Abstract
Aims
This study aimed to determine the incidence, clinical features and management of cicatrising conjunctivitis in Australia and New Zealand, also enabling comparison with data from the United Kingdom.
Methods
A prospective surveillance study was conducted over 17 months via the Australian and New Zealand Ophthalmic Surveillance Unit with a one-year follow-up period. Practicing ophthalmologists on the Surveillance Unit’s database were asked to report recently diagnosed cases of cicatrising conjunctivitis on a monthly basis. Initial and follow-up questionnaires were sent to ophthalmologists who had reported positive cases to obtain demographic and clinical data. The minimum incidence of cicatrising conjunctivitis was calculated based on cases reported during the study period and from population data.
Results
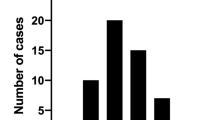
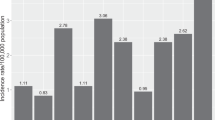
During the 17-month study period (December 2011–April 2013), 56 cases of cicatrising conjunctivitis were reported. Data was obtained for 35 cases (62%) with a mean age of 74 years (range, 28–94 years). The most common aetiologies were ocular mucus membrane pemphigoid (n = 18 cases, 51.4%), Stevens–Johnson Syndrome (n = 3, 8.6%) and graft versus host disease (n = 3, 8.6%). The minimum incidence of cicatrising conjunctivitis in Australia and New Zealand was 1.5 per million, comparable to incidence data from the United Kingdom.
Conclusions
This study is the first to prospectively record the incidence of cicatrising conjunctivitis in Australia and New Zealand and the second worldwide. It provides novel data on demographics and management of cicatrising conjunctivitis, as reported by treating ophthalmologists.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Dart JK. The 2016 Bowman Lecture Conjunctival curses: scarring conjunctivitis 30 years on. Eye. 2017;31:301–32.
Williams GP, Radford C, Nightingale P, Dart JK, Rauz S. Evaluation of early and late presentation of patients with ocular mucous membrane pemphigoid to two major tertiary referral hospitals in the United Kingdom. Eye. 2011;25:1207–18.
Elder MJ, Bernauer W, Leonard J, Dart JK. Progression of disease in ocular cicatricial pemphigoid. Br J Ophthalmol. 1996;80:292–6.
Chan LS, Ahmed AR, Anhalt GJ, Bernauer W, Cooper KD, Elder MJ, et al. The first international consensus of mucous membrane pemphigoid—definition, diagnostic criteria, pathogenic factors, medical treatment, and prognostic indicators. Arch Dermatol. 2002;138:370–9.
Saw VP, Dart JK. Ocular mucous membrane pemphigoid: diagnosis and management strategies. Ocul Surf. 2008;6:128–42.
Tauber J, Sainz DLM, Foster CS. Systemic chemotherapy for ocular cicatricial pemphigoid. Cornea. 1991;10:185–95.
Saw VP, Dart JK, Rauz S, Ramsay A, Bunce C, Xing W, et al. Immunosuppressive therapy for ocular mucous membrane pemphigoid: strategies and outcomes. Ophthalmology. 2008;115:253–61.
Thorne JE, Woreta FA, Jabs DA, Anhalt GJ. Treatment of ocular mucous membrane pemphigoid with immunosuppressive drug therapy. Ophthalmology. 2008;115:2146–52.
Bernauer W, Broadway DC, Wright P. Chronic progressive conjunctival cicatrisation. Eye. 1993;7:371–8.
Thorne JE, Anhalt GJ, Jabs DA. Mucous membrane pemphigoid and pseudopemphigoid. Ophthalmology. 2004;111:45–52.
Shikari H, Antin JH, Dana R. Ocular graft-versus-host disease: a review. Surv Ophthalmol. 2013;58:233–51.
Radford CF, Rauz S, Williams GP, Saw VP, Dart JK. Incidence, presenting features, and diagnosis of cicatrising conjunctivitis in the United Kingdom. Eye. 2012;26:1199–208.
