Abstract
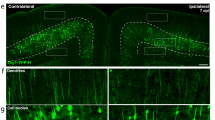
Lactates accumulation following traumatic brain injury (TBI) is detrimental. However, whether lactylation is triggered and involved in the deterioration of TBI remains unknown. Here, we first report that Tufm lactylation pathway induces neuronal apoptosis in TBI. Lactylation is found significantly increased in brain tissues from patients with TBI and mice with controlled cortical impact (CCI), and in neuronal injury cell models. Tufm, a key factor in mitophagy, is screened and identified to be mostly lactylated. Tufm is detected to be lactylated at K286 and the lactylation inhibits the interaction of Tufm and Tomm40 on mitochondria. The mitochondrial distribution of Tufm is then inhibited. Consequently, Tufm-mediated mitophagy is suppressed while mitochondria-induced neuronal apoptosis is increased. In contrast, the knockin of a lactylation-deficient TufmK286R mutant in mice rescues the mitochondrial distribution of Tufm and Tufm-mediated mitophagy, and improves functional outcome after CCI. Likewise, mild hypothermia, as a critical therapeutic method in neuroprotection, helps in downregulating Tufm lactylation, increasing Tufm-mediated mitophagy, mitigating neuronal apoptosis, and eventually ameliorating the outcome of TBI. A novel molecular mechanism in neuronal apoptosis, TBI-initiated Tufm lactylation suppressing mitophagy, is thus revealed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Maas AIR, Menon DK, Adelson PD, Andelic N, Bell MJ, Belli A, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16:987–1048.
Maas AIR, Menon DK, Manley GT, Abrams M, Åkerlund C, Andelic N, et al. Traumatic brain injury: progress and challenges in prevention, clinical care, and research. Lancet Neurol. 2022;21:1004–60.
Jiang J-Y, Gao G-Y, Feng J-F, Mao Q, Chen L-G, Yang X-F, et al. Traumatic brain injury in China. Lancet Neurol. 2019;18:286–95.
World Health Organization. Neurological disorders: public health challenges. 2006. https://www.who.int/publications/i/item/9789241563369/.
Majdan M, Plancikova D, Brazinova A, Rusnak M, Nieboer D, Feigin V, et al. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health. 2016;1:e76–e83.
Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017;66:1–16.
Feigin VL, Theadom A, Barker-Collo S, Starkey NJ, McPherson K, Kahan M, et al. Incidence of traumatic brain injury in New Zealand: a population-based study. Lancet Neurol. 2013;12:53–64.
Corrigan F, Mander KA, Leonard AV, Vink R. Neurogenic inflammation after traumatic brain injury and its potentiation of classical inflammation. J Neuroinflammation. 2016;13:264.
Fesharaki-Zadeh A. Oxidative stress in traumatic brain injury. Int J Mol Sci. 2022;23:13000.
Jamjoom AAB, Rhodes J, Andrews PJD, Grant SGN. The synapse in traumatic brain injury. Brain. 2021;144:18–31.
Hiebert JB, Shen Q, Thimmesch AR, Pierce JD. Traumatic brain injury and mitochondrial dysfunction. Am J Med Sci. 2015;350:132–8.
Nie Z, Tan L, Niu J, Wang B. The role of regulatory necrosis in traumatic brain injury. Front Mol Neurosci. 2022;15:1005422.
Akamatsu Y, Hanafy KA. Cell death and recovery in traumatic brain injury. Neurotherapeutics. 2020;17:446–56.
Cash A, Theus MH. Mechanisms of blood-brain barrier dysfunction in traumatic brain injury. Int J Mol Sci. 2020;21:3344.
Carpenter KLH, Jalloh I, Gallagher CN, Grice P, Howe DJ, Mason A, et al. 13C-labelled microdialysis studies of cerebral metabolism in TBI patients. Eur J Pharm Sci. 2014;57:87–97.
Timofeev I, Carpenter KLH, Nortje J, Al-Rawi PG, O’Connell MT, Czosnyka M, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a microdialysis study of 223 patients. Brain. 2011;134:484–94.
Lozano A, Franchi F, Seastres RJ, Oddo M, Lheureux O, Badenes R, et al. Glucose and lactate concentrations in cerebrospinal fluid after traumatic brain injury. J Neurosurg Anesthesiol. 2020;32:162–9.
