Abstract
The development of chimeric antigen receptor (CAR) T-cells, engineered from peripheral T-lymphocytes of a patient with lymphoma, in order to specifically target tumor cells, has been a revolution in adoptive cell therapy (ACT). As outlined in this review, ACT was initiated by hematopoietic cell transplantation (HSCT) and re-injection of interleukin-boosted tumor-infiltrating lymphocytes (TIL). The innovative venture of genetically modifying autologous peripheral T-cells to target them to cell-surface tumoral antigens through an antibody-derived structure (i.e. independent of major histocompatibility antigen presentation, physiologically necessary for T-cell activation), and intracytoplasmic T-cell costimulatory peptides, via a novel membrane CAR, has been an outstanding breakthrough. Here, focusing on B-cell hematological malignancies and mostly non-Hodgkin lymphoma, attention is brought to the importance of providing an optimal microenvironment for such therapeutic cells to proliferate and positively develop anti-tumoral cytotoxicity. This, perhaps paradoxically, implies a pre-infusion step of deep lymphopenia and deregulation of immunosuppressive mechanisms enhanced by tumoral cells. Fludarabine and cyclophosphamide appear to be the most efficient lymphodepletive drugs in this context, dosage being of importance, as will be illustrated by a thorough literature review.
Similar content being viewed by others
Introduction
Chimeric antigen receptor T-cell (CAR-T) immunotherapy is a form of adoptive cell therapy (ACT) consisting of genetically engineered T-lymphocytes recognizing specific surface targets of tumor cells. This target is usually CD19 for the treatment of B-lineage non-Hodgkin lymphomas (NHL). Peripheral T-lymphocytes are collected from the patient, transfected with a CAR construction, expanded ex-vivo, conditioned and reinfused.
Autologous CAR-T therapy, used in Europe since June 2018, is standard-of-care treatment for refractory and/or relapsed (R/R) B-cell NHL (B-NHL). Up to the summer of 2024, four FDA-approved CAR-T (tisagenlecleucel, [tisa-cel] Kymriah®, axicabtagene ciloleucel, [axi-cel] Yescarta®, brexucabtagene autoleucel, [brexu-cel] Tecartus® and lisocabtagene maraleucel, [liso-cel] Breyanzi®) have been developed in this context. They are reinfused in clinical practice after lymphodepletion (LD) with fludarabine and cyclophosphamide (FluCy) as recommended [1,2,3,4,5,6].
Although CAR-T represent a major advance in R/R B-NHL [1,2,3, 5, 7], less than half the patients have durable responses [2,3,4,5, 8,9,10,11,12,13]. CAR-T resistance is influenced by the construction and doses of CAR-T [3, 8, 14], high tumor volume [4, 11, 15] and tumoral intrinsic factors such as antigen loss, immune dysregulation and T-cell exhaustion [16,17,18], as well as by LD chemotherapy [19, 20]. The latter facilitates CAR-T engraftment, expansion, and persistence [21]. The response and durability of CAR-T therapy in B-NHL CAR-T is conditioned by CAR-T expansion kinetics (peak and first month area under the curve [AUC]) [2, 3, 22]. Many LD regimens have been tested, but FluCy is the most used, owing to its demonstrated superiority [3, 23].
The aim of this review is to present available clinical data on LD, its impact on ATC therapies, and outcomes in hematological malignancies, with a focus on NHL.
ACT historical background
ACT use cells of the immune system to target and eliminate tumor cells. This began with hematopoietic stem cell (HSC) transplantation (HSCT), followed by the reinfusion of tumor-infiltrating lymphocytes (TIL) and, later, CAR-T. The first transfer of HSC from a donor to a patient occurred in 1950, and the first allogenic HSCT (allo-HSCT) was performed in 1957 [24]. TIL were developed in the 1980’s and CAR-T two decades later.
The term “conditioning” for LD designates in HSCT the preparative regimen administered before HSC infusion. It aims at providing immunosuppression, favoring engraftment and reducing the risk of graft rejection by the recipient immune system. Initially, conditioning regimens were myeloablative, involving total body irradiation and Cy. This provided a potent anti-cancer effect and optimal engraftment, yet was associated to significant toxicity (83% mortality by day 100) [24, 25].
In 1983 [26] the introduction of busulfan and Cy allowed to alleviate toxicity, yet induced prolonged cytopenias, restricting HSCT to younger/fit patients. A shift occurred towards non-myeloablative or reduced-intensity regimens [27], using Flu and lower doses of alkylating agents [28]. Moreover, an optimal Flu exposure (AUC 20 mg*h/L), is a strong predictor of both non-relapse mortality and survival after allo-HSCT for hematological malignancies [29].
ACT using T-lymphocytes was found effective in murine models of nude rats [30], lacking a thymus and hence T-cells. Moreover, it was shown in murine models of cancers that LD (irradiation) prior to T-cell infusion favored their expansion and anti-tumor efficacy [31]. In the absence of LD, infused T-cells declined rapidly and failed to produce a response [31]. Moreover, these models showed that more effector T-cells were needed in the absence of LD, confirming the role of LD in curative T-cell expansion [31].
Initial studies using LD in TIL therapy were conducted in metastatic melanoma [32] where, without LD, responses were of short duration [33]. Yet Cy alone was not potent enough [33], while FluCy provided better and longer responses [34], after transient LD.
Although the doses and duration of FluCy varied between trials, it became clear that profound immune depletion was necessary to enhance the efficacy of TIL in solid cancer [33].
