there was no statistically significant difference among the residual IDH2m patients based on treatment regimen. Conditioning intensity was not randomized in this retrospective observational study but was likely determined, at least in part, by judgements regarding patient performance status and comorbidity. Age is an important factor, and as expected RIC/NMA was more frequently given to older patients (<60 yrs vs. ≥60 yrs: 11% vs. 42%, Chi-squared test p < 0.001). While there were few cases of patients <60 years old with persistent IDH2m who received RIC/NMA, when looking at those ≥60 years, higher rates of relapse were observed in patients testing IDH2m positive when given RIC/NMA compared to those testing negative (1 yr: 29% vs. 0, +29%, 95% CI: +13.3% to +43.8%, p < 0.001; Fig. 5b).
Cumulative incidence of relapse on the left and overall survival on the right for (a) the entire cohort of IDH2-mutated AML patients, and (b) those ≥60 years of age based on the presence (IDH2 NGS MRDpos) or absence (IDH2 NGS MRDneg) of residual IDH2 variants and conditioning intensity received. MAC myeloablative conditioning, Mel melphalan, RIC reduced intensity conditioning, NMA nonmyeloablative conditioning.
For the full cohort, multivariable Cox regression analysis for OS indicated that patients with persistent IDH2m had a higher risk of relapse compared to those testing negative (HR: 2.5, 95% CI: 1.5–4.2, p < 0.001) after adjusting for other variables of interest, which also had significant differences in OS risk including hematopoietic cell transplantation-comorbidity index and age group (Table 2). Residual IDH2m remained prognostic in relapse using competing risk regression (IDH2 NGS MRDpos vs. IDH2 NGS MRDneg, HR: 2.1, 95% CI: 1.4–5.7, p = 0.003) when considering graft type and IDH1 baseline status.
The prognostic significance for persistent IDH2m remained when patients did not have NPM1 and/or FLT3-ITD mutations at baseline (HR for OS: 2.5, 95% CI: 1.3–4.7; HR for relapse: 3.3, 95% CI: 1.5–7.2; Table 2) when including other clinically important characteristics in the regression model. For patients with NPM1 and/or FLT3-ITD mutations at baseline, residual NPM1 and/or FLT3-ITD variants was the most significant variable in predicting both OS and relapse outcomes (OS, HR: 10, 95% CI: 3.2–31.2, p < 0.001; relapse, HR: 21, 95% CI: 7–63, p < 0.001), while residual IDH2m was only significant for relapse (HR: 4.36, 95% CI: 1.4–13.7, p = 0.01), when adjusting for other covariates of interest (Table 2).
Since the IDH2 inhibitor enasidenib was approved by the FDA on August 1st of 2017, patients were divided into two subgroups with alloHCT date before (n = 44, 17%) or after (n = 213, 83%) the date of drug approval to examine the potential therapeutic impact. Although the patient numbers were not balanced between the two groups, the difference in rates of relapse between the residual IDH2m positive and negative groups was greater before the approval date versus after (before: 45% vs. 23%, after: 26% vs. 15%, overall p = 0.03; Fig. 6, Supplementary Fig. 8A). There was also a difference in NRM comparing those testing positive versus negative for residual IDH2m (before: 0 vs. 18%, after: 22% vs. 10%, overall p = 0.005), with 9/10 death events relapse related for patients in the IDH2m positive group transplanted before August 2017. The same patterns in clinical outcomes were observed when removing patients with baseline FLT3-ITD mutation (Supplementary Fig. 8B).
Cumulative incidence of relapse on the left and non-relapse related mortality (NRM) on the right for IDH2-mutated AML patients based on the date of transplant occurring before or after the approval date of enasidenib (August 2017) and the presence (IDH2 NGS MRDpos) or absence (IDH2 NGS MRDneg) of residual IDH2 variants.
