Abstract
To present our experience using a multiomic approach, which integrates genetic and biochemical testing as a first-line diagnostic tool for patients with inherited metabolic disorders (IMDs). A cohort of 3720 patients from 62 countries was tested using a panel including 206 genes with single nucleotide and copy number variant (SNV/CNV) detection, followed by semi-automatic variant filtering and reflex biochemical testing (25 assays). In 1389 patients (37%), a genetic diagnosis was achieved. Within this cohort, the highest diagnostic yield was obtained for patients from Asia (57.5%, mainly from Pakistan). Overall, 701 pathogenic/likely pathogenic unique SNVs and 40 CNVs were identified. In 620 patients, the result of the biochemical tests guided variant classification and reporting. Top five diagnosed diseases were: Gaucher disease, Niemann-Pick disease type A/B, phenylketonuria, mucopolysaccharidosis type I, and Wilson disease. We show that integrated genetic and biochemical testing facilitated the decision on clinical relevance of the variants and led to a high diagnostic yield (37%), which is comparable to exome/genome sequencing. More importantly, up to 43% of these patients (n = 610) could benefit from medical treatments (e.g., enzyme replacement therapy). This multiomic approach constitutes a unique and highly effective tool for the genetic diagnosis of IMDs.
Similar content being viewed by others
Introduction
Inherited metabolic disorders (IMD) constitute a vast, complex, and important group of rare genetic diseases. The term “inborn error of metabolism” was first referenced as early as 1902 by Sir Archibald Garrod regarding four diseases: alkaptonuria, pentosuria, cystinuria, and albinism [1]. Approximately 60 years after Garrod’s premonitory dissertations, IMDs were rediscovered and slowly redefined as molecular diseases [2].
IMDs can be described as genetic disorders that cause disruption of a metabolic pathway presenting throughout a patient’s life span, from the prenatal period through adulthood [3]. IMDs can lead to disease either by accumulation of a toxic substrate proximal to the metabolic block, a deficiency of the product distal to the block, or a diversion of the substrate to an alternative pathway. Currently, over 1400 IMDs are recognized [4]. Although each disorder is individually rare, they represent a common group of diseases with a prevalence of 1 in 784–2555 [5,6,7].
Importantly, some IMDs are treatable [8, 9], and thus, many are included in newborn screening programs in various countries, which is pivotal for preventive health care [10]. The past decade has seen revolutionary changes in the discovery and diagnosis of IMDs, as well as in the development of new therapies [11]. The number of recognized IMDs and insights into their varying phenotypes are expanding rapidly using genomic, metabolomic, and deep phenotyping technologies, such as high-resolution and functional neuroimaging [12]. Early disease recognition and treatment are, in many cases, critical for preventing neurological impairment and/or death of the patient.
In order to diagnose IMDs comprehensively, we have implemented a next generation sequencing (NGS) panel with over 200 genes that integrates genetic and biochemical testing performed in the same laboratory. This approach allows the efficient diagnosis of more than 180 metabolic diseases. To our knowledge, there is no such integrated approach currently being offered in clinical practice.
Within this paper, we present our experience of the first 3720 patients in our clinical diagnostic setup. We recommend the use of this kind of multiomic approach as a first-line diagnostic tool for patients suspected of having IMDs.
Materials and methods
Patients
The current study has been conducted within a diagnostic setting. Additionally, in a follow-up step, de-identified data and samples were utilized. Accordingly, this did not require Institutional Review Board approval in our jurisdiction due to the nature in which the study was carried out. Written informed consent for genetic testing related to the disease(s) of the patient was obtained. Additionally, the consent form declaration included information regarding storage of the data and further data processing for research purposes. Written informed consent was given by patients, legal guardians, or referring physicians. The informed consent form is available in English and several other languages at https://www.centogene.com/downloads.html.
All consecutive index patients for whom this panel was performed and reported within the period of July 2019 until July 2021 were included in this study (n = 3720). Tested relatives were excluded from this analysis. Data regarding country of origin, family history, consanguinity, clinical phenotype, as well as panel testing results were extracted from our rare disease-centric Bio/Databank.