Lymphodepletion for autologous CAR-T in NHL
Clinical application of CAR-T was not fully developed until the late 2010’s with tisa-cel approved by 2017 for acute lymphoblastic leukemia (ALL) [35]. In the field of R/R diffuse large B-cell lymphoma (DLBCL), the phase II JULIET (Table 1) trial administered tisa-cel, after various LD regimens of FluCy or bendamustine, recommended in case of Cy-related grade 4 hemorrhagic cystitis or demonstrated previous resistance to Cy [36]. LD was not required in case of leukopenia (1 × 109/L) in the week prior to infusion. Response rates were similar with FluCy or bendamustine, but FluCy allowed for a higher overall response rate (ORR; 57,6% versus 40,9%), 1-year progression-free (PFS; 39,1% vs 21,2%.) and better overall (OS) survival. Only 2/8 patients who did not receive LD achieved a response [3, 36].
As shown in Table 1, FluCy at slightly different dosages was used with axi-cel in ZUMA-1, with tisa-cell in JULIET and ELARA, with liso-cel in TRANSCEND and with brexu-cel in ZUMA-2 [2, 3, 6, 36,37,38,39], in various types of NHL.
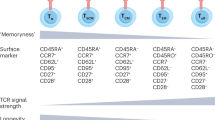
Effects of lymphodepletion on host and tumor cells (Fig. 1)
Endogenous host cells can impact the functionality of ACT by competing for homeostatic and activating cytokines or exerting an immunosuppressive activity. Indeed, successful ACT relies on the differentiation of infused T-cells into functional, long-lived memory cells, facilitated by interleukin (IL)-7, IL-12 and IL-15 through the JAK-STAT pathway [40,41,42], the levels of which are increased by LD. The removal of regulatory T-cells (Tregs), that would tamper these activities is one of the key mechanisms of LD.
Lymphodepletion (LD), primarily consisting of combined fludarabine and cyclophosphamide (FluCy), is administered to induce changes in host cells and the microenvironment. The key effects of LD are: a Elimination of endogenous immune cells (T regs and probably NK cells); enhancing the recognition of tumor antigens by mature dendritic cells (DC) and M1 macrophages. b Induction of immunogenic cell death in tumor cells, which includes the downregulation of 2,3-dioxygenase (IDO), an enzyme that can suppress immune responses. c Improved availability of homeostatic cytokines (IL-7, IL-15, IL-21), which are crucial for survival and proliferation of transferred donor T cells. The final impact will induce the expansion of CAR T-cells (3).
At the tumoral level, LD downregulates the expression of indoleamine 2,3-dioxygenase (IDO) [43], an intracellular enzyme metabolizing tryptophan in derivates inhibiting T-cell activity and cytokine production. CAR-T therapy indeed showed no efficacy in a xenograft murine model of IDO-positive NHL cells [44, 45].
LD, particularly with low Cy doses, induces the conversion of suppressive tumor-promoting M2 macrophages into M1 pro-inflammatory and antigen-presenting cells (APC). LD positively influences the production of oxygen radicals through innate immunity [46].
LD activates dendritic cells (DCs), the most potent professional APCs [40, 47], notably liver and spleen DCs during the early phase of lymphopenia. DCs maturation is crucial for them to participate to anti-tumoral immunity. It is triggered, via Toll-like or other receptors by the uric acid issued tumor cell apoptosis [40] and by translocation of the microbiota upon LD-induced damages to mucosal barriers.
A less positive effect of LD, although controversial, is that they could increase the levels of myeloid-derived suppressor cells (MDSCs), liable to impair CAR-T efficacy, through mobilization of hematopoietic progenitor cells from the bone marrow [16, 20, 43, 48, 49].
Effect of lymphodepletion on CAR-T kinetics
LD significantly impacts the expansion of CAR-T (i.e. peak level and persistence), higher peaks/AUC being associated with better PFS and OS [50, 51], notably through higher levels of LD-induced IL-15 [49]. In the same line, high baseline cytokine levels correlate with those after LD and CAR-T peak [16]. Moreover, CAR-T express high levels of receptors for key homeostatic cytokines, providing them with an advantage over other cell types [41]. Compared to no LD, Flu-based LD was shown to positively impact the kinetics of tisa-cel in DLBCL [19]. In a retrospective study of axi-cel [52], strong expanders had more objective ORR at day30 (91% vs. 40%) and better PFS. Similarly, after liso-cel, higher CAR-T expansion resulted in better overall response and CR rate [37, 53].
The next chapter examines the impact of drug type and dosages used for LD.
Lymphodepletion regimens and CD19-AUTOLOGOUS CAR-T in hematological malignancies
High dose cyclophosphamide
Several studies, primarily in ALL, have demonstrated the advantage of using high doses of Cy [54, 55]. Comparing CAR-T therapy in patients with R/R chronic lymphocytic leukemia (CLL) or ALL [54], split in two cohorts respectively without LD or with Cy alone, it was shown that peripheral CAR-T were respectively undetectable at 1 month vs. still detected at 5 weeks. Cy moreover provided a longer B-cell aplasia (BCA), a good sign of CAR-T efficacy. Another trial in R/R ALL using Cy at two doses (1.5 or 3.0 g/m2) [55] found a better lymphodepletion after 3 g/m² Cy, followed by a higher peak of CAR-T in responders (13 days vs 1). This highlights the importance of achieving a profound lymphodepletion and high post-infusion CAR-T peak, in patients with minimal pre-treatment disease burden, in order to achieve clinical response and longer OS [55, 56].
Addition of fludarabine improves CAR-T KINETICS and response. (Table 1)
Although the first CAR-T LD with FluCy in NHL occurred in 2010 [57], protocols only began to incorporate Flu in conditioning for hematological malignancies from 2016 on, owing to the report of improved CAR-T expansion after Flu-based LD [57, 58].
In a phase I clinical trial in ALL [14], FluCy, Cy alone, or etoposide-based LD were used, showing 100% engraftment after FluCy, i.e. detectable peripheral CAR-T, development of BCA and MRD-negative remission, with a median time to peak of 10 days. The peak and AUC were significantly higher after FluCy compared to Cy alone or etoposide, and BCA lasted longer (6,4 months vs 2.1).
In a CLL trial [59], patients receiving Flu-based LD achieved the lowest lymphocyte nadir and greatest peak expansion of CAR-T.
