Abstract
Aims Access to dental services in England has seen a gradual decline over recent years and this has become increasingly prevalent following the COVID-19 pandemic. This research provides a geographical assessment of access to National Health Service (NHS) dental services in local authorities across England, highlighting regions which require specific interventions to improve patient access.
Methods A Public Dental Access Index is created to assess the levels of patient access, combining metrics representing both the supply and demand of NHS dental services. The transparent nature of the Index allows health analysts/researchers to replicate and update the results using the most recent data as well as providing the opportunity to further develop the Index and assess change over time.
Results Local authorities which have the highest levels of access can be found outside of London in the South East and in regions between the Midlands and West Lancashire. Local authorities with the lowest levels of access are found in the South West, East of England and within London itself.
Discussion The spatial outputs from this research identify specific local authorities in England with low levels of access which should aid policymakers and commissioners to deliver targeted schemes to provide greater levels of access to patients most in need.
Key points
-
The paper quantifies the accessibility of NHS dentistry in England per local authority.
-
The primary demand and supply factors influencing access to NHS dental care for patients are outlined. The regions and local authorities with the most and least desirable levels of access are presented.
-
A reproducible index framework is presented, using only easy/free-to-access data, thus encouraging its replication and transferability.
-
Suggested means to work towards equitable levels of access across the county are proposed.
Similar content being viewed by others
Introduction
The problems surrounding dental care access in England, both during and following the COVID-19 pandemic, have been well-documented. These include children suffering for lengthy periods of time before receiving National Health Service (NHS) dental treatment and so-called ‘DIY' (do-it-yourself) dentistry, as portrayed by the mainstream media.1 In addition to this, it is clear that current dentists and undergraduate students/graduates are now favouring the provision of private care due to NHS dentistry being seen as overstretched and underfunded.2
The notion of access to NHS dental services can be split into four main concepts, which include the ‘opportunity for access', ‘realised access (utilisation)', ‘equity' and ‘outcomes'.3 Opportunities for access have seen considerable strain in England, with many reports suggesting a shortage of dentists to meet the needs of the population.4 The utilisation of dental care following the COVID-19 pandemic differs in rates across England, leaving a wider range of disparities between regions.5 The equity and outcomes of access to dental services also have a greater impact on those who are socioeconomically disadvantaged as they find difficulty in receiving necessary dental provision, often leading to poor oral health.5,6 Although dentistry is considered a type of primary care provided by the NHS, with the patient only contributing to some of the costs, the issues pertaining to the access and availability of NHS dental services have long been recognised and reported by both independent bodies and the United Kingdom (UK) Government.7,8
Dental access, as highlighted by the above four concepts, is a multifaceted issue which requires the use of multiple perspectives in order to truly quantify and assess the prevalence of access across England. Therefore, the creation of a bespoke composite index represents a means to capture and measure access by consolidating factors which relate to the supply and demand of NHS dentistry. This index produces a single numerical figure representing access to NHS dental care, mappable at a spatial scale. The geographical representation of the composite index score will aid analysts and policymakers to plan and address the disparities in access to care across the country.
Approach
This research designs and implements the Public Dental Access Index (PDAI) through following the agreed phases in index development, as set out by the Organisation for Economic Cooperation and Development,9 the only official guide to composite indicator development.
The purpose of any composite indicator is to produce a single and simplified score for a phenomenon or concept which is complex and multidimensional.10 The NHS dentistry landscape and the problems with accessing treatment are complex, thus necessitating the use of multiple perspectives in order to truly understand the level of access across England. The theoretical framework behind the creation of this Index is that there are various socioeconomic factors, as well as the availability of NHS dental services, in different areas, which contribute towards overall access for patients. Consequently, the creation of a specialised composite index will quantify the varying supply and demand factors which are inherently associated with the level of access, or lack thereof, across England and provide a tool to inform future policy and planning decisions.
A thorough review of academic, policy and related literature was undertaken to fully understand the characteristics associated with public dental access in/across England. The factors considered for inclusion in the PDAI can be split into two main categories: supply (dental contracts and dental workforce) and demand (real or perceived) for oral healthcare (socioeconomic factors relating to the general public).
