Abstract
Alzheimer’s disease (AD), the most common dementia in the elderly, is marked by progressive cognitive decline and neurodegeneration. Core pathological hallmarks include amyloid-beta (Aβ) plaques, hyperphosphorylated tau aggregates, neuroinflammation, and metabolic dysfunction (e.g., impaired glucose utilization, mitochondrial deficits). Apolipoprotein E4 (ApoE4), the strongest genetic risk factor for AD, interacts with these processes, yet its precise pathogenic mechanisms remain unclear. This review examines ApoE4’s multifaceted contributions to AD pathogenesis, focusing on its roles in Aβ accumulation, tau hyperphosphorylation, neuroinflammatory activation, and metabolic dysregulation. We further evaluate emerging therapeutic strategies targeting these pathways, including ApoE4 modulation, anti-amyloid/tau interventions, and metabolic rescue approaches. Elucidating the molecular interplay between ApoE4 and AD pathology is critical for developing targeted therapies to modify disease progression and mitigate cognitive decline in patients.
Similar content being viewed by others
Facts
-
ApoE4 exacerbates Aβ pathology by enhancing Aβ production and impairing Aβ clearance mechanisms. ApoE4-induced metabolic dysregulation, oxidative stress, and inflammatory responses further amplify these effects.
-
ApoE4 enhances tau pathology by activating oxidative stress, disrupting lipid metabolism, and triggering inflammatory signaling.
-
ApoE4 increases ROS production, activates the NLRP3 inflammasome, and modulates the TREM2 signaling pathway to amplify microglial inflammation.
-
ApoE4 disrupts neuronal energy metabolism and mitochondrial function by competing for insulin receptors, inhibiting key metabolic enzymes, and promoting lipid accumulation.
Open questions
-
What are the precise molecular mechanisms by which ApoE4 disrupts Aβ clearance and accelerates its production?
-
How does ApoE4 specifically alter tau pathology through oxidative stress and lipid metabolism in neurons and glial cells?
-
What therapeutic strategies can effectively target ApoE4-induced microglial inflammation and improve neuroinflammation in Alzheimer’s disease?
Introduction
Alzheimer’s disease (AD) is a neurodegenerative disorder marked by progressive cognitive decline and memory loss, representing the most common form of dementia in the elderly. While the precise pathogenesis of AD remains elusive, research indicates that key pathological features include the accumulation of extracellular amyloid-beta (Aβ) plaques, abnormal tau phosphorylation and aggregation, neuroinflammation, and various metabolic disruptions, such as impaired glucose metabolism and mitochondrial dysfunction. These factors are interrelated, contributing to the progression of neurodegeneration [1].
Apolipoprotein E (ApoE), an important lipoprotein in the central nervous system, is crucial for lipid transport and cholesterol homeostasis in the brain [1]. It is mainly produced by astrocytes and activated microglia in the brain, although recent studies have also demonstrated ApoE production by neurons [1,2,3]. In peripheral tissues, it is synthesized by the liver and macrophages [3]. The human ApoE gene has three isoforms—ApoE2, ApoE3, and ApoE4—of which ApoE4 is the major genetic risk factor for AD. Despite minor structural differences between ApoE4 and the other isoforms, ApoE4 is more compact and unstable, which affects its lipid-binding ability and impairs the clearance of amyloid-beta degradation products [4]. Furthermore, ApoE4 is implicated in hyperphosphorylation of tau, enhanced neuroinflammation, and increased oxidative stress [5].
The pathological effects of ApoE4 also extend to disruptions in brain energy metabolism. ApoE4 carriers exhibit impaired mitochondrial function, increased lipid oxidation, and interference with insulin signaling, leading to early-stage brain glucose metabolism deficits. These metabolic abnormalities significantly increase the risk of cognitive decline in ApoE4 carriers [6].
This review explores the mechanisms by which ApoE4 influences Aβ accumulation, tau phosphorylation, neuroinflammation, and metabolic dysregulation, and evaluates current therapeutic strategies targeting these processes. By understanding the multifaceted roles of ApoE4, we aim to provide new insights for AD research and support future clinical treatments and personalized medicine.
Mechanisms underlying ApoE4 regulation of Aβ pathology
One of the key pathological features of Alzheimer’s disease (AD) is the extracellular deposition of Aβ in the brain in the form of amyloid fibrils. Aβ is a 38- to 43-residue peptide fragment derived from the membrane-bound β-amyloid precursor protein (APP) via sequential proteolytic cleavages by β- and γ-secretase enzyme activities [4]. The Aβ protein includes two major forms, Aβ42 and Aβ40, with Aβ42 being more toxic and more prone to aggregation [7]. Aβ aggregates, including oligomeric aggregates (oAβ) and amyloid plaques, can interfere with normal neuronal function in various ways, including damaging cell membranes, disrupting intracellular signaling, inducing oxidative stress, and promoting inflammation [8].
Although ApoE’s critical role in AD pathology is well established, the exact mechanisms by which it influences disease progression remain unclear. ApoE may act both as an AD inhibitor and promoter [4, 9], profoundly affecting Aβ metabolism through several pathways: (1) Promoting APP Expression: ApoE4 enhances APP transcription directly or via signaling pathways like extracellular signal-regulated kinase (ERK), nuclear factor-κB (NF-κB), and C/EBPβ [10, 11]. ApoE4 could also boost APP transcription by interacting with transcription factors like Sp1 and through epigenetic modifications that alter the chromatin structure of the APP gene [12, 13]. (2) Enhancing APP Processing Enzyme Activity: ApoE4 increases BACE1 transcription through interactions with transcription factors such as NF-κB, C/EBPβ, and Sp1 [11, 12], and promotes BACE1 activity by inhibiting insulin signaling and activating GSK3β [14]. ApoE’s C-terminal region can inhibit γ-secretase in neurons, providing a protective effect against Aβ generation, though this inhibition is weaker in ApoE4 [15]. (3) Cholesterol Metabolism Disruption: ApoE4 increases cholesterol secretion from astrocytes, which enhances lipid raft formation in neurons, aiding APP localization and processing [16]. High cholesterol levels promote APP transport to lipid rafts, where it interacts with β- and γ-secretase, driving Aβ production [17]. (4) Endosomal Trafficking Abnormalities: ApoE4 promotes APP internalization and colocalizes APP and BACE1 in early endosomes, delaying endosomal-lysosomal trafficking and APP processing, thus promoting Aβ generation [18,19,20]. In addition to these pathways, ApoE4 mediates inflammatory responses, metal ion dysregulation, oxidative stress, and energy metabolism defects, all of which may contribute to Aβ production and aggregation [21,22,23,24].
Aβ is primarily produced in neurons and secreted into the interstitial fluid (ISF). Proteolytic degradation by endopeptidases (e.g., insulin-degrading enzyme (IDE), neprilysin (NEP)) constitutes a major Aβ clearance pathway [25]. Studies have shown that NEP and IDE are expressed in both neurons and glial cells, while ApoE4 can inhibit the expression and activity of IDE and NEP, thereby preventing Aβ clearance [26, 27]. It has been reported that the expression of IDE and NEP in the brains of ApoEε4 carriers is significantly lower compared to non-carriers [26, 28, 29]. In neurons, ApoE4 can downregulate IDE expression by activating the N-methyl-D-aspartate (NMDA)/cAMP-dependent protein kinase (PKA) signaling pathway [30]. Studies on astrocytes have shown that under LPS signaling stimulation, ApoE4 can downregulate NEP expression via TLR4-dependent pathways, and the use of LXR agonists can promote NEP upregulation. This suggests that the impact of ApoE4 on NEP expression may be related to inflammatory responses and cholesterol metabolism dysregulation [31].
Cellular clearance of Aβ, mediated by neurons, microglia, and astrocytes through the lysosomal system, plays a key role in Aβ degradation [25]. Both ApoE and Aβ bind to receptors such as LRP1, LDLR, and HSPGs on neurons and glial cells, meaning ApoE can compete with Aβ for receptor binding, potentially interfering with Aβ uptake and clearance [32, 33]. ApoE4 exacerbates this by impairing the autophagy-lysosome pathway, downregulating autophagy-related genes, inducing lysosomal alkalization, and disrupting lysosomal membrane integrity, all of which hinder Aβ degradation [20, 34, 35]. Furthermore, ApoE4 reduces cholesterol efflux, leading to cholesterol accumulation inside cells, which decreases Rab7 recycling. This slows Aβ transport to the lysosome [36]. Cholesterol buildup in the late endosome-lysosome compartment also raises their pH, impairing function and further obstructing Aβ clearance [37]. On the other hand, ApoE4-induced mitochondrial dysfunction and insulin resistance negatively affect energy metabolism, promoting BACE1 expression and compromising Aβ clearance [24, 38]. Studies show that in response to Aβ, microglia shift from oxidative phosphorylation (OXPHOS) to glycolysis to meet energy demands for proliferation, migration, cytokine secretion, and phagocytosis. However, widespread metabolic defects in both glycolysis and OXPHOS push microglia into a chronic tolerance state, reducing immune responses, including diminished cytokine secretion and phagocytosis [39] (Fig. 1).
1.In the context of ApoE4, microglia exhibit pathological features such as lipid accumulation, increased ROS production, elevated ICs secretion, and lysosomal dysfunction, which impair their phagocytic function and effective clearance of Aβ [36, 94, 129]. ROS reduce the activity of Aβ-degrading enzymes, such as IDE and NEP [130, 131], while inflammatory cytokines promote the expression of APP as well as β- and γ-secretases, thereby enhancing APP processing [132, 133]. 2.ApoE4 may drive microglia to shift from OXPHOS to aerobic glycolysis to meet the high energy demands of the inflammatory respons. In this process, the TREM2/mTOR pathway plays a crucial role [39]. However, ApoE4 may negatively regulate TREM2 signaling [95, 97]. Furthermore, ApoE4 could interfere with Aβ uptake and internalization by competing with Aβ for receptors like LRP1 and LDLR [32, 33]. 3.ApoE4 can activate ERK and NF-κB signaling and inhibit insulin signaling, promoting the transcription of APP and BACE1 [10, 28, 57, 134]. 4.ApoE4 may act as a molecular chaperone to facilitate the internalization of APP and promote the co-localization of APP and BACE1 in EE, while delaying endosome-lysosome recycling [18,19,20]. 5.Both ApoE4 and Aβ can activate CDK5 signaling or increase ROS production, leading to GF, which increases the co-localization of APP and BACE1 and promotes Aβ generation [53, 135]. AKT, protein Kinase B; APP, β-amyloid precursor protein; BACE1, Beta-site amyloid precursor protein cleaving enzyme 1; CDK5, cycline dependent kinase-5; DLK, dual leucine-zipper kinase; EE, early endosome; ERK1/2, extracellular signal-regulated kinase 1/2; GF, golgi fragmentation; GSK-3β, glycogen synthase kinase-3β; ICs, inflammatory cytokines; IDE, insulin-degrading enzyme; IR, insulin receptor; LDLR, low-density lipoprotein receptor; LE, late endosome; MKK7, mitogen-activated protein kinase kinase 7; LRP1, low-density lipoprotein receptor-related protein 1; mTOR, mechanistic target of rapamycin; NEP, neprilysin; NOX, NADPH oxidase; OXPHOS, oxidative phosphorylation; PI3K, phosphoinositide 3-kinase; RE, recycle endosome; ROS, reactive oxygen species; Trem2, Triggering Receptor Expressed on Myeloid Cells 2.