In a trial of liso-cel for B-NHL, FluCy conditioning was also associated to greater CAR-T expansion, higher response rates (50% CR, 72% ORR) and better PFS compared to Cy alone (8% CR, 50% ORR) [23]. Another trial with higher FluCy LD intensity in NHL comparing two dosages of Cy [60] found that Cy 60 mg/kg/d was associated with a favorable cytokine profile correlating with better PFS than Cy 30 mg/kg/d. However, not all patients with high intensity LD achieved such a favorable cytokine profile, indicating that biological individual factors may be also determinant [60]. Using Flu 30 mg/m2 and 3 daily doses of Cy 300 mg/m2 in a phase I first-in-human trial in NHL, yielded an ORR of 70% [61]. Similar CR rates were observed in ALL patients treated with Cy 3 g/m2 alone as LD [62].
Flu is currently dosed based on body surface area and administered IV as a monophosphate prodrug (F-ara-AMP), converted to the circulating metabolite F-ara-A, mainly cleared by the kidney. In ALL, fludarabine exposure is measured by an F-ara-A assay [29], and correlates with leukemia-free survival, CAR-T expansion and better duration of BCA [63]. These results were confirmed in a retrospective real-world analysis of 152 patients with ALL treated by tisa-cel [56], as well as in another with axi-cel in NHL, where optimal Flu exposure correlated with improved PFS [64].
Other agents than flucy
Shortage of Flu in the USA [65] has led to search alternative regimens, bendamustine being a viable option [66, 67]. This alkylating agent offers anti-lymphoma activity, potent lymphodepleting effects, and good tolerability [68]. Moreover, it is metabolized in the liver and not excreted in the kidney, making it appropriate for patients with impaired renal function [66].
A small study in CLL used pentostatin combined with Cy in five patients, bendamustine alone in six, and FluCy in three, without difference in response rates [69].
For tisa-cel, a retrospective multicenter comparison between bendamustine and FluCy resulted in similar efficacy, with lower rates of CRS, neurotoxicity, and hematological toxicity in the bendamustine arm [67]. ORR and PFS were similar with 50% ORR after bendamustine and 42.9% after FluCy. Median PFS were 3.26 and 3.06 months respectively. CRS of any grade were higher in the FluCy group (66.7% versus 40%), without differences in severe CRS. ICANS of any grade were present in 7.8% of patients with bendamustine versus 21.4% for FluCy, severe in 1.1% vs. 9.5%. There were respectively 15.6% and 50% of infections, possibly related to grade 3 neutropenia (28.9% and 90.5%).
For axi-cel, with bendamustine vs FluCy, no differences were seen in PFS and OS, yet there was a lower incidence of ICANS and severe neutropenia with bendamustine [68, 70]. Lymphocyte counts decreased of similar rates after LD. The best ORR/CR were 77.8%/48.1% with bendamustine and 81.0%/50.0% with FluCy. Six-month PFS were 43.8% and 55.6% and 6-month OS 81.5% and 90.4%. Grade ≥3 CRS were observed in 3.7% vs. 4.8% of the patients, grade ≥3 ICANS in 19% vs. 31% and grade ≥3 neutropenia in 68% vs. 100%, while grade 3 infections were similar at 24% vs. 19% respectively [68]. This differs from data obtained with axi-cel in another bendamustine vs. FluCy trial, that reported more febrile neutropenia (13.6% vs. 78.4%) and infections (27.3% vs. 78.4%) [70] with FluCy.
The role of the hypomethylating agent decitabine is currently investigated in CAR-T therapy, with regard to the abnormal hypermethylation in lymphoma. Under decitabine, there is an increased expression of CD19, less T-cell exhaustion, more T-cell activation and modification the tumor microenvironment [71]. Lymphoma cell-lines exposed to decitabine also increase CD19 expression and show no impairment of CAR-T efficacy [71]. Two patients with NHL, conditioned with decitabine and FluCy, achieved optimal responses [71].
Clofarabine has also been used with Cy or bendamustine before tisa-cel or ARI-0001 in pediatric ALL [72,73,74].
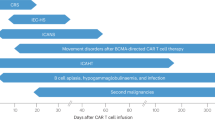
Toxicity related to lymphodepleting regimens
Cytopenias and subsequent infections are the most common adverse effects of LD, causing an initial drop in leukocyte counts within the first two weeks [74]. Hematology toxicity is an early and long-lasting complication with a biphasic pattern [75] which may require blood or platelet transfusions or the use of granulocyte-colony stimulating factor (G-CSF) [50, 76,77,78]. Neutropenia is the most common cytopenia (72%) after CAR-T, followed by thrombopenia [79]. Early neutropenia is mostly related to LD while persisting neutropenia beyond day 28 post infusion can be related to the CAR-T construct, CRS or ICANS [79]. EBMT (European group for bone marrow transplantation) recommendations consider using prophylactic G-CSF in neutropenic patients from day +5, although earlier use has no effect on immunotoxicity, CAR-T expansion nor prognosis, yet reduces febrile neutropenia [77, 78].
High dose LD (Flu 125 mg/m2, Cy 60 to 120 mg/kg) has been reported to result in 67% of patients needing platelet transfusion versus 1% after low-dose LD (Flu 90 mg/m2, Cy 300 mg/m2) [68]. As reported above, bendamustine seems less toxic than FluCy [67, 68, 70].
LD, while not being the main factor, might also influence CRS and ICANS. FluCy conditioning has been correlated with the severity of CRS [80]. For axi-cel in DLBCL and follicular lymphoma, any-grade CRS occurred in 91.9% of the patients after FluCy vs. 72.7% after bendamustine, and any-grade neurotoxicity in 45.9% vs18.2% [70].
Flu was initially thought to be related to the neurotoxicity of CAR-T, as it may lead to reversible somnolence and peripheral neuropathy at the time of infusion. However, the evidence to date does not support a direct role for Flu in ICANS, although it could be a contributing factor in case of impaired renal function [81].