In terms of supply characteristics, shortages in the dental workforce (recruitment and retention) were deemed to be important, given how this impacts patient access to timely care.11 Furthermore, the trend of dentists either leaving the NHS entirely or reducing the number of services they provide to reduce stress and improve mental health and wellbeing was also seen as important, especially following the COVID-19 pandemic.12,13 NHS dental contracts were also seen as particularly impactful and a barrier in maintaining and improving accessibility. The General Dental Services (GDS) contract implemented in 2006 changed how dentists were paid, moving from payment per item of treatment to an annual payment based on an agreed number of courses of treatment.14,15 This put dentists on a ‘treadmill' as they worked to meet their targets of delivering units of dental activity (UDAs) in order to avoid a clawback of payments.16 As a consequence, this introduced effective limits on the number of patients that could be seen within a year.
Research found that dentists' behaviour was impacted by the new model of contracted UDAs.17 Under the new model, dental practices continue to collect patient charges and pay these to the NHS; however, certain treatments for complex and resource intensive work (Band 3) do not lead to the necessary remuneration from the NHS to the dentist to cover many of the costs associated with these treatments. This has led to dentists providing more rudimentary treatments (Bands 1 and 2) to help them reach their UDA targets while also reducing the potential financial loss.18 Therefore, the contract reform has reduced dentists' ability to accept new patients given their limited number of contracted UDAs, and has also lessened their willingness to provide more complex preventive dental care, as treatments which are more financially viable for their practice are favoured.
With regards to demand, a noteworthy factor deemed to drive the need for dental services is the socioeconomic characteristics of a population. It is evident that oral health inequalities exist across England and more affluent individuals are more likely to seek preventive treatment than those deemed less affluent.19 Research suggests that adults employed in more manual occupations have limited time to visit a dental practice, which often results in a greater number of teeth being extracted over time.20,21 As well as this, poor oral health for children and adolescents has been linked to residential deprivation, despite attendance at appointments being the same as more affluent individuals.22 Similarly, physical access to practice is found to be important, with studies deeming short distances, particularly in deprived areas, and convenient transport (public or private) being critically important.23,24
Care was taken to only recommend factors for inclusion in the PDAI that are: 1) comprehensive and consistent in coverage (to ensure fair nationwide comparisons); and 2) freely available and in the public domain, or easily acquired through other means (to enable transparency and reproducibility, particularly with a view to the Index being updateable as/when new data becomes available).
Generally, the factors associated with dental access in England are publicly available at integrated care board and sub-integrated care board spatial scales. However, these spatial scales are rather broad and would provide little information on specific areas that are lacking in public dental access, making targeted interventions more challenging. Due to this, it was necessary to obtain data at a finer spatial resolution and the 2023 Lower Tier Local Authority District Scale (referred to as local authorities hereafter) was selected. Local authorities encompass areas such as Leeds, Manchester, Birmingham etc. Furthermore, with other indices also opting to use (or available at) the local authority scale (such as the new Health Index for England and summaries of the Index of Multiple Deprivation), like-for-like comparisons and validations can be undertaken.
This research opted to include six variables in the PDAI. The variables were sourced from the NHS Business Services Authority (BSA), GP (general practitioner) Patient Survey, Ministry of Housing, Communities and Local Government (MHCLG), and the Office for National Statistics (ONS). Table 1 presents the variables, plus information about the source, measurement and categorisation (demand, supply, or a combination).
Contractor datasets provided by NHS BSA include GDS, Personal Dental Services and PDS Plus.25 For the PDAI, only GDS contracts are counted as these provide the services that the typical patient requires.
The appointment success rates are split into four time periods after having an appointment. For the purpose of the PDAI, the time period selected is ‘after two years' as it includes the greatest number of respondents across the four categories.
The GP Patient Survey is also used, and this is an independent survey carried out by Ipsos on behalf of NHS England in order to improve health services based on patient feedback.26 The results from the survey are standardised to allow for comparisons between different practices, primary care networks and integrated care systems.26 The survey carried out in 2023 asked 2.6 million registered GP patients their views on NHS dentistry with a survey response rate of 29%.
Two additional datasets were used containing denominators and these provided a means to standardise the variables in Table 1. The selected denominators (total population and total households) facilitated the standardisation of all variables, either on a per household, per person, or per 10,000 of a population basis, as appropriate. The denominator variables were obtained from the 2021 census.27,28 Note that all data manipulation and mapping was undertaken using R, an open source software.
