Abstract
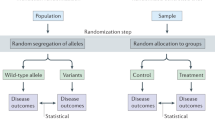
With the rapidly increasing availability of large genetic data sets in recent years, Mendelian Randomization (MR) has quickly gained popularity as a novel secondary analysis method. Leveraging genetic variants as instrumental variables, MR can be used to estimate the causal effects of one phenotype on another even when experimental research is not feasible, and therefore has the potential to be highly informative. It is dependent on strong assumptions however, often producing biased results if these are not met. It is therefore imperative that these assumptions are well-understood by researchers aiming to use MR, in order to evaluate their validity in the context of their analyses and data. The aim of this perspective is therefore to further elucidate these assumptions and the role they play in MR, as well as how different kinds of data can be used to further support them.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Mills MC, Rahal C. A scientometric review of genome-wide association studies. Commun Biol. 2019;2:9.
Pearl J. Causal inference in statistics: an overview. Stat Surv. 2009;3:96–146.
Davey Smith G, Hemani G. Mendelian randomization: genetic anchors for causal inference in epidemiological studies. Hum Mol Genet. 2014;23:R89–98.
von Hinke Kessler Scholder S, Smith GD, Lawlor DA, Propper C, Windmeijer F. Mendelian randomization: the use of genes in instrumental variable analyses. Health Econ. 2011;20:893–6.
Sleiman PMA, Grant SFA. Mendelian randomization in the era of genomewide association studies. Clin Chem. 2010;56:723–8.
Haycock PC, Burgess S, Wade KH, Bowden J, Relton C, Smith GD. Statistical commentary best (but oft-forgotten) practices: the design, analysis, and interpretation of Mendelian randomization studies. Am J Clin Nutr. 2016;103:965–78.
Lousdal ML. An introduction to instrumental variable assumptions, validation and estimation. Emerg Themes Epidemiol. 2018;15:1.
Burgess S, Davey Smith G, Davies NM, Dudbridge F, Gill D, Glymour MM, et al. Guidelines for performing Mendelian randomization investigations. Wellcome Open Res. 2020;4:186.
Skrivankova VW, Richmond RC, Woolf BAR, Davies NM, Swanson SA, VanderWeele TJ, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): explanation and elaboration. BMJ 2021;375:n2233.
Burgess S, Butterworth AS, Thompson JR. Beyond Mendelian randomization: How to interpret evidence of shared genetic predictors. J Clin Epidemiol. 2016;69:208–16.
von Hinke S, Davey Smith G, Lawlor DA, Propper C, Windmeijer F. Genetic markers as instrumental variables. J Health Econ. 2016;45:131–48.
Teumer A. Common methods for performing Mendelian randomization. Front cardiovascular Med. 2018;5:51.
Hemani G, Bowden J, Davey Smith G. Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum Mol Genet. 2018;27:R195–208.
Zhu Z, Zheng Z, Zhang F, Wu Y, Trzaskowski M, Maier R, et al. Causal associations between risk factors and common diseases inferred from GWAS summary data. Nat Commun. 2018;9:224.
Dai JY, Peters U, Wang X, Kocarnik J, Chang-Claude J, Slattery ML, et al. Diagnostics for pleiotropy in Mendelian randomization studies: global and individual tests for direct effects. Am J Epidemiol. 2018;187:2672–80.
Verbanck M, Chen C-Y, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50:693–8.
Bowden J, Davey, Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40:304–14.
Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. 2017;46:1985–98.
Burgess S, Zuber V, Gkatzionis A, Foley CN. Modal-based estimation via heterogeneity-penalized weighting: model averaging for consistent and efficient estimation in Mendelian randomization when a plurality of candidate instruments are valid. Int J Epidemiol. 2018;47:1242–54.
Qi G, Chatterjee N. Mendelian randomization analysis using mixture models for robust and efficient estimation of causal effects. Nat Commun. 2019;10:1941.
Burgess S, Thompson SG. Interpreting findings from Mendelian randomization using the MR-Egger method. Eur J Epidemiol. 2017;32:377–89.
Bucur IG, Claassen T, Heskes T. Inferring the direction of a causal link and estimating its effect via a Bayesian Mendelian randomization approach. Stat Methods Med Res. 2020;29:1081–111.
Darrous L, Mounier N, Kutalik Z. Simultaneous estimation of bi-directional causal effects and heritable confounding from GWAS summary statistics. Genet Genom Med. 2020. http://medrxiv.org/lookup/doi/10.1101/2020.01.27.20018929.
Morrison J, Knoblauch N, Marcus JH, Stephens M, He X. Mendelian randomization accounting for correlated and uncorrelated pleiotropic effects using genome-wide summary statistics. Nat Genet. 2020;52:740–7.
