Abstract
Aims
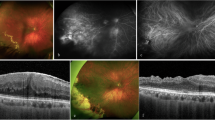
To report anatomical and functional outcomes in patients with proliferative sickle retinopathy (PSR) who underwent 23-gauge (23G) and 20-gauge (20G) vitrectomy.
Methods
Retrospective consecutive case series of patients who underwent vitreoretinal intervention for complications of PSR between April 2009 and February 2015. Operations were performed at a tertiary referral centre, Moorfields Eye Hospital. Visual acuity and anatomical success rates were evaluated for PSR complicated by retinal detachment, tractional vitreous haemorrhage and macular hole. Proliferative diabetic retinopathy cases were excluded.
Results
A total of 71 eyes (63 patients) underwent vitreoretinal surgery for PSR complications with 26 months mean follow-up. Primary indications were: tractional retinal detachment (TRD, n = 17), TRD with rhegmatogenous retinal detachment (n = 16), rhegmatogenous retinal detachment (n = 5, macula-on: 1, macula-off: 4), vitreous haemorrhage (n = 19), epiretinal membrane (n = 6), and full thickness macula hole (n = 8). Thirty-nine cases underwent 20G vitrectomy, and 23G surgery was performed in 32 eyes. Mean best corrected visual acuity (BCVA) improved from pre-operative 1.30 LogMAR to final BCVA of 0.74 LogMAR (p < 0.01, paired t-test). 23G vitrectomy yielded slightly better 32 vs. 25 ETDRS-letter improvement compared with 20G vitrectomy (p = 0.60, NS, unpaired t-test). 23G was associated with fewer per-operative complications (23G, 18% vs. 20G,13%). The subset of 38 eyes with retinal detachment demonstrated 79% primary reattachment rate, and a smaller BCVA improvement of 3 lines (p = 0.07, paired t-test).
Conclusions
Surgical intervention for complicated PSR can preserve and/or improve vision although the degree of visual acuity stabilisation remains guarded in tractional/rhegmatogenous detachments. 23G vitrectomy may give a better functional outcome with lower per-operative complication rates.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rees DC, Williams TN, Gladwin MT. Sickle-cell disease. Lancet. 2010;376:2018–31.
Elagouz M, Jyothi S, Gupta B, Sivaprasad S. Sickle cell disease and the eye: old and new concepts. Surv Ophthalmol. 2010;55:359–77.
Moriarty BJ, Acheson RW, Condon PI, Serjeant GR. Patterns of visual loss in untreated sickle cell retinopathy. Eye. 1988;2:330–5.
Condon PI, Serjeant GR. Behaviour of untreated proliferative sickle retinopathy. Br J Ophthalmol. 1980;64:404–11.
Williamson TH, Rajput R, Laidlaw DAH, Mokete B. Vitreoretinal management of the complications of sickle cell retinopathy by observation or pars plana vitrectomy. Eye. 2009;23:1314–20.
Chen RWS, Flynn HW, Lee WH, et al. Vitreoretinal management and surgical outcomes in proliferative sickle retinopathy: a case series. Am J Ophthalmol. 2014;157:870–5.e1.
Pulido JS, Flynn HW, Clarkson JG, Blankenship GW. Pars plana vitrectomy in the management of complications of proliferative sickle retinopathy. Arch Ophthalmol. 1988;106:1553–7.
Jampol LM, Green JL, Goldberg MF, Peyman GA. An update on vitrectomy surgery and retinal detachment repair in sickle cell disease. Arch Ophthalmol. 1982;100:591–3.
Myint KT, Sahoo S, Thein AW, Moe S, Ni H. Laser therapy for retinopathy in sickle cell disease. Cochrane Database Syst Rev. 2015;CD010790.
Muqit MM, Denniss J, Nourrit V, et al. Spatial and spectral imaging of retinal laser photocoagulation burns. Invest Ophthalmol Vis Sci. 2011:52:994–1002.
Wang Y, Muqit MM, Stanga PE, Young LB, Henson DB. Spatial changes of central field loss in diabetic retinopathy after laser. Optom Vis Sci. 2014;91:111–20.
Acknowledgements
We acknowledge expert advice and non-financial support from the NIHR London Biomedical Research Centre, the Vitreoretinal Service, and Dr Catherine Egan of the Medical Retina Service at Moorfields Eye Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Ho, J., Grabowska, A., Ugarte, M. et al. A comparison of 23-gauge and 20-gauge vitrectomy for proliferative sickle cell retinopathy – clinical outcomes and surgical management. Eye 32, 1449–1454 (2018). https://doi.org/10.1038/s41433-018-0127-y
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-018-0127-y
This article is cited by
-
Proliferative Sickle Cell Retinopathy: A Patient and a Physician’s Perspective on Quality of Life and Quality of Eye Care
Ophthalmology and Therapy (2024)
-
Action on sickle cell retinopathy: the time is now
Eye (2022)
-
Comparison of postoperative ciliary body changes associated with the use of 23-gauge and 20-gauge system for pars plana vitrectomy
BMC Ophthalmology (2018)