LD in other contexts: ANTI-CD30, dual and allogenic CAR-T. (Table 2)
For the treatment of R/R Hodgkin lymphoma (HL) with anti-CD30 CAR-T, different regimens have been evaluated, mostly bendamustine alone, bendamustine and fludarabine or FluCy [82]. Although bendamustine is a potential therapy in R/R HL, it is unlikely to enhance post-CAR-T responses. The combination of Flu with bendamustine promoted a favorable homeostasis of IL-7 and IL-15 compared with FluCy or bendamustine alone, leading to higher antitumor activity and longer CAR-T persistence. However, the 94% 1-year OS did not differ between these regimens [82]. In a phase I trial for CD30-expressing NHL, FluCy allowed for a CAR-T peak in some patients, but all progressed within 6 months, which precluded further development [83].
Dual CAR-T directed to both CD19 and CD22 are under investigation to overcome antigen escape. LD consists of decitabine and FluCy and, so far, some transient grade 3/4 neutropenias have been observed [84].
Allogenic “off-the-shelf” CAR-T, currently used in clinical trials, are generated from healthy donor T-cells. TRAC and CD52 genes are inactivated using TALEN® gene editing to minimize the risk of graft-versus-host disease and improve the compatibility and persistence of CAR-T. For conditioning, alemtuzumab (anti-CD52) may be added in some circumstances. In R/R ALL, UCART19 is under phase I evaluation with a FluCy conditioning with or without alemtuzumab [85]. In R/R aggressive DLBCL, a 3-day LD with FluCy and alemtuzumab has been used [86]. Alemtuzumab seems to be necessary in combination with FluCy before UCART19 [87] for positive IL-7 exposure and UCART19 kinetics, but higher toxicities are expected [74]. In ALL, peripheral UCART19 was detectable from D7, with peak expansion in 72% of the patients between D10 and D17, and a median persistence duration of 28 days. No expansion was observed in 5/18 patients, 3 of whom did not receive alemtuzumab. However, the definitive LD regimen and its impact on UCART19 expansion are currently investigated [85]. Dual allogenic CAR-T against CD19 and CD22 (UCART20x22) are also in phase I/IIa study in R/R NHL with FluCy and alemtuzumab [88]. Preliminary results showed expansion in 3/3 patients with initial detection on day 7 followed by peaks between days 9-14, predominantly CD8+ [88].
Several studies stress the importance of administering LD before each CAR-T infusion, if the procedure needs to be repeated [89, 90]. Better responses have been observed in B-cell malignancies if FluCy was administered before both CART1 and CART2, although an increased dose of CART2 was also needed [88]. In ALL, pre-CAR-T2 intensified LD yielded 71% responders with higher CART2 expansion (yet lower than with CAR-T1) than after standard LD [90].
Another approach is to use NKT-cells which are also potent cytotoxic cells of the innate immune system [91]. In this context, FluCy is being used. Preliminary results indicate responses at day 30 with high peaks [92].
Fourth generation CAR-T or TRUCKs :“T-cells redirected for antigen-unrestricted cytokine-initiated killing” could avoid LD. Indeed, tumor targeting and CAR-T activation and cytotoxicity is completed by the transfection of cytokine genes yielding endogenous production that self-promotes their survival, proliferation and activation [93].
Perspectives
Many questions regarding LD and its future remain unanswered and clinical randomized trials are needed. LD is nonetheless an important factor that significantly affects CAR-T kinetics and response with the goal of achieving the lowest lymphocyte nadir and greatest peak expansion. Flu exposure seems to be a major part of LD, easily modifiable. Moreover, the importance of a personalized approach using PK-directed dosing, based on weight, renal function and drug monitoring, has been stressed, to achieve better outcomes with minimal toxicities [75, 82]. In terms of toxicity, bendamustine appears interesting as LD with a favorable profile, reducing treatment costs and hospitalization duration.
References
Crump M, Neelapu S, Farooq U. Outcomes in refractory diffuse large B-cell lymphoma: results from the international SCHOLAR-1 study. Blood 2017;130:1800–8.
Neelapu SS, Locke FL, Bartlett NL, Lekakis LJ, Miklos DB, Jacobson CA, et al. Axicabtagene ciloleucel CAR T-cell therapy in refractory large B-cell lymphoma. N. Engl J Med. 2017;377:2531–44.
Schuster SJ, Bishop MR, Tam CS, Waller EK, Borchmann P, McGuirk JP, et al. Tisagenlecleucel in adult relapsed or refractory diffuse large B-cell lymphoma. N. Engl J Med. 2019;380:45–56.
Locke FL, Ghobadi A, Jacobson CA, Miklos DB, Lekakis LJ, Oluwole OO, et al. Long-term safety and activity of axicabtagene ciloleucel in refractory large bcell lymphoma (zuma-1): a single-arm, multicenter, phase 1-2 trial. Lancet Oncol. 2019;20:31–42.
Abramson J, Palomba L, Gordon LI, Lunning MA, Wang M, Arnason J, et al. Lisocabtagene maraleucel for patients with relapsed or refractory large B-cell lymphomas (TRANSCEND NHL 001): a multicentre seamless design study. Lancet 2020;396:839–52.
Wang M, Munoz J, Goy A, Locke FL, Jacobson CA, Hill BT, et al. KTE-X19 CAR T-cell therapy in relapsed or refractory mantle-cell lymphoma. N. Engl J Med. 2020;382:1331–42.
Strati P, Neelapu S. Chimeric Antigen Receptor-engineered T cell therapy in Lymphoma. Curr Oncol Rep. 2019;21:38.
Nastoupil L, Jain M, Feng L, Spiegel JY, Ghobadi A, Lin Y, et al. Standard-of-care axicabtagene ciloleucel for relapsed or refractory large B cell lymphoma: results from the US lymphoma CAR T consortium. J Clin Oncol. 2020;38:3119–28.