Lab procedures
DNA was extracted from EDTA blood or from dried blood spots (DBS) on filter cards (CentoCard®) with QIASymphony using a magnetic bead-based method (Qiagen), with an acceptance criterion of minimum 3 ng/µl. Genomic DNA was enzymatically fragmented, and regions of interest were enriched using DNA capture probes (Twist Biosciences, custom design). The final indexed libraries were sequenced on an Illumina platform (MiSeq), with a sequencing quality parameter of 99.5% coverage of the targeted regions with a minimum read depth of 20x. The panel design included 206 genes (listed in the Supplementary Information). We included genes causing diseases in the different metabolic pathways, that are relatively frequent (also in our bio/databank), or treatable/potentially treatable disorders.
When deploying CentoMetabolic panel, the coding regions, 10 bp of flanking intronic sequences, and known coding and non-coding pathogenic/likely pathogenic (P/LP) variants based on ClinVar, Human Gene Mutation Database® (HGMD), and CENTOGENE’s Bio/Databank [13], of the selected genes were targeted for analysis. Data analysis, including alignment to the hg19 human reference genome (Genome Reference Consortium GRCh37), variant calling, and annotation is performed using a validated in-house pipeline [14]. Variants with insufficient quality scores were confirmed via Sanger sequencing according to our established criteria [15].
A semi-automated filtering strategy for the SNV and small indels was used, with the variants fulfilling the following criteria being selected for further evaluation: (1) variants previously classified in CENTOGENE’s Bio/Databank as P/LP, or as variants of uncertain significance (VUS); (2) unclassified variants; (3) variants with minor allele frequency (MAF) < 1% including our healthy cohort, and in silico predictions of high/moderate impact on protein function; (4) all variants described as disease-causing by external databases (HGMD and ClinVar); (5) variants with adaptive boosting (ADA) and random forest (RF) scores from dbscSNV19 > 0.6, consistent with predictions of abnormal splicing; (6) exclusion of variants previously classified as (likely) benign. Our healthy cohort includes approximately 24,000 adult individuals (>18 years) who are said to be unaffected, had no linked human phenotype ontology (HPO) terms, and had genome/exome data available.
A similar strategy was applied for the CNV selection (<2% MAF): (i) homozygous deletions (0 copy number); (ii) heterozygous deletions (1 copy) and duplications (>2 copies), affecting >2 exons. The CNV detection algorithm has a sensitivity of above 95% for all homozygous deletions and heterozygous deletions/duplications spanning at least three consecutive exons, based on the internal validation dataset of 150 individuals. In the current cohort, CNVs were evaluated by visual inspection of the raw data in the integrative genome viewer (IGV). Usually, homozygous variants did not require confirmation by an orthogonal method. Heterozygous CNVs, were always confirmed by qPCR, multiplex ligation-dependent probe amplification (MLPA), or chromosomal microarray (CMA).
When a P/LP/VUS variant was detected with zygosity corresponding to the mode of inheritance of the related disorder, and a biochemical assay was available at CENTOGENE, determination of the corresponding enzymatic activity and/or biomarker concentration was performed to complement and assist on the variant classification. The enzymatic activities were determined either by fluorimetry or liquid chromatography coupled with mass spectrometry in dried blood spots (Supplementary Tables 1 and 2). The quantification of the biomarkers was performed in DBS using mass spectrometry. All tests were accredited according to ISO 15189 guidelines.
The selected variants were then evaluated with respect to their pathogenicity and causality and are classified into five classes (P, LP, VUS, likely benign, benign), according to the ACMG guidelines for variant classification [16]. For final variant classification and reporting, the phenotype of the patient (HPOs), clinical suspicion, and results from other lab tests (if provided) were taken into consideration.
Interpretation of the findings was performed in the clinical context, with reports being issued as: (i) positive, for patients with P/LP variant(s) explaining the phenotype(s); (ii) unclear, for cases with VUS compatible with the clinical phenotype (at least partially); (iii) negative, for cases with no relevant variant identified.