Thomas I, Dickens AM, Posti JP, Czeiter E, Duberg D, Sinioja T, et al. Serum metabolome associated with severity of acute traumatic brain injury. Nat Commun. 2022;13:2545.
Lai J-Q, Shi Y-C, Lin S, Chen X-R. Metabolic disorders on cognitive dysfunction after traumatic brain injury. Trends Endocrinol Metab. 2022;33:451–62.
Jiang J-Y, Xu W, Li W-P, Gao G-Y, Bao Y-H, Liang Y-M, et al. Effect of long-term mild hypothermia or short-term mild hypothermia on outcome of patients with severe traumatic brain injury. J Cereb Blood Flow Metab. 2006;26:771–6.
Hui J, Feng J, Tu Y, Zhang W, Zhong C, Liu M, et al. Safety and efficacy of long-term mild hypothermia for severe traumatic brain injury with refractory intracranial hypertension (LTH-1): a multicenter randomized controlled trial. EClinicalMedicine. 2021;32:100732.
Maxwell WL, Donnelly S, Sun X, Fenton T, Puri N, Graham DI. Axonal cytoskeletal responses to nondisruptive axonal injury and the short-term effects of posttraumatic hypothermia. J Neurotrauma. 1999;16:1225–34.
Koizumi H, Povlishock JT. Posttraumatic hypothermia in the treatment of axonal damage in an animal model of traumatic axonal injury. J Neurosurg. 1998;89:303–9.
Marion DW, White MJ. Treatment of experimental brain injury with moderate hypothermia and 21-aminosteroids. J Neurotrauma. 1996;13:139–47.
Yang K, Fan M, Wang X, Xu J, Wang Y, Tu F, et al. Lactate promotes macrophage HMGB1 lactylation, acetylation, and exosomal release in polymicrobial sepsis. Cell Death Differ. 2022;29:133–46.
Pucino V, Cucchi D, Mauro C. Lactate transporters as therapeutic targets in cancer and inflammatory diseases. Expert Opin Ther Targets. 2018;22:735–43.
Zhang D, Tang Z, Huang H, Zhou G, Cui C, Weng Y, et al. Metabolic regulation of gene expression by histone lactylation. Nature. 2019;574:575–80.
Liu X, Zhang Y, Li W, Zhou X. Lactylation, an emerging hallmark of metabolic reprogramming: current progress and open challenges. Front Cell Dev Biol. 2022;10:972020.
Raghupathi R, Graham DI, McIntosh TK. Apoptosis after traumatic brain injury. J Neurotrauma. 2000;17:927–38.
Zhang X, Chen Y, Jenkins LW, Kochanek PM, Clark RSB. Bench-to-bedside review: apoptosis/programmed cell death triggered by traumatic brain injury. Crit Care. 2005;9:66–75.
Raghupathi R. Cell death mechanisms following traumatic brain injury. Brain Pathol. 2004;14:215–22.
He Z, Lang L, Hui J, Ma Y, Yang C, Weng W, et al. Brain extract of subacute traumatic brain injury promotes the neuronal differentiation of human neural stem cells via autophagy. J Clin Med. 2022;11:2709.
Sarkar C, Zhao Z, Aungst S, Sabirzhanov B, Faden AI, Lipinski MM. Impaired autophagy flux is associated with neuronal cell death after traumatic brain injury. Autophagy. 2014;10:2208–22.
Lin C, Chao H, Li Z, Xu X, Liu Y, Hou L, et al. Melatonin attenuates traumatic brain injury-induced inflammation: a possible role for mitophagy. J Pineal Res. 2016;61:177–86.
Scrivo A, Bourdenx M, Pampliega O, Cuervo AM. Selective autophagy as a potential therapeutic target for neurodegenerative disorders. Lancet Neurol. 2018;17:802–15.
Ashrafi G, Schwarz TL. The pathways of mitophagy for quality control and clearance of mitochondria. Cell Death Differ. 2013;20:31–42.
Wu Q, Gao C, Wang H, Zhang X, Li Q, Gu Z, et al. Mdivi-1 alleviates blood-brain barrier disruption and cell death in experimental traumatic brain injury by mitigating autophagy dysfunction and mitophagy activation. Int J Biochem Cell Biol. 2018;94:44–55.