Pasquini MC, Hu Z-H, Curran K, Laetsch T, Locke F, Rouce R, et al. Real world evidence of tisagenlecleucel for pediatric acute lymphoblastic leukemia and non-Hodgkin lymphoma. Blood Adv. 2020;4:5414–24.
Le Gouill S, Bachy E, Di Blasi R, Cartron G, Beauvais D, Le Bras F, et al. First results of DLBCL patients treated with CAR-T cells and enrolled in DESCAR-T registry, a French real-life database for CAR-T cells in hematologic malignancies. Hematological Oncol. 2021;39:18.
Di Blasi R, Le Gouill S, Bachy E, Cartron G, Beauvais D, Le Bras F, et al. Outcomes of patients with aggressive B-cell lymphoma after failure of anti-CD19 CAR T-cell therapy: a DESCAR-T analysis. Blood. 2022;140:2584–93.
Bethge W, Martus P, Schmitt M, Holtick U, Subklewe M, von Tresckow B, et al. GLA/DRST real-world outcome analysis of CAR T-cell therapies for large B-cell lymphoma in Germany. Blood. 2022;140:349–58.
Kwon M, Iacoboni G, Reguera JL, Corral LL, Morales RH, Ortiz-Maldonado V, et al. Axicabtagene ciloleucel compared to tisagenlecleucel for the treatment of aggressive B-cell lymphoma. Haematologica 2023;108:110–21.
Gardner R, Finney O, Annesley C, Brakke H, Summers C, Leger K, et al. Intent-to-treat leukemia remission by CD19 CAR T cells of defined formulation and dose in children and young adults. Blood 2017;129:3322–31.
Vercellino L, Di Blasi R, Kanoun S, Tessoulin B, Rossi C, D’Aveni-Piney M, et al. Predictive factors of early progression after CAR T-cell therapy in relapsed/refractory diffuse large B-cell lymphoma. Blood Adv. 2020;4:5607–15.
Jain M, Zhao H, Wang H, Atkins R, Menges M, Reid K, et al. Tumor interferon signaling and suppressive myeloid cells are associated with CAR T-cell failure in large B-cell lymphoma. Blood 2021;137:2621–33.
Laurent C, Syrykh C, Hamon M, Adélaïde J, Guille A, Escudié F, et al. Resistance of B-cell lymphomas to CAR T-cell therapy is associated with genomic tumor changes which can result in transdifferentiation. Am J Surg Pathol. 2022;46:742–53.
Rejeski K, Jain M, Smith E. Mechanisms of resistance and treatment of relapse after CAR T-cell therapy for large b-cell lymphoma and multiple myeloma. Transplant Cell Ther. 2023;29:418–28.
Awasthi R, Pacaud L, Waldron E, Tam CS, Jäger U, Borchmann P, et al. Tisagenlecleucel cellular kinetics, dose, and immunogenicity in relation to clinical factors in relapsed/refractory DLBCL. Blood Adv. 2020;4:560–72.
Galli E, Battaglia A, Fossati M, Pansini I, Bellesi S, Buzzonetti A, et al. High levels of circulating granulocytic myeloid-derived suppressor cells (G-MDSCs) predict failure of CD19-targeting CAR-T cell therapy. Blood 2023;142:1015–7.
Brudno J, Kochenderfer J. Chimeric antigen receptor T-cell therapies for lymphoma. Nat Rev Clin Oncol. 2018;15:31–46.
Cappel KM, Kochenderfer J. Long-term outcomes following CAR T cell therapy: what we know so far. Nat Rev Clin Oncol. 2023;20:359–71.
Turtle C, Hanafi L, Berger C, Hudecek M, Pender B, Robinson E, et al. Immunotherapy of non-Hodgkin lymphoma with a defined ratio of CD8+ and CD4+ CD19-specific chimeric antigen receptor-modified T cells. Sci Transl Med. 2016;8:355ra116.
Thomas ED, Lochte HL, Lu WC, Freebee JW. Intravenous infusion of bone marrow in patients receiving radiation and chemotherapy. N. Engl J Med. 1957;157:491–6.
Thomas ED, Buckner CD, Banaji M, Clift RA, Fefer A, Flournoy N, et al. One hundred patients with acute leukemia treated by chemotherapy, total body irradiation, and allogeneic marrow transplantation. Blood 1977;49:511–33.
Santos G. History of bone marrow transplantation. Clin Haematol. 1983;12:611–39.
Gyurkocza B, Sandmaier B. Conditioning regimens for hematopoietic cell transplantation: one size does not fit all. Blood 2014;124:344–53.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009;15:1628–33.
Langenhorst JB, van Kesteren C, van Maarseveen EM, Dorlo TPC, Nierkens S, Lindemans CA, et al. Fludarabine exposure in the conditioning prior to allogeneic hematopoetic cell transplantation predicts outcomes. Blood Adv. 2019;3:2179–87.
Bell EB, Sparshott SM, Drayson MT, Ford WL. The stable and permanent expansion of functional T lymphocytes in athymic nude rats after a single injection of mature T cells. J Immunol. 1987;139:1379–84.
Wang L, Shu S, Plautz G. Host lymphodepletion augments T cell adoptive immunotherapy through enhanced intratumoral proliferation of effector cells. Cancer Res. 2005;65:9547–54.
Rosenberg SA, Yannelli JR, Yang JC, Topalian SL, Schwartzentruber DJ, Weber JS, et al. Treatment of patients with metastatic melanoma with autologous tumor-infiltrating lymphocytes and interleukin 2. J Natl Cancer Inst. 1994;86:1159–66.
Dudley ME, Wunderlich JR, Robbins PF, Yang JC, Hwu P, Schwartzentruber DJ, et al. Cancer regression and autoimmunity in patients after clonal repopulation with antitumor lymphocytes. Science. 2002;298:850–4.
