Abstract
In the process of tumor treatment, systemic drug administration is hindered by biological barriers, leading to the retention of a large number of drug molecules in healthy tissues and causing unavoidable side effects. The precise deployment of drugs at the tumor site is expected to alleviate this phenomenon. Here, we take endostatin and Her2 (+) tumors as examples and develop an intelligent drug with simple “wisdom” by endowing mesenchymal stem cells (MSCs) with an intelligent response program (iMSCEndostatin). It can autonomously perceive and distinguish tumor cells from non-tumor cells, establishing a logical connection between tumor signals and drug release. Enable it to selectively deploy drugs at the tumor site, thereby locking the toxicity of drugs at the tumor site. Unlike traditional aggressive targeting strategies that aim to increase drug concentration at the lesion, intelligent drugs are more inclined to be defensive strategies that prevent the presence of drugs in healthy tissues.
Similar content being viewed by others
Introduction
In the process of tumor treatment, therapeutic drugs administered intravascularly encounter multiple biological barrier systems, including intravascular barriers, endothelial barriers, and extracellular matrix barriers, before reaching the target site [1,2,3]. These barriers can hinder drug molecules from reaching the tumor site, exposing them to healthy tissues and causing unavoidable side effects [4]. For example, although endostatin has shown significant therapeutic effects in lung cancer, breast cancer, ovarian cancer, and lymphoma, it distributes easily to all tissues, with over 90%–95% of endostatin accumulating in normal tissues and organs [5,6,7,8]. And these endostatin, which accumulate in the heart, can cause cardiomyocyte cell apoptosis and mitochondrial dysfunction through Apaf-1 and p53 [9]. In clinical practice, approximately 6.38% of patients may experience varying degrees of adverse cardiac reactions, especially about 2.1% of patients who have to terminate treatment due to cardiac reactions [10].
Although traditional targeted therapy modalities such as antibody-drug conjugates and cell carriers can alleviate this phenomenon [11, 12], off-target effects are difficult to avoid, and a large number of drug molecules still struggle to penetrate these biological barriers. While antibody-drug conjugates can enhance the affinity of drug molecules to tumors, they often lack the ability to chemotactic towards the tumor site and the driving force to break through these biological barriers [13]. Cell carriers can recognize tumor-released cytokines through chemokine receptors on the cell membrane surface and deliver drugs to the tumor site [14,15,16]. However, the microenvironment of many diseases may have similar characteristics to the tumor microenvironment. For example, in viral myocarditis, similar to the tumor microenvironment, the chemokine CCL4 is overexpressed [17, 18]. In addition, the initial function of the receptors on the surface of the platform carried by cells is not to recognize the tumor microenvironment, and they may have difficulty effectively distinguishing the source of chemokines, which may lead to these transport platforms deviating from their targets or losing direction.
Traditional targeting emphasizes “aggressive strategies” to enrich more drug molecules in the lesion. However, we believe that, when drugs cannot entirely avoid off-target effects, strategies focusing on “defensive” to prevent the presence of drug molecules in healthy tissues outside of biological barriers may be more important. Therefore, it is crucial to achieve the intelligence of drugs so that they can autonomously distinguish/judge tumor cells and healthy tissue cells.
The native Notch signaling pathway is an important means of cell-to-cell communication [19, 20]. Previous studies have indicated that in the Notch protein, both the extracellular domain responsible for ligand recognition and the intracellular domain acting as a transcription factor can be replaced. Only the core region of the Notch protein needs to be retained, and it can still exert Notch-like functionality [20,21,22]. This modular signaling mechanism allows for the customization of input and output signals for cells, establishing logical connections between tumor recognition and response feedback signals (Release/deploy drugs).
In order to achieve the above goals, this study takes Her2 (+) tumors and endostatin as examples. By reconstructing the Notch protein for mesenchymal stem cells (MSCs), an artificial receptor for recognizing Her2 (+) tumor cells and a response structure for producing/deploying endostatin were customized to it, creating an intelligent drug based on MSCs (iMSCEndostatin). Experimental verification shows that iMSCEndostatin exhibits extraordinary recognition/distinguishing ability for normal tissue cells from Her2 (+) tumor cells, which can precise deployment of endostatin at the tumor site, and locking treatment and drug toxicity to the lesion. Those iMSCEndostatin that have not broken through the biological barrier will not produce and secrete endostatin due to their inability to receive tumor signals, thus avoiding the damage caused by off-target effects on healthy tissue cells in traditional targeting. In summary, The selective drug deployment of iMSCEndostatin represents a defensive targeting strategy to reduce drug toxicity.
Materials and methods
Patients
This study was approved by the Ethics Committee of Xinxiang Central Hospital, and all patients were recruited from Xinxiang Central Hospital. Prior to participating in the study, all three patients provided written informed consent and agreed to the use of their samples for scientific research purposes. The study subjects were patients diagnosed with Her2-positive breast cancer, and all tumor tissue samples were evaluated using the immunohistochemistry (IHC) scoring system, with results of 3+.