Ren Y-Z, Zhang B-Z, Zhao X-J, Zhang Z-Y. Resolvin D1 ameliorates cognitive impairment following traumatic brain injury via protecting astrocytic mitochondria. J Neurochem. 2020;154:530–46.
Lin C, Li N, Chang H, Shen Y, Li Z, Wei W, et al. Dual effects of thyroid hormone on neurons and neurogenesis in traumatic brain injury. Cell Death Dis. 2020;11:671.
Ma J, Ni H, Rui Q, Liu H, Jiang F, Gao R, et al. Potential roles of NIX/BNIP3L pathway in rat traumatic brain injury. Cell Transplant. 2019;28:585–95.
Chao H, Lin C, Zuo Q, Liu Y, Xiao M, Xu X, et al. Cardiolipin-dependent mitophagy guides outcome after traumatic brain injury. J Neurosci. 2019;39:1930–43.
Wang R, Zhu Y, Ren C, Yang S, Tian S, Chen H, et al. Influenza A virus protein PB1-F2 impairs innate immunity by inducing mitophagy. Autophagy. 2021;17:496–511.
Wang K, Ma H, Liu H, Ye W, Li Z, Cheng L, et al. The glycoprotein and nucleocapsid protein of hantaviruses manipulate autophagy flux to restrain host innate immune responses. Cell Rep. 2019;27:2075–91.e5.
Ding B, Zhang L, Li Z, Zhong Y, Tang Q, Qin Y, et al. The matrix protein of human parainfluenza virus type 3 induces mitophagy that suppresses interferon responses. Cell Host Microbe. 2017;21:538–47.e4.
Choi C-Y, Vo MT, Nicholas J, Choi YB. Autophagy-competent mitochondrial translation elongation factor TUFM inhibits caspase-8-mediated apoptosis. Cell Death Differ. 2022;29:451–64.
Lai F-L, Gao F. Auto-Kla: a novel web server to discriminate lysine lactylation sites using automated machine learning. Brief Bioinform. 2023;24:bbad070.
Araiso Y, Tsutsumi A, Qiu J, Imai K, Shiota T, Song J, et al. Structure of the mitochondrial import gate reveals distinct preprotein paths. Nature. 2019;575:395–401.
Araiso Y, Imai K, Endo T. Role of the TOM complex in protein import into mitochondria: structural views. Annu Rev Biochem. 2022;91:679–703.
Gabriel K, Egan B, Lithgow T. Tom40, the import channel of the mitochondrial outer membrane, plays an active role in sorting imported proteins. EMBO J. 2003;22:2380–6.
Hagihara H, Shoji H, Otabi H, Toyoda A, Katoh K, Namihira M, et al. Protein lactylation induced by neural excitation. Cell Rep. 2021;37:109820.
Dai S-K, Liu P-P, Li X, Jiao L-F, Teng Z-Q, Liu C-M. Dynamic profiling and functional interpretation of histone lysine crotonylation and lactylation during neural development. Development. 2022;149:dev200049.
Pan R-Y, He L, Zhang J, Liu X, Liao Y, Gao J, et al. Positive feedback regulation of microglial glucose metabolism by histone H4 lysine 12 lactylation in Alzheimer’s disease. Cell Metab. 2022;34:634–48.e6.
Yao Y, Bade R, Li G, Zhang A, Zhao H, Fan L, et al. Global-scale profiling of differential expressed lysine-lactylated proteins in the cerebral endothelium of cerebral ischemia-reperfusion injury rats. Cell Mol Neurobiol. 2022;43:1989–2004.
Carpenter KLH, Jalloh I, Hutchinson PJ. Glycolysis and the significance of lactate in traumatic brain injury. Front Neurosci. 2015;9:112.
McGinn MJ, Povlishock JT. Pathophysiology of traumatic brain injury. Neurosurg Clin N Am. 2016;27:397–407.
Pellerin L, Magistretti PJ. Glutamate uptake into astrocytes stimulates aerobic glycolysis: a mechanism coupling neuronal activity to glucose utilization. Proc Natl Acad Sci USA. 1994;91:10625–29.