Discussion
Presented here is the largest observational study of patients with IDH2-mutated AML examining the association between the detection of residual IDH2m in the blood during CR1 prior to the first alloHCT and post-transplant clinical outcomes. Around half of the patients examined had residual IDH2 mutations detected in the blood during CR1 using ultra-deep error-corrected NGS, which was associated with statistically significant increased rates of relapse and decreased OS. Patients without detectable persistence of IDH2m generally had very high survival after transplantation. Further exploratory subgroup and multivariable analyses showed interesting variations in clinical outcomes for patients given different conditioning intensity regimens and with various baseline or transplant-related characteristics, although are limited by subgroup cohort size, imbalance in age groups, and non-random conditioning intensity assignment. In addition, further study on the impact of additional baseline mutational characteristics and targeted inhibitor use was not possible in this large retrospective registry study.
Mutated NPM1 and FLT3-ITD are now well-validated AML MRD targets [17, 27,28,29,30,31], and this IDH2-mutated cohort was further studied by dividing into two subgroups based on whether they also had either of these two mutations reported at initial diagnosis. In patients with IDH2-mutated AML also co-mutated with either NPM1 and/or FLT3-ITD, the persistence of only IDH2m pre-transplant was not associated with increased relapse post-transplant. Persistence of NPM1 and/or FLT3-ITD variants was however very strongly associated with increased relapse and increased death after transplant and proves to be a superior marker to IDH2m in these patients.
In those patients diagnosed with IDH2m AML that was not co-mutated with either NPM1 and/or FLT3-ITD, persistent detection of IDH2m pre-transplant was common and associated with increased relapse and death after transplant.
The prognostic significance of persistent IDH2m pre-transplant was superior to reported clinical flow cytometry results but not as great as that reported in different patient subsets for other molecular AML MRD markers. Definitions based on patient age, VAF, or mutation type did not improve stratification for post-transplant relapse or survival outcomes.
While the primary intent of this study was to determine the ability of pre-transplant IDH2m MRD testing to predict post-transplant relapse, we observed in multiple analyses a trend for the persistence of IDH2m pre-transplant having a greater than expected effect on post-transplant survival relative to relapse rates. There are many potential explanations for this finding, ranging from differences in disease biology such that relapses from those with detectable pre-transplant disease were more likely to be fatal, to differences in pre- and post-transplant therapy (including off-label use of IDH2 inhibitor therapy), to the possibility that NRM is higher in those with persistent IDH2 mutated cells due to differences in immune status [41]. This hypothesis-generating observation is worthy of further study but is beyond the scope of this project.
In summary, persistence of IDH2 variants in the blood during first remission prior to first alloHCT is common and is associated with increased relapse and death post-transplant. Patients with AML co-mutated with either NPM1 or FLT3-ITD should be tested for MRD using mutated NPM1 or FLT3-ITD rather than IDH2 persistence.
Data availability
Sequencing data are available at the NCBI Sequence Read Archive (SRA) (Accession: PRJNA834073 and PRJNA1051602). Clinical data will be published by CIBMTR as a resource.
References
Sasaki K, Ravandi F, Kadia TM, DiNardo CD, Short NJ, Borthakur G, et al. De novo acute myeloid leukemia: A population-based study of outcome in the United States based on the Surveillance, Epidemiology, and End Results (SEER) database, 1980 to 2017. Cancer. 2021;127:2049–61. https://doi.org/10.1002/cncr.33458.
Tyner JW, Tognon CE, Bottomly D, Wilmot B, Kurtz SE, Savage SL, et al. Functional genomic landscape of acute myeloid leukaemia. Nature. 2018;562:526–31. https://doi.org/10.1038/s41586-018-0623-z.
Papaemmanuil E, Gerstung M, Bullinger L, Gaidzik VI, Paschka P, Roberts ND, et al. Genomic Classification and Prognosis in Acute Myeloid Leukemia. N Engl J Med. 2016;374:2209–21. https://doi.org/10.1056/NEJMoa1516192.