Dudley ME, Sherry R, Hughes MS, Hughes MS, Royal R, Kammula U, et al. Adoptive cell therapy for patients with metastatic melanoma: evaluation of intensive myeloablative chemoradiation preparative regimens. J Clin Oncol. 2008;26:5233–9.
Maude SL, Laertsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, et al. Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N. Engl J Med. 2018;378:439–48.
Andreadis C, Tam C, Borchmann P, Jaeger U, McGuirk JP, Holte G, et al. Correlation of bridging and lymphodepleting chemotherapy with clinical outcomes in patients with relapsed/refractory diffuse large B-cell lymphoma treated with Tisagenlecleucel. Blood 2019;134:2883.
Abramson JS, Solomon SR, Arnason J, Johnston PB, Glass B, Bachanova V, et al. Lisocabtagene maraleucel as second-line therapy for large B-cell lymphoma: primary analysis of the phase 3 TRANSFORM study. Blood 2023;141:1675–84.
Kamdar M, Solomon SR, Arnason J, Johnston PB, Glass B, Bachanova V, et al. Lisocabtagene maraleucel versus standard of care with salvage chemotherapy followed by autologous stem cell transplantation as second-line treatment in patients with relapsed or refractory large B-cell lymphoma (TRANSFORM): results from an interim analysis of an open-label, randomised, phase 3 trial. Lancet 2023;399:2294–308.
Fowler NH, Dickinson M, Dreyling M, Martinez-Lopez J, Kolstad A, Butler J, et al. Tisagenlecleucel in adult relapsed or refractory follicular lymphoma: the phase 2 ELARA trial. Nat Med. 2022;28:325–32.
Salem ML, El-Naggar SA, Cole DJ. Cyclophosphamide induces bone marrow to yield higher numbers of precursor dendritic cells in vitro capable of functional antigen presentation to T cells in vivo. Cell Immunol. 2010;261:134–43.
Gattinoni L, Finkelstein S, Klebanoff C, Antony PA, Palmer DC, Spiess PJ, et al. Removal of homeostatic cytokine sinks by lymphodepletion enhances the efficacy of adoptively transferred tumor-specific CD8 T cells. JEM. 2005;202:907–12.
Muranski P, Restifo N. Adoptive immunotherapy of cancer using CD4+ T cells. Curr Opin Immunol. 2009;21:200–8.
Bechman N, Maher J. Lymphodepletion strategies to potentiate adoptive T-cell immunotherapy – what are we doing; where are we going? Expert Opin Biol Ther. 2021;21:627–37.
Ninomiya S, Narala N, Huye L, Yagyu S, Savoldo B, Dotti G, et al. Tumor indoleamine 2,3-dioxygenase (IDO) inhibits CD19-CAR T cells and is downregulated by lymphodepleting drugs. Blood 2015;125:3905–16.
Hanafi LA, Gauchat D, Godin-Ethier J, Possamaï D, Duvignaud JB, Leclerc D, et al. Fludarabine downregulates indoleamine 2,3-dioxygenase in tumors via a proteasome mediated degradation mechanism. PLoS ONE. 2014;9:e99211.
Bryniarski K, Szczepanik M, Ptak M, Zemelka M, Ptak W. Influence of cyclophosphamide and its metabolic products on the activity of peritoneal macrophages in mice. Pharmacol Rep. 2009;61:550–7.
Schiavoni G, Sistigu A, Valentini M, Mattei F, Sestili P, Spadaro F, et al. Cyclophosphamide synergized with type I interferons through systemic dendritic cell reactivation and induction of immunogenic tumor apoptosis. Cancer Res. 2011;71:768–78.
Restifo N, Dudley M, Rosenberg S. Adoptive immunotherapy for cancer: harnessing the T cell response. Nat Rev Immunol. 2018;12:269–81.
Innamarato P, Kodumudi K, Asby S, Schachner B, Hall M, Mackay A, et al. Reactive myelopoiesis triggered by lymphodepleting chemotherapy limits. Mol Ther. 2020;28:2252–70.
Kochenderfer J, Somerville R, Lu T, Shi V, Bot A, Rossi J, et al. Lymphoma remissions caused by anti-CD19 chimeric antigen receptor T cells are associated with high serum interleukin-15 Levels. J Clin Oncol. 2017;35:1803–13.
Wittibschlager V, Bacher U, Seipel K, Porret N, Wiedemann G, Haslebacher C, et al. CAR T-cell persistence correlates with improved outcome in patients with B-cell lymphoma. Int J Mol Sci 2023;24:5688.
Ayuk F, Berger C, Badbaran A, Zabelina T, Sonntag T, Riecken K, et al. Axicabtagene ciloleucel in vivo expansion and treatment outcome in aggressive B-cell lymphoma in a real-world setting. Blood 2021;5:2523–7.
Ogasawara K, Lymp J, Mack T, Dell’Aringa J, Huang CP, Smith J, et al. In vivo cellular expansion of of lisocabtagene maraleucel and association with efficacy and safety in relapsed/refractory large B-cell lymphoma. Clin Pharm Ther. 2022;112:81.
Brentjens RJ, Rivière I, Park JH, Davila ML, Wang X, Stefanski J, et al. Safety and persistence of adoptively transferred autologous CD19-targeted T cells in patients with relapsed or chemotherapy refractory B-cell leukemias. Blood. 2011;118:4817–28.
Curran KJ, Margossian SP, Kernan NA, Silverman LB, Williams DA, Shukla N, et al. Toxicity and response after CD19-specific CAR T-cell therapy in pediatric/young adult relapsed/refractory B-ALL. Blood 2019;134:2361–8.
Fabrizio V, Boelens J, Mauguen A, Baggott C, Prabhu S, Egeler E, et al. Optimal fludarabine lymphodepletion is associated with improved outcomes after CAR T-cell therapy. Blood Adv. 2022;6:1961–8.