Glenn TC, Martin NA, Horning MA, McArthur DL, Hovda DA, Vespa P, et al. Lactate: brain fuel in human traumatic brain injury: a comparison with normal healthy control subjects. J Neurotrauma. 2015;32:820–32.
Patel AB, Lai JCK, Chowdhury GMI, Hyder F, Rothman DL, Shulman RG, et al. Direct evidence for activity-dependent glucose phosphorylation in neurons with implications for the astrocyte-to-neuron lactate shuttle. Proc Natl Acad Sci USA. 2014;111:5385–90.
Glenn TC, Kelly DF, Boscardin WJ, McArthur DL, Vespa P, Oertel M, et al. Energy dysfunction as a predictor of outcome after moderate or severe head injury: indices of oxygen, glucose, and lactate metabolism. J Cereb Blood Flow Metab. 2003;23:1239–50.
Dienel GA. The metabolic trinity, glucose-glycogen-lactate, links astrocytes and neurons in brain energetics, signaling, memory, and gene expression. Neurosci Lett. 2017;637:18–25.
Jiang J-Y, Liang Y-M, Luo Q-Z, Zhu C. Effect of mild hypothermia on brain dialysate lactate after fluid percussion brain injury in rodents. Neurosurgery. 2004;54:713–7.
Zhao Q-J, Zhang X-G, Wang L-X. Mild hypothermia therapy reduces blood glucose and lactate and improves neurologic outcomes in patients with severe traumatic brain injury. J Crit Care. 2011;26:311–5.
Sharma NK, Pal JK. Metabolic ink lactate modulates epigenomic landscape: a concerted role of pro-tumor microenvironment and macroenvironment during carcinogenesis. Curr Mol Med. 2021;21:177–81.
Kalgudi S, Ho KM. Incidence of antithrombin deficiency and anti-cardiolipin antibodies after severe traumatic brain injury: a prospective cohort study. Neurocrit Care. 2021;34:227–35.
Saw MM, Chamberlain J, Barr M, Morgan MPG, Burnett JR, Ho KM. Differential disruption of blood-brain barrier in severe traumatic brain injury. Neurocrit Care. 2014;20:209–16.
Chu CT, Ji J, Dagda RK, Jiang JF, Tyurina YY, Kapralov AA, et al. Cardiolipin externalization to the outer mitochondrial membrane acts as an elimination signal for mitophagy in neuronal cells. Nat Cell Biol. 2013;15:1197–205.
Tian C, Min X, Zhao Y, Wang Y, Wu X, Liu S, et al. MRG15 aggravates non-alcoholic steatohepatitis progression by regulating the mitochondrial proteolytic degradation of TUFM. J Hepatol. 2022;77:1491–503.
Xu X, Huang A, Cui X, Han K, Hou X, Wang Q, et al. Ubiquitin specific peptidase 5 regulates colorectal cancer cell growth by stabilizing Tu translation elongation factor. Theranostics. 2019;9:4208–20.
Wei R, Lv X, Fang C, Liu C, Ma Z, Liu K. Silencing TUFM inhibits development of monocrotaline-induced pulmonary hypertension by regulating mitochondrial autophagy via AMPK/mTOR signal pathway. Oxid Med Cell Longev. 2022;2022:4931611.
Wu X, Xu M, Geng M, Chen S, Little PJ, Xu S, et al. Targeting protein modifications in metabolic diseases: molecular mechanisms and targeted therapies. Signal Transduct Target Ther. 2023;8:220.
Lin J, Chen K, Chen W, Yao Y, Ni S, Ye M, et al. Paradoxical mitophagy regulation by PINK1 and TUFm. Mol Cell. 2020;80:607–20.e12.
Park J, Chen Y, Tishkoff DX, Peng C, Tan M, Dai L, et al. SIRT5-mediated lysine desuccinylation impacts diverse metabolic pathways. Mol Cell. 2013;50:919–30.
Ma X, Aravind A, Pfister BJ, Chandra N, Haorah J. Animal models of traumatic brain injury and assessment of injury severity. Mol Neurobiol. 2019;56:5332–45.
Siebold L, Obenaus A, Goyal R. Criteria to define mild, moderate, and severe traumatic brain injury in the mouse controlled cortical impact model. Exp Neurol. 2018;310:48–57.