Cells and animals
The MSCs utilized in this study were used in this study were obtained from the Zhongyuan Stem Cell Research Institute of Xinxiang High Tech Zone. All cell lines were authenticated by short tandem repeat analysis, and mycoplasma tests were negative. All experimental procedures were conducted in accordance with the guidelines approved by the Ethics Committee of Xinxiang Medical University. Female Balb/c mice and Balb/c nude mice, aged 6–8 weeks (18–25 g), were procured from Vital River Laboratories (Beijing, China; license No. SCXK (Beijing) 2016-0006). Mice were randomly assigned to cages and housed in a specific pathogen-free (SPF) environment, with conditions set to a temperature of 25 °C, humidity of 50 ± 5%, and a 12-h light-dark cycle. In this study, the investigator was blinded to the group allocation of the animals during the experiment. No statistical method was used to predetermine the sample size for the mouse experiment, which was based on preliminary experimental results. No data were excluded from the analysis.
Establishment of iMSCEndostatin and fluorescence-labeled cells
The recognition structure of iMSCEndostatin retains the core of Notch (Notch core), which is derived from the native Notch1 protein (nm_008714; Ile1427 to Arg1752). The extracellular and intracellular domains of the native Notch protein were replaced with Her2-affibody [23] and GAL4-VP64, respectively (recognition structure: Affibody-Notch(core)-GAL4-VP64). The sequence of the C-myc tag in the recognition structure is EQKLISEEDL. In the response structure (Gal4/UAS-Endostatin), we cloned five copies of the Gal4-DBD target sequence (GGAGCACTGTCCGAACG) into the minimal CMV promoter. The signal peptide (SA) sequence in the endostatin of the response structure is MALPVTALLPLALLLHAARP. The response structure contains a BFP tag. Therefore, the plasmid for the recognition structure is pLVX-Affibody-Notch(core)-GAL4-VP64, and the plasmid for the response structure is pHR-Gal4/UAS-Endostatin-IRES-mCherry-PGK-BFP. Subsequently, the recognition and response structures were integrated into the MSC genome via conventional lentiviral-mediated transfection.
BT474, Skov3, 293T, BJ, L02, Svog, HUVEC, and AC16 cells were labeled with GFP using lentivirus.
Immunofluorescence and western blotting
Human breast cancer tissue: The slices were permeabilized with 0.5% Triton X-100 and blocked with 10% goat serum. The primary antibodies are rat anti-Her2 (MA1-82367; invitrogen), mouse anti-mmp-2 (AB3284; Abways), and rabbit anti-mmp-9 (MA5-32705; invitrogen). The secondary antibodies are goat anti-rat Cy5-labeled, mouse anti-mouse FITC-labeled and goat anti-rabbit Cy3-labeled IgG.
iMSCEndostatin: Permeabilization and blocking were conducted following the aforementioned procedure. The primary antibody is a mouse-derived c-myc tag (AB0001; Abways). The secondary antibody is Goat anti-mouse Fitc-labeled IgG.
WB: The protein samples were denatured in a metal bath at 95 °C and blocked with 5% nonfat milk. The primary antibodies are mouse anti-C-myc (ab56; Abcam), rabbit anti-Cyclin B1 (ET1608-27; HUABIO), rabbit anti-CDK2 (ET1602-6; HUABIO), rabbit anti-PCNA (ET1605-38; HUABIO), and mouse anti-GAPDH (60004-1; Proteintech). The secondary antibodies are goat anti-mouse IgG-HRP and goat anti-rabbit IgG-HRP.
Recognition of Her2 (+) tumor by iMSCEndostatin
iMSCEndostatin was co-cultured with BT474-GFP, Skov3-GFP, 293T-GFP, BJ-GFP, L02-GFP, Svog-GFP, HUVEC-GFP, and AC16-GFP cells in DMEM medium for 24 hours. Subsequently, confocal microscopy, live cell imaging, and flow cytometry analyses were conducted.
Qualitative and quantitative analysis of endostatin production
Fluorescence analysis: iMSCEndostatin and Skov3-GFP were inoculated into a 24-well plate coated with fibronectin for different co-culture times (15 min, 12 h, 24 h, 36 h, 48 h). Subsequently, cells were fixed with 4% paraformaldehyde (PFA), and cells exhibiting fluorescence changes were imaged under a microscope.
Microplate reader detection: iMSCEndostatin and Skov3-GFP were co-cultured, and the mCherry signal was detected in the culture medium at 15 min, 12 h, 24 h, 36 h, and 48 h, respectively. Or iMSCEndostatin was co-cultured with Skov3-GFP for 48 hours, and then the mCherry signal was detected every 4 hours.
ELISA: MSCs or iMSCEndostatin will be co-cultured with Skov3-GFP for 48 h, and MSCs and iMSCEndostatin cells will be sorted by flow cytometry and cultured in a 24-well plate coated with fibronectin for 24 h. The content of endostatin will be detected using an ELISA detection kit (CSB-E07973h; CUSABIO).
Detection of vascular endothelial cell viability
Skov3h or AC16 cells were co-cultured with iMSCEndostatin (without mCherry labeling) for 48 h using the medium composed of a 1:1 mixture of DMEM and ECM. The conditioned medium was then collected and concentrated 5-fold using an ultracentrifugation tube.