Cho Y, Haycock PC, Sanderson E, Gaunt TR, Zheng J, Morris AP, et al. Exploiting horizontal pleiotropy to search for causal pathways within a Mendelian randomization framework. Nat Commun. 2020;11:1010.
Rees JMB, Wood AM, Burgess S. Extending the MR-Egger method for multivariable Mendelian randomization to correct for both measured and unmeasured pleiotropy. Stat Med. 2017;36:4705–18.
Gkatzionis A, Burgess S. Contextualizing selection bias in Mendelian randomization: how bad is it likely to be? Int J Epidemiol. 2019;48:691–701.
Swanson SA, Tiemeier H, Ikram MA, Hernán MA. Nature as a trialist?: deconstructing the analogy between Mendelian randomization and randomized trials. Epidemiology. 2017;28:653–9.
Lipsitch M, Tchetgen Tchetgen E, Cohen T. Negative controls. Epidemiology. 2010;21:383–8.
Chen L, Davey Smith G, Harbord RM, Lewis SJ. Alcohol intake and blood pressure: a systematic review implementing a Mendelian randomization approach. PLoS Med. 2008;5:e52.
Van Kippersluis H, Rietveld CA. Pleiotropy-robust Mendelian randomization. Int J Epidemiol. 2018;47:1279–88.
Richardson TG, Sanderson E, Elsworth B, Tilling K, Smith GD. Use of genetic variation to separate the effects of early and later life adiposity on disease risk: mendelian randomisation study. BMJ 2020;369:m1203.
Streeter AJ, Lin NX, Crathorne L, Haasova M, Hyde C, Melzer D, et al. Adjusting for unmeasured confounding in nonrandomized longitudinal studies: a methodological review. J Clin Epidemiol. 2017;87:23–34.
Sanderson E, Richardson T, Hemani G, Smith GD. The use of negative control outcomes in Mendelian Randomisation to detect potential population stratification or selection bias. bioRxiv. 2020. https://doi.org/10.1101/2020.06.01.128264.
Hughes RA, Davies NM, Davey Smith G, Tilling K. Selection bias when estimating average treatment effects using one-sample instrumental variable analysis. Epidemiology. 2019;30:350–7.
Smit RAJ, Trompet S, Dekkers OM, Jukema JW, Le, Cessie S. Survival bias in Mendelian randomization studies: a threat to causal inference. Epidemiology. 2019;30:813–6.
Swanson SA. A practical guide to selection bias in instrumental variable analyses. Epidemiology. 2019;30:345–9.
Pierce BL, Vanderweele TJ. The effect of non-differential measurement error on bias, precision and power in Mendelian randomization studies. Int J Epidemiol. 2012;41:1383–93.
Hemani G, Tilling K, Davey, Smith G. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 2017;13:1–22.
Burgess S, Labrecque JA. Mendelian randomization with a binary exposure variable: interpretation and presentation of causal estimates. Eur J Epidemiol. 2018;33:947–52.
Burgess S, Butterworth A, Malarstig A, Thompson SG. Use of Mendelian randomisation to assess potential benefit of clinical intervention. BMJ. 2012;345:1–6.
Swanson SA, Hernan MA. The challenging interpretation of instrumental variable estimates under monotonicity. Int J Epidemiol. 2018;47:1289–97.
Acknowledgements
This work was funded by The Netherlands Organization for Scientific Research (NWO VICI 453-14-005 (DP), 645-000-003 (DP), CHiLL 617-001-451 (IGB)) and by F. Hoffman-La Roche AG (CdL).
Author information
Authors and Affiliations
Contributions
CdL wrote and revised the paper. The other authors contributed to revision and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
de Leeuw, C., Savage, J., Bucur, I.G. et al. Understanding the assumptions underlying Mendelian randomization. Eur J Hum Genet 30, 653–660 (2022). https://doi.org/10.1038/s41431-022-01038-5
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41431-022-01038-5
This article is cited by
-
Identification of loci associated with women’s reproductive traits and exploration of a shared genetic basis with obesity
Human Genomics (2025)
-
Unveiling the genetic association between rheumatoid arthritis and four common hand pathologies
European Journal of Medical Research (2025)
-
A causal effects of neutrophil extracellular traps and its biomarkers on acute respiratory distress syndrome: a two-sample Mendelian randomization study
Scientific Reports (2025)
-
Cardiovascular diseases and depression: A meta-analysis and Mendelian randomization analysis
Molecular Psychiatry (2025)
-
Distinguishing the causative, correlative and bidirectional roles of the gut microbiota in mental health
Nature Mental Health (2025)