Abstract
Background
Patients with RAS wild-type (WT), left-sided metastatic colorectal cancer (mCRC), negatively hyperselected for anti-EGFR resistance alterations, benefit most from anti-EGFR-based first-line treatment. The predictive impact of these stratification parameters on maintenance strategy efficacy is unclear.
Methods
This pooled analysis included individual patient data from the PanaMa (NCT01991873) and Valentino (NCT02476045) phase 2 trials. Patients with RAS WT mCRC received FOLFOX plus Panitumumab induction therapy followed by maintenance with 5-fluorouracil/leucovorin (5-FU/LV) plus Panitumumab vs. 5-FU/LV monotherapy (PanaMa) or Panitumumab monotherapy (Valentino). Outcomes included progression-free survival (PFS) and overall survival (OS). Subgroup analyses examined primary tumor sidedness (left vs. right) and hyperselection status (negative vs. altered).
Results
Among 607 patients receiving induction, sidedness and hyperselection status were available for 589 and 511 patients, respectively. Left-sided and negative hyperselected tumors were observed in 80.2% and 63.9% of patients, respectively. Panitumumab-based maintenance improved PFS in left-sided, negative hyperselected patients compared to 5-FU/LV alone, with no OS differences. PFS and OS were comparable for Panitumumab alone vs. Panitumumab plus 5-FU/LV.
Conclusion
Tumor sidedness and hyperselection status significantly influence maintenance strategy efficacy in mCRC. For left-sided, negative hyperselected patients, Panitumumab monotherapy may optimize efficacy while minimizing toxicity. Further investigation into the relative contribution of individual hyperselection parameters in this setting is warranted.
Similar content being viewed by others
Introduction
In the therapeutic management of patients with RAS and BRAF wild-type (WT) metastatic colorectal cancer (mCRC), chemotherapy in combination with monoclonal antibodies directed against vascular endothelial growth factor (VEGF) or epithelial growth factor receptor (EGFR) are standard options in the first-line setting [1]. Previous studies have highlighted the impact of left-sided primary tumor location to identify patients who benefit from the selection for anti-EGFR therapy combination [2,3,4]. Moreover, negative hyperselection of patients by the absence of gene alterations associated with anti-EGFR resistance (i.e. mutations in BRAF V600E, KRAS, NRAS, PIK3CA, and PTEN, amplifications in HER2 and MET, and fusions in ALK, RET, and NTRK1) can optimize treatment stratification [5,6,7,8,9].
De-intensification of first-line treatment with oxaliplatin-based doublet or triplet therapies using maintenance strategies demonstrated improved tolerability and quality of life without compromising survival outcomes, compared to the continuation of intensive induction therapy until disease progression or treatment holidays [10,11,12,13]. After anti-EGFR based first-line treatment, several maintenance strategies were previously investigated, ranging from single-agent anti-EGFR antibody, fluoropyrimidine monotherapy or the combination of 5-fluorouracil/leucovorin (5-FU/LV) with an anti-EGFR antibody [14,15,16,17,18,19,20].
Based on the evidence from multiple phase 2 randomized clinical trials, the current European Society of Medical Oncology (ESMO) consensus guideline recommends maintenance therapy with 5-FU/LV plus an anti-EGFR after FOLFOX (5-FU/LV and oxaliplatin) plus anti-EGFR induction [1, 16, 18, 21]. In a previous pooled analysis of four randomized clinical trials investigating anti-EGFR based maintenance strategies, the combination of 5-FU/LV plus an anti-EGFR was confirmed as the optimal treatment strategy in this setting, especially in patients with stable disease to induction therapy, right-sided primary tumors or BRAF mutated status [21]. However, the combined impact of primary tumor sidedness and hyperselection status on the efficacy of maintenance strategies such as anti-EGFR or 5-FU/LV mono- or combination-therapy remains unclear. Given the highest predicted benefit of additional anti-EGFR based first-line in patients with left-sided primary tumors and absence of alterations associated with resistance to anti-EGFR treatment, the magnitude of the benefit of 5-FU/LV added to anti-EGFR maintenance in this subgroup is uncertain according to the risk/benefit ratio.
In this international individual patient data (IPD) pooled analysis of the randomized PanaMa (NCT01991873) and Valentino (NCT02476045) phase 2 trials that investigated anti-EGFR or 5-FU/LV mono- or combination maintenance regimens, we aimed to understand the individual and combined prognostic value of primary tumor sidedness and hyperselection status, and their predictive impact on the efficacy outcomes of the individual maintenance strategies, especially in the left-sided, negative hyperselected subgroup.
Results
Patient characteristics
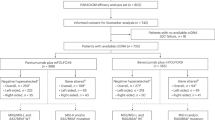
A total of 607 (PanaMa: 378; Valentino: 229) patients received induction therapy. Of these, valid information on primary tumor sidedness and hyperselection status was available for 589 (PanaMa 360; Valentino: 229) and 511 (PanaMa: 303; Valentino: 208), respectively (Fig. 1, Induction set). Of these, 487 (80.2%) and 388 (63.9%) comprised the left-sided and negative hyperselected induction set, respectively (Fig. 1, Table 1).
A total of 412 (PanaMa: 248; Valentino: 164) patients received maintenance therapy. Of these, valid information on primary tumor sidedness and hyperselection status was available for 401 (PanaMa: 237; Valentino: 164) and 360 (PanaMa: 202; Valentino: 158), respectively (Fig. 1, Maintenance set). Of these, 336 (83.8%) and 287 (79.7%) comprised the left-sided and negative hyperselected maintenance set, respectively (Fig. 1, Supplementary Table 1).
