Abstract
The cytogenetic risk category retains a pivotal role in the prediction of prognosis in acute myeloid leukemia (AML) patients undergoing hematopoietic stem cell transplantation (HSCT), however, its impact on secondary AML (sAML) is less established. We assessed whether the ELN 2022 cytogenetic risk score predicts outcomes in sAML patients in remission undergoing HSCT from HLA-matched donors performed between 2010 and 2022. Among 1119 patients, 829 had intermediate and 284 had adverse cytogenetics (6 with favorable risk were excluded). Engraftment rates was 72.4% vs. 99.5%. Acute graft-versus-host disease (GVHD) incidence did not differ, but 2-years all grades and extensive chronic GVHD were higher in the intermediate vs. adverse cytogenetics risk groups, hazard ratio (HR) = 0.72; p = 0.034 and HR = 0.58; p = 0.027, respectively. Two-year non-relapse mortality (NRM) was similar. All other HSCT outcomes were inferior in the adverse risk vs. intermediate-risk patients: The HR for 2-year relapse incidence (RI) was 2.48 (95% CI 1.95–3.15, p < 0.001). The HRs for 2-year leukemia-free survival (LFS), overall survival (OS), and GVHD-free/relapse-free survival (GRFS) were 1.62 (95% CI 1.34–1.95, p < 0.001), 1.59 (95% CI 1.3–1.93, p < 0.001) and 1.38 (95% CI 1.15–1.65, p < 0.001), respectively. We conclude that cytogenetic risk score predicts HSCT outcomes in sAML patients.
Similar content being viewed by others
Introduction
Secondary acute myeloid leukemia (sAML) comprises a heterogeneous group of diseases evolving from a preexisting hematologic disorder, predominantly myelodysplastic syndrome (MDS) or myeloproliferative disorders (MPD), or as a complication of prior cytotoxic chemotherapy or radiation therapy [1,2,3,4,5,6,7,8]. sAML has been associated with inferior outcomes compared to de novo AML due to factors such as the antecedent hematological disorder, older age, more aggressive biology of the leukemia with adverse cytogenetics and a high-risk mutation profile, lower chemotherapy susceptibility and reduced treatment tolerance, among others [1, 6, 7, 9]. Allogeneic stem hematopoietic cell transplantation (HSCT) remains the only known potentially curative therapy [10,11,12,13,14,15]. While HSCT is commonly employed in fit de novo AML patients with high-risk cytogenetics to mitigate relapse risk, significant post-transplant relapse rates are persist in this high-risk patient population [6,7,8, 16]. The cytogenetic risk category retains a pivotal role in predicting prognosis in AML patients owing to its tight association with survival and heightened risk of disease relapse [6,7,8, 16]. Currently, the prognosis of AML patients is determined by cytogenetic risk score and karyotypic abnormalities. However, it remains unclear whether the cytogenetic risk group, assessed at baseline, retains similar prognostic value in patients with high risk or active disease referred for HSCT [17,18,19]. We previously studied the impact of baseline cytogenetic risk on various transplantation outcomes in patients with relapsed/refractory (R/R) de novo AML with active disease undergoing HSCT. In multivariate analysis (MVA), the relapse incidence (RI) was significantly higher, and leukemia-free survival (LFS) and overall survival (OS), were significantly lower for patients with adverse-risk cytogenetics compared to those with intermediate-risk cytogenetics [17]. Furthermore, we assessed the prognostic impact of cytogenetics in patients with AML harboring FMS-like tyrosine kinase 3 internal tandem duplication (FLT3-ITD), as it remained unclear whether baseline cytogenetics significantly impacts the post-HSCT outcome in these patients. Our study demonstrated that the cytogenetic risk category retained its prognostic impact in transplanted high-risk FLT3-ITD AML patients. In MVA, LFS and OS were significantly lower and relapse higher in patients with adverse risk cytogenetics, and intermediate and compared with those with favorable risk cytogenetics [18]. Finally, we assessed the prognostic impact of cytogenetics risk in AML patients with positive pre-HSCT measurable residual disease (MRD). Once more, the cytogenetic risk score retained its prognostic impact in transplanted MRD+ AML patients [19]. However, no prior study has evaluated the prognostic impact of cytogenetic risk in sAML patients undergoing HSCT. This assessment is of particular clinical importance, as sAML is a high risk leukemia and thus, in contrast to de novo AML, with favorable risk cytogenetics is referred to HSCT in first complete remission. We therefore assessed the prognostic significance of the LeukemiaNet (ELN) 2022 cytogenetic risk score in patients with sAML undergoing HSCT from HLA matched siblings (MSD) or matched unrelated donors (MUD) using the dataset of the Acute Leukemia Working Party (ALWP) of the European Society for Blood and Marrow Transplantation (EBMT).
