Abstract
Background
Comparison of presentation and outcomes of central serous chorioretinopathy (CSC) between male and female subjects in different ethnic populations.
Methods
Retrospective comparison between male and female subjects with CSC was completed. Demographic details, clinical presentations, imaging features and treatment outcomes were compared at baseline and at last follow-up.
Results
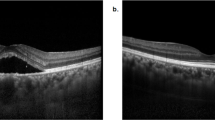
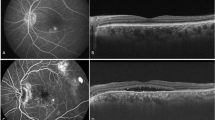
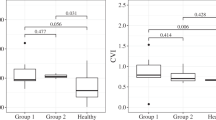
This study included 155 male and 155 female subjects with a mean (CSD) age of 43.8 ± 10.3 and 57.0 ± 12.1 years, respectively, and a mean duration of follow-up of 8.49 ± 12.6 months. At presentation, there was no difference in visual acuity; however, visual acuity was significantly higher for female subjects at last follow-up (p = 0.02). Optical coherence tomography (OCT) analysis showed that subretinal deposits (p < 0.001), hyperreflective foci (p = 0.001), retinal pigment epithelial detachment (p = 0.01) and retinal pigment epithelium (RPE) irregularities (p = 0.03) were higher in male subjects at presentation. Angiographic analysis showed that diffuse leakage and RPE tracts were common in males (p = 0.01 and p = 0.02). No significant differences in choroidal dilatation or diffuse choroidal leakages were noted.
Conclusions
Female subjects with CSC appear to have better outcomes, with less chances of diffuse RPE damage and other OCT features compared to males.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Colijn JM, Buitendijk GHS, Prokofyeva E, Alves D, Cachulo ML, Khawaja AP, et al. Prevalence of age-related macular degeneration in Europe: the past and the future. Ophthalmology. 2017;124:1753–63.
Rudnicka AR, Jarrar Z, Wormald R, Cook DG, Fletcher A, Owen CG. Age and gender variations in age-related macular degeneration prevalence in populations of European ancestry: a meta-analysis. Ophthalmology. 2012;119:571–80.
Shin JY, Kwon KY, Byeon SH. Association between choroidal thickness and the response to intravitreal ranibizumab injection in age-related macular degeneration. Acta Ophthalmol. 2015;93:524–32.
Chatziralli I, Kabanarou SA, Parikakis E, Chatzirallis A, Xirou T, Mitropoulos P. Risk factors for central serous chorioretinopathy: multivariate approach in a case–control study. Curr Eye Res. 2017;42:1069–73.
Spaide RF, Campeas L, Haas A, Yannuzzi LA, Fisher YL, Guyer DR, et al. Central serous chorioretinopathy in younger and older adults. Ophthalmology. 1996;103:2070–2079. discussion 2079–80
Matet A, Dariuch A, Zola M, Behar Cohen F. Risk factors for recurrences of central serous chorioretinopathy Retina 2018 Jul; 38(7):1403-1414
Kitzmann AS, Pulido JS, Diehl NN, Hodge DO, Burke JP. The incidence of central serous chorioretinopathy in Olmsted County, Minnesota, 1980–2002. Ophthalmology. 2008;115:169–73.
Tsai DC, Chen SJ, Huang CC, Chou P, Chung CM, Huang PH, et al. Epidemiology of idiopathic central serous chorioretinopathy in Taiwan, 2001–2006: a population-based study. PLoS ONE. 2013;8:e66858.
Kuroda S, Ikuno Y, Yasuno Y, Nakai K, Usui S, Sawa M, et al. Choroidal thickness in central serous chorioretinopathy. Retina. 2013;33:302–8.
Yang L, Jonas JB, Wei W. Optical coherence tomography-assisted enhanced depth imaging of central serous chorioretinopathy. Invest Ophthalmol Vis Sci. 2013;54:4659–65.
Mitarai K, Gomi F, Tano Y. Three-dimensional optical coherence tomographic findings in central serous chorioretinopathy. Graefe’s Arch Clin Exp Ophthalmol. 2006;244:1415–20.
Landa G, Barnett JA, Garcia PM, Tai KW, Rosen RB. Quantitative and qualitative spectral domain optical coherence tomography analysis of subretinal deposits in patients with acute central serous retinopathy. Ophthalmologica. 2013;230:62–68.
Ahlers C, Geitzenauer W, Stock G, Golbaz I, Schmidt-Erfurth U, Prunte C. Alterations of intraretinal layers in acute central serous chorioretinopathy. Acta Ophthalmol. 2009;87:511–6.
Kunavisarut P, Pathanapitoon K, van Schooneveld M, Rothova A. Chronic central serous chorioretinopathy associated with serous retinal detachment in a series of Asian patients. Ocul Immunol Inflamm. 2009;17:269–77.
Patel PJ, Foster PJ, Grossi CM, Keane PA, Ko F, Lotery A, et al. Spectral-domain optical coherence tomography imaging in 67 321 adults: associations with macular thickness in the UK Biobank Study. Ophthalmology. 2016;123:829–40.
von Hanno T, Lade AC, Mathiesen EB, Peto T, Njolstad I, Bertelsen G. Macular thickness in healthy eyes of adults (N = 4508) and relation to sex, age and refraction: the Tromso Eye Study (2007–2008). Acta Ophthalmol. 2017;95:262–9.
Maruko I, Iida T, Sugano Y, Ojima A, Sekiryu T. Subfoveal choroidal thickness in fellow eyes of patients with central serous chorioretinopathy. Retina. 2011;31:1603–08.
Smith W, Mitchell P, Wang JJ. Gender, oestrogen, hormone replacement and age-related macular degeneration: results from the Blue Mountains Eye Study. Aust NZ J Ophthalmol. 1997;25 Suppl 1:S13–15.
You QS, Xu L, Yang H, Li YB, Wang S, Wang JD, et al. Five-year incidence of age-related macular degeneration: the Beijing Eye Study. Ophthalmology. 2012;119:2519–25.
Srinivasan S, Swaminathan G, Kulothungan V, Raman R, Sharma T. Prevalence and the risk factors for visual impairment in age-related macular degeneration. Eye (Lond). 2017;31:846–55.
Brandl C, Breinlich V, Stark KJ, Enzinger S, Assenmacher M, Olden M, et al. Features of age-related macular degeneration in the general adults and their dependency on age, sex, and smoking: results from the German KORA Study. PLoS ONE. 2016;11:e0167181.
Mehlsen J, Erlandsen M, Poulsen PL, Bek T. Identification of independent risk factors for the development of diabetic retinopathy requiring treatment. Acta Ophthalmol. 2011;89:515–21.
Author contributions
All authors were involved in the design of the project (or the acquisition of the data), drafting of the article and final approval of the version to be published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hanumunthadu, D., Van Dijk, E.H.C., Gangakhedkar, S. et al. Gender variation in central serous chorioretinopathy. Eye 32, 1703–1709 (2018). https://doi.org/10.1038/s41433-018-0163-7
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-018-0163-7
This article is cited by
-
Gender differences in central serous chorioretinopathy based on the new multimodal imaging classification
Eye (2024)
-
Automatic Segmentation of Hyperreflective Foci in OCT Images Based on Lightweight DBR Network
Journal of Digital Imaging (2023)
-
Distinct characteristics of central serous chorioretinopathy according to gender
Scientific Reports (2022)
-
Pre- and post-operative differences between genders in idiopathic macular holes
BMC Ophthalmology (2020)
-
Gender-Medizin in der Augenheilkunde
Der Ophthalmologe (2020)