Baseline characteristics of subgroups by primary tumor sidedness (left- and right-sided) and hyperselection status (negative hyperselected and gene altered) revealed significantly increased fractions of female patients in the right-sided subgroup (Chi-square P < 0.001; Table 1); liver-limited disease in the left-sided, and the negative hyperselected subgroups, respectively (Chi-square P = 0.025 and Chi-square P = 0.029; Table 1). Remaining baseline characteristics were well comparable across all subgroups (Table 1).
Prevalence of genomic alterations
In 511 patients with available hyperselection status, a total of 136 genomic alterations were detected across 123 (24.1%) patients. Mutations were detected with a prevalence of BRAF V600E, N = 42 (34.2%); PIK3CA, N = 31 (25.2%); RAS, N = 29 (23.6%); PTEN, N = 14 (11.4%); AKT1, N = 5 (4.1%), ERBB2, N = 1 (0.8%). Overexpression/amplification of HER2 was detected in 14 patients (11.4%; Fig. 2; Supplementary Table 2). In 12 (9.8%) patients, more than 1 alteration was detected, of which 1 (0.8%) patient, had 3 detectable alterations (Fig. 2; Supplementary Table 2).
Prognostic impact of primary tumor sidedness and hyperselection status on efficacy of induction therapy
Response rates to induction treatment were significantly higher in patients with left-sided primary tumors compared to those with right-sided primaries (69.2% vs. 49.0%; Chi-square P < 0.001; Table 1). Significantly higher response rates to induction treatment were also observed in patients in the negative hyperselected group compared to those in the gene altered group (69.1% vs. 55.3%; Chi-square P = 0.005; Table 1).
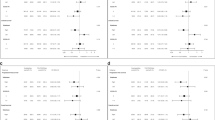
In patients receiving induction therapy, both left-sided primary tumor versus right-sided and negative hyperselected status versus gene altered status were associated with a significantly prolonged induction PFS (HR: 0.74; 95% CI: 0.59–0.93; P = 0.009 and HR: 0.65; 95% CI: 0.50–0.85; P < 0.001, respectively; Fig. 3a, b) and induction OS (HR: 0.60; 95% CI: 0.47–0.76; P < 0.001 and HR: 0.57; 95% CI: 0.43–0.75; P < 0.001, respectively; Fig. 3c, d). Combining sidedness with hyperselection, the best outcomes in terms of induction PFS and induction OS were observed in the left-sided, negative hyperselected subgroup, compared to worst outcomes in the right-sided, gene altered subgroup. Patients in the left-sided, negative hyperselected subgroup, compared to the right-sided, gene altered subgroup, significant benefits were noted in terms of induction PFS (HR: 0.53; 95% CI: 0.38–0.74; P < 0.001; Fig. 3e) and induction OS (HR: 0.37; 95% CI: 0.26–0.51; P < 0.001; Fig. 3f). In the left-sided, negative hyperselected subgroup, compared to the left-sided, gene altered, there was a significant benefit in induction PFS and induction OS (HR: 0.63; 95% CI: 0.48–0.83; P < 0.001 and HR: 0.62; 95% CI: 0.47–0.83; P < 0.001, respectively; Fig. 3e, f) and a numerical benefit in terms of induction PFS and induction OS compared to the right-sided, negative hyperselected subgroups (HR: 0.85; 95% CI: 0.62 - 1.17; P = 0.297 and HR: 0.82; 95% CI: 0.58–1.15 P = 0.255, respectively; Fig. 3e, f). In the right-sided population, patients in the negative hyperselected subgroup had numerically improved induction PFS (HR: 0.81; 95% CI: 0.65–1.00; P = 0.054; Fig. 3e) and significantly prolonged induction OS (HR: 0.70; 95% CI: 0.56–0.89; P = 0.002; Fig. 3f), compared to the gene altered subgroup.
Restricting the analysis to alterations with established impact on anti-EGFR efficacy routinely tested in clinical practice (RAS, BRAF V600E, HER2) maintained the prognostic significance of negative hyperselection and primary tumor sidedness, aligning with the findings obtained using the full alteration panel (Supplementary Table 3).
Impact of primary tumor sidedness and hyperselection status on the efficacy of maintenance strategies
In patients receiving maintenance therapy, a left-sided primary tumor was associated with a significant benefit in maintenance PFS in patients receiving 5-FU/LV plus Panitumumab (HR: 0.72; 95% CI: 0.56–0.93; P = 0.010; Fig. 4a) or Panitumumab alone (HR: 0.68; 95% CI: 0.49–0.95; P = 0.049; Fig. 4a) when compared to 5-FU/LV monotherapy, while no significant benefit in maintenance OS was noted (Fig. 4b). In patients with left-sided primary tumors, the addition of 5-FU/LV to Panitumumab maintenance was not associated with a significant benefit in maintenance PFS or maintenance OS (HR: 1.06; 95% CI: 0.78–1.43; P = 0.680 and HR: 1.11; 95% CI: 0.80–1.54; P = 0.584, respectively; Fig. 4a, b). In patients with right-sided primary tumors, maintenance PFS and maintenance OS were comparable irrespective of maintenance treatment, except for a significant maintenance OS benefit for the addition of Panitumumab to 5-FU/LV (HR: 0.59; 95% CI: 0.27–0.94; P = 0.029; Supplementary Fig. 1a, b).
a Progression-free survival, b overall survival of patients with left-sided primary tumors. c Progression-free survival, d overall survival of patients with negative hyperselected status. e Progression-free survival, f overall survival of patients with combination of left-sided primary tumors and negative hyperselected status.