Patients and methods
Study design and data collection
This was a retrospective, multicenter analysis using the dataset of the ALWP of the EBMT. The EBMT is a voluntary working group of more than 600 transplant centers that are required to report all consecutive stem cell transplantations and follow-ups once a year. EBMT minimum essential data forms are submitted to the registry by transplant center personnel following written informed consent from patients in accordance with the centers’ ethical research guidelines. Data accuracy is assured by the individual transplant centers and by quality control measures such as regular internal and external audits. In addition, the study protocol was approved by each site and complied with country-specific regulatory requirements.
Eligibility criteria for this analysis included adult patients ≥18 years of age with sAML post-MDS or MPD in first complete remission (CR1) who underwent a first HSCT from a human leukocyte antigen (HLA) matched sibling donor (MSD) or 10/10 HLA matched unrelated donor MUD 2010 and 2022. Exclusion criteria were HSCT from other donor types (haploidentical or cord blood donor), prior HSCT, ex vivo T cell-depleted hematopoietic cell graft, and disease status beyond CR1 at the time of transplantation. Data collected included recipient and donor characteristics (age, gender, cytomegalovirus (CMV) serostatus, and Karnofsky performance status (KPS)), disease characteristics, year of transplant, type of conditioning regimen, stem cell source, and GVHD prophylaxis regimen. The conditioning regimen was defined as myeloablative (MAC) when containing total body irradiation (TBI) with a dose >6 Gray or a total dose of busulfan (Bu) > 8 mg/kg or >6.4 mg/kg when administered orally or intravenously, respectively. All other regimens were defined as reduced intensity conditioning (RIC) [20]. Grading of acute (a) GVHD was performed using established criteria [21]. Chronic (c) GVHD was classified as limited or extensive according to published criteria [22]. For this study, all necessary data were collected according to the EBMT guidelines, using the EBMT minimum essential data forms. A list of institutions contributing data to this study is provided in the Supplemental Appendix.
Statistical analysis
The median, range, and interquartile range (IQR) were used to express quantitative variables and frequency and percentage for categorical variables. The study endpoints were OS, LFS, relapse incidence (RI), non-relapsed mortality (NRM), and engraftment, aGVHD, cGVHD, and GVHD-free, relapse-free survival (GRFS). All endpoints were measured from the time of transplantation. Myeloid engraftment was defined as achieving an absolute neutrophil count of ≥0.5 × 109/L at day 30 for three consecutive days. Platelet engraftment was defined as achieving a platelet count of ≥20 × 109/L at day 60 for three consecutive days. OS was defined as time to death from any cause. LFS was defined as survival with no evidence of relapse or progression. NRM was defined as death from any cause without previous relapse or progression. We used modified GRFS criteria. GRFS events were defined as the first event among grade III-IV aGVHD, extensive cGVHD, relapse, or death from any other cause [23]. Patient, disease, and transplant-related characteristics were compared using the Mann–Whitney U test for numerical variables, and the chi-squared or Fisher’s exact test for categorical variables. The probabilities of OS, LFS, and GRFS were calculated using the Kaplan–Meier estimate. The RI and NRM were calculated using cumulative incidence functions in a competing risk setting, with death in remission being treated as a competing event for relapse. Early death was considered as a competing event for engraftment. To estimate the cumulative incidence of aGVHD or cGVHD, relapse, and death were considered as competing events. Multivariate analyses were performed using the Cox proportional-hazards regression model [24]. Results were expressed as the hazard ratio (HR) with a 95% confidence interval (95% CI). All p values were two-sided with a type 1 error rate fixed at 0.05. Statistical analyses were performed with SPSS 27.0 (SPSS Inc., Chicago, IL, USA) and R 4.3.2 (R Core Team Fifty (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/) [25].