It should be noted again that the variables presented in Table 1 were sourced based on: 1) their general suitability for the context; and 2) their general availability and ease of interpretation for a non-expert user. Given that the Index has been designed to be replicated and updated as/when new data become available, a trade-off was required to ensure all data were fit for purpose while also being easy to source and process, without users needing to overcome any technical or access barriers.
As such, decisions were made on certain variables (such as car ownership as a proxy for ease of physical access to dental practice, and deprivation). Regarding car ownership, while alternative variables could have been used to capture physical access, such as distance between Middle-layer Super Output Area centroid and nearest dental practice using spatial software, replicating this for practitioners in the future may prove problematic. The selection of non-car ownership thus represents a simple measure of physical access, taking into account that this is the most likely means of travel to dental practice. Furthermore, the use of this variable over more complex distance measures also does not assume that patients use their nearest dental practice, as this may not be the case due to oversubscription or other factors.
In terms of deprivation, it is recognised by the authors that a relationship exists between deprivation and oral health ‘need'. While this relationship is linear, with the most deprived communities generally ‘needing' the most care, a similar relationship is not always observed between deprivation and oral health ‘demand'. As such ‘need' and ‘demand' can be regarded as related but different metrics. In addition, the provision of private dentistry further alters the ‘demand' for NHS dental care versus deprivation relationship, with those least deprived often seeking private care rather than NHS provision. However, in line with the purpose of the Index and its need to be replicable, updatable and easy to understand, the use of deprivation as a proxy for demand is deemed fair as the measure is freely available and does, on the whole, capture demand, albeit not perfectly at the extremes of the scale.
Following standardisation to ensure comparability, all variables were tested for multicollinearity in a bid to gauge any compounding effects within the Index. Compounding in this case refers to any variable pair with a particularly high correlation coefficient and thus potentially contributing the same or similar influence on the overall Index. For the purposes of this research, a high correlation coefficient is considered to be 0.75, which is similar to the ‘rule of thumb' set in other studies.29 All variable pairs satisfy this condition.
Skewness of variables was also considered given the influence outliers can have on the Index score. Households with no car was deemed to be skewed to the right (2.01) when assessed using the Fisher-Pearson standardised moment coefficient of skewness, likely due to particular locations in England which heavily rely on public transport, such as London. However, given the known importance of this variable, it was retained in the Index.
All variables were also assessed to ensure polarity (directionality) and it was confirmed that a high score in four of the six variables implied greater dental access, and a low score restricted access. In the remaining two variables (income deprivation and no car), values imply the reverse and as such, these variables were polarised to ensure a consistent meaning across component variable scores.
Following the above statistical due diligence, all variables underwent normalisation. This study used the min-max normalisation approach and thus rescaled all data points for each of the six variables onto a zero-to-one scale. This ensures uniformity and improved comparability between variables operating on different numerical scales or using different numerical units. The highest data point per variable is rescaled to the value 1 and the lowest data point to the value zero, and all other data points proportionally in between using the following equation:

The input variable data point, xraw, is subtracted by the lowest value of xi (mini) for the same variable. This is divisible by the product of the maximum value of xi (maxi) subtracted by mini, to produce xnorm where i = variable value from 1 to n.
Following the above data preparation phases, the final PDAI score was generated by aggregating the six variable scores per local authority. There are numerous means of aggregation; however, this research opted for the additive aggregation method due to its simplicity and ease of interpretation and replication.30 The final PDAI score was normalised onto a 0 (lowest access) to 100 (highest access) scale for further simplicity using the following equation, where xtotal is the raw index score following aggregation.

Results
The PDAI comprised six input variables (Table 1) and these individual standardised components can be seen mapped in Figure 1.