The negative hyperselected subgroup showed a significant improvement in maintenance PFS in patients receiving 5-FU/LV plus Panitumumab (HR: 0.68; 95% CI: 0.51–0.91; P = 0.009; Fig. 4c) or Panitumumab alone (HR: 0.63; 95% CI: 0.44–0.91; P = 0.028; Fig. 4c) when compared to 5-FU/LV monotherapy, while no significant benefit in maintenance OS was noted (Fig. 4d). In patients with negative hyperselected tumors, the addition of 5-FU/LV to Panitumumab maintenance was not associated with a significant benefit in maintenance PFS or maintenance OS (HR: 1,08; 95% CI: 0.78–1.50; P = 0.604 and HR: 0.89; 95% CI: 0.63–0.126; P = 0.486, respectively; Fig. 4c, d). In patients in the gene altered subgroup, maintenance PFS and maintenance OS were comparable irrespective of maintenance treatment (Supplementary Fig. 2a, b).
In the left-sided, negative hyperselected subgroup, there was a significant improvement in maintenance PFS in patients receiving 5-FU/LV plus Panitumumab (HR: 0.67; 95% CI: 0.49–0.90; P = 0.010; Fig. 4e) or Panitumumab alone (HR: 0.58; 95% CI: 0.39–0.85; P = 0.010; Fig. 4f) when compared to 5-FU/LV monotherapy, while no significant benefit in maintenance OS was noted (Fig. 4f). However, in the left-sided, negative hyperselected subgroup, the addition of 5-FU/LV to Panitumumab maintenance was not associated with a benefit in maintenance PFS (median PFS, Panitumumab monotherapy: 9.4 months; 95% CI: 7.5–11.3 and median PFS, 5-FU/LV plus Panitumumab: 8.8 months; 95% CI: 7.1–10.5; HR: 1.16; 95% CI: 0.82–1.64; P = 0.371; Fig. 4e) or maintenance OS (median OS, Panitumumab monotherapy: 39.0 months; 95% CI: 24.0–56.0 and median OS, 5-FU/LV plus Panitumumab: 33.7 months; 95% CI: 27.0–40.5; HR: 1.06; 95% CI: 0.73–1.54; P = 0.795; Fig. 4f), irrespective of the inclusion of BRAF V600E into the gene altered panel (Supplementary Table 4).
In the right-sided subgroup, stratification of hyperselection status by BRAF V600E status, restriction to alterations with established impact on anti-EGFR efficacy routinely tested in clinical practice (RAS, BRAF V600E, HER2), and including all alterations revealed significantly improved PFS and OS in patients without BRAF V600E receiving 5-FU/LV plus Panitumumab compared to those with BRAF V600E (Supplementary Table 5). As the remaining hyperselection definitions showed only a numerical trend, these findings underscore the predictive impact of BRAF V600E status in this subgroup.
Restricting the analysis to alterations with established impact on anti-EGFR efficacy routinely tested in clinical practice (RAS, BRAF V600E, HER2) maintained the significant impact of negative hyperselection and primary tumor sidedness, aligning with the findings obtained using the full alteration panel (Supplementary Table 6).
In patients receiving 5-FU/LV plus Panitumumab as maintenance therapy, the pooled analysis demonstrated that hyperselection status and primary tumor sidedness significantly impacted treatment outcomes. In contrast, analyses of the individual trial cohorts did not reach statistical significance for impact of these factors on maintenance treatment outcomes (Supplementary Table 7).
Discussion
This IPD pooled analysis of the PanaMa and Valentino trials provides intriguing insights into the prognostic and predictive roles of primary tumor sidedness and hyperselection status in patients with RAS WT mCRC receiving an anti-EGFR and oxaliplatin-based first-line treatment followed by maintenance strategy. Results of this analysis confirm the prognostic impact of these stratification factors during induction therapy in terms of PFS and OS and outline their potential to predict maintenance treatment efficacy in terms of PFS, especially in the left-sided, negative hyperselected subgroup.
Our results verify that among patients receiving anti-EGFR and FOLFOX-based first-line treatment, those with left-sided primary tumors and negative hyperselected status have a more favorable prognosis compared to those with right-sided, gene-altered tumors. These findings align with previous studies highlighting the importance of tumor location and hyperselection status in predicting response to anti-EGFR based first-line therapies [2,3,4,5,6, 8, 22, 23]. Primary tumor sidedness is indicated in guidelines as a selection factor for the first-line treatment choice and its prognostic value was confirmed in this IPD pooled analysis [1]. Additional molecular selection beyond sidedness is fundamental to optimize RAS wild-type mCRC patient stratification in the maintenance setting, as previously reported [7, 9]. The combination of both factors underlined their prognostic potential and confirmed the left-sided, negative hyperselected as the best and right-sided, gene altered as the worst subgroup in terms of PFS and OS outcomes for an anti-EGFR-based first-line strategy. This was underlined by the enrichment of patients with negative hyperselected status in patients in the maintenance set as compared to the induction set.
However, it is worth noting that in a subset of patients in both trials RAS and BRAF mutations were identified during the hyperselection analysis. While RAS mutations were exclusion criteria, the secondary identification of RAS mutations in both trial cohorts underlines the significance of central and sensitive RAS testing to potentially identify subclonal drivers of early resistance. In addition, patients with BRAF-mutated mCRC are now commonly excluded from anti-EGFR therapy but were included in both trial populations [1, 16, 18]. However, our observations in the left-sided, negative hyperselected subgroup were validated irrespective of BRAF-status. To assess the impact of RAS, RAF and HER2 alterations, a revised hyperselection definition, that included exclusively alterations routinely assessed for anti-EGFR resistance (RAS, BRAF V600E, HER2) was used to re-analyze the impact on treatment outcomes. This restricted analysis yielded prognostic findings consistent with those obtained using the broader gene panel, underscoring the robustness of hyperselection status as a biomarker in induction and maintenance settings and underscoring the impact of broadly assessed alterations in guiding maintenance therapy in this setting.