Results
Patient, disease, and transplant-related characteristics
A total of 1119 patients met the inclusion criteria. The cytogenetic risk scores were as follows: intermediate in 829 patients and adverse in 284. Six patients with favorable cytogenetics were not included in the analysis. The median follow-up was 3.1 years (range, 2.9–3.7) for patients with intermediate and 4.0 years (range, 3–4.1) for those with adverse risk cytogenetics. The median age was 61.9 (range 18.5–74.9) vs. 61.0 (18.6-74.9) years (p = 0.20). Males comprised 62% and 55% of the intermediate- and adverse-risk groups, respectively (p = 0.043). The median year of the transplant was 2018 and 2017 (range, 2010–2021 in both) (p = 0.34). The antecedent hematological disease for all patients was MDS/MPD (p = 0.12). Donors were siblings in 34% vs. 38% and unrelated in 66% and 62%, respectively (p = 0.22). The graft source was mobilized peripheral blood stem cells (PB) in 94% and 97% of the patients with intermediate and adverse risk cytogenetics, respectively (p = 0.084). Performance status, patient and donor CMV seropositivity, and female-to-male combination did not differ between the groups (Table 1). The median time from diagnosis to HSCT was 4.5 (range 0.6–17.7) compared to 4.4 (0.9–16.6) months (p = 0.11). Sixty-one percent and 64% of the patients in both groups received RIC (p = 0.1), with busulfan/fludarabine (Flu) being the most frequent regimen for both groups (45% vs. 46%) to be followed by treosulfan/Flu (17% in both) (p = 058) (Supplementary Table S1). GVHD disease prophylaxis was cyclosporine A (CSA)/mycophenolate mofetil in 35% if the intermediate-risk group and 38% of the adverse-risk group, while CSA/methotrexate was used in 33% vs. 37%, respectively. Anti-thymocyte globulin was administered to 62% vs. 66% of patients, while post-transplant cyclophosphamide was given to 6.3% vs. 5.6%, respectively (p = 0.68) (Supplemental Table S2).
Transplantation outcomes
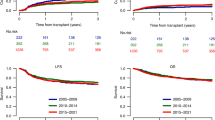
The day 30 cumulative incidence of neutrophil engraftment was 96.6% (95% CI 95.1– 97.6%) in the intermediate risk group and 95.3% (95% CI 92–97.3%) in the adverse risk group (Table 2A). The day 60 cumulative incidence of platelet engraftment was 95.3% (95% CI 93.6–96.6%) vs. 92.9% (95% CI 88.9–95.5%) of the patients, respectively (Table 2A). At day 180, the incidence of aGVHD grades II-IV and III-IV was 25.8% (95% CI 22.8–28.9%) vs. 22.6% (95% CI 17.8–27.7%) and 8.5% (95% CI 6.7–10.5) vs. 6.9% (95% CI 4.3–10.4%), respectively (Table 2B, Fig. 1). The 2-year cumulative incidence of all grades and extensive cGVHD was higher in the intermediate compared to the adverse cytogenetics risk group: 40.5% (95% CI 36.8–44.2%) vs. 23.7% (95% CI 18.4–29.4%) and 18.3% (95% CI 15.5–21.3%) vs. 9.3% (95% CI 5.9–13.5%), respectively (Table 2B, Fig. 1).
The 2-year NRM was 20.5% (95% CI 17.6–23.5%) in the intermediate risk group vs. 15.5% (95% CI 11.3–20.3%) in the adverse risk group (Table 2B, Fig. 2). All other HSCT outcomes were inferior in the adverse risk compared to the intermediate risk patients: The 2-year RI was 48.5% (95% CI 42.1–54.6%) vs. 24.6% (95% CI 21.5–27.9%) (Table 2B, Fig. 2). The 2-year LFS, OS, and GRFS were 35.9% (95% CI, 29.9–42%) vs. 54.9% (95% CI, 51.1–58.5%); 44.4% (95% CI, 38–50.6%) vs. 60.6% (95% CI, 56.8–64.2%) and 28.1% (95% CI, 22.3–33.9%) vs. 41.9% (95% CI, 38.2–45.6%), respectively (Table 2B, Fig. 2).