Kochenderfer J, Wilson W, Janik J. Eradication of B-lineage cells and regression of lymphoma in a patient treated with autologous T cells genetically engineered to recognize CD19. Blood 2010;116:4099–102.
Kochenderfer JN, Dudley ME, Feldman SA, Wilson WH, Spaner DE, Maric I, et al. B-cell depletion and remissions of malignancy along with cytokine-associated toxicity in a clinical trial of anti-CD19 chimeric-antigen-receptor-transduced T cells. Blood 2012;119:2709.
Geyer MB, Rivière I, Sénéchal B, Wang X, Wang Y, Purdon TJ, et al. Safety and tolerability of conditioning chemotherapy followed by CD19-targeted CAR T cells for relapsed/refractory CLL. JCI Insight. 2019;5:e122627.
Hirayama A, Gauthier J, Hay KA, Voutsinas JM, Wu Q, Gooley T, et al. The response to lymphodepletion impacts PFS in patients with aggressive non-Hodgkin lymphoma treated with CD19 CAR T cells. Blood 2019;133:1876–87.
Brudno J, Lam N, Venasse D. Safety and feasibility of anti-CD19 CAR T cells with fully-human binding domains in patients with B-cell lymphoma. Nat Med. 2020;26:270–80.
Park J, Riviere I, Gonen M, Wang X, Sénéchal B, Curran KJ, et al. Long-Term Follow-up of CD19 CAR Therapy in acute lymphoblastic leukemia. N. Engl J Med. 2018;378:449–59.
Dekker L, Calkoen F, Jiang Y, Blok H, Veldkamp SR, De Koning C, et al. Fludarabine exposure predicts outcome after CD19 CAR T-cell therapy in children and young adults with acute leukemia. Blood Adv. 2022;6:1969–76.
Scordo M, Flynn J, Gonen M, Devlin SM, Parascondola A, Tomas AA, et al. Identifying an optimal fludarabine exposure for improved outcomes after axi-cel therapy for aggressive B-cell non-Hodgkin lymphoma. Blood Adv. 2023;7:5579–85.
Maziarz RT, Diaz A, Miklos DB, Shah NN. Perspective: an International Fludarabine shortage: supply chain issues impacting transplantation and immune effector cell therapy delivery. Transpl Cell Ther. 2022;28:723–6.
F Filioglou D, Husnain M, Khurana S, Simpson RJ, Katsanis E. Has the shortage of fludarabine altered the current paradigm of lymphodepletion in favor of bendamustine? Font Immunol. 2023;14:1329850.
Ghilardi G, Chong E, Svoboda J, Wohlfarth P, Nasta SD, Williamson S, et al. Bendamustine is safe and effective for lymphodepletion before tisagenlecleucel in patients with refractory or relapsed large B-cell lymphomas. Ann Oncol. 2022;33:916–28.
Ong S, Pak S, Mei M, Wang Y, Popplewell L, Baird JH, et al. Bendamustine lymphodepletion is a well-tolerated alternative to fludarabine and cyclophosphamide lymphodepletion for axicabtagene ciloleucel therapy for aggressive B-cell lymphoma. Am J Hematol. 2023;98:1751–61.
Porter D, Hwang WT, Frey N, Lacey SF, Shaw PA, Loren AW, et al. Chimeric antigen receptor T cells persist and induce sustained remissions in relapsed refractory chronic lymphocytic leukemia. Sci Transl Med. 2015;7:303ra139.
Ghilardi G, Paruzzo L, Svoboda J, Chong EA, Shestov AA, Chen L, et al. Bendamustine lymphodepletion before axicabtagene ciloleucel is safe and associates with reduced inflammatory cytokines. Blood Adv. 2024;8:653–66.
Li S, Xue L, Wang M, Qiang P, Xu H, Zhang X, et al. Decitabine enhances cytotoxic effect of T cells with an anti-CD19 chimeric antigen receptor in treatment of lymphoma. Onco Targets Ther. 2019;12:5627–38.
Green S, Schultz L. Rational alternatives to fludarabine and cyclophosphamide-based pre-CAR lymphodepleting regimens in the pediatric and young adult B-ALL setting. Curr Oncol Rep. 2023;25:841–6.
Foti A, Stein D, Seidel D. Clofarabine for Lymphodepletion before CAR-T-Cell Infusion: A brief Case Report. J Pedriatr Hematol Oncol. 2023;45:e551–e554.
Lickefett B, Chu L, Ortiz-Maldonado V, Warmuth L, Barba P, Doglio M, et al. Lymphodepletion – an essential but undervalued part of the chimeric antigen receptor T-cell therapy cycle. Front Immunol 2023;14:1303935.
Fried S, Avigdor A, Bielorai B, Meir A, Besser MJ, Schachter J, et al. Early and late hematologic toxicity following CD19 CAR-T cells. Bone Marrow Transplant. 2019;54:1643–50.
Galli E, Allain V, Di Blasi R, Bernard S, Vercellino L, Morin F, et al. G-CSF does not worsen toxicities and efficacy of CAR-T cells in refractory/relapsed B-cell lymphoma. Bone Marrow Transpl. 2020;55:2347–9.
Lievin R, Di Blasi R, Morin F, Galli E, Allain V, De Jorna R, et al. Effect of early granulocyte-colony-stimulating factor administration in the prevention of febrile neutropenia and impct on toxicity and efficacy of anti-CD19 CAR-T in patients with relapsed/refractory B-cell lymphoma. Bone Marrow Transpl. 2023;57:431–9.
Hayden PJ, Roddie C, Bader P. Management of adults and children receiving CAR T-cell therapy: 2021 best practice recommendations of the European Society for Blood and Marrow Transplantation (EBMT) and the Joint Accreditation Committee of ISCT and EBMT (JACIE) and the European Haematology Association (EHA). Ann Oncol. 2022;33:259–75.
Gea-Banacloche J. Infectious complications of Chimeric Antigen Receptor (CAR) T-Cell therapies. Semin Hematol. 2023;60:52–58.