The supply variables (number of dentists and contracted UDAs, plus delivered UDAs which is primarily supply-led), display considerable variation. Higher proportions of dentists can be found in the South East, despite there being fewer contracted UDAs per 10,000 of the population, compared to other parts of the country. Despite this, the percentage of UDAs delivered is high. In contrast, the South West lacks the number of dentists per 10,000 of the population, excluding South Hams and Torridge. Interestingly, there is a higher number of contracted UDAs in the South West region compared to the rest of England; although, the overall delivery of UDAs is low. The local authorities located in the North of England share a similar pattern, albeit with better proportions. To the contrary, the local authorities in the East of England show low proportions across all categories, with authorities closer to London indicating improved proportions of dentists, contracted and delivered UDAs. The local authorities within London itself show higher numbers of dentists relative to the population size; although, the number of contracted UDAs vary in size. Most of London achieves a higher percentage of UDA delivery compared to other local authorities in England.
The demand variables (income deprivation scores and households with no car, plus appointment success rate which is largely demand-led) also display spatially varying results. Appointment success rates across England show that the majority of patients are successful in obtaining a dental appointment in a variety of locations in England, including local authorities in Midlands and Cheshire, West and South Yorkshire, Northumberland, plus local authorities in the South East surrounding London. Local authorities which lack the same level of success can be found within London itself, parts of Lincolnshire and Cumbria, the majority of the East of England and the entirety of the South West. Income deprivation is more concentrated in local authorities across Lancashire, Yorkshire, and Lincolnshire, as well as in and around County Durham. Outside of this trend, Birmingham, certain local authorities in London and several local authorities on the East of England coast, South East and South West display higher levels of deprivation. Similarly, the majority of households with no car are located in the North of England, with the highest proportion being in West and South Yorkshire, parts of Lancashire and the North West. Outside of this pattern, local authorities such as Birmingham, the London boroughs and smaller cities, such as Oxford and Cambridge, also see a higher proportion of households without cars, but for different reasons, given the provision and historical use of public and other modes of transport.
The six supply and demand variables consolidate to create the PDAI, which is presented in Figure 2. Local authorities are scored based on access to fundamental dental services and these scores are grouped into one of five categories (quintiles) to aid map interpretability.
Local authorities with the highest access score (in the 70-100) bracket are primarily located between the Midlands and West Lancashire, as well as local authorities surrounding the London region in the South East of England. There are certain outliers which show high levels of access compared to the overall spatial trend in Lincoln, Fareham and Havant.
Local authorities with the lowest levels of access are located in London and across the East and South West of England. Local authorities in the North and North East of England show a mix of moderate to low access, with authorities such as North Yorkshire, Northumberland, Calderdale and Kirklees displaying scores of 62-70 compared to Bradford, County Durham, Sunderland and Cumberland with scores of 0-42. There are some notable outliers for lower access in both the East of England and South West, with Broadland and South Hams showing higher access scores of 62-70 compared to surrounding areas.
The full results illustrated in Figure 2 are available in tabular form and are included in the paper repository.
Discussion
The holistic view of access to NHS dental services in England, shown in Figure 2, illustrates some standout insights. As a whole, a higher level of access can be seen in local authorities which are generally of greater wealth and are not located in the rural and coastal regions of England. In particular, the South West and the East of England display some of the lowest access scores, which correlates strongly with recent reports of poor dental access in areas, such as Bristol.31 The PDAI also indicates that lower scores are prevalent in England's major cities. This further highlights the local authorities which need specific intervention in order to improve overall dental access. The uniqueness of this Index makes it difficult to find existing indices to compare and contrast with, either for additional insight or validation purposes. However, when compared to the wider literature attempting to understand dental access, there are some notable similarities and differences in results. For instance, the higher levels of access in local authorities which surround London largely differs from the lower ‘realised access' found by O´Connor et al.32 based on delivered treatments. In addition, a comparison between the PDAI and the traffic light map produced by Jo et al.23 show similar variations in the assessment of access in local authorities, such as the London boroughs.
Table 2 and Table 3 indicate the best and worst performing local authorities, respectively, with regards to the PDAI.
On the whole, the PDAI presents results which support the wider discourse on the varying factors related to dental access and dental health, but their interplay is important to highlight. The South West of England, in general, presents low dental access scores. This is not solely influenced by a lack of dental professionals. The number of contracted UDAs is one of the highest per 10,000 in the country outside of the major cities. This suggests dentists in rural and coastal England are being burdened with larger contracts to meet the demands of their patients, which is reflected in the percentage of UDAs delivered. Subsequently, local authorities which are more rural and costal look unattractive to new graduates seeking employment and this same pattern is driving the existing dentists out as they try to avoid the stressful workload.