Currently FDA-approved Aβ-targeting drugs include Aducanumab and Lecanemab. While Aducanumab slows AD progression by reducing Aβ plaques, its cognitive benefits remain controversial, and some patients may experience side effects such as brain edema [40]. Lecanemab, in clinical trials, has demonstrated efficacy in slowing cognitive decline in patients with mild AD and significantly reducing Aβ deposition, though challenges remain in fully addressing both clinical efficacy and side effects [41]. Besides, several anti-amyloid antibodies currently under investigation, such as Crenezumab and Gantenerumab, have also shown great potential in clearing Aβ. However, these antibodies generally carry a significant risk of amyloid-related imaging abnormalities (ARIA), particularly in ApoE4 carriers, which limits their use [42]. At present, new immunotherapies and vaccines are also under development, aiming to eliminate Aβ deposition through more precise immune responses (Table 1).
It is noteworthy that both AD and cerebral amyloid angiopathy (CAA) are characterized by the accumulation of Aβ in the brain. However, while Aβ primarily deposits in the brain parenchyma in AD, in CAA, it mainly deposits in the walls of cerebral blood vessels [43]. CAA is commonly observed in patients with AD. Genetically, AD and CAA share the ApoEε4 gene as one of the strongest genetic risk factors for both diseases. This shared genetic risk may contribute to vascular damage in CAA during anti-Aβ antibody treatments, which manifests as amyloid-related imaging abnormalities (ARIA) [43, 44]. Current epidemiological studies suggest that the ApoEε2 allele may promote specific ‘CAA-related vascular changes’ and potentially act as a risk factor for amyloid-related vascular hemorrhage. In contrast, ApoEε4 primarily enhances Aβ deposition in the walls of cerebral blood vessels, with oxidative stress potentially playing a key role in this process [45, 46]. In the 5XFAD mouse model, which expresses human ApoE4+/+ (5XE4) and exhibits prominent CAA and parenchymal plaque pathology, treatment with anti-Aβ antibodies exacerbated the severity of microhemorrhages. However, treatment with the anti-human ApoE antibody HAE-4 effectively reduced Aβ deposition [44]. These findings suggest that the risks associated with CAA and the complex role of ApoE in anti-Aβ treatment for AD should be considered, highlighting the importance of personalized treatment strategies.
Mechanisms underlying ApoE4 regulation of tau pathology
Phosphorylated tau (p-tau) is another hallmark of Alzheimer’s disease, alongside Aβ plaques. Tau, a protein mainly found in neuronal axons, stabilizes microtubules essential for maintaining neuronal structure and function. Under normal conditions, moderately phosphorylated tau binds to microtubules and lipid membranes, supporting neuronal integrity and signaling. However, excessive phosphorylation impairs tau’s binding to microtubules, destabilizing the cytoskeleton, leading to neurofibrillary tangles (NFTs) and disrupting normal neuronal function [47]. For a long time, the prevailing view has been that the abnormal accumulation of Aβ and p-tau are interrelated in the pathology of AD [48]. However, several studies have pointed out that these two pathologies may be independent of each other [49, 50]. Specifically, research by Wang et al. showed that in human neurons derived from induced pluripotent stem cells (hiPSC) expressing ApoE4, p-tau levels were abnormally elevated even when Aβ generation was blocked, specifically leading to degeneration and loss of GABAergic neurons. This finding suggests that ApoE4 may independently promote tau pathology through mechanisms unrelated to Aβ pathology [49]. In P301S Tau transgenic mice carrying different ApoE isoforms, tau protein-mediated neurodegeneration exhibited an ApoE isoform-dependent pattern (ApoE4 > ApoE3 > ApoE2), and the deletion of ApoE4 significantly reduced tau pathology, implying that ApoE4 may participate in the progression of tau pathology through a toxic gain-of-function mechanism [50]. It has been reported that knocking down ApoE4 in astrocytes can rescue tau pathology and microglial phagocytosis of synaptic material [51]. However, other studies have shown that human astrocyte-derived ApoE4 does not confer detrimental effects in human neurons (at least with regard to tau phosphorylation, GABAergic neuron degeneration, and Aβ production) [49]. In tau mouse models, selective knockout of ApoEε4 in neurons led to significant improvements in tau pathology, glial proliferation, neurodegeneration, neuronal hyperexcitability, and myelin loss [52]. These findings suggest that the toxic effects of ApoE4 may be neuron-specific. The specific toxic role of ApoE4 from different cell sources in tau pathology requires further investigation to provide a comprehensive understanding.
The exact mechanisms by which ApoE4 regulates tau pathology are not yet fully understood, but several possible pathways have been proposed based on current research: (1) Imbalance in Tau Kinases/Phosphatases System: ApoE4 can promote tau phosphorylation by activating several kinases, such as glycogen synthase kinase-3β (GSK-3β), cyclin-dependent kinase-5 (CDK5), and mitogen-activated protein kinase (MAPK) [53,54,55]. On the other hand, ApoE4 can influence tau dephosphorylation by inhibiting the activity of the major tau phosphatase protein phosphatase 2A (PP2A) [56]. (2) Neuroinflammation: ApoE4 plays a critical role in neuroinflammation. ApoE4 can activate inflammatory signaling pathways through multiple routes, promoting the release of pro-inflammatory cytokines, which in turn activate kinases such as GSK-3β, inducing tau hyperphosphorylation and the formation of NFTs [57,58,59]. (3) Dysregulation of Lipid Metabolism: The inefficiency of ApoE4 in lipid transport leads to inadequate cholesterol turnover in neurons, an imbalance in specific phospholipid ratios, lipid accumulation, and increased lipid peroxidation. These changes disrupt the structure and function of cell membranes, affect tau phosphorylation-related signaling, and ultimately exacerbate tau pathology [60,61,62]. (4) Iron Overload: ApoE4 increases the expression of ferritin, the iron storage protein, leading to excessive intracellular iron deposition. This excess iron activates kinases associated with tau phosphorylation by promoting oxidative stress (OS) and other signaling pathways. Severe OS can even trigger ferroptosis [63, 64]. (5) Oxidative Stress: ApoE4 can impair mitochondrial function through various mechanisms, leading to increased ROS generation and triggering OS [65, 66]. OS not only activates kinases such as GSK-3β and CDK5 but also promotes tau phosphorylation through mechanisms such as inducing inflammation, inhibiting insulin secretion, and altering tau protein conformation [65,66,67,68].
Under both physiological and pathological conditions, tau protein metabolism involves two major pathways: the autophagy-lysosome pathway and the ubiquitin-proteasome system (UPS) [69]. The presence of ApoE4 has been shown to be associated with dysfunction in the autophagy-lysosome pathway. Specifically, ApoE4-expressing cells exhibit inhibited autophagy, reduced lysosomal proteolysis, insufficient lysosomal acidification, and lysosomal rupture, leading to the premature release of undigested contents, which may affect tau clearance [20, 70, 71]. Additionally, ApoE4 has been confirmed to potentially interfere with ubiquitin signaling and protein degradation processes, thereby affecting tau metabolism and aggregation [72, 73]. Recent studies have confirmed that LRP1 plays a key role in controlling tau endocytosis, degradation, and subsequent propagation [74]. ApoE4, through its cofactor glypican-4 (GPC-4), not only strongly induces tau hyperphosphorylation but also promotes the transport of LRP1 to the cell surface, providing a crucial channel for tau protein diffusion [75]. However, other studies have found that ApoE4 can reduce the distribution of receptors such as LRP1 on the cell membrane by interfering with receptor-mediated endocytic recycling through the endosome pathway [76]. Moreover, ApoE4 can also compete with tau protein for binding to LRP1, thereby slowing down LRP1-mediated tau endocytosis and degradation [77]. These findings suggest that ApoE4 provides a crucial channel for tau protein diffusion but also somewhat limits this diffusion, reflecting the complexity of ApoE4’s role in the regulation of tau uptake, degradation, and propagation (Fig. 2).
1.ApoE4 may promote tau phosphorylation by activating relevant kinases [53,54,55]. 2.ApoE4 can enhance the expression of ferritin, induce iron overload, trigger oxidative stress and lipid peroxidation, and even lead to ferroptosis [22, 63, 64]. 3.ApoE4-mediated lipid metabolism defects result in elevated fatty acid levels, which activate tau phosphorylation-related kinases, impair mitochondrial function, and activate the NF-κB pathway [60,61,62]. 4.ApoE4 can promote the generation of ROS and activate the NF-κB signaling pathway, which in turn activates kinases such as GSK-3β, leading to tau phosphorylation [65,66,67,68, 88]. Phosphorylated tau, in turn, can further activate the NF-κB pathway, exacerbating the inflammatory response [136]. 5.ApoE4 significantly downregulates the expression of the PPP2R5E gene, leading to decreased activity of the major tau phosphatase PP2A [56]. 6.ApoE4 can promote the endocytic recycling of LRP1, providing a channel for tau diffusion [75]. 7.ApoE4 competes with tau for LRP1, restricting tau diffusion [77]. 8. ApoE4 interferes with the autophagy-lysosome pathway and the ubiquitin-proteasome system (UPS), hindering tau degradation [20, 71,72,73]. CDK5 cycline dependent kinase-5, GSK-3β glycogen synthase kinase-3β, MAPK mitogen- activated protein kinase, FFA free fatty acid, NFTs neurofibrillary tangles, PP2A protein phosphatase 2A, Tf transferrin, TfR transferrin receptor.