Hay K, Hanafi LA, Li D, Gust J, Liles WC, Wurfel MM, et al. Kinetics and biomarkers of severe cytokine release syndrome after CD19 chimeric antigen receptor–modified T-cell therapy. Blood 2017;130:2295–306.
Lowe KL, Mackall CL, Norry E, Amado R, Jakobsen BK, Binder G. Fludarabine and neurotoxicity in engineered T-cell therapy. Gene Ther. 2018;25:176–91.
Ramos C, Grover N, Beaven A, Lulla PD, Wu MF, Ivanova A, et al. Anti-CD30 CAR-T cell therapy in relapsed and refractory Hodgkin lymphoma. J Clin Oncol. 2020;38:3794–804.
Brudno JN, Natrakul DA, Karrs J, Patel N, Maass-Moreno R, Ahlman MA, et al. Transient responses and significant toxicities of anti-CD30 CAR T cells for CD30+ lymphomas: results of a phase 1 trial. Blood Adv. 2024;8:802–14.
Qu C, Zou R, Wang P, Zhu Q, Kang L, Ping N, et al. Decitabine-primed tandem CD19/CD22 CAR-T therapy in relapsed/refractory diffuse large B-cell lymphoma patients. Front Immunol 2022;13:969660.
Benjamin R. Preliminary data on safety, cellular kinetics and anti-leukemic activity of UCART19, an allogeneic anti-CD19 CAR T-cell product, in a pool of adult and pediatric patients with high-risk CD19+ relapsed/refractory B-cell acute lymphoblastic leukemia. Blood 2018;132:896.
Locke FL, Munoz JL, Tees MT, Lekakis LJ, Eradat HA, de Vos S, et al. ALLO-647 for lymphodepletion in the allogeneic CAR T setting: safety experience with ALLO-501/501A in patients (pts) with relapsed/refractory (r/r) large B-Cell and follicular lymphomas. Blood 2023;142:2095.
Dupouy S, Marchiq I, Derippe T, Almena-Carrasco M, Jozwik A, Fouliard S, et al. Clinical pharmacology and determinants of response to UCART19, an allogeneic anti-CD19 CAR-T cell product, in adult B-cell acute lymphoblastic leukemia. Cancer Res Commun. 2022;2:1520–31.
Abramson J, Ramakrishnan A, Alfonso Pierola A, Braunschweig I, Cartron G, Thieblemeont C, et al. Preliminary results of Nathali-01: a first-in-human phase I/IIa study of UCART20x22, a dual allogeneic CAR-T cell product targeting CD20 and CD22, in relapsed or refractory (R/R) non-Hodgkin Lymphoma (NHL). Blood 2023;142:2110–2.
Gauthier J, Bezerra E, Hirayama A, Fiorenza S, Sheih A, Chou CK, et al. Factors associated with outcomes after a second CD19-targeted CAR T-cell infusion for refractory B-cell malignancies. Blood 2021;137:323–35.
Holland EM, Molina JC, Dede K, Moyer D, Zhou T, Yuan CM, et al. Efficacy of second CAR-T (CART2) infusion limited by poor CART expansion and antigen modulation. J Immunother Cancer. 2022;10:e004483.
Hadiloo K, Tahmasebi S, Esmaeilzadeh A. CAR-NKT cell therapy: a new promising paradigm of cancer immunotherapy. Cancer Cell Int. 2023;23:86.
Liu E, Marin D, Banerjee P, Macapinlac HA, Thompson P, Basar R, et al. Use of CAR-transduced Natural Killer cells in CD19-positive lymphoid tumors. NEJM 2020;382:545–53.
Chmielewski M, Abken H. TRUCKS, the fourth-generation CAR T cells: Current developments and clinical translation. Adv Cell Gene Ther. 2020;3:e84.
Neelapu SS, Jacobson CA, Ghobadi A, Miklos DB, Lekakis LJ, Oluwole OO, et al. Five-year follow-up of ZUMA-1 supports the curative potential of axicabtagene ciloleucel in refractory large B-cell lymphoma. Blood. 2023;141:2307–15.
Locke FL, Miklos DB, Jacobson CA, Perales MA, Kersten MJ, Oluwole OO, et al. Axicabtagene ciloleucel as second-line therapy for large B-Cell lymphoma. N. Engl J Med. 2022;386:640–54.
Wang M, Munoz J, Goy A, Locke FL, Jacobson CA, Hill BT, et al. Three-year follow-up of KTE-X19 in patients with relapsed/refractory mantle cell lymphoma, including high-risk subgroups, in the ZUMA-2 study. J Clin Oncol. 2022;41:555–67.
Acknowledgements
Medical writing for this manuscript was assisted by MPIYP (MC Béné), Paris, France.
Author information
Authors and Affiliations
Contributions
MCV and MS and CT contributed to the design of the article. MCV, MS, RDB, CC, AS, SCZ, CT contributed to the writing of the manuscript.
Corresponding author
Ethics declarations
Competing interests
MCV: no COI. MS: no conflict of interest. RdiB: Honoraria for boards, conferences and travellings: Roche, Kyte/Gilead, Novartis, BMS. CC: no COI. AS Honoraria for boards, conferences and travellings: Roche, Kyte/Gilead, Novartis, BMS. SC-Z no COI. CT Honoraria for boards, conferences and travellings: Roche, Kyte/Gilead, Novartis, BMS, Incyte, Amgen.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Canelo-Vilaseca, M., Sabbah, M., Di Blasi, R. et al. Lymphodepletion chemotherapy in chimeric antigen receptor-engineered T (CAR-T) cell therapy in lymphoma. Bone Marrow Transplant 60, 559–567 (2025). https://doi.org/10.1038/s41409-025-02539-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02539-9
This article is cited by
-
In vivo CAR-T cell engineering: concept, research progress, potential challenges and enhancement strategies
Experimental Hematology & Oncology (2025)