During maintenance therapy, both anti-EGFR based treatment arms showed significant improvement in PFS compared to 5-FU/LV monotherapy both in the individually left-sided or negative hyperselected subgroups, and in the combination of both subgroups. However, no statistically significant or apparently clinically meaningful PFS benefit for adding 5-FU/LV to anti-EGFR based could be observed in any of these subgroups. In line, previous individual analyses of sidedness and hyperselection status revealed their predictive impact on anti-EGFR based maintenance strategies [7, 9]. In PanaMa, addition of Panitumumab to 5-FU/LV maintenance resulted in significantly prolonged OS in patients with right-sided primary tumors, despite limited numbers in these subgroups [18]. In agreement with our results, a combined analysis of primary tumor sidedness and negative hyperselection from the PARADIGM trial described a numeric OS benefit for the right-sided, negative hyperselected cohort for a Panitumumab vs. Bevacizumab based first-line in mCRC [24]. Additionally, previous studies have demonstrated Amphiregulin expression as a predictive biomarker of anti-EGFR efficacy, also in the right sided colon, as a potential explanation of this observation [25, 26]. In line with the previous individual trial reports, no significant benefit in OS was observed across any of the subgroups, suggesting that while maintenance strategies can delay disease progression, although the existing trials were not powered to detect differences in OS [16, 18].
Our study has several limitations, including the retrospective nature of the IPD pooled analysis and potential heterogeneity between the included trials and the fact that other maintenance studies such as MACRO-2, or COIN-B, or studies with FOLFIRI-based induction such as ERMES and PRODIGE-28 were not included [14, 15, 27, 28]. In addition, the methods and definitions for negative hyperselection were slightly divergent in the PanaMa and Valentino trials, i.e. the use of HER2 in situ hybridization (ISH) was restricted to the Valentino cohort, while in PanaMa only HER2 3+ immunohistochemistry (IHC) and ERBB2 mutations were considered to assess HER2 alterations [7, 9]. Patients who did not have disease progression during induction and reached the maintenance phase may be positively selected, potentially not representing the overall population, particularly respective to RAS/BRAF mutations and right-sided primary tumors, hampering conclusions to be drawn from these subpopulations. Finally, evaluation of combined primary tumor sidedness and hyperselection status on efficacy of maintenance strategies was limited to the left-sided, negative hyperselected population due to limited numbers in the remaining subgroups. The comparator arms from PanaMa and Valentino were analyzed separately, and no formal direct comparison was intended. As such, any contextual interpretation of outcomes across these groups should be made with caution, given the methodological limitations of cross-trial comparisons. However, pooled patient cohorts enhanced statistical power, and while separate subgroup analyses corroborated our findings, the combined analysis provided a more robust assessment of the biomarkers’ predictive value. In routine practice, patients with left-sided tumors that are RAS and BRAF WT, HER2-negative, and microsatellite stable are considered optimal candidates for anti-EGFR based treatment strategies. Although this study additionally explored more extensive molecular hyperselection parameters, the present data do not establish a clear added value for these markers beyond the current standard-of-care. Despite these limitations, our findings provide evidence for novel maintenance treatment stratification approaches in mCRC.
In clinical practice, these results support the stratification of patients based on primary tumor sidedness and hyperselection status when considering maintenance therapy options following oxaliplatin- and anti-EGFR based induction. Stratification of patients with left-sided, negative hyperselected tumors to anti-EGFR based maintenance could optimize treatment choices in this population, potentially sparing patients from additional toxicity, clinic time, and financial burden associated with 5-FU/LV, helping to increase the overall quality of life in this patient population without compromising PFS outcomes. However, the skin toxicity related to anti-EGFR treatment should be considered also in light of the potential use of stop and go strategies, especially in adequately selected patients based on depth of response to therapy, disease burden, extended molecular profile and patients’ preferences in a shared decision making process [29,30,31]. Further investigation into the relative contribution of individual hyperselection parameters in this setting is warranted.
In conclusion, our analysis highlights the significant prognostic value of primary tumor sidedness and hyperselection status in mCRC. Personalized maintenance strategies based on these factors can enhance treatment efficacy and improve patient outcomes.
Methods
Study design and patients
This was a secondary, exploratory analysis of a previously published IPD pooled analysis including the PanaMa and Valentino ranomized phase 2 trials [16, 18, 21]. In the Panama trial (NCT01991873), maintenance therapy involving Panitumumab combined with 5-FU/LV demonstrated significantly superior PFS compared to 5-FU/LV alone, in patients with RAS WT mCRC who achieved at least disease control after six cycles of Panitumumab plus FOLFOX. The Valentino phase II trial (NCT02476045) employed a randomization to a 4-month induction phase with panitumumab plus FOLFOX, followed by maintenance therapy with Panitumumab alone or the same induction treatment followed by maintenance with Panitumumab plus 5-FU/LV, in patients with RAS WT mCRC. The trial aimed at demonstrating non-inferiority of maintenance therapy with single-agent Panitumumab as compared to its combination with 5-FU/LV in terms of 10-month PFS. Non-inferiority was not proved and the results showed that Panitumumab was inferior in terms of PFS compared to panitumumab plus 5-FU/LV, although the combination arm had a slightly increased treatment-related toxicity.
The eligibility criteria, detailed methods of the studies, along with efficacy and safety results, have been reported previously [16, 18]. The present analysis included all patients who received the pre-planned induction therapy for analyses regarding induction therapy and all patients who started the assigned maintenance regimen for analyses regarding maintenance therapy. The study protocols and its amendments were approved by an independent institutional review board or ethics committee at each study site. The study was conducted in compliance with Good Clinical Practice guidelines and the Declaration of Helsinki. All patients provided written, informed consent. This secondary analysis is part of an IPD pooled analysis study and was approved by the ethical committee of Fondazione IRCCS Istituto Nazionale dei Tumori, which assessed consent to and granted authorization for future research use and data sharing (Identifier: INT 99/22) [21].