CCK-8: 8 × 103 HUVEC cells were added into 96-well plates and cultured in different conditioned media for 48 h. The cell viability was detected using the CCK-8 assay.
CD105& WB: HUVEC cells were cultured in 6-well plates using different conditioned media for 48 h. Flow cytometry was conducted after incubation with CD105 antibody (51-9007648; BD StemflowTM) for 30 min. Or the expression of C-myc, Cyclin B1, CDK2, and PCNA were detected by WB.
Tube formation assay and matrigel plug assay
Tube formation assay: HUVEC cells were cultured with the aforementioned conditioned medium for 24 h (The experiment was divided into three groups: Control, Unactivated iMSCEndostatin, and Activated iMSCEndostatin). Subsequently, 50 µL of Matrigel was added to each well of a 96-well plate and HUVEC cells were incubated with the corresponding conditioned medium for 6 h. HUVEC cells were stained with calcein and imaged using a fluorescence microscope.
Matrigel plug assay: 200 µL Matrigel containing 50 µg bFGF was mixed with the above-conditioned medium and transplanted subcutaneously into female Balb/c nude mice (The experiment was divided into three groups: Control, Unactivated iMSCEndostatin, and Activated iMSCEndostatin, with each group consisting of 3 mice). After 9 days, the Matrigel was harvested for sectioning and CD34 staining (ab81289; abcam).
Tumor recognition and antitumor effect of iMSCEndostatin in vivo
Emt-6 cells were transfected with human Her2 protein and GFP by lentivirus.
Lung metastasis model: 2 × 106 Emt-6-GFP cells were injected into female Balb/c mice through the tail vein. 3 × 106 iMSCEndostatin cells were injected into the tail vein 3 days after colonization (n = 5). After 48 h, the samples were harvested, sectioned, and imaged by a confocal microscope.
Solid tumor model: 1 × 106 Emt-6-GFP cells were transplanted subcutaneously into mice, and 3 × 106 iMSCEndostatin cells were transplanted through the tail vein on day 11 (n = 5). After 48 h, tumors were harvested, sectioned, and imaged by confocal microscope.
Antitumor experiment: 1×106 Emt-6 cells were subcutaneously transplanted into mice. The experiment was divided into three groups: The control group, the MSC group, and iMSCEndostatin group (n = 5 mice per group). Subsequently, 3 × 106 iMSCEndostatin (without mCherry labeling)(iMSCEndostatin group) or MSC (MSC group) cells were transplanted through the tail vein on the 4th, 7th, and 10th days, respectively. On the 14th day, the tumor was harvested and weighed, the volume was measured and CD34 immunofluorescence staining was performed.
Cardiotoxicity
On the 14th day, ECG detection was performed on the aforementioned solid tumor mice. Serum was extracted for myocardial enzyme detection, and the heart was stained with hematoxylin and eosin (HE).
Statistical analysis
Statistical analysis was performed with the SPSS 8.0 statistics software. All data were reported as mean ± standard deviation. All cell experiments were performed in triplicate at least. Dunnett’s test was used for comparisons among ≥3 groups. Statistical testing was conducted bilaterally, with a p-value < 0.05 to indicate statistical significance.
Results
Design principles of iMSCEndostatin
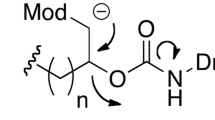
Our study aimed to design an intelligent drug that can recognize/distinguish normal tissue cells from Her2(+) tumor cells, and selectively deploy the drug (in this study is endostatin) only at the tumor site. The Her2 protein is a prevalent clinical marker for malignant tumors and is often accompanied by the upregulation of matrix metalloproteinase (mmp)-2 and mmp-9, thereby promoting tumor proliferation and metastasis (Fig. 1A). The native Notch protein consists of three parts: Notch extracellular domain (NECD), Transmembrane domain (TM), and Notch intracellular domain (NICD) (Fig. 1B). Previous studies have confirmed that Notch proteins can still perform Notch-like functions even after their extracellular and intracellular domains are replaced. Her2 (+) tumors, we retained the core region of the Notch protein (nm_008714; Ile1427 to Arg1752), substituted its extracellular and intracellular domains with the Her2-affibody and GAL4-VP64, and introduced CD8α signal peptide (MALPVTALLLPLALLLHAARP) and C-myc tag (EQKLISEEDL) in turn at the N-terminus of Her2-affibody (Fig. 1B and Fig. S1). Subsequently, to enable iMSCEndostatin to express endostatin, we designed a Gal4/UAS-endostatin structure in the response structure and added a BFP tag (Fig. 1B and Fig. S2). GAL4-VP64 in the iMSCEndostatin can connect recognition and response structures and transform tumor signals into signals related to the expression and secretion of endostatin. Due to the preservation of the core region of the native Notch protein in this program, when iMSCEndostatin recognizes Her2 (+) tumors, the γ-secretase in the cell can act on the S3 hydrolysis site of the core region, causing GAL4-VP64 to detach from the recognition structure and bind to the responsive structure, resulting in the expression of endostatin gene in iMSCEndostatin (Fig. S3). The green fluorescence and blue fluorescence in Fig. 1C represent the recognition structure and response structure of iMSCEndostatin, respectively, which together constitute the intelligent response program of iMSCEndostatin.