Currently, there are relatively few targeted drugs aimed at the tau protein. LMTM is a small-molecule drug designed to inhibit tau aggregation and tangling. While it has demonstrated good safety, it failed to significantly improve cognitive function in AD patients during clinical trials [78]. Ongoing drug developments, such as BIIB092 (Tilavonemab) and TPI-287, aim to precisely target tau protein to reduce its propagation or aggregation and improve cognitive function in patients (Table 2).
Mechanisms underlying the role of ApoE4 in neuroinflammation
Neuroinflammation is one of the key drivers of neurodegenerative changes and is considered the third most important mechanism in AD pathology, following Aβ deposition and neurofibrillary tangles [79]. Neuroinflammation is instigated by the misfiring of immune cells in the central nervous system (CNS), involving microglia and astrocytes as key cell types [80]. In the early stages of AD, the activation of microglia and astrocytes may initially serve as a defense mechanism, aimed at protecting the brain by promoting tissue repair and clearing cellular debris and Aβ aggregates. However, over time, chronic inflammation can lead to synaptic loss and neuronal death, which exacerbates the progression of AD [81].
Microglia, the primary innate immune cells in the brain, play a central role in the brain’s immune response. However, in the context of AD, excessive microglial activation is not merely an inflammatory bystander effect, but likely a critical upstream mechanism. Research has shown that the interaction between microglial activation and Aβ pathology promotes tau protein propagation, eventually leading to widespread brain damage and cognitive impairment [82]. There is substantial evidence indicating that ApoE4 plays a key role in the activation of microglia and influences the risk and progression of AD through neuroinflammation [50, 83]. In vitro experiments have confirmed that microglia expressing ApoE4 exhibit a stronger immune response upon lipopolysaccharide (LPS) stimulation. When co-cultured with neurons, the levels of TNF-α significantly increase, leading to a notable decrease in neuronal viability and an increase in cell death [50]. Similar results have been observed in vivo, where ApoE4 mice showed increased glial cell activation in response to LPS injected into the lateral ventricle compared to ApoE2 and ApoE3 mice. Additionally, these ApoE4 mice displayed higher levels of IL-1β, IL-6, TNF-α secretion, and greater synaptic protein loss [84]. ApoE not only affects innate immunity but also participates in the regulation of a wider range of adaptive immune responses [85]. In tauopathy mouse models, ApoE4 significantly increases cytotoxic T cell numbers. Mechanistically, ApoE4 may recruit T cells by modulating microglial activation. The IFN-γ secreted by these T cells worsens microglial inflammation and antigen presentation, creating a feedback loop that accelerates tau pathology and neuronal damage [86].
During the immune activation of microglia, ROS play a crucial role as pro-inflammatory molecules [87]. ApoE4 and Aβ have been shown to increase ROS production through various mechanisms, including mitochondrial damage, activation of NADPH oxidase (NOX), and induction of endoplasmic reticulum stress [65, 88,89,90]. ROS, in turn, activate inflammatory signaling pathways such as NF-κB and MAPK, thereby promoting the expression of pro-inflammatory factors [91]. ROS can also enhance microglial sensitivity to pathological signals, thereby exacerbating neuroinflammatory responses [92]. Choi et al. examined human AD postmortem brain samples and found that, compared to age-matched controls, microglial “pro-inflammatory” (M1) marker gene expression was increased, and this effect was associated with an increase in the NOX2 p47phox subunit [93]. In vitro and in vivo experiments have also confirmed that inhibition or knockout of NOX2 significantly reduces the ability of Aβ to induce ROS in microglia and in the brains of aged mice [94]. These findings suggest that NOX2-derived ROS may play a key role in microglial activation. In addition, ApoE4, Aβ, and damage-associated molecular patterns (DAMPs) such as cell debris, ATP, and HMGB1 released after cellular damage can bind to various receptors on the surface of microglial membranes, including TREM2, microglial toll-like receptor 4 (TLR4), and CD36, thereby activating microglia (Table 3).
Existing studies have shown that TREM2, one of the receptors for ApoE, plays a complex and dynamic role in the progression of AD. In the early stages, TREM2 activation may aid in clearing Aβ plaques and suppressing inflammation through the PI3K/NF-κB pathway, providing neuroprotective effects. However, as the disease advances, prolonged TREM2 activation fails to effectively clear Aβ and instead exacerbates inflammation [95, 96]. To explore whether ApoE4 affects TREM2-mediated phagocytosis of apoptotic cells, Kloske et al. activated phagocytic responses in mice by injecting phosphatidylserine (PS), a key marker on the membrane of apoptotic cells and a major activator of TREM2. The results showed that, compared to control mice, ApoE4 mice exhibited lower levels of microglial activation and weakened TREM2-mediated phagocytosis. However, these mice showed significantly upregulated pro-inflammatory gene expression, suggesting that ApoE4 may have a negative regulatory effect on TREM2 signaling [95]. In vitro experiments by Li et al. also supported this view [97]. TREM2 has also been confirmed to be a key transcriptional regulator of cholesterol transport and metabolism, and its functional deficiency leads to the accumulation of pathogenic lipids in microglia [98]. Conversely, ApoE4-mediated lipid metabolism dysregulation can inhibit TREM2 signaling, impairing the clearing function and anti-inflammatory capacity of microglia [99] (Fig. 3).
1.The exogenous and endogenous ROS generation mediated by ApoE4 and Aβ can activate inflammatory signaling pathways, primarily through NF-κB [65, 88,89,90]. ApoE4 can also directly influence NF-κB transcription [57]. 2.Excessive ROS production and lysosomal damage (leakage of hydrolases) induced by ApoE4, Aβ, tau, and other factors can activate the NLRP3 inflammasome, promoting the cleavage of Pro-IL-1β and Pro-IL-18 [71, 90]. 3.TREM2 not only promotes phagocytosis, suppresses inflammation, and reduces lipid accumulation, but also supports aerobic glycolysis via the mTOR pathway to provide energy for the inflammatory response; however, its signaling may be negatively regulated by ApoE4 [39, 95, 98]. 4. ApoE4-mediated lipid metabolism dysregulation can also enhance MHC-II-dependent antigen presentation and T cell activation in microglia, while upregulating neuronal MHC-I expression, thereby amplifying immune signaling [129]. 5.Under inflammatory conditions, ApoE4 increases GLS activity, further inducing microglial activation and promoting glutamate production and release, exacerbating neurotoxicity [137]. ATP adenosine triphosphate; DAP12 DNAX-activating protein of 12 kDa; HMGB1 high mobility group box 1; Gln glutamine; GLS glutaminase; GLu glutamate; LilrB3 leukocyte immunoglobulin-like receptor B3; MHC major histocompatibility complex; MyD88 myeloid differentiation primary response gene 88; TLR4 toll-like receptor 4; TRAF2 nuclear factor receptor-associated factor 2.
Astrocytes primarily function to provide metabolic support to neurons, but like microglia, they also play an important role in immune responses in the central nervous system and are considered key regulators of neuroinflammation in AD [100]. Studies show that when microglia are activated and produce IL-1β, C1q, and TNF-α, astrocytes respond and become activated, forming a positive feedback loop that releases inflammatory factors, thus creating a harmful environment for surrounding tissue [101]. Moreover, increasing evidence suggests that ApoE4-mediated lipid dysregulation also plays a significant role in the pro-inflammatory activation of astrocytes. Recent research by Sienski et al., using astrocytes derived from iPSCs of ApoE4 or ApoE3 carriers, indicated that compared to ApoE3-carrying astrocytes, ApoE4 promotes the accumulation of lipid droplets and the buildup of unsaturated fatty acids [102]. This ApoE4-dependent lipid droplet accumulation impairs the ability of astrocytes to support neuronal metabolism and synaptic function [103]. Furthermore, the accumulation of lipid droplets is sufficient to induce astrocyte reactivity, triggering the secretion of inflammatory chemokines and cytokines [99, 104]. These two types of glial cells cooperate to amplify neuroinflammatory signaling, leading to oxidative stress, iron overload, and neurotoxicity, which worsen neuronal damage [101, 104].
Based on the current understanding of the inflammatory mechanisms in AD, regulating the inflammatory response appears to be a promising therapeutic strategy for AD. Although many epidemiological studies support the idea that long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) can help prevent AD, these drugs do not slow the progression of the disease in diagnosed patients and may cause many adverse side effects during prolonged use [105]. One potential reason for their limited efficacy is the challenge of crossing the blood-brain barrier (BBB), a key factor influencing drug effectiveness. To address this, we have explored strategies to enhance drug delivery across the BBB. By synthesizing ApoE or ApoB amino acid fragments that bind to the low-density lipoprotein receptor (LRP) and conjugating them with our designed iron-chelating peptide J-bs5YP, we successfully transported the peptide into the brains of AD mice. This promoted Slc40a1 transcription and increased ferroportin levels, facilitating excess iron and free radical clearance, thereby reducing Aβ plaque formation, tau phosphorylation, and neuronal damage [106, 107]. Future advancements in optimizing BBB-targeting strategies and developing multifunctional drug designs could enhance therapeutic efficacy, offering new hope for AD treatment.