Cancer Genome Atlas Research N, Ley TJ, Miller C, Ding L, Raphael BJ, Mungall AJ, et al. Genomic and epigenomic landscapes of adult de novo acute myeloid leukemia. N Engl J Med. 2013;368:2059–74. https://doi.org/10.1056/NEJMoa1301689.
Metzeler KH, Herold T, Rothenberg-Thurley M, Amler S, Sauerland MC, Gorlich D, et al. Spectrum and prognostic relevance of driver gene mutations in acute myeloid leukemia. Blood. 2016;128:686–98. https://doi.org/10.1182/blood-2016-01-693879.
Ravindra N, Dillon LW, Gui G, Smith M, Gondek LP, Jones RJ, et al. Persistent IDH mutations are not associated with increased relapse or death in patients with IDH-mutated acute myeloid leukemia undergoing allogeneic hematopoietic cell transplant with post-transplant cyclophosphamide. Bone Marrow Transplant. 2024;59:428–30. https://doi.org/10.1038/s41409-023-02189-9.
Meggendorfer M, Cappelli LV, Walter W, Haferlach C, Kern W, Falini B, et al. IDH1R132, IDH2R140 and IDH2R172 in AML: different genetic landscapes correlate with outcome and may influence targeted treatment strategies. Leukemia. 2018;32:1249–53. https://doi.org/10.1038/s41375-018-0026-z.
Stein EM, DiNardo CD, Pollyea DA, Fathi AT, Roboz GJ, Altman JK, et al. Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood. 2017;130:722–31. https://doi.org/10.1182/blood-2017-04-779405.
Abou Dalle I, DiNardo CD. The role of enasidenib in the treatment of mutant IDH2 acute myeloid leukemia. Ther Adv Hematol. 2018;9:163–73. https://doi.org/10.1177/2040620718777467.
Pollyea DA, Tallman MS, de Botton S, Kantarjian HM, Collins R, Stein AS, et al. Enasidenib, an inhibitor of mutant IDH2 proteins, induces durable remissions in older patients with newly diagnosed acute myeloid leukemia. Leukemia. 2019;33:2575–84. https://doi.org/10.1038/s41375-019-0472-2.
Venugopal S, Takahashi K, Daver N, Maiti A, Borthakur G, Loghavi S, et al. Efficacy and safety of enasidenib and azacitidine combination in patients with IDH2 mutated acute myeloid leukemia and not eligible for intensive chemotherapy. Blood Cancer J. 2022;12:10. https://doi.org/10.1038/s41408-021-00604-2.
Heuser M, Freeman SD, Ossenkoppele GJ, Buccisano F, Hourigan CS, Ngai LL, et al. 2021 Update on MRD in acute myeloid leukemia: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2021;138:2753–67. https://doi.org/10.1182/blood.2021013626.
Hourigan CS. Achieving MRD negativity in AML: how important is this and how do we get there? Hematology Am Soc Hematol Educ Program. 2022;2022:9–14. https://doi.org/10.1182/hematology.2022000323.
Gui G, Hourigan CS. Measurable Residual Disease Assessment as a Surrogate Marker in New Drug Development in Acute Myeloid Leukemia. Cancer J. 2022;28:73–77. https://doi.org/10.1097/PPO.0000000000000572.
Wong ZC, Dillon LW, Hourigan CS. Measurable residual disease in patients undergoing allogeneic transplant for acute myeloid leukemia. Best Pract Res Clin Haematol. 2023;36:101468 https://doi.org/10.1016/j.beha.2023.101468.
Dillon LW, Higgins J, Nasif H, Othus M, Beppu L, Smith TH et al. Quantification of measurable residual disease using duplex sequencing in adults with acute myeloid leukemia. Haematologica. 2023;20230803; https://doi.org/10.3324/haematol.2023.283520.
Dillon LW, Gui G, Page KM, Ravindra N, Wong ZC, Andrew G, et al. DNA Sequencing to Detect Residual Disease in Adults With Acute Myeloid Leukemia Prior to Hematopoietic Cell Transplant. JAMA. 2023;329:745–55. https://doi.org/10.1001/jama.2023.1363.