A Human Her2 (+) breast cancer samples. Pink, green, and red fluorescence of the presence of Her2 protein, mmp-2, and mmp-9, respectively. B The structure of iMSCEndostatin and its principle of responding to Her2 tumors. On the left side, display the structure of the native Notch protein and the structure of iMSCEndostatin. The structure of the native Notch protein includes the NECD (Notch extracellular domain), TM (transmembrane domain), and NICD (Notch intracellular domain). The recognition structure of iMSCEndostatin includes Her2-affibody, TM, and GAL4-VP64. The response structure of iMSCEndostatin mainly comprises the GAL4/UAS genetic regulatory elements and endostatin (therapeutic protein). On the right side is the process of iMSCEndostatin responding to Her2 tumors: iMSCEndostatin recognizes the Her2 protein on the tumor surface through its recognition structure, and subsequently, GAL4-VP64 transmits the tumor signal to initiate the expression of the drug-protein (endostatin). C Immunofluorescence images of the recognition structure and response structure of iMSCEndostatin.
iMSCEndostatin recognizes Her2 (+) tumors in vitro
The IRES structure guaranteed the co-expression of endostatin and mCherry in iMSCEndostatin. When iMSCEndostatin recognizes the tumor, the cells will exhibit red fluorescence (mCherry). To assess iMSCEndostatin’s recognition capability for Her2 (+) tumors, two co-culture systems were established: BT474 (human breast cancer)—iMSCEndostatin and Skov3 (human ovarian cancer)—iMSCEndostatin. The results revealed that iMSCEndostatin showed extraordinary recognition of Her2 (+) tumor cells (Fig. 2A–C). In the BT474—iMSCEndostatin co-culture system, iMSCEndostatin (red), which recognizes BT474 (green), closely encompassed the tumor cell mass, while unactivated iMSCEndostatin (blue) is observed where no recognition occurs (blue) (Fig. 2A, B). Similarly, in the Skov3-iMSCEndostatin co-culture system, the iMSCEndostatin that recognized Skov3 exhibited a distribution pattern similar to that of tumors (Fig. 2C). To further verify the reliability of the recognition of iMSCEndostatin, we divided the tumor area and non-tumor area in a macroscopic field of view with a diameter of 20 mm. As anticipated, iMSCEndostatin accurately distinguishes between tumor and non-tumor sites and achieved exclusive deployment of endostatin (red) in the tumor area (Fig. 2D). Subsequent flow cytometry indirectly confirmed the superior recognition capacity of iMSCEndostatin for Her2(+) tumors (Fig. 2E).
A–C Accurate recognition of BT474 and Skov3 tumors by iMSCEndostatin. The green fluorescent cells represent BT474 or Skov3 cells. Red cells indicate iMSCEndostatin that recognizes tumors, while blue cells indicate those that do not recognize tumors. D Macroscopic view of Her2 (+) tumor recognition by iMSCEndostatin. E Her2 (+) Tumor recognition by iMSCEndostatin detected by flow cytometry.
Intelligent differentiation of tumor and normal tissue cells by iMSCEndostatin
The intelligence of iMSCEndostatin is reflected not only in its ability to recognize tumors but also in its ability to distinguish tumor tissue from normal tissue cells. To verify this property, two types of tumor cells (breast cancer and ovarian cancer) and four types of normal tissue cells (kidney, skin, liver, and ovary) were co-cultured with iMSCEndostatin. The results demonstrated that iMSCEndostatin accurately distinguished between tumor and normal tissue cells, with activation occurring exclusively in Her2 (+) tumor cells and energy to the four types of normal tissue cells (Fig. 3A). Cardiotoxicity is the main side effect of endostatin, so it is necessary to prevent the deployment of endostatin in the heart. Considering the structure of the heart, cardiomyocyte cells (AC16) and vascular endothelial cells (HUVEC) were selected for co-culture with iMSCEndostatin. The results indicated that neither AC16 nor HUVEC could activate iMSCEndostatin (Fig. 3B). The biological barrier hinders a large number of drugs from reaching the tumor site, leading to the drugs being distributed in the lesions and healthy tissues respectively. The recognition and distinguishing ability of iMSCEndostatin to the tumor and normal tissue cells laid the foundation for its precise deployment of endostatin at the tumor site. This will avoid the toxic effects of drugs on healthy tissues and organs.