Multivariate analysis
The incidence of aGVHD grades II-IV and III-IV did not differ between the intermediate risk and adverse risk groups (HR = 0.91, 95% CI: 0.68–1.23; p = 0.55 and HR = 0.83 95% CI: 0.5–1.38; p = 0.47, respectively). At 2 years, the incidence of all grades and extensive cGVHD was higher in the intermediate compared to the adverse cytogenetics risk group (HR = 0.72, 95% CI: 0.53–0.98; p = 0.034 and HR = 0.58, 95% CI: 0.36–0.94; p = 0.027, respectively; Table 3). Myeloid engraftment was also higher in the intermediate risk compared to the adverse risk group (HR = 0.85, 95% CI: 0.72–1; p = 0.045). Two-year NRM did not differ, HR = 0.78 (95% CI 0.55–1.11, p = 0.166). All other HSCT outcomes were inferior in the patients with adverse risk compared to those with intermediate-risk cytogenetics: The HR for 2-year RI was 2.48 (95% CI 1.95–3.15, p < 0.001). The HRs for 2-year LFS, OS, and GRFS were 1.62 (95% CI 1.34–1.95, p < 0.001), 1.59 (95% CI 1.3–1.93, p < 0.001) and 1.38 (95% CI 1.15–1.65, p < 0.001), respectively (Table 3). Other significant prognostic factors in the MVA were KPS ≥ 90 which was a prognostic factor for lower NRM, and better LFS, OS and GRFS. Increasing age predicted a higher NRM and a decrease of LFS and OS. CMV seronegativity was associated with a better myeloid engraftment. Unrelated vs. sibling donor was associated with a higher incidence of cGVHD and inferior LFS, GRFS, and myeloid engraftment. Finally, RIC, compared to MAC, was associated with higher RI and lower GRFS (Table 3).
Cause of death
A total of 480 patients died during the study period—324 in the intermediate-risk patients group and 156 in the adverse-risk group (Table 4). The primary cause of death was the original disease, accounting for 50% and 76% of deaths in the intermediate risk and adverse risk groups, respectively. The second most common cause was HSCT-related complications (infection and GVHD), occurring in 46% and 22% of deaths, respectively (Table 4). Secondary malignancies accounted for 2.8% and 1.3% of the deaths, respectively. Other causes of death were rare (Table 4).
Discussion
In the current study we focused on a large homogenous group of 1119 patients with sAML transplanted from HLA matched sibling or unrelated donor while in CR1. We have demonstrated better outcomes for patients with intermediate-risk cytogenetics defined by ELN2022 compared to outcomes of sAML patients in adverse risk category with better LFS, OS, and GRFS primarly due to lower relapse rate. This finding is expected, as cytogenetic abnormalities detected at the time of diagnosis are well-known independent predictors of the initial response to therapy, remission duration, and OS in AML patients with conventional therapies [26, 27] as well as post-HSCT. However, most prior studies reported the correlation between cytogenetic risk category and post-HSCT survival mainly in de novo AML.