Bobba S, Di Girolamo N, Mills R, Daniell M, Chan E, Harkin DG, et al. Nature and incidence of severe limbal stem cell deficiency in Australia and New Zealand. Clin Exp Ophthalmol. 2017;45:174–81.
Foot B, Stanford M, Rahi J, Thompson J. The British Ophthalmological Surveillance Unit: an evaluation of the first 3 years. Eye. 2003;17:9–15.
Hazin R, Ibrahimi OA, Hazin MI, Kimyai‐Asadi A. Stevens‐Johnson syndrome: Pathogenesis, diagnosis, and management. Ann Med. 2008;40:129–38.
Bernard P, Vaillant L, Labeille B, Bedane C, Arbeille B, Denoeux JP, et al. Incidence and distribution of subepidermal autoimmune bullous skin diseases in three French regions. Bullous Diseases French Study Group. Arch Dermatol. 1995;131:48–52.
Zillikens D, Wever S, Roth A, Weidenthaler-Barth B, Hashimoto T, Brocker EB. Incidence of autoimmune subepidermal blistering dermatoses in a region of central Germany. Arch Dermatol. 1995;131:957–8.
Hubner F, Recke A, Zillikens D, Linder R, Schmidt E. Prevalence and age distribution of pemphigus and pemphigoid diseases in Germany. J Invest Dermatol. 2016;136:2495.
Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS): Volume 3 – Non ABS Structures, July 2011. Canberra: Australian Bureau of Statistics; 2011 Jul. Accessed 10/10/2017, available at http://www.abs.gov.au/ausstats/abs@.nsf/0/736A18F4CBF81595CA2578D40012CF51.
Bernauer W, Elder MJ, Leonard JN, Wright P, Dart JK. The value of biopsies in the evaluation of chronic progressive conjunctival cicatrisation. Graefes Arch Clin Exp Ophthalmol. 1994;232:533–7.
Power WJ, Neves RA, Rodriguez A, Dutt JE, Foster CS. Increasing the diagnostic yield of conjunctival biopsy in patients with suspected ocular cicatricial pemphigoid. Ophthalmology. 1995;102:1158–63.
Grau AE, Setterfield J, Saw VP. How to do conjunctival and buccal biopsies to investigate cicatrising conjunctivitis: improving the diagnosis of ocular mucous membrane pemphigoid. Br J Ophthalmol. 2013;97:530–1.
Leonard JN, Hobday CM, Haffenden GP, Griffiths CE, Powles AV, Wright P, et al. Immunofluorescent studies in ocular cicatricial pemphigoid. Br J Dermatol. 1988;118:209–17.
Acknowledgements
NHMRC Career Development Fellowship for Author SW (APP1050524). Professor Watson is also supported by the Sydney Medical School Foundation. Australian and New Zealand Ophthalmic Surveillance Unit. Valerie P. Saw FRCOphth, Moorfields Eye Hospital, London, United Kingdom—collaboration in study design. Geraint P. Williams FRCOphth, Academic Unit of Ophthalmology, University of Birmingham, Birmingham, United Kingdom—collaboration in study design. Saaehla Rauz FRCOphth, Academic Unit of Ophthalmology, University of Birmingham, Birmingham, United Kingdom—collaboration in study design. Cherry Radford FRCOphth, Moorfields Eye Hospital, NHS Foundation Trust, City Road, London, United Kingdom—collaboration in study design. John Dart FRCOphth, Moorfields Eye Hospital, NHS Foundation Trust, City Road, London, United Kingdom—collaboration in study design.
Funding
NHMRC Career Development Fellowship for Author SW (APP1050524)
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Bobba, S., Devlin, C., Di Girolamo, N. et al. Incidence, clinical features and diagnosis of cicatrising conjunctivitis in Australia and New Zealand. Eye 32, 1636–1643 (2018). https://doi.org/10.1038/s41433-018-0155-7
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-018-0155-7
This article is cited by
-
Defining the limits of upper and lower conjunctival fornix depths in a healthy Asian Chinese population
Eye (2025)
-
Klinik des okulären Schleimhautpemphigoids
Die Ophthalmologie (2023)