iMSCEndostatin deploys endostatin
In this study, the drug released by iMSCEndostatin upon recognition of tumors is endostatin. Since endostatin is a 20 kDa proteolytic fragment of the C-terminal noncollagenous domain (NC1) of type XVIII collagen, natural endostatin lacks a signal peptide structure. The deployment capability of iMSCEndostatin refers to secreting its produced endostatin out of the cell. Therefore, we reconstructed the SP structure of endostatin in iMSCEndostatin. To verify the capacity of iMSCEndostatin to produce and deploy endostatin, we removed mCherry from the response structure and fused it to the N-terminus of endostatin (iMSCEndostatin) (Fig. 4A). Under this structure, the red fluorescence signal will represent the endostatin produced by iMSCEndostatin, and subsequent confocal imaging confirmed the production capacity of iMSCEndostatin (Fig. 4B). The phenomenon of endostatin-mCherry secretion and deployment by iMSCEndostatin was further demonstrated through 3D imaging of Fig. 4B local (Fig. 4C). Subsequent live cell workstation imaging also dynamically showed iMSCEndostatin’s extraordinary recognition ability for Her2 (+) tumor cells and the phenomenon of deploying endostatin around the tumor (Fig. 5A and Video 1). For a more intuitive demonstration of iMSCEndostatin’s ability to secrete endostatin, we conducted 3D model fluorescence intensity imaging for Fig. 4C (Fig. 5B). The strong signal peak and weak signal peak in Fig. 5B correspond to the extracellular endostatin-mCherry that has not yet been secreted and the extracellular endostatin-mCherry that has been secreted, respectively. After washing with PBS, these weak signal peaks were lost in the endostatin-Skov3 co-culture system, which confirmed that these weak signal peaks originated from the secretion of iMSCEndostatin into extracellular endostatin (Fig. 5B).
Quantitative analysis of iMSCEndostatin’s deployment of endostatin
The quantitative analysis of the capacity of iMSCEndostatin to produce and deploy endostatin indirectly evaluated its therapeutic potential. Since the IRES structure in iMSCEndostatin enables the co-expression of endostatin and the mCherry gene, the accumulated red fluorescence intensity in iMSCEndostatin will reflect the expression of endostatin. Through fluorescence imaging of iMSCEndostatin-Her2 (+) tumor cells co-culture system, we can conclude that iMSCEndostatin can start to produce endostatin within 12 h after recognizing Her2 (+) tumor cells and reach the peak at 48 h (Fig. 6A). This conclusion was further supported by the fluorescence intensity of endostatin-mCherry accumulated every 12 h in the medium of iMSCEndostatin-Her2 (+) tumor cells co-culture system (Fig. 6B). Moreover, once the production of endostatin reaches a peak, iMSCEndostatin can continuously and stably produce endostatin, and similar amounts of endostatin-mCherry will be secreted into the medium every four hours (Fig. 6C). Given the similar domains of natural collagen XVIII and endostatin, to determine the concentration of endostatin, we subtracted the ELISA signal of the naïve MSCs group from that of the iMSCEndostatin group to exclude the interference of collagen XIII. The results indicated that every 5×104 activated iMSCEndostatin cells produced approximately 0.62 pg of endostatin every 24 h (Fig. 6D). Notably, in clinical practice, the number of stem cells injected intravenously can reach hundreds of millions, and the cells can survive in animal models for more than 6 months [24, 25]. The release of drug molecules is a specific response of iMSCEndostatin to received tumor signals, which will lock the toxicity of drugs at the tumor site. Although the process of iMSCEndostatin processing tumor signals is a slow response, it can continuously and selectively produce endostatin in high yields at the tumor site after being fully activated.
A Fluorescence intensity at various time points following iMSCEndostatin recognition of tumors. B The endostatin-mCherry released by iMSCEndostatin at different time points was detected by a microplate reader. C The microplate reader was utilized to detect the total amount of endostatin-mCherry accumulated every four hours following full activation of iMSCEndostatin. D The amount of released endostatin by iMSCEndostatin was quantified using ELISA detection.
iMSCEndostatin inhibits angiogenesis in vitro
The antitumor activity (in this article is inhibition of angiogenesis) of intelligent drugs originates from the drug proteins (in this article is endostatin) expressed by response structure. In vitro, the co-culture system of iMSCEndostatin-Her2 (+) tumor cells and iMSCEndostatin-AC16 cells (cardiomyocytes) can simulate iMSCEndostatin (recognition) activated at the tumor site and iMSCEndostatin (non-recognition) unactivated in healthy tissue, respectively. In the CCK-8 assay, we observed that only the activated iMSCEndostatin, which recognizes tumors, can inhibit the activity of vascular endothelial cells. In contrast, iMSCEndostatin that is not activated by cardiomyocytes (non-tumor cells) does not significantly affect the activity of vascular endothelial cells (Fig. 7A). CD105 is highly expressed in reshaped or newly formed blood vessels and can accurately reflect the proliferation status of endothelial cells and serve as a typical marker for evaluating the proliferation of vascular endothelial cells. Flow cytometry revealed that only activated iMSCEndostatin significantly inhibited the expression of CD105 in HUVEC (Fig. 7B, C), and consistent results were obtained via WB (Fig. 7D, E). Additionally, the tube formation assay is an important experiment for simulating vascular formation in vitro. Our results further demonstrated that the covered area, total branching points, total tube length, and total tubes in the activated iMSCEndostatin group were significantly lower than those in the control group (Fig. 7F–J), which strongly suggested that activated iMSCEndostatin significantly inhibits angiogenesis in vitro. Consistently, in the subsequent matrigel plug assay, the fluorescence area of CD34+ cells in the activated iMSCEndostatin group was also significantly lower than that in the control group (Fig. 7K, L). In conclusion, cell sensing/response pathways customized for iMSCEndostatin can enable them to autonomously sense user-specified disease or injury signals, and selectively deploy therapeutic functions at tumor sites.