Yanada M and colleagues from Japan assessed the impact of cytogenetic risk on transplantation outcomes of a big cohort of 7812 AML patients demonstrating in MVA the significant effects of cytogenetic risk status on survival irrespective of donor type (related, unrelated, and umbilical cord blood) and even disease status at the time of transplantation (first or second complete remission, and more advanced disease status) [28]. The Center for International Blood and Marrow Transplant Research (CIBMTR), in collaboration with the National Marrow Donor Program (NMDP), assessed transplantation outcomes in 196 patients >60 years of age transplanted in second CR (CR2) (49 of them with sAML). They demonstrated in MVA that cytogenetic risk was the only independent risk factor for OS and relapse, with outcomes being significantly better in patients with intermediate-risk cytogenetics compared to those with unfavorable-risk cytogenetics [29]. The results reported by Tallman et al differ slighty. The authors assessed the impact of the cytogenetic risk group on HSCT outcomes in 261 patients with AML in CR1 and 299 patients in CR2 undergoing matched unrelated HSCT. For patients in first CR, the disease free survival (DFS) and OS at 5 years were similar for the favorable, intermediate, and unfavorable risk groups. In contrast, for patients transplanted in CR2, outcomes were modestly but not significantly better for those with favorable cytogenetics and relapse was somewhat more frequent in patients with unfavorable cytogenetics compared with favorable cytogenetics [30]. Notably, in our cohort focusing on sAML, only 6 patients had favorable cytogenetics risk scores and were therefore not included in the analysis, emphasizing the high risk of the leukemia and the different biology than de novo AML [1,2,3]. Addressing high risk AML, we at the ALWP conducted a retrospective analysis to determine the clinical outcomes of AML patients undergoing HSCT with respect to specific recurring cytogenetic abnormalities complemented with FLT3-ITD status. We analyzed a cohort of 8558 adult AML patients who underwent HSCT from either a matched sibling or a matched unrelated donor demonstrating inferior LFS and patients with adverse cytogenetics and the added prognostic significance of FLT3-ITD to baseline cytogenetics in AML patients undergoing HSCT [31]. Regarding FLT3, we subsequently performed a retrospective analysis of 1631 FLT3-ITD AML patients who underwent HSCT demonstrating the influence of cytogenetic risk category in transplanted FLT3-ITD AML patients. On MVA, LFS was significantly lower in patients with intermediate and adverse risk cytogenetics compared to those with favorable risk cytogenetics. OS was significantly lower in patients with adverse risk cytogenetics compared with patients with favorable risk cytogenetics with a trend toward lower OS in patients with intermediate risk cytogenetics compared to those with favorable risk cytogenetics. Finally adverse risk patients and intermediate risk patients experienced higher relapse rates compared with favorable risk patients [18]. Similar findings were observed in the high risk AML subset with pre HSCT positive AML: In MVA, adverse and intermediate/FLT3-ITD3 risk patients were more likely to experience disease relapse compared with favorable risk patients [19]. AML patients with the poorest prognosis are those undergoing HSCT while having active leukemia, either primary refractory or relapsed disease. Poiani M, on behalf of the ALWP, assessed the impact of cytogenetic risk in 2089 patients with refractory or relapsed AML, confirming the prognostic significance of cytogenetics in this very high-risk population. Specifically, compared to the favorable risk group, intermediate and adverse risk patients were associated with worse LFS and OS, as well as a higher incidence of relapse [32]. We subsequently confirmed these findings in AML patients undergoing non-T depleted haploidentical HSCT while having active disease. In MVA, the relapse rate was significantly higher, and LFS and OS significantly lower for patients with adverse risk cytogenetics compared to those with intermediate-risk cytogenetics [17]. As for the sAML subgroup analysis of the MRC 10 trial, which included 1,602 adults with AML (1,797 with de novo AML and 141 with sAML), it demonstrated that cytogenetic risk at diagnosis retained its predictive value in both de novo as well as sAML. Cytogenetic risk was found to be a key determinant of outcomes following HSCT in first CR [33]. Similarly, Armand P and colleagues assessed the prognostic significance of cytogenetic risk in 80 patients with therapy-related AML and reported that cytogenetics was the strongest prognostic factor for relapse and OS. Moreover, after accounting for cytogenetics, patients with therapy-related AML or MDS had an equivalent outcome to those with de novo disease [34]. Similar findings were recently reported in a cohort focusing on MDS, including high-risk patients [35]. Our study aligns with these initial pivotal studies that established the field but now focuses on the impact of cytogenetic risk, as defined by ELN 2022, in a homogenous group of recently transplanted sAML patients, predicting post-transplantation outcomes. Overall, cytogenetic risk predicts transplantation outcomes in high-risk AML, including patients harboring the FLT3+ mutation, those with positive MRD before transplantation as well AML patients active disease at time of transplantation. It is remarkable that, despite significant advances in the field of transplantation [36] and improved outcomes, cytogenetics remains the most important prognostic factor for transplantation success. Furthermore, it is noteworthy that cytogenetic risk is the strongest predicting factor in transplanted sAML patients as within this population many other predicting factors are operating including age, more aggressive biology of the leukemia, lower susceptibility and lower ability to tolerate chemotherapy, and others [1, 6, 7, 9].