Results
The implemented panel included 206 genes related to more than 180 metabolic diseases assembled in 18 metabolic categories, with predominance of the lysosomal disorders (48 genes), carbohydrate (35 genes), and amino acid/peptide metabolism disorders (33 genes) (Supplementary Table 3). A full list of the genes included in the panel is shown in the Supplementary Information.
With this panel, we tested a global cohort with patients that originated from 62 countries (Supplementary Table 4). Over 60% of the patients were referred from Africa and Asia (n = 1232, 33% and n = 1122, 30%, respectively). Other patients originated from Europe (n = 901, 24%), Latin America (n = 218, 6%), the Middle East (n = 201, 6%), and North America (n = 45, 1%) (Table 1).
We were particularly interested in age at onset, family history, and consanguinity, but in many cases, the information was not provided by the referring clinicians (Table 1). For example, in only half of the cases, data on consanguinity was available. In 30.4% (n = 1133), the presence of parental consanguinity was reported. Most of the patients from the cohort were children younger than 5 years (n = 2392; 64.3%). On average, symptoms started around 1 year of age (range 0 to 34 years), with an average age at testing of 3 years (range 1 month to 38 years).
The main reasons for referrals are presented in Fig. 1 (HPOs). Neurological and non-neurological features were at the top of the list. Global developmental delay was the most frequently reported HPO (878 patients), followed by hepatomegaly (771 patients), seizures (443 patients), and coarse facial features (381 patients).
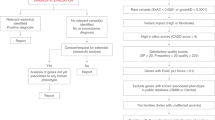
After NGS of the genes in the panel, variant calling, and annotation, a semi-automatic filtering of the NGS data was performed considering variant frequency, type, classification, and zygosity, among others. Biochemical testing was then carried out if applicable (Fig. 2).
Diagnostic yield, genetic variants, and biochemical testing
A variant compatible with the phenotype was reported in 52% of the cases (n = 1943), from whom 37% (n = 1389) received a genetic diagnosis based on P/LP variants explaining the phenotype (Fig. 3A). Interestingly, the diagnostic yield varied per geographic origin, with the highest diagnostic yield obtained for patients from Asia (nearly 60%, n = 645), followed by patients from Africa (41%, n = 505), and from Latin America (29%, n = 63) (Fig. 3B).
We explored which factors could be contributing to the diagnostic yield by comparing features of the ‘positive’ and ‘negative’ cohorts. Besides differences observed in country of origin, positive family history and parental consanguinity, were more frequently reported in the positive group compared to the negative cohort (Supplementary Table 5).
We identified a total of 1415 P/LP variant occurrences, from which 701 were unique variants. Most of the P/LP variants were SNV (94%, n = 649) with missense, loss of function (LoF) variants (nonsense, frameshift, splicing), and other detected variants (Fig. 4A). In addition, we identified 40 unique CNVs (6%), given that the panel included detection of large CNVs based on the NGS data analysis. Most of the CNVs were deletions (85%, n = 34) and affected a single gene. However, in four cases, we found large CNVs affecting multiple genes and leading to unexpected diagnoses of distal trisomy 2p, trisomy 12p, Turner syndrome, and Xq microdeletion syndrome. These patients presented features such as hepatomegaly, hypoglycemia, hypertriglyceridemia (childhood or juvenile onset), nausea and vomiting, jaundice, macroglossia, and coarse facial features, which likely led to the referral of the patients with suspicion of a metabolic disorder. Recurrent CNVs were detected affecting the IDS, IDUA, SLC3A1, and LDLR genes (4x each), GLB1 and AGL (3x each), GALNS, ATP7A, CYP21A2, and SLC7A7 (2x each).