A HUVEC cell viability was assessed using the CCK-8 assay. B, C The effect of activated iMSCEndostatin on the expression of CD105 in HUVEC was detected by flow cytometry. D, E Proliferation-related protein expression levels, including C-myc, Cyclin B1, CDK2, and PCNA in HUVEC, were assessed using WB. The relative expression of targeted proteins was quantified using ImageJ. The original blots corresponding to these experiments are displayed in Fig. S4. F–L The ability of activated iMSCEndostatin to inhibit vascular formation in vitro and in vivo was evaluated through tube formation assay and matrigel plug assay, respectively.
Tumor recognition and antitumor effect of iMSCEndostatin in vivo
Intelligent drugs are based on MSCs as the main structure and previous studies have demonstrated that the chemotaxis of MSCs facilitates them to perceive chemotactic signals and penetrate into tumor tissue [26]. To verify the ability of iMSCEndostatin to recognize Her2(+) tumor cells and its efficacy in inhibiting tumor growth in vivo, we established solid Her2(+) tumor and lung metastasis models. The results indicate that even within the in vivo context, the intelligent response program of iMSCEndostatin remains operational and allows the recognition of Her2(+) tumors and the administration of endostatin (Fig. 8A–C). Moreover, only a small number of cells were required to fully activate iMSCEndostatin (Fig. 8D). This may also enable iMSCEndostatin to play an advantage in micrometastasis lesions. After the transplantation of iMSCEndostatin (without mCherry labeling), significant inhibitory effects were observed on the weight (Fig. 8F), volume (Fig. 8E, G), and vascular density of the tumor (Fig. 8H, I) in model mice. Nevertheless, since natural MSCs do not contain an intelligent response program that drives endostatin, they cannot inhibit the formation of blood vessels and the progression of tumors (Fig. 8E–I). More importantly, consistent with our design expectations, there were no significant cardiotoxic reactions observed during iMSCEndostatin treatment. The heart structure (Fig. 9A), serum myocardial enzyme concentration (Fig. 9B–D), electrocardiogram (Fig. 9E), and heart rate (Fig. 9F) in the treatment group did not significantly differ from those in the control group.
A Recognition of solid tumors by iMSCEndostatin. B–D Recognition of tumors by iMSCEndostatin in lung metastasis models. E–G Images of tumor in model mice after iMSCEndostatin treatment, as well as tumor weight and volume. H, I CD34 staining of tumor sections in model mice after iMSCEndostatin treatment.
Discussion
Drug molecules distributed in healthy tissues due to the hindrance of biological barriers can cause potential toxic side effects [4]. Although traditional targeting strategies can increase the enrichment ability of drugs at the tumor site, they still cannot avoid a large number of drugs remaining in normal tissues [27,28,29,30]. Therefore, there is an urgent need for a drug-targeting approach capable of avoiding the presence of drug molecules in healthy tissues while completing treatment. Here, we introduce a completely different drug form using Endostatin and Her2 (+) tumors as an example: intelligent drug (iMSCEndostatin). In this study, we reconstructed the Notch protein in MSC cells, enabling iMSCEndostatin to acquire the ability to perceive/distinguish tumor and non-tumor cells and selectively deploy drugs (Figs. 2 and 4).
Intelligent drugs exhibit several distinct features over traditional drugs. Firstly, iMSCEndostatin is an intelligent drug with simple “wisdom”. Its intelligence is reflected in the recognition and distinguishing of tumor cells from healthy tissue cells. Through reshaping cellular behavior, intelligent drugs can convert recognized tumor signals into the production/secretion of drugs, establishing a logical connection between the two. This allows iMSCEndostatin to deploy drugs only at tumor sites, thereby confining/locking treatment and drug toxicity to the tumor site. Therefore, even though biological barriers can isolate drugs outside the lesion, unactivated iMSCEndostatin in healthy tissues does not deploy any drug molecules. Pursuing defense is the core advantage of intelligent drugs, which differs from traditional targeting strategies that focus on increasing drug concentration within lesions; intelligent drugs focus more on removing drugs outside lesions. Secondly, the intelligent drugs (iMSCEndostatin) is composed of MSCs and an intelligent response program (Fig. 1C). The advantage of MSCs is that they can have the ability to home to tumors like T cells, but unlike T cells, they can avoid tumor-induced immunosuppressive blockade [26, 31]. Moreover, the response program in iMSCEndostatin operates independently of the cell’s original structural proteins, freeing it from constraints imposed by the MSCs’s endogenous system. The expression/secretion of endostatin in iMSCEndostatin is solely regulated by the tumor signals received by iMSCEndostatin (Fig. 3B). Lastly, iMSCEndostatin serves as both a drug and a “drug factory”. Therefore, Once the recognition of the tumor is completed, it can continuously produce and secrete endostatin in high yield (Fig. 6C, D), which can greatly shorten the treatment cycle and frequency.