The impact of ApoE4 on brain energy metabolism
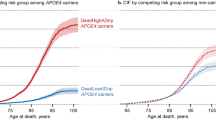
The brain is a high-energy-consuming organ with extremely active metabolism. Under normal physiological conditions, the primary source of energy for the brain is glucose. Despite comprising only about 2% of body weight, the brain consumes approximately 20–25% of the body’s glucose, providing energy through glycolysis, the tricarboxylic acid cycle, and mitochondrial OXPHOS [108]. Impaired glucose metabolism in the brain is an early feature of AD. Before clinical symptoms appear in individuals with mild cognitive impairment (MCI) or AD, the brain already shows a decline in glucose metabolism, and there is evidence suggesting that ApoE4 may play a key role in this process [109, 110]. An 84-month longitudinal FDG-PET study showed that, in the context of MCI, the ApoE ε4 genotype is associated with a longitudinal decline in glucose uptake in multiple brain regions [109]. In a study involving 806 cognitively normal (CN) participants, 35 MCI patients, and 35 AD patients, ApoE ε4 carriers exhibited significantly lower glucose metabolism in multiple brain regions, including those characteristic of AD, compared to non-carriers. In particular, the decline in glucose metabolism was especially pronounced in AD patients carrying ApoE ε4 [110]. These findings underscore the potential importance of the ApoE ε4 gene’s influence on glucose metabolism in the pathophysiology of AD. Although the exact mechanisms remain unclear, existing studies suggest that the effects may be linked to impaired insulin receptor signaling [28, 111]. Decreased expression of key glycolytic enzymes such as hexokinase and glucose transporters [28, 112, 113]. PPAR-γ and PGC-1α are two crucial regulators of energy metabolism, and they work synergistically to play a critical role in maintaining the bioenergetic homeostasis of the brain [112]. The PPAR-γ/PGC-1α signaling pathway has been shown to be inhibited in the brains of ApoE4 carriers, and overexpression of PGC-1α improves the defects in glycolysis and mitochondrial respiration induced by ApoE4 [112]. PPAR-γ agonists, such as Thiazolidinediones (TZDs), can improve insulin sensitivity and glucose metabolism, potentially offering benefits for AD patients [114]. As the most abundant glial cells in the brain, astrocytes play a key role in providing metabolic substrates to neurons, including lactate, lipids, amino acids, and ketone bodies [115]. Astrocytes are also the only cell type in the brain that stores glycogen, and they can sense synaptic activity and energy demands. During energy crises, they convert glycogen into lactate and shuttle it to neurons as a metabolic fuel, a process known as the astrocyte-neuron lactate shuttle (ANLS) [116]. By relying on lactate produced by astrocytes, neurons are able to maintain a high rate of OXPHOS while ensuring sufficient glucose enters the pentose phosphate pathway to generate NADPH, which is crucial for maintaining their antioxidant status and normal function [117]. It has been reported that in young adult ApoE4 carriers, the expression of MCT4, a key transporter involved in astrocytic lactate secretion, is reduced, while the expression of MCT2, a lactate transporter in neurons, is upregulated. The abnormal expression of these two key ANLS components suggests that the ANLS may be disrupted by ApoE4 [113]. A study by Lee et al. found that astrocytes from ApoE4 carriers exhibit significant mitochondrial respiratory dysfunction, while their glycolytic activity is markedly increased [118]. Excessive glycolysis in astrocytes could lead to the production of more lactate, which may acidify the extracellular environment and impact the function of other cells, including promoting Aβ aggregation [118, 119]. Additionally, mitochondrial dysfunction in ApoE4 astrocytes may limit metabolite supply and accumulate oxidative stress, triggering AD-related pathological changes [118]. Although fatty acids are not the primary energy source for the brain, in situations of glucose and glycogen depletion, fatty acids and ketone bodies provided by astrocytes become important alternative energy sources. In addition, fatty acids provide essential structural support for neurons and play a significant role in antioxidant protection, injury repair, and signal transduction regulation [120]. However, due to the limited ability of neurons to oxidize fatty acids, this can lead to elevated levels of free fatty acids (FFAs) and lipid peroxidation [121]. As a result, neurons need to transfer oxidized fatty acids to nearby glial cells to avoid the toxic effects of lipid peroxides [102, 122]. In the lipid transport process between neurons and glial cells, fatty acid transport proteins (FATPs) and ApoE play key roles. The absence of FATPs and the presence of ApoE4 both impair lipid transport [103, 122, 123]. A study by Qi et al. on primary embryonic neurons from the hippocampus of humanized ApoE3 and ApoE4 knockin mice revealed that damage to lipid turnover caused by ApoE4 leads to elevated FA levels in neurons, which subsequently suppresses neuronal glucose metabolism and mitochondrial OXPHOS. At the same time, FA output, as well as subsequent uptake and degradation by astrocytes, is impaired, leading to the accumulation of lipid droplets (LDs) in astrocytes. The mitochondrial function and aerobic glycolysis in astrocytes are suppressed, reducing their metabolic and structural support for neurons, which in turn affects neuronal axonal growth and synaptic density [103]. Based on the tight coupling of lipid metabolism between glial cells and neurons, abnormal lipid metabolism in glial cells inevitably leads to changes in the composition and proportion of neuronal membrane lipids, thereby affecting the efficiency of synaptic signaling [124]. A study by Miranda et al. demonstrated that in neurons treated with conditioned medium from ApoE4 astrocytes, several lipids associated with endosomal-lysosomal trafficking accumulated in a dose-dependent manner, leading to significant alterations in neuronal membrane lipid composition. Levels of the primary membrane phospholipids, phosphatidylcholines (PC) and ether phosphatidylcholines (PCe), decreased, while levels of phosphatidic acid (PA), which is associated with neurotransmitter vesicle cycling, increased. This has been suggested as a potential mechanism underlying the hyperactivity of ApoE4 neurons [125]. Neuronal hyperactivity is an early phenotype of human AD and may play a direct role in disease pathogenesis [126]. Additionally, since PCe species are natural scavengers of reactive oxygen species, their reduction may weaken the antioxidant protection of neurons [125].
A study by Victor et al. showed that ApoE4 impairs the lipid uptake ability of microglia, leading to cholesterol accumulation in specific regions of the neuronal cell membrane. This enhances the activity of lipid-gated G-protein-gated inwardly rectifying K+ channels, resulting in hyperpolarization of the neuronal resting membrane potential and reduced neuronal excitability—a phenomenon commonly observed in later stages of AD [127]. Oligodendrocytes, the myelinating cells of the central nervous system, are also affected by ApoE4. Studies have shown that in both human and mouse oligodendrocytes, ApoE4 disrupts cholesterol synthesis and its transport to the plasma membrane, leading to increased intracellular cholesterol accumulation and endoplasmic reticulum stress, which impacts myelination and neuronal synaptic signaling. Treatment with cyclodextrin to promote cholesterol transport has been shown to enhance axonal myelination in ApoE4 mice, improving learning and memory [128]. These findings support the role of ApoE4-mediated lipid metabolic dysregulation in AD pathology and highlight the therapeutic potential of lipid regulation in AD treatment (Fig. 4).
1. ApoE4 competes with insulin for the IR and traps the IR in the endosome, thereby hindering the endocytic recycling of IR [111]. 2. ApoE4 inhibits key molecules in the insulin signaling pathway, including the HK, GLUT, and PGC-1α, the master regulator of mitochondrial biogenesis, leading to impaired insulin signaling, glycolytic function, and mitochondrial respiration [28, 112, 138]. 3. Under specific conditions (such as low ATP and high FAs levels), AMPK may be activated in ApoE4-expressing neurons to adapt to and mitigate fatty acid toxicity [103]. 4. ApoE4-mediated cholesterol accumulation may interfere with ABCA1 localization or recycling at the plasma membrane, impairing its lipid efflux function and disrupting ApoE lipidation. ApoE levels may also be affected, and inadequate cholesterol transport leads to further intracellular lipid accumulation [139,140,141]. Excess fatty acids (FAs) can cause mitochondrial uncoupling and dysfunction, further inhibiting glucose metabolism and mitochondrial OXPHOS in neurons [103]. 5. Lipid degradation in astrocytes is also impaired due to mitochondrial dysfunction, leading to lipid accumulation and reduced ability to receive additional lipid transfer from neurons. Aerobic glycolysis is suppressed, resulting in excessive lactate production [103, 118, 119]. Although lactate shuttling can provide metabolic fuel to neurons, this compromised metabolic state cannot effectively support sustained and stable neuronal metabolism, and excessive lactate accumulation may further damage the surrounding environment [118, 119]. Red lines indicate blocked pathways. Ac-CoA acetyl-CoA, ABCA1 ATP-binding cassette transporter A1, FAs fatty acids, G6P glucose-6-Phosphate, GLUT glucose transporter, HDL high density lipoprotein, HK hexokinase, IR insulin receptor, IRS insulin receptor substrate, MCT monocarboxylate Transporter, PGC-1α peroxisome proliferator-activated receptor gamma coactivator 1 alpha, PPP Pentose Phosphate Pathway, TCA tricarboxylic Acid Cycle, UCP uncoupling Protein.
Summary and perspectives
Despite over a century of research, the etiology of late-onset Alzheimer’s disease (LOAD) remains elusive, and effective treatments continue to be a major medical challenge. ApoE4, the strongest genetic risk factor for AD, plays a central role in Aβ deposition, tau tangles, neuroinflammation, and various downstream pathways. Thus, targeting ApoE4 offers a promising therapeutic strategy for AD. Current approaches focus on: (1) blocking ApoE4-Aβ interactions, (2) targeting ApoE4 receptors, (3) enhancing ApoE4 lipidation, (4) developing ApoE4 antibodies, and (5) gene therapy to correct the ApoE4 genotype or function. While most research remains at the preclinical stage, significant progress has been made, particularly in gene therapy. Several teams are currently conducting clinical trials using ApoE2-expressing constructs (e.g., LX1001) to treat AD patients carrying the ApoE4 allele, with the goal of converting the ApoE genotype from ApoE4 to ApoE2. The Phase I safety study (NCT03634007) has been completed, and the trial is now progressing into a longer-term follow-up study (NCT05400330, for further details see: clinicaltrials.gov).
While substantial progress has been made, several challenges remain that hinder further advancement. First, AD’s complex, heterogeneous etiology makes targeting a single pathway unlikely to yield significant results. Second, the exact mechanisms by which ApoE4 contributes to AD, whether through a toxic gain-of-function or loss of protective function, are not yet fully understood. Nonetheless, ApoE4 remains a promising target for therapy.
Future research should utilize large-scale genomic technologies to deepen our understanding of ApoE4’s role in AD pathology and to identify new therapeutic targets. Enhanced interdisciplinary collaboration, integrating basic research, clinical trials, and translational medicine, will accelerate the development of ApoE4-related therapies. Emerging technologies like artificial intelligence and big data analysis will help clarify the complex relationship between ApoE4 and AD, paving the way for personalized treatments tailored to specific genotypes. Long-term studies are essential to evaluate the efficacy and safety of new therapies for ApoE4 carriers.
Data availability
Data sharing not applicable to this article as no datasets were generated or analyzed during this study.