Data collection
Anonymized data collection included patients’ characteristics, i.e. age, sex, Eastern cooperative oncology group (ECOG) performance status, primary tumor location, hyperselection status (negative hyperselected vs. gene altered), primary tumor resection status, previous adjuvant treatment, number and site of metastases, first-line treatment start and stop dates, number of cycles administered and best response to induction therapy, treatment arm (maintenance with Panitumumab, maintenance with 5-FU/LV monotherapy, maintenance with Panitumumab plus 5-FU/LV) treatment durations, and efficacy outcomes (disease progression and survival), as previously described [21]. A trial database was set up to include the information extrapolated from the two study datasets to ensure the collection of appropriately comparable data and to facilitate the planned IPD pooled analysis. Primary tumor sidedness was assessed as left-sided (splenic flexure to rectum) versus right-sided (caecum to transverse colon) primary tumors.
Molecular analyses for negative hyperselection were previously reported for PanaMa and Valentino, respectively [7, 9]. Briefly, in PanaMa, negative hyperselection was performed using targeted next-generation sequencing (NGS; Illumina Cancer Hotspot Panel v2) to detect mutations in RAS, BRAF (V600E only), PIK3CA, AKT1, ERBB2, PTEN and IHC for HER2 overexpression/amplification [9]. In addition, in Valentino, IHC and dual-color silver ISH for HER2 and MET were performed. Actionable gene fusions were screened using IHC for ALK/ROS1/panTRK/RET; in all samples with evidence of IHC staining of any intensity/extension, whole-transcriptome shotgun sequencing was performed to confirm the presence of specific rearrangements. Oncogenic mutations in RAS, BRAF (V600E only), PIK3CA, AKT1, ERBB2, PTEN were assessed using NGS (Illumina Cancer Hotspot Panel v2) [7]. While presence of RAS mutations precluded inclusion in the original trials, they used assays with a limited RAS mutation panel, subsequent testing with more comprehensive panels identified additional mutations and they were included in this analysis.
For this IPD pooled analysis, selection criteria for both trials were combined to achieve comparable definitions for hyperselection status. Namely, patients were negatively hyperselected by the presence of mutations in RAS, BRAF (V600E only), PIK3CA, AKT1, ERBB2, PTEN or HER2 overexpression detected by IHC and ISH as previously described [7, 9]. Of note, for patients from the PanaMa cohort, no ISH was available, so only patients with a HER2 IHC score 3+ were defined as HER2-positive. Patients presenting with at least one of the aforementioned alterations were grouped in the gene altered cohort. If no alteration was detected, patients were defined as negative hyperselected.
Endpoints and statistical analysis
Patients were grouped and compared based on the specific maintenance treatment received: 5-FU/LV + anti-EGFR, anti-EGFR monotherapy, or 5-FU/LV alone. The primary outcome measures were progression-free survival (PFS) and overall survival (OS) in the overall study population and within key subgroups, including primary tumor sidedness and hyperselection status. PFS was defined as the time from the start of induction (induction PFS) or maintenance (maintenance PFS) treatment to disease progression (PD) according to RECIST 1.1 criteria or death from any cause, while OS was defined as the time from the start of induction (induction OS) or maintenance (maintenance OS) treatment to death from any cause. If patients did not experience progression or death, data were censored at the last date known event-free. Two sets of patients with available information on sidedness and hyperselection status were defined for the prognostic and predictive analyses, respectively. The induction set of patients included all patients who received at least one cycle of first-line induction therapy and was used for the prognostic analyses. The maintenance set of patients included all patients who received at least one cycle of maintenance therapy and was used for the predictive analyses.
Clinical and biological characteristics of patients according to the maintenance treatment arms were summarized using standard descriptive statistics and compared using Pearson’s Chi-squared test. PFS and OS curves were estimated using the Kaplan–Meier method. The impact of different maintenance regimens on the overall study cohort and various subgroups was investigated using Cox proportional hazards regression models.
Exploratory analyses were performed on the main subgroups based on the following baseline characteristics: sex (male vs. female), age (>65 vs. ≤65 years), ECOG PS (0 vs. 1), primary tumor resection (yes vs. no), prior adjuvant therapy (yes vs. no), synchronous vs. metachronous presentation of metastases, number of metastatic sites (1 vs. >1), primary tumor sidedness (left- vs. right-sided), hyperselection status (negative hyperselected vs. gene altered), sites of metastases (liver-limited vs. non-liver-limited), and overall response rate to first-line treatment according to RECIST 1.1 criteria (progressive disease [PD] or stable disease [SD] vs. complete response [CR] or partial response [PR]). Given the similar eligibility criteria, treatment protocols and endpoint definitions in both trials, and supported by prior IPD analyses, the maintenance chemo plus Panitumumab arms were pooled to increase statistical power and precision in evaluating this ESMO-recommended treatment strategy. As the comparator arms (chemo alone from PanaMa and panitumumab alone from Valentino) were not pooled, direct comparisons between these groups should be interpreted with caution due to the limitations of cross-trial analyses.
Results from the models were summarized using hazard ratios (HR) with corresponding 95% confidence intervals (CI) and likelihood ratio test P values. P values < 0.05 (two-sided) were considered statistically significant. SPSS PASW 29.0 (SPSS, Chicago, IL) and R v4.3.2 (The R Foundation for Statistical Computing, Vienna, Austria) software were used for statistical analyses.
Data availability
Data will be made available upon reasonable request to the corresponding authors.
References
Cervantes A, Adam R, Rosello S, Arnold D, Normanno N, Taieb J, et al. Metastatic colorectal cancer: ESMO Clinical Practice Guideline for diagnosis, treatment and follow-up. Ann Oncol. 2023;34:10–32.