Buckley SA, Wood BL, Othus M, Hourigan CS, Ustun C, Linden MA, et al. Minimal residual disease prior to allogeneic hematopoietic cell transplantation in acute myeloid leukemia: a meta-analysis. Haematologica. 2017;102:865–73. https://doi.org/10.3324/haematol.2016.159343.
Hourigan CS, Gale RP, Gormley NJ, Ossenkoppele GJ, Walter RB. Measurable residual disease testing in acute myeloid leukaemia. Leukemia. 2017;31:1482–90. https://doi.org/10.1038/leu.2017.113.
Short NJ, Zhou S, Fu C, Berry DA, Walter RB, Freeman SD, et al. Association of Measurable Residual Disease With Survival Outcomes in Patients With Acute Myeloid Leukemia: A Systematic Review and Meta-analysis. JAMA Oncol. 2020;6:1890–9. https://doi.org/10.1001/jamaoncol.2020.4600.
Short NJ, Fu C, Berry DA, Walter RB, Freeman SD, Hourigan CS, et al. Association of hematologic response and assay sensitivity on the prognostic impact of measurable residual disease in acute myeloid leukemia: a systematic review and meta-analysis. Leukemia. 2022;36:2817–26. https://doi.org/10.1038/s41375-022-01692-0.
Hourigan CS, Dillon LW, Gui G, Logan BR, Fei M, Ghannam J, et al. Impact of Conditioning Intensity of Allogeneic Transplantation for Acute Myeloid Leukemia With Genomic Evidence of Residual Disease. J Clin Oncol. 2020;38:1273–83. https://doi.org/10.1200/JCO.19.03011.
Othus M, Gale RP, Hourigan CS, Walter RB. Statistics and measurable residual disease (MRD) testing: uses and abuses in hematopoietic cell transplantation. Bone Marrow Transplant. 2020;55:843–50. https://doi.org/10.1038/s41409-019-0729-4.
Ravandi F, Cloos J, Buccisano F, Dillon R, Dohner K, Freeman SD, et al. Measurable residual disease monitoring in patients with acute myeloid leukemia treated with lower-intensity therapy: Roadmap from an ELN-DAVID expert panel. Am J Hematol. 2023. https://doi.org/10.1002/ajh.27087.
Schuurhuis GJ, Heuser M, Freeman S, Bene MC, Buccisano F, Cloos J, et al. Minimal/measurable residual disease in AML: a consensus document from the European LeukemiaNet MRD Working Party. Blood. 2018;131:1275–91. https://doi.org/10.1182/blood-2017-09-801498.
Roloff GW, Lai C, Hourigan CS, Dillon LW. Technical Advances in the Measurement of Residual Disease in Acute Myeloid Leukemia. J Clin Med. 2017;6:20170919; https://doi.org/10.3390/jcm6090087.
Grob T, Sanders MA, Vonk CM, Kavelaars FG, Rijken M, Hanekamp DW, et al. Prognostic Value of FLT3-Internal Tandem Duplication Residual Disease in Acute Myeloid Leukemia. J Clin Oncol. 2023;41:756–65. https://doi.org/10.1200/JCO.22.00715.
Loo S, Dillon R, Ivey A, Anstee NS, Othman J, Tiong IS, et al. Pretransplant FLT3-ITD MRD assessed by high-sensitivity PCR-NGS determines posttransplant clinical outcome. Blood. 2022;140:2407–11. https://doi.org/10.1182/blood.2022016567.
Gui G, Dillon LW, Hourigan CS. DNA Sequencing in Adults With Acute Myeloid Leukemia to Detect Residual Disease Prior to Hematopoietic Cell Transplant-Reply. JAMA. 2023;330:190–1. https://doi.org/10.1001/jama.2023.8653.
Dillon LW, Gui G, Ravindra N, Andrew G, Mukherjee D, Wong ZC, et al. Measurable Residual FLT3 Internal Tandem Duplication Before Allogeneic Transplant for Acute Myeloid Leukemia. JAMA Oncol. 2024;20240502; https://doi.org/10.1001/jamaoncol.2024.0985.