References
Blumenfeld J, Yip O, Kim MJ, Huang Y. Cell type-specific roles of APOE4 in Alzheimer disease. Nat Rev Neurosci. 2024;25:91–110.
Wadhwani AR, Affaneh A, Van Gulden S, Kessler JA. Neuronal apolipoprotein E4 increases cell death and phosphorylated tau release in alzheimer disease. Ann Neurol. 2019;85:726–39.
Liu CC, Zhao J, Fu Y, Inoue Y, Ren Y, Chen Y, et al. Peripheral apoE4 enhances Alzheimer’s pathology and impairs cognition by compromising cerebrovascular function. Nat Neurosci. 2022;25:1020–33.
Islam T, Gharibyan AL, Golchin SA, Pettersson N, Brännström K, Hedberg I, et al. Apolipoprotein E impairs amyloid-β fibril elongation and maturation. FEBS J. 2020;287:1208–19.
Lanfranco MF, Sepulveda J, Kopetsky G, Rebeck GW. Expression and secretion of apoE isoforms in astrocytes and microglia during inflammation. Glia. 2021;69:1478–93.
Lee S, Devanney NA, Golden LR, Smith CT, Schwartz JL, Walsh AE, et al. APOE modulates microglial immunometabolism in response to age, amyloid pathology, and inflammatory challenge. Cell Rep. 2023;42:112196.
Chakraborty D, Straub JE, Thirumalai D. Differences in the free energies between the excited states of Aβ40 and Aβ42 monomers encode their aggregation propensities. Proc Natl Acad Sci USA. 2020;117:19926–37.
Salvadores N, Moreno-Gonzalez I, Gamez N, Quiroz G, Vegas-Gomez L, Escandón M, et al. Aβ oligomers trigger necroptosis-mediated neurodegeneration via microglia activation in Alzheimer’s disease. Acta Neuropathol Commun. 2022;10:31.
Chai AB, Lam HHJ, Kockx M, Gelissen IC. Apolipoprotein E isoform-dependent effects on the processing of Alzheimer’s amyloid-β. Biochim Biophys Acta Mol Cell Biol Lipids. 2021;1866:158980.
Huang YA, Zhou B, Wernig M, Südhof TC. ApoE2, ApoE3, and ApoE4 differentially stimulate APP transcription and Aβ secretion. Cell. 2017;168:427–41.e21.
Wang ZH, Xia Y, Wu Z, Kang SS, Zhang JC, Liu P, et al. Neuronal ApoE4 stimulates C/EBPβ activation, promoting Alzheimer’s disease pathology in a mouse model. Prog Neurobiol. 2022;209:102212.
Hou X, Adeosun SO, Zhang Q, Barlow B, Brents M, Zheng B, et al. Differential contributions of ApoE4 and female sex to BACE1 activity and expression mediate Aβ deposition and learning and memory in mouse models of Alzheimer’s disease. Front Aging Neurosci. 2015;7:207.
Iwata A, Nagata K, Hatsuta H, Takuma H, Bundo M, Iwamoto K, et al. Altered CpG methylation in sporadic Alzheimer’s disease is associated with APP and MAPT dysregulation. Hum Mol Genet. 2014;23:648–56.
Gao Y, Yu H, Liu Y, Xu Z, He B, Liu H, et al. GSK-3β activation mediates apolipoprotein E4-associated cognitive impairment in type 2 diabetes mellitus: A multicenter, cross-sectional study. J Diab. 2024;16:e13470.
Hou X, Zhang X, Zou H, Guan M, Fu C, Wang W, et al. Differential and substrate-specific inhibition of γ-secretase by the C-terminal region of ApoE2, ApoE3, and ApoE4. Neuron. 2023;111:1898–913.e5.
Lee SI, Jeong W, Lim H, Cho S, Lee H, Jang Y, et al. APOE4-carrying human astrocytes oversupply cholesterol to promote neuronal lipid raft expansion and Aβ generation. Stem Cell Rep. 2021;16:2128–37.
Wang H, Kulas JA, Wang C, Holtzman DM, Ferris HA, Hansen SB. Regulation of beta-amyloid production in neurons by astrocyte-derived cholesterol. Proc Natl Acad Sci USA. 2021;118:e2102191118.
Nixon RA. Amyloid precursor protein and endosomal-lysosomal dysfunction in Alzheimer’s disease: inseparable partners in a multifactorial disease. FASEB J. 2017;31:2729–43.
Fote GM, Steffan JS. APOE4 dysregulates autophagy in cultured cells. Autophagy Rep. 2022;1:29–33.
Krogsaeter EK, McKetney J, Valiente-Banuet L, Marquez A, Willis A, Cakir Z, et al. Lysosomal proteomics reveals mechanisms of neuronal apoE4-associated lysosomal dysfunction. bioRxiv. 2025;2023.10.02.560519.
Wang ZH, Xia Y, Liu P, Liu X, Edgington-Mitchell L, Lei K, et al. ApoE4 activates C/EBPβ/δ-secretase with 27-hydroxycholesterol, driving the pathogenesis of Alzheimer’s disease. Prog Neurobiol. 2021;202:102032.
Ayton S, Faux NG, Bush AI. Alzheimer’s Disease Neuroimaging Initiative. Ferritin levels in the cerebrospinal fluid predict Alzheimer’s disease outcomes and are regulated by APOE. Nat Commun. 2015;6:6760.
Yin J, Nielsen M, Carcione T, Li S, Shi J. Apolipoprotein E regulates mitochondrial function through the PGC-1α-sirtuin 3 pathway. Aging (Albany NY). 2019;11:11148–56.
Wei P, Lin K, Chen X, Fang C, Qiu L, Hu J, et al. Sequential proteomic analysis reveals the key APOE4-induced pathological and molecular features at the presymptomatic stage in Alzheimer’s disease mice. CNS Neurosci Ther. 2025;31:e70306.
Kanekiyo T, Bu G. The low-density lipoprotein receptor-related protein 1 and amyloid-β clearance in Alzheimer’s disease. Front Aging Neurosci. 2014;6:93.
Miners JS, Van Helmond Z, Chalmers K, Wilcock G, Love S, Kehoe PG. Decreased expression and activity of neprilysin in Alzheimer disease are associated with cerebral amyloid angiopathy. J Neuropathol Exp Neurol. 2006;65:1012–21.
Jiang Q, Lee CY, Mandrekar S, Wilkinson B, Cramer P, Zelcer N, et al. ApoE promotes the proteolytic degradation of Abeta. Neuron. 2008;58:681–93.
Keeney JT, Ibrahimi S, Zhao L. Human ApoE isoforms differentially modulate glucose and amyloid metabolic pathways in female brain: evidence of the mechanism of neuroprotection by ApoE2 and implications for Alzheimer’s disease prevention and early intervention. J Alzheimers Dis. 2015;48:411–24.
Zhao L, Teter B, Morihara T, Lim GP, Ambegaokar SS, Ubeda OJ, et al. Insulin-degrading enzyme as a downstream target of insulin receptor signaling cascade: implications for Alzheimer’s disease intervention. J Neurosci. 2004;24:11120–6.
Du J, Chang J, Guo S, Zhang Q, Wang Z. ApoE 4 reduces the expression of Abeta degrading enzyme IDE by activating the NMDA receptor in hippocampal neurons. Neurosci Lett. 2009;464:140–5.
Graykowski D, Kasparian K, Caniglia J, Gritsaeva Y, Cudaback E. Neuroinflammation drives APOE genotype-dependent differential expression of neprilysin. J Neuroimmunol. 2020;346:577315.
Verghese PB, Castellano JM, Garai K, Wang Y, Jiang H, Shah A, et al. ApoE influences amyloid-β (Aβ) clearance despite minimal apoE/Aβ association in physiological conditions. Proc Natl Acad Sci USA. 2013;110:E1807–16.
Joshi SS. Rescuing the Secretion and Lipidation Deficits of APOE4 Using HDL Mimetic Peptides in Primary Glial Cells. University of Minnesota (2023).
Balasubramaniam M, Narasimhappagari J, Liu L, Ganne A, Ayyadevara S, Atluri R, et al. Rescue of ApoE4-related lysosomal autophagic failure in Alzheimer’s disease by targeted small molecules. Commun Biol. 2024;7:60.
Fote GM, Geller NR, Efstathiou NE, Hendricks N, Vavvas DG, Reidling JC, et al. Isoform-dependent lysosomal degradation and internalization of apolipoprotein E requires autophagy proteins. J Cell Sci. 2022;135:jcs258687.
Lee CY, Tse W, Smith JD, Landreth GE. Apolipoprotein E promotes β-amyloid trafficking and degradation by modulating microglial cholesterol levels. J Biol Chem. 2012;287:2032–44.
Chen X, Hui L, Geiger JD. Role of LDL cholesterol and endolysosomes in amyloidogenesis and Alzheimer’s disease. J Neurol Neurophysiol. 2014;5:236.
Fiala M. Omega-3 fatty acid add-on nutritional immunotherapy delays progression to dementia in MCI patients on cholinesterase therapy: Human/Human trials: Nutraceuticals and non-pharmacological interventions. Alzheimer’s & dementia. Dementia. 2020;16:e041293.
Baik SH, Kang S, Lee W, Choi H, Chung S, Kim JI, et al. A Breakdown in metabolic reprogramming causes microglia dysfunction in Alzheimer’s disease. Cell Metab. 2019;30:493–507.e6.
Salloway S, Chalkias S, Barkhof F, Burkett P, Barakos J, Purcell D, et al. Amyloid-related imaging abnormalities in 2 phase 3 studies evaluating aducanumab in patients with early Alzheimer disease. JAMA Neurol. 2022;79:13–21.
Qiao Y, Chi Y, Zhang Q, Ma Y. Safety and efficacy of lecanemab for Alzheimer’s disease: a systematic review and meta-analysis of randomized clinical trials. Front Aging Neurosci. 2023;15:1169499.
Withington CG, Turner RS. Amyloid-related imaging abnormalities with anti-amyloid antibodies for the treatment of dementia due to Alzheimer’s disease. Front Neurol. 2022;13:862369.
Xiong M, Wang C, Gratuze M, Saadi F, Bao X, Bosch ME, et al. Astrocytic APOE4 removal confers cerebrovascular protection despite increased cerebral amyloid angiopathy. Mol Neurodegener. 2023;18:17.