In some cases, the genetic diagnosis was based on the detection of a SNV and a CNV affecting the same gene. For example, in a 3-month-old male index with seizures, body odor, hyperisoleucinemia, hyperleucinemia, and hypervalinemia, we identified a heterozygous likely pathogenic frameshift variant and a heterozygous likely pathogenic deletion of exons 2-3 of the DBT gene. This, together with the specific clinical presentation strongly suggests the diagnosis of autosomal recessive maple syrup urine disease type II. Indeed, further carrier testing in the parents confirmed the trans phase of the alleles. In addition, a 2-year-old male index presenting with abdominal distention and splenomegaly had a heterozygous pathogenic missense variant and a heterozygous pathogenic deletion of exons 8-10 of the GBA gene. The activity of beta-glucocerebrosidase was extremely low, and the biomarker lyso-Gb1 was pathologically increased—establishing the diagnosis of Gaucher disease. The last patient of this group was a 1-year-old male that presented with global developmental delay, hepatosplenomegaly, cherry red spot of the macula, and hyperammonemia. We identified a pathogenic heterozygous deletion encompassing exons 1 to 17, and a pathogenic hemizygous frameshift variant, both affecting the GLB1 gene. In addition, the activity of beta-galactosidase was pathologically reduced, confirming the genetic diagnosis of GM1-gangliosidosis type I.
Usefulness of combined genetic/biochemistry testing
For over half of the 1415 variants classified as P/LP, biochemical testing was carried out (51.8%, n = 733). From the variants that were ultimately classified as P/LP, 176 were novel and located within genes with biochemical testing available. The results of the enzymatic and/or biomarker testing were essential to decide on the clinical relevance of the variant. For example, 23 and 20 novel variants were classified as P/LP in SMPD1 and NPC1, respectively. The list of 176 novel variants is presented in Supplementary Table 6.
To further assess the impact of the biochemical testing, we evaluated all variants that had triggered a biochemical analysis, and the resulting variant classification and reports. In 620 patients, the diagnostic conclusion had been influenced by the result of the biochemical testing (Table 2). Having the biochemical result likely led to the low number of VUS reported in this cohort. Among those, in only 11 cases a VUS was reported, along with a negative or positive biochemical result. For example, we identified two heterozygous missense variants in PSAP in a 1-year-old patient with abdominal distention, hepatomegaly, and hyperlipidemia, and normal biomarker lyso-Gb1. The variants were reported (VUS) with recommendation to further parental targeted testing and biomarker lyso-Gb1 follow-up. Conversely, we also had cases with pathological enzymatic or biomarker testing, but the detected variants were classified as VUS based on the presence of contradictory evidence.
In other cases, the result from biochemical testing was instrumental for excluding the clinical relevance of the variant(s). Specifically, in 19 patients, the identified variant was excluded from reporting after the enzymatic/biomarker determination was within normal values (Table 2). In some cases, intronic variants could be excluded (e.g. GALNS, NM_001323544.1:c.1020 + 307 G > C), and in others, the phase of two heterozygous variants was inferred as being in the same allele (cis configuration), as examples: TPP1 (NM_000391.3:c.340 G > A, p.(Val114Met) and NM_000391.3:c.1033 A > C, p.(Met345Leu)).
More importantly, in 590 cases the pathological result of the biochemical tests guided the variant classification and final reporting. These 590 patients received a genetic diagnosis with supportive biochemical evidence. The most impacted gene was GBA (103 patients with Gaucher disease).
Diseases detected in this cohort
Overall, 120 different diseases were diagnosed with the top five diseases being Gaucher disease, Niemann-Pick disease type A/B, mucopolysaccharidosis type I, phenylketonuria, and Wilson disease (Fig. 4B). Conversely, 30 diseases were ultra-rare in this cohort and were detected only once each. Most disorders were autosomal recessive (n = 102). All diseases that were diagnosed are provided in Supplementary Table 6.
Considering the different geographic regions, the top three diseases in patients from Asia and Africa were Gaucher disease, Niemann-Pick disease type A, Wilson disease (Asia), and phenylketonuria, Gaucher disease, and mucopolysaccharidosis type II (Africa). Surprisingly, phenylketonuria was one of the top three diseases in tested patients from Europe.