Arnold D, Lueza B, Douillard JY, Peeters M, Lenz HJ, Venook A, et al. Prognostic and predictive value of primary tumour side in patients with RAS wild-type metastatic colorectal cancer treated with chemotherapy and EGFR directed antibodies in six randomized trials. Ann Oncol. 2017;28:1713–29.
Alig AHS, Modest DP, Stintzing S, Heinrich K, Geissler M, Fischer von Weikersthal L, et al. Impact of primary tumor sidedness and sex on prognosis and anti-epidermal growth factor receptor antibody efficacy in BRAF-mutant metastatic colorectal cancer: a pooled analysis of AIO studies FIRE-1, CIOX, FIRE-3, XELAVIRI, and VOLFI. ESMO Open. 2024;9:103677.
Rossini D, Boccaccino A, Carullo M, Antoniotti C, Dima G, Ciraci P, et al. Primary tumour side as a driver for treatment choice in RAS wild-type metastatic colorectal cancer patients: a systematic review and pooled analysis of randomised trials. Eur J Cancer. 2023;184:106–16.
Van Cutsem E, Lenz HJ, Kohne CH, Heinemann V, Tejpar S, Melezinek I, et al. Fluorouracil, leucovorin, and irinotecan plus cetuximab treatment and RAS mutations in colorectal cancer. J Clin Oncol. 2015;33:692–700.
Cremolini C, Morano F, Moretto R, Berenato R, Tamborini E, Perrone F, et al. Negative hyper-selection of metastatic colorectal cancer patients for anti-EGFR monoclonal antibodies: the PRESSING case-control study. Ann Oncol. 2017;28:3009–14.
Morano F, Corallo S, Lonardi S, Raimondi A, Cremolini C, Rimassa L, et al. Negative hyperselection of patients with RAS and BRAF wild-type metastatic colorectal cancer who received panitumumab-based maintenance therapy. J Clin Oncol. 2019;37:3099–110.
Randon G, Maddalena G, Germani MM, Pircher CC, Manca P, Bergamo F, et al. Negative ultraselection of patients with RAS/BRAF wild-type, microsatellite-stable metastatic colorectal cancer receiving anti-EGFR-based therapy. JCO Precis Oncol. 2022;6:e2200037.
Stahler A, Kind AJ, Sers C, Mamlouk S, Muller L, Karthaus M, et al. Negative hyperselection of resistance mutations for panitumumab maintenance in RAS wild-type metastatic colorectal cancer (PanaMa Phase II Trial, AIO KRK 0212). Clin Cancer Res. 2024;30:1256–63.
Tournigand C, Cervantes A, Figer A, Lledo G, Flesch M, Buyse M, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer-a GERCOR study. J Clin Oncol. 2006;24:394–400.
Diaz-Rubio E, Gomez-Espana A, Massuti B, Sastre J, Abad A, Valladares M, et al. First-line XELOX plus bevacizumab followed by XELOX plus bevacizumab or single-agent bevacizumab as maintenance therapy in patients with metastatic colorectal cancer: the phase III MACRO TTD study. Oncologist. 2012;17:15–25.
Chibaudel B, Maindrault-Goebel F, Lledo G, Mineur L, Andre T, Bennamoun M, et al. Can chemotherapy be discontinued in unresectable metastatic colorectal cancer? The GERCOR OPTIMOX2 Study. J Clin Oncol. 2009;27:5727–33.
Adams RA, Meade AM, Seymour MT, Wilson RH, Madi A, Fisher D, et al. Intermittent versus continuous oxaliplatin and fluoropyrimidine combination chemotherapy for first-line treatment of advanced colorectal cancer: results of the randomised phase 3 MRC COIN trial. Lancet Oncol. 2011;12:642–53.
Wasan H, Meade AM, Adams R, Wilson R, Pugh C, Fisher D, et al. Intermittent chemotherapy plus either intermittent or continuous cetuximab for first-line treatment of patients with KRAS wild-type advanced colorectal cancer (COIN-B): a randomised phase 2 trial. Lancet Oncol. 2014;15:631–9.
Boige V, Blons H, Francois E, Ben Abdelghani M, Phelip JM, Le Brun-Ly V, et al. Maintenance therapy with cetuximab after FOLFIRI plus cetuximab for RAS wild-type metastatic colorectal cancer: a phase 2 randomized clinical trial. JAMA Netw Open. 2023;6:e2333533.
Pietrantonio F, Morano F, Corallo S, Miceli R, Lonardi S, Raimondi A, et al. Maintenance therapy with panitumumab alone vs panitumumab plus fluorouracil-leucovorin in patients with RAS wild-type metastatic colorectal cancer: a phase 2 randomized clinical trial. JAMA Oncol. 2019;5:1268–75.
Munemoto Y, Nakamura M, Takahashi M, Kotaka M, Kuroda H, Kato T, et al. SAPPHIRE: a randomised phase II study of planned discontinuation or continuous treatment of oxaliplatin after six cycles of modified FOLFOX6 plus panitumumab in patients with colorectal cancer. Eur J Cancer. 2019;119:158–67.
Modest DP, Karthaus M, Fruehauf S, Graeven U, Muller L, Konig AO, et al. Panitumumab plus fluorouracil and folinic acid versus fluorouracil and folinic acid alone as maintenance therapy in RAS wild-type metastatic colorectal cancer: the randomized PANAMA trial (AIO KRK 0212). J Clin Oncol. 2022;40:72–82.
Pinto C, Normanno N, Orlandi A, Fenizia F, Damato A, Maiello E, et al. Phase III study with FOLFIRI + cetuximab versus FOLFIRI + cetuximab followed by cetuximab alone in RAS and BRAF WT mCRC. Future Oncol. 2018;14:1339–46.