The other prognostic factors we observed in the MVA, including age, KPS, CMV serostatus, dose intensity, and donor type, are in agreement with previous publications of allogeneic transplantations, including in sAML [11,12,13,14,15, 37,38,39]. Being retrospective and registry-based, this transplantation study has several limitations, including the risk of selection bias and the possibility of unavailable data that could not be considered, such as frontline therapies, molecular and MRD data. In summary, our study demonstrated that the cytogenetic risk score defined by ELN2022 predicts HSCT outcomes in a large cohort of sAML patients transplanted between 2010 and 2022. Patients with adverse cytogenetics exhibited significantly higher RI and lower LFS, OS, and GRFS compared to those with intermediate cytogenetics. Notably, the impact of the cytogenetic risk score in sAML is similar to that reported in de novo AML. Hopefully, with the recently approved novel agents for sAML [40], it will be possible to further improve outcomes including in patients with high-risk cytogenetics.
Data availability
AN, ATF, MM and FC had full access to all study data (available upon data-specific request).
References
Lindsley RC, Mar BG, Mazzola E, Grauman PV, Shareef S, Allen SL, et al. Acute myeloid leukemia ontogeny is defined by distinct somatic mutations. Blood. 2015;125:1367–76.
Granfeldt Ostgard LS, Medeiros BC, Sengelov H, Norgaard M, Andersen MK, Dufva IH, et al. Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukemia: A National Population-Based Cohort Study. J Clin Oncol. 2015;33:3641–9.
Hulegårdh E, Nilsson C, Lazarevic V, Garelius H, Antunovic P, Rangert Derolf Å, et al. Characterization and prognostic features of secondary acute myeloid leukemia in a population-based setting: a report from the Swedish Acute Leukemia Registry. Am J Hematol. 2015;90:208–14.
Winer ES. Secondary acute myeloid leukemia: a primary challenge of diagnosis and treatment. Hematol Oncol Clin North Am. 2020;34:449–63.
Dunbar AJ, Rampal RK, Levine R. Leukemia secondary to myeloproliferative neoplasms. Blood. 2020;136:61–70.
Dohner H, Wei AH, Appelbaum FR, Craddock C, Dinardo CD, Dombret H, et al. Diagnosis and management of AML in adults:2022 ELN recommendations from an international expert panel on behalf of ELN. Blood. 2022;140:1345–77.
Döhner, DiNardo H, Appelbaum CD, Craddock c FR, Dombret H, Ebert BL, et al. Genetic risk classification for adults with AML receiving less-intensive therapies: the 2024 ELN recommendations. Blood. 2024;144:2169–73.
Tazi Y, Arango-Ossa JE, Zhou Y, Bernard E, Thomas I, Gilkes A, et al. Unified classification and risk-stratification in Acute Myeloid Leukemia. Nat Commun. 2022;13:4622.
Martínez-Cuadrón D, Megías-Vericat JE, Serrano J, Martínez-Sánchez P, Rodríguez-Arbolí E, Gil C, et al. Treatment patterns and outcomes of 2310 patients with secondary acute myeloid leukemia: a PETHEMA registry study. Blood Adv. 2022;6:1278–95.
Litzow MR, Tarima S, Perez WS, Bolwell BJ, Cairo MS, Camitta BM, et al. Allogeneic transplantation for therapy-related myelodysplastic syndrome and acute myeloid leukemia. Blood. 2010;115:1850–7.
Sengsayadeth S, Labopin M, Boumendil A, Finke J, Ganser A, Stelljes M, et al. Transplant outcomes for secondary acute myeloid leukemia: acute leukemia working party of the European Society for Blood and Bone Marrow Transplantation Study. Biol Blood Marrow Transpl. 2018;24:1406–14.
Schmaelter A-K, Labopin M, Socié G, Itälä-Remes M, Blaise D, Yakoub-Agha I, et al. Inferior outcome of allogeneic stem cell transplantation for secondary acute myeloid leukemia in first complete remission as compared to de novo acute myeloid leukemia. Blood Cancer J. 2020;10:26.
Nagler A, Ngoya M, Jacques-Emmanuel G, Labopin M, Kröger N, Socié G, et al. Trends in the outcome of transplantation in patients with secondary acute myeloid leukemia: an analysis from the Acute Leukemia Working Party (ALWP) of the EBMT. Bone Marrow Transpl. 2022;57:1788–96.