When combined, 300 patients were diagnosed with a type of mucopolysaccharidosis (ARSB, GALNS, GLB1, GUSB, HGSNAT, IDS, IDUA, NAGLU, and SGSH genes). Mucopolysaccharidosis type I (IDUA = 81 patients), type IVA (GALNS = 50 patients), and type II (IDS = 41 patients) were the most commonly diagnosed. Importantly, for five of these diseases there is enzyme replacement therapy (ERT) available. Thus, 200 of these patients would be eligible for treatment. Furthermore, from this cohort, 610 patients (43%, n = 1389) were diagnosed with diseases which are treatable.
We also investigated the time between the onset of symptoms and the establishment of a genetic diagnosis (often referred to as a “diagnostic odyssey”). Data was available for 126 patients with positive reports. On average, these patients waited 2 years from the described onset of symptoms until a diagnosis could be established, with a range from 0 to 20 years. Five patients waited over 10 years to receive a diagnosis. These cases were from Asia, Africa, and Latin America with Dubin-Johnson syndrome, alkaptonuria, fucosidosis, Gaucher disease, and phenylketonuria.
Discussion
IMDs can present at any time, from the antenatal period to adulthood, with insidious or acute presentations, and with a wide clinical spectrum ranging from unspecific neurodevelopmental delay to acute metabolic decompensation and death. Early disease recognition, accurate diagnosis, and treatment are lifesaving in many cases [17].
The use of NGS panels for phenotypically related disorders can increase the likelihood of identifying an underlying genetic cause and may be preferred to exome or genome sequencing to maximize target coverage and avoid secondary findings [18]. Traditionally, the diagnosis of metabolic diseases is achieved via genetic testing (NGS panels—Sanger sequencing) or biochemical testing, in patients with a clinical presentation suggestive of an IMD. Current testing methods for IMDs comprise a stepwise strategy starting with molecular and followed by biochemical testing or vice versa [19] (ACMG Statements and Guidelines—https://www.nature.com/collections/afebagafci).
Approaches that combine genetic and metabolomic/biochemical data have been suggested as highly beneficial for the diagnosis of IMDs [17, 20, 21], but to our knowledge, this multiomic approach has not been implemented in the clinical practice so far.
In this study, we describe our applied tool with integrated genetic and biochemical testing for the diagnosis of genetic metabolic disorders. This approach has several advantages: (i) convenient use of filter cards (CentoCard) for handling, transportation, and genetic—biochemical testing using DBS; (ii) simultaneous detection of SNVs and CNVs; (iii) semi-automatic filtering of variants, with subsequent biochemical workflow activation in the same laboratory; (iv) comprehensive interpretation and classification of genetic variants; and (v) shortened diagnostic odyssey by avoiding stepwise testing.
Within this study, we report the results of our first 3720 patients. The obtained diagnostic yield of 37%, with genetic diagnoses established in 1389 patients, is comparable or even higher than the average reported yield after exome sequencing [14, 22]. Within this cohort, the diagnostic yield raised to nearly 60% in patients that originated from Asia (mainly Pakistan), which is also comparable to the results from exome sequencing in patients from the same area and hospital [23]. This could be due to the specific referral centers some of them with specialization on metabolic disorders, and the simultaneous lack of local resources for neonatal screening and genetic testing. Other factors such as the presence of parental consanguinity and positive family history are influencing the diagnostic yield (Supplementary Table 5), as described by us before [14, 23].
We identified 1415 P/LP variant occurrences; for 51.8% of them, a biochemical test was performed. In the majority of the patients, the variant classification as P/LP was supported by the result of the enzymatic/biomarker testing (Table 2). This was particularly relevant for intronic variants and novel missense variants, which are usually classified as VUS, in the absence of additional evidence (Table 2). In addition, the biochemical testing allowed the exclusion of other genetic variants based on normal test results.
