Abstract
Purpose
To report surgical outcomes and endothelial cell density (ECD) trends up to 2 years post-operatively in the first cohort of eyes undergoing Descemet’s membrane endothelial keratoplasty (DMEK) for low-to-moderate risk indications at our UK centre. Tight corneal sutures were used to ensure high intraoperative pressure from intracameral air for 10-min and to maintain a good post-operative air fill. Outcomes were compared to a prior series at our unit of similar eyes having Descemet’s stripping endothelial keratoplasty (DSEK).
Methods
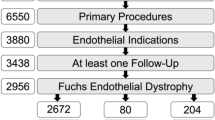
Retrospective, interventional series. Inclusions: all DMEKs with a minimum of 1-month follow-up. Exclusions: prior glaucoma surgery, penetrating keratoplasty or anterior chamber lens.
Results
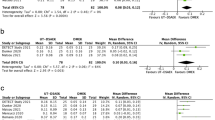
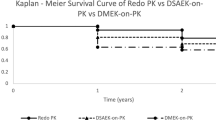
88 DMEKs met inclusion. Median follow-up: 332 days. Main indication: Fuchs dystrophy (90%). Complications: re-bubbling 2%, primary failure 6%, retinal detachment 2%, rejection 3%. At 3 months, BCVA ≥6/6 and ≥6/9 were 67% and 86%, respectively. Graft survival at both 1 and 2 years was 94 ± 2%. Mean(±SD) cell-loss at 1 month, 3 months, 6 months, 12 months and 24 months: 30 ± 15%, 29 ± 16%, 33 ± 17%, 35 ± 17% and 48 ± 16%, respectively. Compared to a prior series at our unit of 210 low-to-moderate risk DSEKs, cell loss was lower for DMEK at all time-points (p < 0.001) through to 12 months but was not statistically different at 24 months. Mixed-modelling of ECD over time demonstrated the convergence of DMEK and DSEK curves by 2 years.
Conclusions
DMEK using tissue from UK eye-banks resulted in high survival and excellent visual acuity. ECD through 1 year was superior to DSEK in a similar cohort. Our low re-bubble rate (2%) may be attributable to use of intracameral air at temporarily elevated intraocular pressure.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Melles GRJ, Lander F, Rietveld FJR. Transplantation of Descemet’s membrane carrying viable endothelium through a small scleral incision. Cornea. 2002;21:415–8.
Melles GRJ, Ong T, Ververs B, van der Wees J. Descemet membrane endothelial keratoplasty. Cornea. 2006;25:987–90.
Ham L, Dapena I, van Luijk C, van der Wees J, Melles GRJ. Descemet membrane endothelial keratoplasty (DMEK) for Fuchs endothelial dystrophy: review of the first 50 consecutive cases. Eye (Lond). 2009;23:1990–8.
Deng SX, Lee WB, Hammersmith KM, Kuo AN, Li JY, Shen JF, et al. Descemet membrane endothelial keratoplasty: safety and outcomes. Ophthalmology. 2017. https://doi.org/10.1016/j.ophtha.2017.08.015.
Oellerich S, Baydoun L, Peraza-Nieves J, Ilyas A, Frank L, Binder PS, et al. Multicenter study of 6-month clinical outcomes after Descemet’s membrane endothelial keratoplasty. Cornea. 2017;36:1467–76.
Melles GRJ, Wijdh RHJ, Nieuwendaal CP. A technique to excise the Descemet membrane from a recipient cornea (descemetorhexis). Cornea. 2004;23:286–8.
Armitage WJ, Dick A, Bourne WM. Predicting endothelial cell loss and long-term corneal graft survival. Invest Ophthalmol Vis Sci. 2003;44:3326–31.
Fajgenbaum MA, Hollick EJ. Modeling endothelial cell loss after Descemet stripping endothelial keratoplasty. Cornea. 2017;36:553–60.
Price MO, Fairchild KM, Price DA, Price FW. Descemet’s stripping endothelial keratoplasty: five-year graft survival and endothelial cell loss. Ophthalmology. 2011;118:725–9.
Wacker K, Baratz KH, Maguire LJ, McLaren JW, Patel SV. Descemet stripping endothelial keratoplasty for Fuchs’ endothelial corneal dystrophy: five-year results of a prospective study. Ophthalmology. 2016;123:154–60.
Ang M, Soh Y, Htoon HM, Mehta JS, Tan D. Five-year graft survival comparing Descemet stripping automated endothelial keratoplasty and penetrating keratoplasty. Ophthalmology. 2016;123:1646–52.