Nagler A, Labopin M, Blaise D, Raiola AM, Corral LL, Bramanti S, et al Non-T-depleted haploidentical transplantation with post-transplant cyclophosphamide in patients with secondary versus de novo AML in first complete remission: a study from the ALWP/EBMT. J Hematol Oncol. 2023;16:58.
Nagler A, Labopin M, Tischer J, Raiola AM, Kunadt D, Vydra J, et al. Haploidentical transplantation in primary refractory/relapsed secondary vs de novo AML: from the ALWP/EBMT. Blood Adv. 2024;8:4223–33.
Shimony S, Stahl M, Stone RM. Acute myeloid leukemia: 2023 update on diagnostic, risk-stratification, and management. Am J Hematol. 2023;98:502–26.
Nagler A, Labopin M, Dholaria B, Ciceri F, Fraccaroli A, Blaise D, et al. Impact of cytogenetic risk on outcomes of non-T-Cell-depleted haploidentical hematopoietic cell transplantation in patients with relapsed or refractory acute myeloid leukemia. Transpl Cell Ther. 2022;28:773.e1–773.e8.
Nagler A, Labopin M, Craddock C, Socié G, Yakoub-Agha I, Gedde-Dahl T, et al. Cytogenetic risk classification maintains its prognostic significance in transplanted FLT3-ITD mutated acute myeloid leukemia patients: On behalf of the acute leukemia working party/European Society of Blood and Marrow Transplantation. Am J Hematol. 2022;97:274–82.
Nagler A, Labopin M, Canaani J, Niittyvuopio R, Socié G, Kröger N, et al. Cytogenetic risk score maintains its prognostic significance in AML patients with detectable measurable residual disease undergoing transplantation in remission: On behalf of the acute leukemia working party of the European Society for Blood and Marrow transplantation. Am J Hematol. 2020;95:1135–41.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transpl. 2009; 15: 1628-33.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transpl. 1995;15:825–8.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE. et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologicstudy of 20 Seattle patients. Am J Med. 1980;69:204–17.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP-EBMT analysis on patients with AML in remission. Bone marrow Transpl. 2016;51:610–1.
Kanate AS, Nagler A, Savani B. Summary of scientific and statistical methods, study endpoints and definitions for observational and registry-based studies in hematopoietic cell transplantation. Clin Hematol Int. 2019;2:2–4.
A language and environment for statistical computing. https://www.R-project.org/. R Core Team: R Foundation for Statistical Computing, Vienna, Austria; 2020.
Medeiros BC, Othus M, Fang M, Appelbaum FR, Erba. HPl. Cytogenetic heterogeneity negatively impacts outcomes in patients with acute myeloid leukemia. Haematologica. 2015;100:331–5.
Slovak ML, Kopecky KJ, Cassileth PA, Harrington, et al. Karyotypic analysis predicts outcome of pre-remission and post-remission therapy in adult acute myeloid leukemia: a Southwest Oncology Group/Eastern Cooperative Oncology Group Study. Blood. 2000;96:4075–83.
Yanada M, Mori J, Aoki J, Harada K, Mizuno S, Uchida N, et al. Effect of cytogenetic risk status on outcomes for patients with acute myeloid leukemia undergoing various types of allogeneic hematopoietic cell transplantation: an analysis of 7812 patients. Leuk Lymphoma. 2018;59:601–9.
Michelis FV, Gupta V, Zhang MJ, Wang HL, Aljurf M, Bacher U, et al. Cytogenetic risk determines outcomes after allogeneic transplantation in older patients with acute myeloid leukemia in their second complete remission: A Center for International Blood and Marrow Transplant Research cohort analysis. Cancer. 2017;123:2035–42.
Tallman MS, Dewald GW, Gandham S, Logan BR, Keating A, Lazarus HM, et al. Impact of cytogenetics on outcome of matched unrelated donor hematopoietic stem cell transplantation for acute myeloid leukemia in first or second complete remission. Blood. 2007;110:409–17.