Our results also contribute to increased knowledge on the genetic etiology of rare diseases. Taking peroxisomal biogenesis disorders as an example, the Zellweger spectrum disorder is caused by pathogenic variants in 13 known ZSD-PEX genes [24]. According to the literature PEX1 is responsible for over 60% of the cases. However, in our cohort PEX12 is the major gene involved, with five patients diagnosed (Supplementary Table 6). The wide spectrum of novel causative genetic variants reported here is likely due to the testing of a global cohort, with inclusion of patients from geographic regions that usually have limited access to molecular testing resources and are underrepresented in the scientific literature and genetic databases.
We also confirm previous findings on specific established pathogenic variants. For example, Gaucher disease was the most frequently detected disorder in our cohort, with 126 newly diagnosed patients. Over half of them were homozygote or compound heterozygotes for a single specific GBA pathogenic variant (NM_000157.3:c.1448 T > C, p.(Leu483Pro)), which is known to be among the four most common pathogenic variants in GBA [25]. Of note, we also detected seven novel P/LP variants in GBA.
Unexpectedly, phenylketonuria was among the top five diseases detected in this cohort (58 patients, Fig. 4B), and it was diagnosed mainly in tested patients from Africa (Egypt). In addition, this is one of the top three diseases being diagnosed in tested patients from Europe (Georgia and Romania). Phenylketonuria is an excellent example of a treatable disease and a model for early detection and treatment, as this was one of the first diseases covered by newborn screening programs in the early 1960s [26, 27].
The aim for newborn screening is early detection of treatable disorders, and a small group of metabolic disorders is usually included in the different screening programs. This ensures that at least part of the infants with IMDs are diagnosed before the onset of symptoms—significantly improving the options for therapy and health outcomes [28]. Unfortunately, newborn screening is not well-established in most resource limited countries. The fact that phenylketonuria is still a common disorder being diagnosed in our study cohort illustrates the challenges that mainly developing countries have with implementation and expansion of their newborn screening programs (major problems are financial issues, medical and logistical support, society education, policy development, program evaluation, and sustainability) [27].
As such, our integrated diagnostic approach is relevant for improvement of the diagnosis and early detection of IMDs. This is even more relevant for groups of IMDs, such as mucopolysaccharidosis, aminoacidopathies, and organic acidemias, amongst others, that are treatable via nutritional therapy, vitamin and trace element substitution, enzyme replacement therapy, hematopoietic stem cell transplant, solid organ transplantation, pharmacological therapy, and gene-based therapy, among others [8]. This holds especially true as one of the most effective treatments are nutritional, which are relatively affordable, widely available, and in many cases, highly effective [8]. It is striking that four of the top five diseases have specific treatments, such as dietary management, enzyme replacement therapy, and substrate reduction therapy, among others.
In conclusion, we show that combined genetic and biochemical testing facilitated the decision on clinical relevance of the variants and led to a high diagnostic yield (37%). The established genetic diagnosis in nearly 1400 patients is expected to lead to benefits in treatment and/or counseling for the families. Future approaches should integrate transcriptomics, proteomics, and/or metabolomics for an enhanced detection and treatment of IMDs.
Data availability
The de-identified data set is available on request to the corresponding author.
References
Garrod AE. The incidence of alkaptonuria: a study in chemical individuality. 1902. Mol Med. 1996;2:274–82.
Saudubray JM, Garcia-Cazorla À. Inborn Errors of Metabolism Overview: Pathophysiology, Manifestations, Evaluation, and Management. Pediatr Clin North Am. 2018;65:179–208.
Fukao T, Nakamura K. Advances in inborn errors of metabolism. J Hum Genet. 2019;64:65.
Ferreira CR, Rahman S, Keller M, Zschocke J. An international classification of inherited metabolic disorders (ICIMD). J Inherit Metab Dis. 2021;44:164–77.
Sanderson S, Green A, Preece MA, Burton H. The incidence of inherited metabolic disorders in the West Midlands, UK. Arch Dis Child. 2006;91:896–9.