The lack of access identified within the major cities in England (including London, Birmingham, Manchester, Liverpool and Leeds) is driven by various interconnected factors. Excluding London and Leeds, the supply variables do not present low values, with higher contracted UDAs being awarded and a large percentage of UDAs being delivered. However, the demand variables provide particularly low values, thus leading to the lack of access in these local authorities, supporting claims made by Cheema and Sabbah whereby socioeconomic factors are of particular importance.20 Furthermore, in such areas, higher populations and increased levels of deprivation make the need for more reactive (urgent) as opposed to preventive (scheduled) care more likely, thus increasing the number of appointment requests.
Additionally, not owning a car makes transport to and from the dental practices much more difficult in some locations, particularly for the older person. In London, the majority of boroughs have a sufficient supply of dentists, but the lack of contracted UDAs, in addition to the effect of the demand variables seen in the other major cities, contributes towards the low dental access scores.
Conclusion
This research has presented a bespoke dental access Index (the PDAI) combining a mix of both demand and supply variables to score/rank local authorities in England based on perceived access to primary NHS dental care. This builds on previous studies where dental access has been assessed using only standalone methods and variables.
The work has made use of accessible sources of data, the selection of which was driven by a thorough review of academic, policy and related literature to understand the primary factors influencing access to care. The use of accessible datasets allows for the Index to be replicated (for transparency) and reproduced using new data when available to benchmark and understand change over time, including the influences of any policy changes. The Index is likely to be of use for integrated care boards exploring specific interventions and commissioning, with a view to improving patient access to NHS dental services and recovering dental access post COVID-19.
The work has highlighted local authorities most in need of intervention and areas where access is currently favourable. Areas scoring poorly in the Index ought to be considered for additional resource allocation, incentives for dental professionals to provide care (and relocate, as needed) and other short-term measures to lessen the inequalities that currently exists through improving supply.
Longer-term, this research suggests further investigation into the interrelationships between the demand and supply variables, with a view to identifying cost-effective actions that are not simply about providing additional services or capacity. Working with local government and planning authorities to lessen the impact of certain demand variables on the Index may be as impactful as investing in additional dentists or dental contracts. Such demand-impacting initiatives may include public education on the importance of scheduled check-up appointments (preventive care) to lessen the need for more expensive and schedule-impacting emergency and reactive care. Any low-cost investment in this or similar initiatives is likely to be offset by reduced demand on practice and emergency care services when patients begin to display distressing symptoms. Such investigative work may also lead to an enhanced PDAI whereby variables can be weighted based on their importance, driven by intelligence garnered from the sector.
The general failure to implement the recommendation put forward by the National Institute for Health and Care Excellence33 regarding the frequency of recall appointments for ‘healthy' patients is also not conducive to improved access, despite a requirement for dentists to declare such personalised recommendations via FP17 forms.34 Estimates suggest that recalling healthy patients every 12 months (as opposed to six months, as is generally the case now) would reduce demand and consequently generate thousands more appointments across the system. The results of the PDAI and associated research presented in this paper may prompt further debate on the implementation of this guidance.
Understanding the interrelationships between the supply and demand variables provides the opportunity through which overall access to care can be improved. Despite what may be perceived, it is not simply the case that additional provision of dentists or delivered UDAs will improve access to the desired levels. The demand variables also play a very important role in the overall Index score, and as such, area deprivation and travel/transport to practice impact a patient's need and ability to access care.
While this research has focused exclusively on access to fundamental NHS-run dental care, it is important to acknowledge the role of private dental care. Dentists providing and patients accessing such care may impact on both the supply of and demand for NHS dentistry, particularly within less-deprived communities where the uptake of private care is known to be at its highest. Capturing such information from within the public domain, thus in-keeping with the remit of ensuring the PDAI is both replicable and updatable, is challenging but it does represent a means to improve the Index for future iterations, subject to data availability.
Data availability
The data that support the findings of this study are available in the public domain. The sources are clearly flagged with the manuscript (see Table 1). The data mapped in Fig. 1 is also included in the paper repository.