Levis MJ, Hamadani M, Logan B, Jones RJ, Singh AK, Litzow M, et al. Gilteritinib as Post-Transplant Maintenance for AML With Internal Tandem Duplication Mutation of FLT3. J Clin Oncol. 2024;42:1766–75. https://doi.org/10.1200/JCO.23.02474.
Ghannam J, Dillon LW, Hourigan CS. Next-generation sequencing for measurable residual disease detection in acute myeloid leukaemia. Br J Haematol. 2020;188:77–85. https://doi.org/10.1111/bjh.16362.
El Chaer F, Hourigan CS, Zeidan AM. How I treat AML incorporating the updated classifications and guidelines. Blood. 2023;141:2813–23. https://doi.org/10.1182/blood.2022017808.
Freeman SD, Hourigan CS. MRD evaluation of AML in clinical practice: are we there yet? Hematology Am Soc Hematol Educ Program. 2019;2019:557–69. https://doi.org/10.1182/hematology.2019000060.
Blachly JS, Walter RB, Hourigan CS. The present and future of measurable residual disease testing in acute myeloid leukemia. Haematologica. 2022;107:2810–22. https://doi.org/10.3324/haematol.2022.282034.
Blackmon AL, Hourigan CS. Test Then Erase? Current Status and Future Opportunities for Measurable Residual Disease Testing in Acute Myeloid Leukemia. Acta Haematol. 2024;147:133–46. https://doi.org/10.1159/000535463.
Hourigan CS, McCarthy P, de Lima M. Back to the future! The evolving role of maintenance therapy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20:154–63. https://doi.org/10.1016/j.bbmt.2013.11.017.
Bill M, Jentzsch M, Bischof L, Kohlschmidt J, Grimm J, Schmalbrock LK, et al. Impact of IDH1 and IDH2 mutation detection at diagnosis and in remission in patients with AML receiving allogeneic transplantation. Blood Adv. 2023;7:436–44. https://doi.org/10.1182/bloodadvances.2021005789.
Ok CY, Loghavi S, Sui D, Wei P, Kanagal-Shamanna R, Yin CC, et al. Persistent IDH1/2 mutations in remission can predict relapse in patients with acute myeloid leukemia. Haematologica. 2019;104:305–11. https://doi.org/10.3324/haematol.2018.191148.
Paiva B, Manrique I, Dimopoulos MA, Gay F, Min CK, Zweegman S, et al. MRD dynamics during maintenance for improved prognostication of 1280 patients with myeloma in the TOURMALINE-MM3 and -MM4 trials. Blood. 2023;141:579–91. https://doi.org/10.1182/blood.2022016782.
Hong LE, Wechalekar MD, Kutyna M, Small A, Lim K, Thompson-Peach C, et al. IDH-mutant myeloid neoplasms are associated with seronegative rheumatoid arthritis and innate immune activation. Blood. 2024;143:1873–7. https://doi.org/10.1182/blood.2023023593.