Dionisi-Vici C, Rizzo C, Burlina AB, Caruso U, Sabetta G, Uziel G, et al. Inborn errors of metabolism in the Italian pediatric population: a national retrospective survey. J Pediatr. 2002;140:321–7.
Applegarth DA, Toone JR, Lowry RB. Incidence of inborn errors of metabolism in British Columbia, 1969-1996. Pediatrics. 2000;105:e10.
Hoytema van Konijnenburg EMM, Wortmann SB, Koelewijn MJ, Tseng LA, Houben R, Stöckler-Ipsiroglu S, et al. Treatable inherited metabolic disorders causing intellectual disability: 2021 review and digital app. Orphanet J Rare Dis. 2021;16:170.
van Karnebeek CD, Stockler S. Treatable inborn errors of metabolism causing intellectual disability: a systematic literature review. Mol Genet Metab. 2012;105:368–81.
El-Hattab AW, Almannai M, Sutton VR. Newborn Screening: History, Current Status, and Future Directions. Pediatr Clin North Am. 2018;65:389–405.
van Karnebeek CDM, Wortmann SB, Tarailo-Graovac M, Langeveld M, Ferreira CR, van de Kamp JM, et al. The role of the clinician in the multi-omics era: are you ready? J Inherit Metab Dis. 2018;41:571–82.
Ferreira CR, van Karnebeek CDM. Chapter 22—Inborn errors of metabolism. In: de Vries LS, Glass HC, editors. Handbook of Clinical Neurology. Elsevier, The Netherlands; 2019, Vol 162, p. 449–81.
Trujillano D, Oprea GE, Schmitz Y, Bertoli-Avella AM, Abou Jamra R, Rolfs A. A comprehensive global genotype-phenotype database for rare diseases. Mol Genet Genom Med. 2017;5:66–75.
Trujillano D, Bertoli-Avella AM, Kumar Kandaswamy K, Weiss ME, Koster J, Marais A, et al. Clinical exome sequencing: results from 2819 samples reflecting 1000 families. Eur J Hum Genet. 2017;25:176–82.
Bauer P, Kandaswamy KK, Weiss MER, Paknia O, Werber M, Bertoli-Avella AM, et al. Development of an evidence-based algorithm that optimizes sensitivity and specificity in ES-based diagnostics of a clinically heterogeneous patient population. Genet Med. 2019;21:53–61.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Stenton SL, Kremer LS, Kopajtich R, Ludwig C, Prokisch H. The diagnosis of inborn errors of metabolism by an integrative “multi-omics” approach: A perspective encompassing genomics, transcriptomics, and proteomics. J Inherit Metab Dis. 2020;43:25–35.
Bean LJH, Funke B, Carlston CM, Gannon JL, Kantarci S, Krock BL, et al. Diagnostic gene sequencing panels: from design to report-a technical standard of the American College of Medical Genetics and Genomics (ACMG). Genet Med. 2020;22:453–61.
De Biase I, Tortorelli S, Kratz L, J. Steinberg S, Cusmano-Ozog K, Braverman N, et al. Laboratory diagnosis of disorders of peroxisomal biogenesis andfunction: a technical standard of the American College of Medical Genetics and Genomics(ACMG). Genet Med. 2020;22:686–97.
Alaimo JT, Glinton KE, Liu N, Xiao J, Yang Y, Reid Sutton V, et al. Integrated analysis of metabolomic profiling and exome data supplements sequence variant interpretation, classification, and diagnosis. Genet Med. 2020;22:1560–6.
Ghosh A, Schlecht H, Heptinstall LE, Bassett JK, Cartwright E, Bhaskar SS, et al. Diagnosing childhood-onset inborn errors of metabolism by next-generation sequencing. Arch Dis Child. 2017;102:1019–29.
Clark MM, Stark Z, Farnaes L, Tan TY, White SM, Dimmock D, et al. Meta-analysis of the diagnostic and clinical utility of genome and exome sequencing and chromosomal microarray in children with suspected genetic diseases. NPJ Genom Med. 2018;3:16.