References
Green R, Fagg J, Hughes D. Children waiting over a year in pain for NHS tooth removal. 2023. Available at https://www.bbc.co.uk/news/health-66095984 (accessed December 2023).
British Dental Association Nearly half of dentists severing ties with NHS as government fails to move forward on reform. 2022. Available at https://www.bda.org/media-centre/nearly-half-of-dentists-severing-ties-with-nhs-as-government-fails-to-move-forward-on-reform/ (accessed December 2023).
Harris R V. Operationalisation of the construct of access to dental care: a position paper and proposed conceptual definitions. Community Dent Health 2013; 30: 94-101.
Goodier M, Ambrose T. Parts of England have one NHS dentist for thousands of people, data shows. 2022. Available at https://www.theguardian.com/society/2022/aug/25/england-nhs-dentists-dental-deserts-data (accessed May 2024).
Joseph M. From crisis to care: navigating dental access disparities in NHS England post-COVID-19. Br Dent J 2023; 235: 324.
Public Health England. Inequalities in oral health in England: summary. 2021. Available at https://www.gov.uk/government/publications/inequalities-in-oral-health-in-england/inequalities-in-oral-health-in-england-summary (accessed May 2024).
Healthwatch. Lack of NHS dental appointments widens health inequalities. 2022. Available at https://www.healthwatch.co.uk/news/2022-05-09/lack-nhs-dental-appointments-widens-health-inequalities (accessed May 2024).
UK Parliament. Access to NHS dentistry. 2022. Available at https://commonslibrary.parliament.uk/research-briefings/cdp-2022-0029/ (accessed May 2024).
Organisation for Economic Co-operation and Development. Handbook on constructing composite indicators: methodology and user guide. 2008. Available at https://www.oecd.org/en/publications/handbook-on-constructing-composite-indicators-methodology-and-user-guide_9789264043466-en.html (accessed April 2025).
Drowley C, Burns L. Dementia in England: quantifying and analysing modifiable risk. Arxiv 2022; DOI: 10.48550/arXiv.2204.05863.
Evans D, Burns L, Mills I, Bryce M, Hanks S. Recruitment and retention in dentistry in the UK: a scoping review to explore the challenges across the UK, with a particular interest in rural and coastal areas. Br Dent J 2023; DOI: 10.1038/s41415-022-5406-0.
Gallagher J E, Colonio-Salazar F B, White S. Supporting dentists' health and wellbeing - a qualitative study of coping strategies in ‘normal times'. Br Dent J 2021; DOI: 10.1038/s41415-021-3205-7.
Gallagher J E, Colonio-Salazar F B, White S. Supporting dentists' health and wellbeing - workforce assets under stress: a qualitative study in England. Br Dent J 2021; DOI: 10.1038/s41415-021-3130-9.
Steele J. NHS dental services in England. 2009. Available at http://www.sigwales.org/wp-content/uploads/dh_101180.pdf (accessed December 2023).
Tickle M. Revolution in the provision of dental services in the UK. Community Dent Oral Epidemiol 2012; 40: 110-116.
Tickle M, McDonald R, Franklin J, Aggarwal V R, Milsom K, Reeves D. Paying for the wrong kind of performance? Financial incentives and behaviour changes in National Health Service dentistry 1992-2009. Community Dent Oral Epidemiol 2011; 39: 465-473.
Holmes R D, Steele J G, Donaldson C, Exley C. Learning from contract change in primary care dentistry: a qualitative study of stakeholders in the north of England. Health Policy 2015; 119: 1218-1225.
Chestnutt I G, Davies L, Thomas D R. Practitioners' perspectives and experiences of the new National Health Service dental contract. Br Dent J 2009; DOI: 10.1038/sj.bdj.2009.354.
Cookson R, Propper C, Asaria M, Raine R. Socio-economic inequalities in health care in England. Fiscal Stud 2016; 37: 371-403.
Cheema J, Sabbah W. Inequalities in preventive and restorative dental services in England, Wales and Northern Ireland. Br Dent J 2016; 221: 235-239.
Ahmadi O, Machuca C, Sabbah W. Socioeconomic inequality in the provision of health advice in dental setting in England, Wales and Northern Ireland. Patient Educ Couns 2019; 102: 2068-2072.