Acknowledgements
This study was previously presented on December 10, 2023, at the 2023 American Society of Hematology Annual Meeting. This work was supported by the Intramural Research Program of the National Heart, Lung, and Blood Institute, the National Institutes of Health Director’s Challenge Innovation Award, and the Foundation of the NIH AML MRD Biomarkers Consortium. Sequencing was performed in the NHLBI Intramural DNA Sequencing and Genomics Core. This work utilized the computational resources of the NIH HPC Biowulf cluster (http://hpc.nih.gov). The CIBMTR is a research collaboration between the Medical College of Wisconsin and the NMDP and is supported primarily by Public Health Service U24CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); 75R60222C00011 from the Health Resources and Services Administration (HRSA); and N00014-23-1-2057 and N00014-24-1-2057 from the Office of Naval Research. Support for the FNIH Biomarkers Consortium project MRD in AML (Measurable Residual Disease in Acute Myeloid Leukemia) was provided by AbbVie; Amgen; AstraZeneca; Genentech, a member of the Roche Group; Gilead Sciences, Inc.; GSK; Jazz Pharmaceuticals, Inc.; LGC Clinical Diagnostics, Inc.; Novartis; Syndax Pharmaceuticals, Inc.; Sysmex Inostics, Inc. In-kind donations of standards and methods materials and equipment to support the project were provided to the FNIH by AccuGenomics, Inc; Bio-Rad Laboratories, Inc.; Invivoscribe, Inc.; LGC Clinical Diagnostics, Inc.; Mission Bio; 10x Genomics, Inc.; Takeda Pharmaceuticals U.S.A., Inc.; Thermo Fisher Scientific Inc.; TwinStrand Biosciences, Inc.; Twist Bioscience Corporation. The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense, Health Resources and Services Administration (HRSA) or any other agency of the U.S. Government. Our co-author, colleague, and friend Kristin Page MD (June 7, 1974 - September 5, 2024) died during the review process. This paper is dedicated to her memory.
Funding
Open access funding provided by the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
GG, LD, CH designed the research. LD, NR, PH, GA, DM, ZW performed the experiments. GG, LD, KP, CH performed the clinical data checking. GG, SZ, CH made the statistical analysis plan and analyzed the data. GG and LD wrote the manuscript and prepared the figures. All authors reviewed the manuscript and provided suggestions. Hourigan: The National Heart, Lung, and Blood Institute receives research funding for the laboratory of Dr. Hourigan from the Foundation of the NIH AML MRD Biomarkers Consortium. Auletta: Advisory Committee: AscellaHealth and Takeda. El Chaer: Consultant: SPD Oncology, Amgen, Association of Community Cancer Centers; Clinical Trial Grant Support (PI) to the University of Virginia: Amgen, BMS, Celgene, SPD Oncology, Sanofi, Bristol Myers Squibb, FibroGen, PharmaEssentia, BioSight, MEI Pharma, Novartis, Arog pharmaceuticals; Travel grant: DAVA Oncology. E Chen: Consultant: Rigel Pharmaceuticals and AbbVie. Y Chen: Consultant: Incyte, Takeda, Astellas, Editas, Novo Nordisk, Pharmacosmos, Vor. Corner: Employment: Bio-Rad Laboratories. Jimenez Jimenez: Funding: Abbvie. De Lima: Advisory Board: Pfizer, Bristol Myers Squibb; Data Safety Monitoring Board: Novartis, Abbvie; Research Funding: Miltenyi Biotec. Litzow: Research support: Abbvie, Astellas, Amgen, Actinium, Pluristem, Sanofi; Speakers Bureau: Beigene, Amgen; Data Safety Monitoring Committee: Biosight. Kebriaei: Consultant: Pfizer, Jazz Pharmaceuticals
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Protected health information for research was collected and maintained in CIBMTR’s capacity as a public health authority under the Health Insurance Portability and Accountability Act (HIPAA) privacy rule. All patients provided written informed consent for participation in the National Marrow Donor Program institutional review board–approved CIBMTR database (NCT01166009) and repository (NCT04920474) research protocols. Research was performed in compliance with all applicable federal regulations pertaining to the protection of human research participants and with the approval of the CIBMTR observational research group.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gui, G., Ravindra, N., Hegde, P.S. et al. Measurable residual mutated IDH2 before allogeneic transplant for acute myeloid leukemia. Bone Marrow Transplant 60, 144–153 (2025). https://doi.org/10.1038/s41409-024-02449-2
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41409-024-02449-2
This article is cited by
-
Precision medicine results from equitable representation
Bone Marrow Transplantation (2025)
-
Disease characteristics and monitoring of IDH1/IDH2-mutated acute myeloid leukemia
Blood Cancer Journal (2025)
-
Measurable residual mutated IDH1 before allogeneic transplant for acute myeloid leukemia
Bone Marrow Transplantation (2025)