Cheema H, Bertoli-Avella AM, Skrahina V, Anjum MN, Waheed N, Saeed A, et al. Genomic testing in 1019 individuals from 349 Pakistani families results in high diagnostic yield and clinical utility. NPJ Genom Med. 2020;5:44.
Steinberg SJ, Raymond GV, Braverman NE, Moser AB. Zellweger Spectrum Disorder. In: Adam MP, Ardinger HH, Pagon RA et al. editors. Seattle (WA): GeneReviews((R)); 1993.
Pastores GM, Hughes DA. Gaucher Disease. In: Adam MP, Ardinger HH, Pagon RA et al., editors. GeneReviews(®). Seattle (WA): University of Washington, SeattleCopyright © 1993-2021, University of Washington, Seattle. GeneReviews is a registered trademark of the University of Washington, Seattle. All rights reserved., 1993.
Guthrie R, Susi A. A Simple Phenylalanine Method For Detecting Phenylketonuria In Large Populations Of Newborn Infants. Pediatrics. 1963;32:338–43.
McCabe LL, Therrell BL Jr, McCabe ER. Newborn screening: rationale for a comprehensive, fully integrated public health system. Mol Genet Metab. 2002;77:267–73.
Fuller M. Laboratory Diagnosis of Lysosomal Diseases: Newborn Screening to Treatment. Clin Biochem Rev. 2020;41:53–66.
Acknowledgements
We thank the patients and families, as well as their referring clinicians for their participation. No specific funding was received for this manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: AB-A, PB; Data curation and formal analysis: LSA, CP, RA, SS, TBo, AK; Method development:, AU, CC, CJM, FV; Sample collection logistics/supervision: MA, SA, SI; Sample and laboratory processing: TCLSS, NV, SO; Supervision of sample processing and/or diagnostics: OP, CC, PGM, TB, FV, JPB, AB-A, PB; Clinical assessment and referral of patients: EJ, SME, HT, IM, ABJ, AC, RC, TT, AMN, IGEDM, FM, MK, LAMS, HAC; Writing-original draft: LSA, CP, AB-A; Writing-review, editing, and project supervision: JPB, AB-A, PB.
Corresponding author
Ethics declarations
Competing interests
LSA, CP, RA, SS, TBo, AK, AU, TCLSS, NV, SO, MA, SA, SI, PG-M, OP, CC, CJM, TB, FV, JP-B, AB-A, and PB are employees at CENTOGENE GmbH. None of the other authors declare a conflict of interest.
Ethics approval
The current project has been conducted within a diagnostic setting and in a second step, utilized de-identified data and samples, and thus did not require Institutional Review Board approval in our jurisdiction. Written informed consent for genetic testing related to the disease(s) of the patient was obtained. Additionally, the consent form declaration included information regarding storage of the data and further data processing for research purposes. Written informed consent was given by patients, parents, or referring physicians. The informed consent form is available in English and several other languages at https://www.centogene.com/downloads.html.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Almeida, L.S., Pereira, C., Aanicai, R. et al. An integrated multiomic approach as an excellent tool for the diagnosis of metabolic diseases: our first 3720 patients. Eur J Hum Genet 30, 1029–1035 (2022). https://doi.org/10.1038/s41431-022-01119-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41431-022-01119-5
This article is cited by
-
Beyond genomics: using RNA-seq from dried blood spots to unlock the clinical relevance of splicing variation in a diagnostic setting
European Journal of Human Genetics (2025)
-
Adult genomic medicine: lessons from a multisite study of 2700 patients
Genome Medicine (2025)
-
Further evidence supporting the role of GTDC1 in glycine metabolism and neurodevelopmental disorders
European Journal of Human Genetics (2024)
-
Facing the challenges to shorten the diagnostic odyssey: first Whole Genome Sequencing experience of a Colombian cohort with suspected rare diseases
European Journal of Human Genetics (2024)
-
2022: the year that was in the European Journal of Human Genetics
European Journal of Human Genetics (2023)