Rouxel P, Chandola T. Socioeconomic and ethnic inequalities in oral health among children and adolescents living in England, Wales and Northern Ireland. Community Dent Oral Epidemiol 2018; 46: 426-434.
Jo O, Kruger E, Tennant M. Disparities in the geographic distribution of NHS general dental care services in England. Br Dent J 2021; DOI: 10.1038/s41415-021-3005-0.
Jo O, Kruger E, Tennant M. Public transport access to NHS dental care in Great Britain. Br Dent J 2021; DOI: 10.1038/s41415-021-3002-3.
NHS Business Services Authority. Freedom of information act: FOI 01702. 2024.
GP Patient Survey. Homepage. 2023. Available at https://www.gp-patient.co.uk (accessed February 2024).
Office for National Statistics. Number of households. 2023. Available at https://www.ons.gov.uk/datasets/TS041/editions/2021/versions/3#version-history (accessed February 2024).
Office for National Statistics. Sex. 2023. Available at https://www.ons.gov.uk/datasets/TS041/editions/2021/versions/3#version-history (accessed February 2024).
Schober P, Boer C, Schwarte L A. Correlation coefficients: appropriate use and interpretation. Anesth Analg 2018; 126: 1763-1768.
Greco S, Ishizaka A, Tasiou M, Torrisi G. On the methodological framework of composite indices: a review of the issues of weighting, aggregation, and robustness. Soc Indicators Res 2019; 141: 61-94.
Boobyer L, Lamdin F. Bristol: queues for NHS dental treatment hit third day. 2024. Available at https://www.bbc.co.uk/news/uk-england-bristol-68225400 (accessed May 2024).
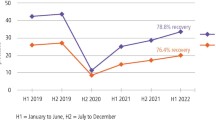
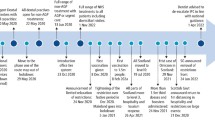
O'Connor R, Landes D, Harris R. Trends and inequalities in realised access to NHS primary care dental services in England before, during and throughout recovery from the COVID-19 pandemic. Br Dent J 2023; DOI: 10.1038/s41415-023-6032-1.
National Institute for Health Care Excellence. Dental checks: intervals between oral health reviews. 2004. Available at https://www.nice.org.uk/guidance/cg19 (accessed November 2024).
NHS England. First stage of dental reform. 2022. Available at https://www.england.nhs.uk/publication/first-stage-of-dental-reform/ (accessed December 2024).
MHCLG 2019. English indices of deprivation 2019. 2019. Available at https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed February 2024).
Office for National Statistics. Car or van availability. 2023. Available at https://www.ons.gov.uk/datasets/TS045/editions/2021/versions/4/filter-outputs/6e5d1869-6110-4a41-82fa-fa6e310e7d16#get-data (accessed February 2024).
Office for National Statistics. Local Authority Districts (December 2023) Boundaries UK BFC. Available at https://geoportal.statistics.gov.uk/datasets/ons::local-authority-districts-december-2023-boundaries-uk-bfc-2/about (accessed February 2024).
Acknowledgements
The authors acknowledge and thank both the NHS Business Services Authority and NHS England for the support and provision of data required to carry out this research. AH completed this work as part of a data-led final year dissertation, and a shortened version is presented in this paper.
The final results/data from the PDAI are available in the paper repository, accessible at: https://zenodo.org/records/15384023
Author information
Authors and Affiliations
Contributions
AH led the work and acted as first author. LB provided supervision, guided the research from inception to completion, and supported the transition from written dissertation to academic publication.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest. This research was undertaken following a block ethical approval, approved by the University of Leeds and Faculty of Environment Ethics Committee for all relevant student-facing research on GEOG3630: Human Geography Dissertation (Quantitative Methods) module (Ref: AREA FREC 2023-0528-555). A more in-depth ethical approval was not required given the use of solely publicly available aggregate data (see Table 1 for all sources of data used in this research). No study participant consent was required to facilitate this research, given the use of solely publicly available aggregate data (see Table 1 for all sources of data used in this research).
Supplementary Information
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2025.
About this article
Cite this article
Hafesji, A., Burns, L. Waiting in line for a check-up: evaluating access to NHS dental services in England. Br Dent J (2025). https://doi.org/10.1038/s41415-025-8320-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-025-8320-4