Flierl MA, Stahel PF, Beauchamp KM, Morgan SJ, Smith WR, Shohami E. Mouse closed head injury model induced by a weight-drop device. Nat Protoc. 2009;4:1328–37.
Shan H-M, Maurer MA, Schwab ME. Four-parameter analysis in modified rotarod test for detecting minor motor deficits in mice. BMC Biol. 2023;21:177.
Gong W, Das S, Sierra-Pagan JE, Skie E, Dsouza N, Larson TA, et al. ETV2 functions as a pioneer factor to regulate and reprogram the endothelial lineage. Nat Cell Biol. 2022;24:672–84.
Sciarretta C, Minichiello L. The preparation of primary cortical neuron cultures and a practical application using immunofluorescent cytochemistry. Methods Mol Biol. 2010;633:221–31.
Ji J, Kline AE, Amoscato A, Samhan-Arias AK, Sparvero LJ, Tyurin VA, et al. Lipidomics identifies cardiolipin oxidation as a mitochondrial target for redox therapy of brain injury. Nat Neurosci. 2012;15:1407–13.
Weng W, Gu X, Yang Y, Zhang Q, Deng Q, Zhou J, et al. N-terminal α-amino SUMOylation of cofilin-1 is critical for its regulation of actin depolymerization. Nat Commun. 2023;14:5688.
Liu H, Weng W, Guo R, Zhou J, Xue J, Zhong S, et al. Olig2 SUMOylation protects against genotoxic damage response by antagonizing p53 gene targeting. Cell Death Differ. 2020;27:3146–61.
Ma R, Ma L, Weng W, Wang Y, Liu H, Guo R, et al. DUSP6 SUMOylation protects cells from oxidative damage via direct regulation of Drp1 dephosphorylation. Sci Adv. 2020;6:eaaz0361.
Acknowledgements
The authors acknowledge the use of Biorender.com which is used to create the schematic model in Supplementary Information, Fig. S7.
Funding
This study was supported by grants from the National Natural Science Foundation of China (82071358 and 82371379 to JF, 82372501 to JJ, 82401610 to W Weng), the Program of Shanghai Academic Research Leader (21XD1422400 to JF), Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Support (02.101005.001.30.30A to JF), and the Project of Shanghai Medical And Health Development Foundation (20224Z0012 to JF).
Author information
Authors and Affiliations
Contributions
JF and W Weng conceived the study and designed the experiments. W Weng, ZH, ZM, JH and YH carried out the experiments. QF and WQ assisted with data analysis and analyzed the results. YP, JW, JG, W Wang, YL, JJ, GJ, W Weng and JF discussed the results. W Weng, ZH and JF wrote the manuscript. W Weng, JH, JJ and JF reviewed/edited the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
All methods were performed in accordance with the relevant guidelines and regulations. All animal experiments were conducted in agreement with the Guide for the Care and Use of Laboratory Animals and approved by the Institutional Animal Care and Use Committee of Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine (Reference No. 2023-106). This study related to patients has been approved by the Ethics Committee of Ren Ji Hospital, Shanghai Jiao Tong University School of Medicine (Reference No. LY2023-017-B). The informed consent was obtained from all participants.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Weng, W., He, Z., Ma, Z. et al. Tufm lactylation regulates neuronal apoptosis by modulating mitophagy in traumatic brain injury. Cell Death Differ 32, 530–545 (2025). https://doi.org/10.1038/s41418-024-01408-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41418-024-01408-0
This article is cited by
-
Intranasal delivery of hypoxia-preconditioned extracellular vesicles derived from BMSCs alleviates neuroinflammation and brain dysfunction in TBI
Stem Cell Research & Therapy (2025)
-
Histone and non-histone lactylation: molecular mechanisms, biological functions, diseases, and therapeutic targets
Molecular Biomedicine (2025)
-
FGF21 maintains redox homeostasis and promotes neuronal survival after traumatic brain injury by targeting SLC25A39-mediated mitochondrial GSH transport
Journal of Translational Medicine (2025)
-
Lactylation associated biomarkers and immune infiltration in aortic dissection
Scientific Reports (2025)
-
Roles of lactylation in lipid metabolism and related diseases
Cell Death Discovery (2025)