Avallone A, Giuliani F, De Stefano A, Santabarbara G, Nasti G, Montesarchio V, et al. Intermittent or Continuous Panitumumab Plus Fluorouracil, Leucovorin, and Irinotecan for First-Line Treatment of RAS and BRAF Wild-Type Metastatic Colorectal Cancer: The IMPROVE Trial. J Clin Oncol. 2025;43:829–39.
Raimondi A, Nichetti F, Stahler A, Wasan HS, Aranda E, Randon G, et al. Optimal maintenance strategy following FOLFOX plus anti-EGFR induction therapy in patients with RAS wild type metastatic colorectal cancer: An individual patient data pooled analysis of randomised clinical trials. Eur J Cancer. 2023;190:112945.
Yoshino T, Hooda N, Younan D, Muro K, Shitara K, Heinemann V, et al. A meta-analysis of efficacy and safety data from head-to-head first-line trials of epidermal growth factor receptor inhibitors versus bevacizumab in adult patients with RAS wild-type metastatic colorectal cancer by sidedness. Eur J Cancer. 2024;202:113975.
Watanabe J, Muro K, Shitara K, Yamazaki K, Shiozawa M, Ohori H, et al. Panitumumab vs Bevacizumab Added to Standard First-line Chemotherapy and Overall Survival Among Patients With RAS Wild-type, Left-Sided Metastatic Colorectal Cancer: A Randomized Clinical Trial. JAMA. 2023;329:1271–82.
Shitara K, Muro K, Watanabe J, Yamazaki K, Ohori H, Shiozawa M, et al. Baseline ctDNA gene alterations as a biomarker of survival after panitumumab and chemotherapy in metastatic colorectal cancer. Nat Med. 2024;30:730–9.
Stahler A, Stintzing S, Modest DP, Ricard I, Giessen-Jung C, Kapaun C, et al. Amphiregulin expression is a predictive biomarker for EGFR inhibition in metastatic colorectal cancer: combined analysis of three randomized trials. Clin Cancer Res. 2020;26:6559–67.
Williams CJM, Elliott F, Sapanara N, Aghaei F, Zhang L, Muranyi A, et al. Associations between AI-assisted tumor amphiregulin and epiregulin IHC and outcomes from anti-EGFR therapy in the routine management of metastatic colorectal cancer. Clin Cancer Res. 2023;29:4153–65.
Aranda E, Garcia-Alfonso P, Benavides M, Sanchez Ruiz A, Guillen-Ponce C, Safont MJ, et al. First-line mFOLFOX plus cetuximab followed by mFOLFOX plus cetuximab or single-agent cetuximab as maintenance therapy in patients with metastatic colorectal cancer: Phase II randomised MACRO2 TTD study. Eur J Cancer. 2018;101:263–72.
Pinto C, Orlandi A, Normanno N, Maiello E, Calegari MA, Antonuzzo L, et al. Fluorouracil, leucovorin, and irinotecan plus cetuximab versus cetuximab as maintenance therapy in first-line therapy for RAS and BRAF wild-type metastatic colorectal cancer: phase III ERMES study. J Clin Oncol. 2024;42:1278–87.
Ballhausen A, Karthaus M, Fruehauf S, Graeven U, Muller L, Konig AO, et al. Dermatology-related quality-of-life outcomes in patients with RAS wild-type metastatic colorectal cancer treated with fluorouracil and folinic acid with or without panitumumab (Pmab) maintenance after FOLFOX + Pmab induction: a prespecified secondary analysis of the phase II randomized PanaMa (AIO KRK 0212) trial. ESMO Open. 2024;9:103628.
Ballhausen A, Karthaus M, Fruehauf S, Graeven U, Muller L, Konig AO, et al. Health-related quality of life in patients with RAS wild-type metastatic colorectal cancer treated with fluorouracil and folinic acid with or without panitumumab as maintenance therapy: a prespecified secondary analysis of the PanaMa (AIO KRK 0212) trial. Eur J Cancer. 2023;190:112955.
Raimondi A, Di Maio M, Morano F, Corallo S, Lonardi S, Antoniotti C, et al. Health-related quality of life in patients with RAS wild-type metastatic colorectal cancer treated with panitumumab-based first-line treatment strategy: a pre-specified secondary analysis of the Valentino study. Eur J Cancer. 2020;135:230–9.
Acknowledgements
We thank all patients and their families who agreed to take part in the trial, as well as the investigators and the study teams who participated in the PanaMa and Valentino trials.
Funding
This Research Project was supported by the International Cancer Foundation. Any views, opinions, findings, conclusions, or recommendations expressed in this material are those solely of the author(s) and do not necessarily reflect those of the International Cancer Foundation. No additional fundings were received for this individual patient data meta-analysis of previously reported randomized clinical trials. Fundings received by each trial were reported in the respective trial publications.
Author information
Authors and Affiliations
Contributions
Alexej Ballhausen: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Software; Validation; Visualization; Writing – original draft; Writing – review and editing. Federica Morano: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Software; Validation; Writing – review and editing. Arndt Stahler: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Software; Validation; Writing – review and editing. Sara Lonardi: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – review and editing. Andreas Jay Kind: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Software; Validation; Writing – review and editing. Chiara Cremolini: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – review and editing. Susanna Swoboda: Formal analysis; Investigation; Writing – review and editing. Giovanni Randon: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. David Horst: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. Michele Prisciandaro: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. Annabel Helga Sophie Alig: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. Chiara Carlotta Pircher: Writing – review and editing. Armin Jarosch: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. Paola Andena: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. Annika Kurreck: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. Anna Alessandra Chiaramonte: Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Writing – review and editing. Sebastian Stintzing: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – review and editing. Filippo Pietrantonio: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review and editing. Dominik Paul Modest: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Project administration; Resources; Software; Supervision; Validation; Visualization; Writing – original draft; Writing – review and editing. Alessandra Raimondi: Conceptualization; Formal analysis; Investigation; Methodology; Project administration; Software; Validation; Visualization; Writing – original draft; Writing – review and editing.