Xiong M, Jiang H, Serrano JR, Gonzales ER, Wang C, Gratuze M, et al. APOE immunotherapy reduces cerebral amyloid angiopathy and amyloid plaques while improving cerebrovascular function. Sci Transl Med. 2021;13:eabd7522.
McCarron MO, Nicoll JA. Apolipoprotein E genotype and cerebral amyloid angiopathy-related hemorrhage. Ann N Y Acad Sci. 2000;903:176–9.
Mazur-Kolecka B, Kowal D, Sukontasup T, Dickson D, Frackowiak J. The effect of oxidative stress on amyloid precursor protein processing in cells engaged in beta-amyloidosis is related to apolipoprotein E genotype. Acta Neuropathol. 2004;108:287–94.
Wang Y, Mandelkow E. Tau in physiology and pathology. Nat Rev Neurosci. 2016;17:5–21.
Lloret A, Fuchsberger T, Giraldo E, Viña J. Molecular mechanisms linking amyloid β toxicity and Tau hyperphosphorylation in Alzheimer׳s disease. Free Radic Biol Med. 2015;83:186–91.
Wang C, Najm R, Xu Q, Jeong DE, Walker D, Balestra ME, et al. Gain of toxic apolipoprotein E4 effects in human iPSC-derived neurons is ameliorated by a small-molecule structure corrector. Nat Med. 2018;24:647–57.
Shi Y, Yamada K, Liddelow SA, Smith ST, Zhao L, Luo W, et al. ApoE4 markedly exacerbates tau-mediated neurodegeneration in a mouse model of tauopathy. Nature. 2017;549:523–7.
Wang C, Xiong M, Gratuze M, Bao X, Shi Y, Andhey PS, et al. Selective removal of astrocytic APOE4 strongly protects against tau-mediated neurodegeneration and decreases synaptic phagocytosis by microglia. Neuron. 2021;109:1657–74.e7.
Koutsodendris N, Blumenfeld J, Agrawal A, Traglia M, Grone B, Zilberter M, et al. Neuronal APOE4 removal protects against tau-mediated gliosis, neurodegeneration and myelin deficits. Nat Aging. 2023;3:275–96.
Zhou M, Huang T, Collins N, Zhang J, Shen H, Dai X, et al. APOE4 induces site-specific tau phosphorylation through calpain-CDK5 signaling pathway in EFAD-Tg mice. Curr Alzheimer Res. 2016;13:1048–55.
Piccarducci R, Giacomelli C, Bertilacchi MS, Benito-Martinez A, Di Giorgi N, Daniele S, et al. Apolipoprotein E ε4 triggers neurotoxicity via cholesterol accumulation, acetylcholine dyshomeostasis, and PKCε mislocalization in cholinergic neuronal cells. Biochim Biophys Acta Mol Basis Dis. 2023;1869:166793.
Salomon-Zimri S, Koren A, Angel A, Ben-Zur T, Offen D, Michaelson DM. The role of MAPK’s signaling in mediating ApoE4-driven pathology in vivo. Curr Alzheimer Res. 2019;16:281–92.
Theendakara V, Bredesen DE, Rao RV. Downregulation of protein phosphatase 2A by apolipoprotein E: implications for Alzheimer’s disease. Mol Cell Neurosci. 2017;83:83–91.
Theendakara V, Peters-Libeu CA, Spilman P, Poksay KS, Bredesen DE, Rao RV. Direct transcriptional effects of apolipoprotein E. J Neurosci. 2016;36:685–700.
Shi Y, Manis M, Long J, Wang K, Sullivan PM, Remolina Serrano J, et al. Microglia drive APOE-dependent neurodegeneration in a tauopathy mouse model. J Exp Med. 2019;216:2546–61.
Ghosh S, Wu MD, Shaftel SS, Kyrkanides S, LaFerla FM, Olschowka JA, et al. Sustained interleukin-1β overexpression exacerbates tau pathology despite reduced amyloid burden in an Alzheimer’s mouse model. J Neurosci. 2013;33:5053–64.
Lazar AN, Hanbouch L, Boussicaut L, Fourmaux B, Daira P, Millan MJ, et al. Lipid dys-homeostasis contributes to APOE4-associated AD pathology. Cells. 2022;11:3616.
García-Cruz VM, Arias C. Palmitic acid induces posttranslational modifications of tau protein in Alzheimer’s disease-related epitopes and increases intraneuronal tau levels. Mol Neurobiol. 2024;61:5129–41.
Kwon B, Lee HK, Querfurth HW. Oleate prevents palmitate-induced mitochondrial dysfunction, insulin resistance and inflammatory signaling in neuronal cells. Biochim Biophys Acta. 2014;1843:1402–13.
Wu TY, Zhao LX, Zhang YH, Fan YG. Activation of vitamin D receptor inhibits Tau phosphorylation is associated with reduction of iron accumulation in APP/PS1 transgenic mice. Neurochem Int. 2022;153:105260.
Thorwald MA, Godoy-Lugo JA, Garcia G, Silva J, Kim M, Christensen A, et al. Iron-associated lipid peroxidation in Alzheimer’s disease is increased in lipid rafts with decreased ferroptosis suppressors, tested by chelation in mice. Alzheimers Dement. 2025;21:e14541.
Pires M, Rego AC. Apoe4 and Alzheimer’s disease pathogenesis-mitochondrial deregulation and targeted therapeutic strategies. Int J Mol Sci. 2023;24:778.
Bartolome F, Carro E, Alquezar C. Oxidative stress in tauopathies: from cause to therapy. Antioxid (Basel). 2022;11:1421.
Kang SW, Kim SJ, Kim MS. Oxidative stress with tau hyperphosphorylation in memory impaired 1,2-diacetylbenzene-treated mice. Toxicol Lett. 2017;279:53–9.
Saha D, Paul S, Gaharwar U, Priya A, Neog A, Singh A, et al. Cdk5-mediated brain unfolded protein response upregulation associated with cognitive impairments in type 2 diabetes and ameliorative action of NAC. ACS Chem Neurosci. 2023;14:2761–74.
Zhang Y, Chen X, Zhao Y, Ponnusamy M, Liu Y. The role of ubiquitin proteasomal system and autophagy-lysosome pathway in Alzheimer’s disease. Rev Neurosci. 2017;28:861–8.
Persson T, Lattanzio F, Calvo-Garrido J, Rimondini R, Rubio-Rodrigo M, Sundström E, et al. Apolipoprotein E4 elicits lysosomal cathepsin D release, decreased thioredoxin-1 levels, and apoptosis. J Alzheimers Dis. 2017;56:601–17.
Huang S. Evaluate the Therapeutic Efficacy of Lysosome Re-acidification by Tetrandrine on Tauopathy Models. Hong Kong Baptist University (2023).
Maniv I, Sarji M, Bdarneh A, Feldman A, Ankawa R, Koren E, et al. Altered ubiquitin signaling induces Alzheimer’s disease-like hallmarks in a three-dimensional human neural cell culture model. Nat Commun. 2023;14:5922.
Paradise V, Sabu M, Bafia J, et al. ApoE isoforms differentially regulate neuronal membrane proteasomes to shift the threshold for pathological aggregation of endogenous Tau. Biorxiv https://doi.org/10.1101/2022.11.29.518293 (2022).
Rauch JN, Luna G, Guzman E, Audouard M, Challis C, Sibih YE, et al. LRP1 is a master regulator of tau uptake and spread. Nature. 2020;580:381–5.
Saroja SR, Gorbachev K, Julia T, Goate AM, Pereira AC. Astrocyte-secreted glypican-4 drives APOE4-dependent tau hyperphosphorylation. Proc Natl Acad Sci USA. 2022;119:e2108870119.
Safieh M, Liraz O, Ovadia M, Michaelson D. The role of impaired receptor trafficking in mediating the pathological effects of APOE4 in Alzheimer’s disease. J Alzheimers Dis. 2024;97:753–75.
Cooper JM, Lathuiliere A, Migliorini M, Arai AL, Wani MM, Dujardin S, et al. Regulation of tau internalization, degradation, and seeding by LRP1 reveals multiple pathways for tau catabolism. J Biol Chem. 2021;296:100715.
Gauthier S, Feldman HH, Schneider LS, Wilcock GK, Frisoni GB, Hardlund JH, et al. Efficacy and safety of tau-aggregation inhibitor therapy in patients with mild or moderate Alzheimer’s disease: a randomised, controlled, double-blind, parallel-arm, phase 3 trial. Lancet. 2016;388:2873–84.
Hasel P, Liddelow SA. Isoform-dependent APOE secretion modulates neuroinflammation. Nat Rev Neurol. 2021;17:265–6.
Singh D. Astrocytic and microglial cells as the modulators of neuroinflammation in Alzheimer’s disease. J Neuroinflammation. 2022;19:206.
Parhizkar S, Holtzman DM. APOE mediated neuroinflammation and neurodegeneration in Alzheimer’s disease. Semin Immunol. 2022;59:101594.
Pascoal TA, Benedet AL, Ashton NJ, Kang MS, Therriault J, Chamoun M, et al. Microglial activation and tau propagate jointly across Braak stages. Nat Med. 2021;27:1592–9.
Ferrari-Souza JP, Lussier FZ, Leffa DT, Therriault J, Tissot C, Bellaver B, et al. APOEε4 associates with microglial activation independently of Aβ plaques and tau tangles. Sci Adv. 2023;9:eade1474.
Zhu Y, Nwabuisi-Heath E, Dumanis SB, Tai LM, Yu C, Rebeck GW, et al. APOE genotype alters glial activation and loss of synaptic markers in mice. Glia. 2012;60:559–69.
Bouchareychas L, Raffai RL. Apolipoprotein E and Atherosclerosis: from Lipoprotein Metabolism to MicroRNA control of inflammation. J Cardiovasc Dev Dis. 2018;5:30.
Chen X, Firulyova M, Manis M, Herz J, Smirnov I, Aladyeva E, et al. Microglia-mediated T cell infiltration drives neurodegeneration in tauopathy. Nature. 2023;615:668–77.
Park J, Min JS, Kim B, Chae UB, Yun JW, Choi MS, et al. Mitochondrial ROS govern the LPS-induced pro-inflammatory response in microglia cells by regulating MAPK and NF-κB pathways. Neurosci Lett. 2015;584:191–6.