Due to the plasticity of its DNA-driven response program and the modular structure of the Notch protein [21, 32], intelligent drugs can predefine different input signals and output signals (Figs. 2 and 3). For example, by replacing the antigen receptor in the recognition structure to change the signal type recognized by intelligent drugs (target tumor type), or by changing the drug sequence in the response structure to enable iMSCEndostatin to output different drug types (Fig. 10). This enables users to design different drugs for personalized treatment according to different types of tumors.
Furthermore, the Notch pathway possesses a direct and simple signal transduction mechanism, and the signal transduction in its core region is triggered by the physical tension generated between cells [21, 33]. Therefore, the recognition of tumors by intelligent drugs only depends on their contact with it and is not regulated by various cytokines. This mechanism prevents the tumor from remotely activating intelligent drugs, thereby averting endostatin leakage. In addition, applying different signal transduction structures (such as Gal4-VP64 in the article) is expected to simultaneously introduce multiple sets of different response programs into intelligent drugs, giving them more “intelligence” to perform more complex actions (Fig. 10). In conclusion, the precise deployment of iMSCEndostatin for drug toxicity is an effective means to improve the side effects of drugs caused by biological barriers. This defensive targeting strategy provides a new option for cancer treatment.
Data availability
The raw data generated in this study are available upon request from the corresponding authors.
References
Blanco E, Shen H, Ferrari M. Principles of nanoparticle design for overcoming biological barriers to drug delivery. Nat Biotechnol. 2015;33:941–51.
Rosenblum D, Joshi N, Tao W, Karp JM, Peer D. Progress and challenges towards targeted delivery of cancer therapeutics. Nat Commun. 2018;9:1410.
Heldin CH, Rubin K, Pietras K, Ostman A. High interstitial fluid pressure—an obstacle in cancer therapy. Nat Rev Cancer. 2004;4:806–13.
Zhao Z, Ukidve A, Kim J, Mitragotri S. Targeting strategies for tissue-specific drug delivery. Cell. 2020;181:151–67.
Lopes-Coelho F, Martins F, Pereira SA, Serpa J. Anti-angiogenic therapy: current challenges and future perspectives. Int J Mol Sci. 2021;22:3765.
Guo J, Qin S, Liang J, Lin T, Si L, Chen X, et al. Chinese guidelines on the diagnosis and treatment of melanoma (2015 edition). Chin Clin Oncol. 2016;5:57.
Chen Y, Wang S, Lu X, Zhang H, Fu Y, Luo Y. Cholesterol sequestration by nystatin enhances the uptake and activity of endostatin in endothelium via regulating distinct endocytic pathways. Blood. 2011;117:6392–403.
Guo L, Li Z, Xu B, Yu M, Fu Y, Liu L, et al. Pharmacokinetics of PEGylated recombinant human endostatin in rhesus monkeys. Life Sci. 2019;238:116967.
Guan X, Li W, Wang Y, Zhao Q, Yu X, Jiang J, et al. The mechanism of rh-endostatin-induced cardiotoxicity and its protection by dihydromyricetin[in vivo/in vitro, C57BL/6 mice, AC16 and hiPSC-CMs. Toxicol Lett. 2023;377:29–37.
Mendez-Valdes G, Gomez-Hevia F, Lillo-Moya J, Gonzalez-Fernandez T, Abelli J, Cereceda-Cornejo A. et al. Endostatin and cancer therapy: a novel potential alternative to anti-VEGF monoclonal antibodies. Biomedicines. 2023;11:718.
Dean AQ, Luo S, Twomey JD, Zhang B. Targeting cancer with antibody-drug conjugates: promises and challenges. MAbs. 2021;13:1951427.
Wang H, Alarcon CN, Liu B, Watson F, Searles S, Lee CK, et al. Genetically engineered and enucleated human mesenchymal stromal cells for the targeted delivery of therapeutics to diseased tissue. Nat Biomed Eng. 2022;6:882–97.
Thanuja MY, Anupama C, Ranganath SH. Bioengineered cellular and cell membrane-derived vehicles for actively targeted drug delivery: so near and yet so far. Adv Drug Deliv Rev. 2018;132:57–80.
Ali S, Xia Q, Muhammad T, Liu L, Meng X, Bars-Cortina D, et al. Glioblastoma therapy: rationale for a mesenchymal stem cell-based vehicle to carry recombinant viruses. Stem Cell Rev Rep. 2022;18:523–43.
Gao C, Wang Q, Li J, Kwong CHT, Wei J, Xie B, et al. In vivo hitchhiking of immune cells by intracellular self-assembly of bacteria-mimetic nanomedicine for targeted therapy of melanoma. Sci Adv. 2022;8:eabn1805.
Xuan M, Shao J, Dai L, Li J, He Q. Macrophage cell membrane camouflaged Au nanoshells for in vivo prolonged circulation life and enhanced cancer photothermal therapy. ACS Appl Mater Interfaces. 2016;8:9610–8.
Zhu H, Galdos FX, Lee D, Waliany S, Huang YV, Ryan J, et al. Identification of pathogenic immune cell subsets associated with checkpoint inhibitor-induced myocarditis. Circulation. 2022;146:316–35.
Zhu Y, Chen M, Xu D, Li TE, Zhang Z, Li JH, et al. The combination of PD-1 blockade with interferon-alpha has a synergistic effect on hepatocellular carcinoma. Cell Mol Immunol. 2022;19:726–37.