Corresponding authors
Ethics declarations
Competing interests
AB: Stock and other ownership interests: BioNTech SE. Honoraria: Amgen. Research funding: Amgen (Inst). Travel, Accommodations, Expenses: Amgen. FM: Honoraria from Pierre Fabre and Servier; research grants from Incyte (to their institution); travel grants from Amgen and Pierre Fabre. AS: Honoraria: Roche, Servier, Taiho Pharmaceutical. Consulting or advisory role: Bristol Myers Squibb/Pfizer, Novocure. Travel, Accommodations, Expenses: Amgen, Roche, Lilly, Pfizer. SL: Participation in advisory boards for Amgen, Astellas, AstraZeneca, Bayer, Bristol-Myers Squibb, Daiichi Sankyo, GSK, Incyte, Lilly, Merck Serono, MSD, Servier, Takeda, Rottapharm, and Beigene; personal honoraria as invited speaker from Amgen, AstraZeneca, Bristol-Myers Squibb, Incyte, GSK, Lilly, Merck Serono, MSD, Pierre Fabre, Roche, and Servier; research funding (to their institution) from Amgen, Astellas, AstraZeneca, Bayer, Bristol-Myers Squibb, Daiichi Sankyo, Hutchinson, Incyte, Merck Serono, Mirati, MSD, Pfizer, Roche, and Servier. AJK: No competing interests declared. CC: Advisory board or consultant role with Astra Zeneca, Bicara Therapeutics, BMS, GSK, Lilly, Merck, Mirati, MSD, Nordic Pharma, Roche, Pfizer, Pierre Fabre, Revolution Medicine, Rottapharm, Takeda, Tempus; Invited speaker with compensation for Amgen, Bayer, Merck Serono, MSD, Pierre Fabre Servier, Takeda; Research grants by Amgen, Merck, Pierre Fabre, Roche, Seagen (Pfizer), Servier, Tempus. SS: No competing interests declared. GR: No competing interests declared. DH: No competing interests declared. MP: No competing interests declared. AHSA: Honoraria: MSD. Travel, Accommodations, Expenses: Merck, BMS GmbH and Co. KG. CCP: No competing interests declared. AJ: No competing interests declared. PA: No competing interests declared. Annika Kurreck: Honoraria: Taiho Pharmaceutical, Amgen, Servier. Travel, Accommodations, Expenses: medac, Amgen, Servier. AAC: No competing interests declared. SS: Honoraria: Merck KGaA, Roche, Amgen, Servier, MSD, Pfizer, Pierre Fabre, Bristol Myers Squibb GmbH, Nordic Bioscience, AstraZeneca. Consulting or advisory role: Merck Kgaa, Roche, Amgen, Pierre Fabre, MSD, AstraZeneca, Servier, GlaxoSmithKline, Terumo, Nordic Bioscience, Seagen. Research Funding: Pierre Fabre (Inst), Roche Molecular Diagnostics (Inst), Merck Serono (Inst), Amgen (Inst). Travel, Accommodations, Expenses: Merck KGaA, Roche, Sanofi, Bayer, Sirtex Medical, Amgen, Lilly, Takeda, Pierre Fabre, AstraZeneca. FP: Research funding (to their institution) from Lilly, Bristol-Myers Squibb, Incyte, AstraZeneca, Amgen, and Agenus; personal honoraria as an invited speaker from BeiGene, Daiichi Sankyo, Seagen, Astellas, Ipsen, AstraZeneca, Servier, Bayer, Takeda, Johnson & Johnson, Bristol-Myers Squibb, MSD, Amgen, Merck Serono, Pierre Fabre; and advisory or consultancy fees from Bristol-Myers Squibb, MSD, Amgen, Pierre Fabre, Johnson & Johnson, Servier, Bayer, Takeda, Astellas, GSK, Daiichi Sankyo, Pfizer, BeiGene, Jazz Pharmaceuticals, Incyte, Rottapharm, and Merck Serono. DPM: Honoraria: Merck Serono, Amgen, Servier, Bristol Myers Squibb, Taiho Pharmaceutical, Merck Sharp and Dohme, Pierre Fabre, Onkowissen, Sanofi, Lilly, AstraZeneca/MedImmune, Incyte, Takeda. Consulting or advisory role: Merck Serono, Amgen, Merck Sharp and Dohme, Roche, Servier, Incyte, Bristol Myers Squibb, Pierre Fabre, Lilly, Cor2Ed, IQVIA, Onkowissen. Research funding: Amgen (Inst), Servier (Inst). Travel, Accommodations, Expenses: Amgen, Merck Serono, Servier. AR: Honoraria for speaker bureau or advisory board participation from Servier and MSD.
Ethics approval and consent to participate
The study protocols and its amendments were approved by an independent institutional review board or ethics committee at each study site. The study was conducted in compliance with Good Clinical Practice guidelines and the Declaration of Helsinki. All patients provided written, informed consent. This secondary analysis is part of an IPD pooled analysis study and was approved by the ethical committee of Fondazione IRCCS Istituto Nazionale dei Tumori (Identifier: INT 99/22).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ballhausen, A., Morano, F., Stahler, A. et al. Primary tumor sidedness and negative hyperselection to modulate anti-EGFR-based maintenance strategies in patients with RAS wild-type metastatic colorectal cancer: individual patient data pooled analysis of two randomized clinical trials. Br J Cancer 133, 1297–1306 (2025). https://doi.org/10.1038/s41416-025-03164-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41416-025-03164-5