Jiang S, Zhao Y, Zhang T, Lan J, Yang J, Yuan L, et al. Galantamine inhibits β-amyloid-induced cytostatic autophagy in PC12 cells through decreasing ROS production. Cell Prolif. 2018;51:e12427.
Orr AL, Kim C, Jimenez-Morales D, Newton BW, Johnson JR, Krogan NJ, et al. Neuronal apolipoprotein E4 expression results in proteome-wide alterations and compromises bioenergetic capacity by disrupting mitochondrial function. J Alzheimers Dis. 2019;68:991–1011.
Liu XT, Chen X, Zhao N, Geng F, Zhu MM, Ren QG. Synergism of ApoE4 and systemic infectious burden is mediated by the APOE-NLRP3 axis in Alzheimer’s disease. Psychiatry Clin Neurosci. 2024;78:517–26.
Simpson DSA, Oliver PL. ROS generation in microglia: understanding oxidative stress and inflammation in neurodegenerative disease. Antioxid (Basel). 2020;9:743.
Agrawal I, Jha S. Mitochondrial dysfunction and Alzheimer’s disease: role of microglia. Front Aging Neurosci. 2020;12:252.
Choi SH, Aid S, Kim HW, Jackson SH, Bosetti F. Inhibition of NADPH oxidase promotes alternative and anti-inflammatory microglial activation during neuroinflammation. J Neurochem. 2012;120:292–301.
Geng L, Fan LM, Liu F, Smith C, Li J-. Nox2 dependent redox-regulation of microglial response to amyloid-β stimulation and microgliosis in aging. Sci Rep. 2020;10:1582.
Kloske CM. Uncovering the Role of ApoE4 on Alzheimer’s Disease-related Neuroinflammation [dissertation]. University of Kentucky (2021).
Li C, Zhao B, Lin C, Gong Z, An X. TREM2 inhibits inflammatory responses in mouse microglia by suppressing the PI3K/NF-κB signaling. Cell Biol Int. 2019;43:360–72.
Li X, Montine KS, Keene CD, Montine TJ. Different mechanisms of apolipoprotein E isoform-dependent modulation of prostaglandin E2 production and triggering receptor expressed on myeloid cells 2 (TREM2) expression after innate immune activation of microglia. FASEB J. 2015;29:1754–62.
Nugent AA, Lin K, van Lengerich B, Lianoglou S, Przybyla L, Davis SS, et al. TREM2 regulates microglial cholesterol metabolism upon chronic phagocytic challenge. Neuron. 2020;105:837–54.e9.
Tcw J, Qian L, Pipalia NH, Chao MJ, Liang SA, Shi Y, et al. Cholesterol and matrisome pathways dysregulated in astrocytes and microglia. Cell. 2022;185:2213–33.e25.
Kumari S, Dhapola R, Sharma P, Singh SK, Reddy DH Implicative role of Cytokines in Neuroinflammation mediated AD and associated signaling pathways: current Progress in molecular signaling and therapeutics. Ageing Res Rev. 2023:102098.
Liddelow SA, Guttenplan KA, Clarke LE, Bennett FC, Bohlen CJ, Schirmer L, et al. Neurotoxic reactive astrocytes are induced by activated microglia. Nature. 2017;541:481–7.
Sienski G, Narayan P, Bonner JM, Kory N, Boland S, Arczewska AA, et al. APOE4 disrupts intracellular lipid homeostasis in human iPSC-derived glia. Sci Transl Med. 2021;13:eaaz4564.
Qi G, Mi Y, Shi X, Gu H, Brinton RD, Yin F. ApoE4 impairs neuron-astrocyte coupling of fatty acid metabolism. Cell Rep. 2021;34:108572.
Kwon YH, Kim J, Kim CS, Tu TH, Kim MS, Suk K, et al. Hypothalamic lipid-laden astrocytes induce microglia migration and activation. FEBS Lett. 2017;591:1742–51.
Villarejo-Galende A, González-Sánchez M, Blanco-Palmero VA, Llamas-Velasco S, Benito-León J. Non-Steroidal Anti-inflammatory Drugs as Candidates for the Prevention Or Treatment of Alzheimer’s disease: do they still have a role?. Curr Alzheimer Res. 2020;17:1013–22.
Zou Z, Wu F, Chen L, Yao H, Wang Z, Chen Y, et al. The J bs-5YP peptide can alleviate dementia in senile mice by restoring the transcription of Slc40a1 to secrete the excessive iron from brain. J Adv Res. 2025;69:51–9.
Zou Z, Shen Q, Pang Y, Li X, Chen Y, Wang X, et al. The synthesized transporter K16APoE enabled the therapeutic HAYED peptide to cross the blood-brain barrier and remove excess iron and radicals in the brain, thus easing Alzheimer’s disease. Drug Deliv Transl Res. 2019;9:394–403.
Steiner P. Brain fuel utilization in the developing brain. Ann Nutr Metab. 2019;75:8–18.
Paranjpe MD, Chen X, Liu M, Paranjpe I, Leal JP, Wang R, et al. The effect of ApoE ε4 on longitudinal brain region-specific glucose metabolism in patients with mild cognitive impairment: a FDG-PET study. Neuroimage Clin. 2019;22:101795.
Knopman DS, Jack CR Jr, Wiste HJ, Lundt ES, Weigand SD, Vemuri P, et al. 18F-fluorodeoxyglucose positron emission tomography, aging, and apolipoprotein E genotype in cognitively normal persons. Neurobiol Aging. 2014;35:2096–106.
Zhao N, Liu CC, Van Ingelgom AJ, Martens YA, Linares C, Knight JA, et al. Apolipoprotein E4 impairs neuronal insulin signaling by trapping insulin receptor in the endosomes. Neuron. 2017;96:115–29.e5.
Wu L, Zhang X, Zhao L. Human ApoE isoforms differentially modulate brain glucose and ketone body metabolism: implications for Alzheimer’s disease risk reduction and early intervention. J Neurosci. 2018;38:6665–81.
Perkins M, Wolf AB, Chavira B, Shonebarger D, Meckel JP, Leung L, et al. Altered energy metabolism pathways in the posterior cingulate in young adult apolipoprotein E ɛ4 carriers. J Alzheimers Dis. 2016;53:95–106.
Huang J, Huang N, Cui D, Shi J, Qiu Y. Clinical antidiabetic medication used in Alzheimer’s disease: From basic discovery to therapeutics development. Front Aging Neurosci. 2023;15:1122300.
Williams HC, Farmer BC, Piron MA, Walsh AE, Bruntz RC, Gentry MS, et al. APOE alters glucose flux through central carbon pathways in astrocytes. Neurobiol Dis. 2020;136:104742.
Yassine HN, Self W, Kerman BE, Santoni G, Navalpur Shanmugam N, Abdullah L, et al. Nutritional metabolism and cerebral bioenergetics in Alzheimer’s disease and related dementias. Alzheimers Dement. 2023;19:1041–66.
Xue X, Liu B, Hu J, Bian X, Lou S. The potential mechanisms of lactate in mediating exercise-enhanced cognitive function: a dual role as an energy supply substrate and a signaling molecule. Nutr Metab (Lond). 2022;19:52.
Lee H, Cho S, Kim MJ, Park YJ, Cho E, Jo YS, et al. ApoE4-dependent lysosomal cholesterol accumulation impairs mitochondrial homeostasis and oxidative phosphorylation in human astrocytes. Cell Rep. 2023;42:113183.
Decker Y, Németh E, Schomburg R, Chemla A, Fülöp L, Menger MD, et al. Decreased pH in the aging brain and Alzheimer’s disease. Neurobiol Aging. 2021;101:40–9.
Yin F. Lipid metabolism and Alzheimer’s disease: clinical evidence, mechanistic link and therapeutic promise. FEBS J. 2023;290:1420–53.
Li Y, Munoz-Mayorga D, Nie Y, Kang N, Tao Y, Lagerwall J, et al. Microglial lipid droplet accumulation in tauopathy brain is regulated by neuronal AMPK. Cell Metab. 2024;36:1351–70.e8.
Ioannou MS, Jackson J, Sheu SH, Chang CL, Weigel AV, Liu H, et al. Neuron-astrocyte metabolic coupling protects against activity-induced fatty acid toxicity. Cell. 2019;177:1522–35.e14.
Liu L, MacKenzie KR, Putluri N, Maletić-Savatić M, Bellen HJ. The glia-neuron lactate shuttle and elevated ROS promote lipid synthesis in neurons and lipid droplet accumulation in glia via APOE/D. Cell Metab. 2017;26:719–37.e6.
Barber CN, Raben DM. Lipid metabolism crosstalk in the brain: glia and neurons. Front Cell Neurosci. 2019;13:212.
Miranda AM, Ashok A, Chan RB, Zhou B, Xu Y, McIntire LB, et al. Effects of APOE4 allelic dosage on lipidomic signatures in the entorhinal cortex of aged mice. Transl Psychiatry. 2022;12:129.
Nuriel T, Angulo SL, Khan U, Ashok A, Chen Q, Figueroa HY, et al. Neuronal hyperactivity due to loss of inhibitory tone in APOE4 mice lacking Alzheimer’s disease-like pathology. Nat Commun. 2017;8:1464.
Victor MB, Leary N, Luna X, Meharena HS, Scannail AN, Bozzelli PL, et al. Lipid accumulation induced by APOE4 impairs microglial surveillance of neuronal-network activity. Cell Stem Cell. 2022;29:1197–212.e8.
Blanchard JW, Akay LA, Davila-Velderrain J, von Maydell D, Mathys H, Davidson SM, et al. APOE4 impairs myelination via cholesterol dysregulation in oligodendrocytes. Nature. 2022;611:769–79.
Wang C, Lu J, Sha X, Qiu Y, Chen H, Yu Z. TRPV1 regulates ApoE4-disrupted intracellular lipid homeostasis and decreases synaptic phagocytosis by microglia. Exp Mol Med. 2023;55:347–63.
Lim CS, Han JS. The antioxidant xanthorrhizol prevents amyloid-β-induced oxidative modification and inactivation of neprilysin. Biosci Rep. 2018;38:BSR20171611.
de Dios C, Bartolessis I, Roca-Agujetas V, Barbero-Camps E, Mari M, Morales A, et al. Oxidative inactivation of amyloid beta-degrading proteases by cholesterol-enhanced mitochondrial stress. Redox Biol. 2019;26:101283.