Fajgenbaum M, Hollick EJ. Center and surgeon effect on outcomes of endothelial keratoplasty versus penetrating keratoplasty in the United Kingdom. Am J Ophthalmol. 2015;160:392–3.
Riddlesworth TD, Kollman C, Lass JH, Patel SV, Stulting RD, Benetz BA, et al. A mathematical model to predict endothelial cell density following penetrating keratoplasty with selective dropout from graft failure. Invest Ophthalmol Vis Sci. 2014;55:8409–15.
Brissette A, Conlon R, Teichman JC, Yeung S, Ziai S, Baig K. Evaluation of a new technique for preparation of endothelial grafts for Descemet membrane endothelial keratoplasty. Cornea. 2015;34:557–9.
Dapena I, Moutsouris K, Droutsas K, Ham L, van Dijk K, Melles GRJ. Standardized “no-touch” technique for Descemet membrane endothelial keratoplasty. Arch Ophthalmol. 2011;129:88–94.
Rodríguez-Calvo-De-Mora M, Quilendrino R, Ham L, Liarakos VS, van Dijk K, Baydoun L, et al. Clinical outcome of 500 consecutive cases undergoing Descemet’s membrane endothelial keratoplasty. Ophthalmology. 2015;122:464–70.
Hamzaoglu EC, Straiko MD, Mayko ZM, Sáles CS, Terry MA. The first 100 eyes of standardized Descemet stripping automated endothelial keratoplasty versus standardized Descemet membrane endothelial keratoplasty. Ophthalmology. 2015;122:2193–9.
Deng SX, Sanchez PJ, Chen L. Clinical outcomes of Descemet membrane endothelial keratoplasty using eye bank-prepared tissues. Am J Ophthalmol. 2015;159:590–6.
Guerra FP, Anshu A, Price MO, Giebel AW, Price FW. Descemet’s membrane endothelial keratoplasty: prospective study of 1-year visual outcomes, graft survival, and endothelial cell loss. Ophthalmology. 2011;118:2368–73.
Siggel R, Adler W, Stanzel TP, Cursiefen C, Heindl LM. Bilateral Descemet membrane endothelial keratoplasty. Cornea. 2016;35:772–7.
Dapena I, Ham L, Droutsas K, Van Dijk K, Moutsouris K, Melles GR. Learning curve in Descemet’s membrane endothelial keratoplasty: first series of 135 consecutive cases. Ophthalmology. 2011;118:2147–54.
Singh A, Zarei-Ghanavati M, Avadhanam V, Liu C. Systematic review and meta-analysis of clinical outcomes of Descemet membrane endothelial keratoplasty versus Descemet stripping endothelial keratoplasty/Descemet stripping automated endothelial keratoplasty. Cornea. 2017;36:1437–43.
Khor W-B, Han S-B, Mehta JS, Tan DTH. Descemet stripping automated endothelial keratoplasty with a donor insertion device: clinical results and complications in 100 eyes. Am J Ophthalmol. 2013;156:773–9.
Busin M, Bhatt PR, Scorcia V. A modified technique for Descemet membrane stripping automated endothelial keratoplasty to minimize endothelial cell loss. Arch Ophthalmol. 2008;126:1133.
Feng MT, Burkhart ZN, Price FW, Price MO. Effect of donor preparation-to-use times on Descemet membrane endothelial keratoplasty outcomes. Cornea. 2013;32:1080–2.
Ham L, Dapena I, Liarakos VS, Baydoun L, van Dijk K, Ilyas A, et al. Midterm results of Descemet membrane endothelial keratoplasty: 4 to 7 years clinical outcome. Am J Ophthalmol. 2016;171:113–21.
Schlögl A, Tourtas T, Kruse FE, Weller JM. Long-term clinical outcome after Descemet membrane endothelial keratoplasty. Am J Ophthalmol. 2016;169:218–26.
Acknowledgements
The authors acknowledge David Johnson, PhD, for assistance in the database management.
Funding
The authors declare no financial or proprietary interest in the materials presented. No funding or financial support was provided for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fajgenbaum, M.A.P., Kopsachilis, N. & Hollick, E.J. Descemet’s membrane endothelial keratoplasty: surgical outcomes and endothelial cell count modelling from a UK centre. Eye 32, 1629–1635 (2018). https://doi.org/10.1038/s41433-018-0152-x
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-018-0152-x
This article is cited by
-
Rebubbling and graft detachment in Descemet membrane endothelial keratoplasty using a standardised protocol
Eye (2023)
-
Changing trends in corneal transplantation: a national review of current practices in the Republic of Ireland
Irish Journal of Medical Science (1971 -) (2021)