Poiani M, Labopin M, Battipaglia G, Beelen DW, Tischer J, Finke J, et al. The impact of cytogenetic risk on the outcomes of allogeneic hematopoietic cell transplantation in patients with relapsed/refractory acute myeloid leukemia: on behalf of the acute leukemia working party (ALWP) of the European group for blood and marrow transplantation (EBMT). Am J Hematol. 2021;96:40–50.
Canaani J, Labopin M, Itälä-Remes M, Blaise D, Socié G, Forcade E, et al. Prognostic significance of recurring chromosomal abnormalities in transplanted patients with acute myeloid leukemia. Leukemia. 2019;33:1944–52.
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. Med Res Counc Adult Child’s Leuk Working Parties Blood. 1998;92:2322–33.
Armand P, Kim HT, DeAngelo DJ, Ho VT, Cutler CS, Stone RM, et al. Impact of cytogenetics on outcome of de novo and therapy-related AML and MDS after allogeneic transplantation. Biol Blood Marrow Transpl. 2007;13:655–64.
Koenecke C, Göhring G, de Wreede LC, van Biezen A, Scheid C, Volin L, et al. Impact of the revised International Prognostic Scoring System, cytogenetics and monosomal karyotype on outcome after allogeneic stem cell transplantation for myelodysplastic syndromes and secondary acute myeloid leukemia evolving from myelodysplastic syndromes: a retrospective multicenter study of the European Society of Blood and Marrow Transplantation. Haematologica. 2015;100:400–8.
Shouval R, Fein JA, Labopin M, Kröger N, Duarte RF, Bader P, et al. Outcomes of allogeneic haematopoietic stem cell transplantation from HLA-matched and alternative donors: a European Society for Blood and Marrow Transplantation registry retrospective analysis. Lancet Haematol 2019;6:e573–e584.
Kida M, Usuki K, Uchida N, Fukuda T, Katayama Y, Kondo T, et al. Outcome and risk factors for therapy-related myeloid neoplasms treated with allogeneic stem cell transplantation in Japan. Biol Blood Marrow Transpl. 2020;26:1543–51.
Bazarbachi A, Schmid C, Labopin M, Beelen D, Wolfgang Blau I, Potter V, et al. Evaluation of trends and prognosis over time in patients with AML relapsing after allogeneic hematopoietic cell transplant reveals improved survival for young patients in recent years. Clin Cancer Res. 2020;26:6475–82.
Nagler A, Labopin M, Dholaria B, Angelucci E, Afanasyev B, Cornelissen JJ, et al. Comparison of haploidentical bone marrow versus matched unrelated donor peripheral blood stem cell transplantation with post-transplant cyclophosphamide in Patients with Acute Leukemia. Clin Cancer Res. 2021;27:843–51.
Uy GL, Newell LF, Lin TL, Goldberg SL, Wieduwilt MJ, Ryan RJ, et al. Transplant outcomes after CPX-351 vs 7 + 3 in older adults with newly diagnosed high-risk and/or secondary AML. Blood Adv 2022;6:4989–93.
Acknowledgements
We thank all the EBMT centers and national registries for contributing patients to this study (Supplementary Appendix material). We also thank the data managers for their excellent work.
Funding
Open access funding provided by Tel Aviv University.
Author information
Authors and Affiliations
Contributions
AN wrote the manuscript, designed the study, and interpreted the data. ATF performed the statistical analyses, interpreted the data, and edited the manuscript. SK edited the manuscript. MM and FC designed the study, interpreted the data, and edited the manuscript. ME, NK, MS, JM, RFDL, IWB, TS, PR, TGD, GB, DB, AB, and JE reviewed the manuscript and provided clinical data. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no relevant conflict of interest and no competing financial interests. NK received research grant and honoraium from Neovii.
Ethics approval and consent to participate
The scientific boards of the ALWP of the EBMT approved this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Data presented in part at the EBMT 2025 meeting, Florence, Italy.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nagler, A., Ferhat, AT., Kayser, S. et al. Prognostic significance of cytogenetic risk score in patients with secondary acute myeloid leukemia undergoing allogeneic stem cell transplantation from HLA-matched unrelated donors: a study from the ALWP /EBMT. Bone Marrow Transplant 60, 1218–1227 (2025). https://doi.org/10.1038/s41409-025-02620-3
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41409-025-02620-3