Domingues C, da Cruz E Silva OAB, Henriques AG. Impact of cytokines and chemokines on Alzheimer’s disease neuropathological Hallmarks. Curr Alzheimer Res. 2017;14:870–82.
Cheng F, Fransson LÅ, Mani K. Proinflammatory cytokines induce accumulation of glypican-1-derived heparan sulfate and the C-terminal fragment of β-cleaved APP in autophagosomes of dividing neuronal cells. Glycobiology. 2020;30:539–49.
Ong QR, Chan ES, Lim ML, Cole GM, Wong BS. Reduced phosphorylation of brain insulin receptor substrate and Akt proteins in apolipoprotein-E4 targeted replacement mice. Sci Rep. 2014;4:3754.
Joshi G, Chi Y, Huang Z, Wang Y. Aβ-induced Golgi fragmentation in Alzheimer’s disease enhances Aβ production. Proc Natl Acad Sci USA. 2014;111:E1230–9.
Dong Y, Yu H, Li X, Bian K, Zheng Y, Dai M, et al. Hyperphosphorylated tau mediates neuronal death by inducing necroptosis and inflammation in Alzheimer’s disease. J Neuroinflammation. 2022;19:205.
Hollinger KR, Zhu X, Khoury ES, Thomas AG, Liaw K, Tallon C, et al. Glutamine antagonist JHU-083 normalizes aberrant hippocampal glutaminase activity and improves cognition in APOE4 Mice. J Alzheimers Dis. 2020;77:437–47.
Zhang X, Wu L, Swerdlow RH, Zhao L. Opposing effects of ApoE2 and ApoE4 on glycolytic metabolism in neuronal aging supports a warburg neuroprotective cascade against Alzheimer’s disease. Cells. 2023;12:410.
Boehm-Cagan A, Bar R, Liraz O, Bielicki JK, Johansson JO, Michaelson DM. ABCA1 agonist reverses the ApoE4-driven cognitive and brain pathologies. J Alzheimers Dis. 2016;54:1219–33.
Wang S, Li B, Li J, Cai Z, Hugo C, Sun Y, et al. Cellular senescence induced by cholesterol accumulation is mediated by lysosomal ABCA1 in APOE4 and AD. Mol Neurodegener. 2025;20:15.
Koldamova R, Staufenbiel M, Lefterov I. Lack of ABCA1 considerably decreases brain ApoE level and increases amyloid deposition in APP23 mice. J Biol Chem. 2005;280:43224–35. Dec 30.
Budd Haeberlein S, Aisen PS, Barkhof F, Chalkias S, Chen T, Cohen S, et al. Two randomized phase 3 studies of aducanumab in Early Alzheimer’s disease. J Prev Alzheimers Dis. 2022;9:197–210.
Toda Y, Iwatsubo T, Nakamura Y, Matsuda N, Miyata M, Jin M, et al. Japanese subgroup analyses from EMERGE and ENGAGE, phase 3 clinical trials of aducanumab in patients with early Alzheimer’s Disease. J Prev Alzheimers Dis. 2024;11:1260–9.
van Dyck CH, Swanson CJ, Aisen P, Bateman RJ, Chen C, Gee M, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388:9–21.
Sperling RA, Donohue MC, Raman R, Rafii MS, Johnson K, Masters CL, et al. Trial of solanezumab in preclinical Alzheimer’s disease. N Engl J Med. 2023;389:1096–107.
Ostrowitzki S, Bittner T, Sink KM, Mackey H, Rabe C, Honig LS, et al. Evaluating the safety and efficacy of crenezumab vs placebo in adults with early Alzheimer disease: two phase 3 randomized placebo-controlled trials. JAMA Neurol. 2022;79:1113–21.
Bateman RJ, Li Y, McDade EM, Llibre-Guerra JJ, Clifford DB, Atri A, et al. Safety and efficacy of long-term gantenerumab treatment in dominantly inherited Alzheimer’s disease: an open-label extension of the phase 2/3 multicentre, randomised, double-blind, placebo-controlled platform DIAN-TU trial. Lancet Neurol. 2025;24:316–30.
Pasquier F, Sadowsky C, Holstein A, Leterme GleP, Peng Y, Jackson N, et al. Two phase 2 multiple ascending-dose studies of vanutide cridificar (ACC-001) and QS-21 adjuvant in mild-to-moderate Alzheimer’s disease. J Alzheimers Dis. 2016;51:1131–43.
Hull M, Sadowsky C, Arai H, Le Prince Leterme G, Holstein A, Booth K, et al. Long-term extensions of randomized vaccination trials of ACC-001 and QS-21 in mild to moderate Alzheimer’s disease. Curr Alzheimer Res. 2017;14:696–708.
Baddeley TC, McCaffrey J, Storey JM, Cheung JK, Melis V, Horsley D, et al. Complex disposition of methylthioninium redox forms determines efficacy in tau aggregation inhibitor therapy for Alzheimer’s disease. J Pharm Exp Ther. 2015;352:110–8.
Wilcock GK, Gauthier S, Frisoni GB, Jia J, Hardlund JH, Moebius HJ, et al. Potential of low dose leuco-methylthioninium bis(hydromethanesulphonate) (LMTM) monotherapy for treatment of mild Alzheimer’s disease: cohort analysis as modified primary outcome in a phase III clinical trial. J Alzheimers Dis. 2018;61:435–57.
Wischik CM, Bentham P, Gauthier S, Miller S, Kook K, Schelter BO. Oral tau aggregation inhibitor for alzheimer’s disease: design, progress and basis for selection of the 16 mg/day dose in a phase 3, randomized, placebo-controlled trial of hydromethylthionine mesylate. J Prev Alzheimers Dis. 2022;9:780–90.
Bittner T, Tonietto M, Klein G, Belusov A, Illiano V, Voyle N, et al. Biomarker treatment effects in two phase 3 trials of gantenerumab. Alzheimers Dement. 2025;21:e14414.
Salloway S, Farlow M, McDade E, Clifford DB, Wang G, Llibre-Guerra JJ, et al. A trial of gantenerumab or solanezumab in dominantly inherited Alzheimer’s disease. Nat Med. 2021;27:1187–96.
Tsai RM, Miller Z, Koestler M, Rojas JC, Ljubenkov PA, Rosen HJ, et al. Reactions to multiple ascending doses of the microtubule stabilizer TPI-287 in patients with alzheimer disease, progressive supranuclear palsy, and corticobasal syndrome: a randomized clinical trial. JAMA Neurol. 2020;77:215–24.
Florian H, Wang D, Arnold SE, Boada M, Guo Q, Jin Z, et al. Tilavonemab in early Alzheimer’s disease: results from a phase 2, randomized, double-blind study. Brain. 2023;146:2275–84.
McQuade A, Kang YJ, Hasselmann J, Jairaman A, Sotelo A, Coburn M, et al. Gene expression and functional deficits underlie TREM2-knockout microglia responses in human models of Alzheimer’s disease. Nat Commun. 2020;11:5370.
Griciuc A, Federico AN, Natasan J, Forte AM, McGinty D, Nguyen H, et al. Gene therapy for Alzheimer’s disease targeting CD33 reduces amyloid beta accumulation and neuroinflammation. Hum Mol Genet. 2020;29:2920–35.
He Y, Ruganzu JB, Zheng Q, Wu X, Jin H, Peng X, et al. Silencing of LRP1 exacerbates inflammatory response Via TLR4/NF-κB/MAPKs signaling pathways in APP/PS1 transgenic mice. Mol Neurobiol. 2020;57:3727–43.
Imraish A, Abu-Thiab T, Hammad H. P2X and P2Y receptor antagonists reduce inflammation in ATP-induced microglia. Pharm Pr (Granada). 2023;21:2788.
Leitner GR, Wenzel TJ, Marshall N, Gates EJ, Klegeris A. Targeting toll-like receptor 4 to modulate neuroinflammation in central nervous system disorders. Expert Opin Ther Targets. 2019;23:865–82.
Zhou J, Wang Y, Huang G, Yang M, Zhu Y, Jin C, et al. LilrB3 is a putative cell surface receptor of APOE4. Cell Res. 2023;33:116–30.
Shen C, Ma Y, Zeng Z, Yin Q, Hong Y, Hou X, et al. RAGE-specific inhibitor FPS-ZM1 attenuates AGEs-induced neuroinflammation and oxidative stress in rat primary microglia. Neurochem Res. 2017;42:2902–11.
Dobri AM, Dudău M, Enciu AM, Hinescu ME. CD36 in Alzheimer’s disease: an overview of molecular mechanisms and therapeutic targeting. Neuroscience. 2021;453:301–11.
Eshraghi M, Adlimoghaddam A, Mahmoodzadeh A, Sharifzad F, Yasavoli-Sharahi H, Lorzadeh S, et al. Alzheimer’s disease pathogenesis: role of autophagy and mitophagy focusing in microglia. Int J Mol Sci. 2021;22:3330.
Xiang X, Werner G, Bohrmann B, Liesz A, Mazaheri F, Capell A, et al. TREM2 deficiency reduces the efficacy of immunotherapeutic amyloid clearance. EMBO Mol Med. 2016;8:992–1004.
Allendorf DH, Puigdellívol M, Brown GC. Activated microglia desialylate their surface, stimulating complement receptor 3-mediated phagocytosis of neurons. Glia. 2020;68:989–98.
Funding
This research was supported by Zhejiang Medical and Health Project: 2019KY246; Liuzhou Science and Technology Project: 2024YB0101A018; Guangxi Zhuang Natural Science Foundation: 2024GXNSFAA010022; Guangxi Zhuang Natural Science Foundation: 2025GXNSFAA069923; National Natural Science Foundation of China: 82060268.
Author information
Authors and Affiliations
Contributions
Conceptualization, YC, JC, and ZZ; Writing—original draft preparation, YC, JC and HJ; Writing—review and editing, YC, ZZ, JL, and M-AG; Prepared figures, YC, JC and HJ; Supervision, YC, JL, and ZZ. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Y., Jin, H., Chen, J. et al. The multifaceted roles of apolipoprotein E4 in Alzheimer’s disease pathology and potential therapeutic strategies. Cell Death Discov. 11, 312 (2025). https://doi.org/10.1038/s41420-025-02600-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41420-025-02600-y