Zhou B, Lin W, Long Y, Yang Y, Zhang H, Wu K, et al. Notch signaling pathway: architecture, disease, and therapeutics. Signal Transduct Target Ther. 2022;7:95.
Choe JH, Watchmaker PB, Simic MS, Gilbert RD, Li AW, Krasnow NA. SynNotch-CAR T cells overcome challenges of specificity, heterogeneity, and persistence in treating glioblastoma. Sci Transl Med. 2021;13:eabe7378.
Morsut L, Roybal KT, Xiong X, Gordley RM, Coyle SM, Thomson M, et al. Engineering customized cell sensing and response behaviors using synthetic notch receptors. Cell. 2016;164:780–91.
Tiemeijer LA, Sanlidag S, Bouten CVC, Sahlgren CM. Engineering tissue morphogenesis: taking it up a Notch. Trends Biotechnol. 2022;40:945–57.
Guo R, Zhang D, Zhang C, Yang Y, Liu H, Yang Y, et al. Immunotoxin IHP25-BT with low immunogenicity and off-target toxicity inhibits the growth and metastasis of trastuzumab-resistant tumor cells. Int J Pharm. 2021;608:121081.
Zangi L, Margalit R, Reich-Zeliger S, Bachar-Lustig E, Beilhack A, Negrin R, et al. Direct imaging of immune rejection and memory induction by allogeneic mesenchymal stromal cells. Stem Cells. 2009;27:2865–74.
Chung JW, Chang WH, Bang OY, Moon GJ, Kim SJ, Kim SK, et al. Efficacy and safety of intravenous mesenchymal stem cells for ischemic stroke. Neurology. 2021;96:e1012–e23.
Aravindhan S, Ejam SS, Lafta MH, Markov A, Yumashev AV, Ahmadi M. Mesenchymal stem cells and cancer therapy: insights into targeting the tumour vasculature. Cancer Cell Int. 2021;21:158.
Lammers T, Kiessling F, Ashford M, Hennink W, Crommelin D, Storm G. Cancer nanomedicine: is targeting our target? Nat Rev Mater. 2016;1:1–2.
Torrice M. Does nanomedicine have a delivery problem? ACS Cent Sci. 2016;2:434–7.
Kon E, Ad-El N, Hazan-Halevy I, Stotsky-Oterin L, Peer D. Targeting cancer with mRNA-lipid nanoparticles: key considerations and future prospects. Nat Rev Clin Oncol. 2023;20:739–54.
Chen S, Zhong Y, Fan W, Xiang J, Wang G, Zhou Q, et al. Enhanced tumour penetration and prolonged circulation in blood of polyzwitterion-drug conjugates with cell-membrane affinity. Nat Biomed Eng. 2021;5:1019–37.
Liang W, Chen X, Zhang S, Fang J, Chen M, Xu Y, et al. Mesenchymal stem cells as a double-edged sword in tumor growth: focusing on MSC-derived cytokines. Cell Mol Biol Lett. 2021;26:3.
Hyrenius-Wittsten A, Su Y, Park M, Garcia JM, Alavi J, Perry N. et al. SynNotch CAR circuits enhance solid tumor recognition and promote persistent antitumor activity in mouse models. Sci Transl Med. 2021;13:eabd8836.
Gordon WR, Vardar-Ulu D, Histen G, Sanchez-Irizarry C, Aster JC, Blacklow SC. Structural basis for autoinhibition of Notch. Nat Struct Mol Biol. 2007;14:295–300.
Acknowledgements
The authors wish to thank the Zhongyuan Stem Cell Research Institute of Xinxiang High Tech Zone for providing mesenchymal stem cells.
Funding
The authors also would like to acknowledge the Breast Cancer Translational Research Program (BCTRP@IPPT) matching grant scheme (1001/CIPPT/8070033), a collaboration between Universiti Sains Malaysia (1001/CIPPT/8070035) and CryoCord Sdn Bhd (304/CIPPT/6501351), which funded part of the project and provided Graduate Research Assistance (GRA). This work was also supported by the Natural Science Foundation of Henan Province (242300421199 and 235101610002).
Author information
Authors and Affiliations
Contributions
Conception and design: Yuliang Sun, Xinze Li, Yanan He, and Juntang Lin. Development of methodology: Yuliang Sun, Badrul Yahaya, Yilin Lu, Then Kong Yong, Cheong Soon Keng, and Juntang Lin. Conducted the experiments and analyzed the data: Yuliang Sun and Yanan He. Supervised the experimental design: Badrul Yahaya, Yanli Liu, and Juntang Lin. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The studies involving animals and human participants were reviewed and approved by the Ethics Committee of Xinxiang Medical University (Ethical approval number: XYLL-2020B005) and the Ethics Committee of Xinxiang Central Hospital (Ethical approval number: LHG20191311).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by Boris Zhivotovsky
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, Y., Lu, Y., Li, X. et al. Intelligent drugs based on notch protein remodeling: a defensive targeting strategy for tumor therapy. Cell Death Dis 15, 632 (2024). https://doi.org/10.1038/s41419-024-07008-7
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41419-024-07008-7