Abstract
Aim
Meibomian gland dysfunction (MGD) is one of the most common disorders in ophthalmology. The aim of this study was to evaluate the use of this in vivo confocal microscopy (IVCM)-MGD description to classify patients affected by clinical MGD and measure the correlation with standard clinical criteria and subjective symptoms.
Methods
One hundred eyes of 100 patients suffering from MGD and 15 eyes of normal subjects were included. A comprehensive evaluation with the ocular surface disease index (OSDI), Schirmer test, tear break-up time (TBUT), tear osmolarity, Oxford score, Meibomian gland expression, palpebral IVCM, and meibography was performed. Then each patient was classified using a new IVCM classification: type 0 for normality, type 1 for meibum obstruction, type 2 for inflammation, and type 3 for fibrosis.
Results
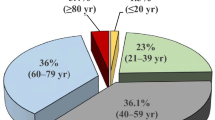
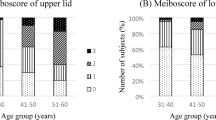
The mean age of patients was 52 ± 20 years old, the OSDI was 38 ± 23, the BUT 5 ± 2.6 s, the Schirmer test 13 ± 7 mm, tear osmolarity 300 ± 11 osmol/L, the Oxford score 0.5 ± 0.6, the meibum expression score 1.7 ± 1.02, and the meibography score 1.3 ± 0.9. The IVCM MG classification of the 15 normal subjects was 0. For MGD patients, 29% were in type 1, 40% were type 2, and 31% were type 3. The patients in IVCM MG type 2 had a higher OSDI (p = 0.001) compared with the other types. There was a strong correlation between the IVCM score and the meibography score (r = 0.71 p < 0.0001).
Conclusion
This new IVCM classification provided a practical pathophysiological system for MGD. By giving objective criteria, this IVCM classification may help advance the understanding of patients’ symptoms and enhance treatment effectiveness in MGD.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
25 February 2019
Since the online publication of the above article, the authors have noted an error with the name of the co-author Dr Liang (Last name) Hong (first name).
References
Schaumberg DA, Nichols JJ, Papas EB, et al. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for MGD. Invest Ophthalomol Vis Sci. 2011;52:1994–2005.
Hom MM, Martinson JR, Knapp LL, et al. Prevalence of meibomian gland dysfunction. Optom Vis Sci. 1990;67:710–2.
Molinari JF, Stanek S. Meibomian gland status comparison between active duty personnel and U.S. veterans. Mil Med. 2000;165:591–3.
McCulley JP, Shine WE. Meibomian gland function and the tear lipid layer. Ocul Surf. 2003;1:97–106.
Baudouin C. Revisiting meibomian gland dysfunction. J Fr Ophtalmol. 2014;37:757–62.
Ban Y, Shimazaki-Den S, Tsubota K, et al. Morphological evaluation of Meibomian glands using noncontact infrared meibography. Ocul Surf. 2013;11:47–53.
Geerling G, Baudouin C, Aragona P, et al. Emerging strategies for the diagnosis and treatment of meibomian gland dysfunction: Proceedings of the OCEAN group meeting. Ocul Surf. 2017;172:179–92.
Eom Y, Choi KE, Kang SY, et al. Comparison of meibomian gland loss and expressed meibum grade between the upper and lower eyelids in patients with obstructive meibomian gland dysfunction cornea. Cornea. 2014;33:448–52.
Pult H, Riede-Pult BH. Non-contact meibography: keep it simple but effective. Cont Lens Anterior Eye. 2011;35:77–80.
Srinivasan S, Menzies K, Sorbara L, et al. Infrared imaging of meibomian gland structure using a novel keratograph. Optom Vis Sci. 2012;89:788–94.
Yoo YS, Na KS, Kim DY, et al. Morphological evaluation for diagnosis of dry eye related to meibomian gland dysfunction. Exp Eye Res. 2017;10:72–7.
Liang Q, Pan Z, Zhou M, et al. Evaluation of optical coherence tomography meibography in patients with obstructive meibomian gland dysfunction. Cornea. 2015;34:1193–9.
Wolffsohn JS. Arita R2, Chalmers R. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15:539–74.
Randon M, Liang H, Abbas R, et al. A new classification for meibomian gland diseases with in vivo confocal microscopy. J Fr Ophtalmol. 2016;39:239–47.
Shimazaki J, Goto E, Ono M, et al. Meibomian gland dysfunction in patients with Sjögren syndrome. Ophthalmology. 1998;105:1485–8.
Villani E, Beretta S, De Capitani M, et al. In vivo confocal microscopy of meibomian glands in Sjogren’s Syndrome. Invest Ophthalomol Vis Sci. 2011;52:933–9.
Baudouin C, Messmer EM, Aragona P, et al. Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. Br J Opthalmol. 2016;100:300–6.
Kobayashi A, Yoshita T, Sugiyama K. In vivo findings of the bulbar/palpebral conjunctiva and presumed meibomian glands by Laser scanning confocal microscopy. Cornea. 2005;24:985–8.
Agnifili L, Fasanella V, Costagliola C, et al. In vivo confocal microscopy of meibomian glands in glaucoma. Br J Opthalmol. 2013;97:343–9.
Ban Y, Ogawa Y, Ibrahim OM, et al. Morphologic evaluation of meibomian glands in chronic graft versus-host disease using in vivo laser confocal microscopy. Mol Vis. 2011;17:2533–43.
Ibrahim OM, Matsumoto Y, Dogru M, et al. In vivo confocal microscopy evaluation of meibomian gland dysfunction in atopic-keratoconjunctivitis patients. Ophthalmology. 2012;119:1961–8.
Villani E, Ceresara G, Beretta S, et al. In vivo confocal microscopy of meibomian glands in contact lens wearers. Invest Ophthalomol Vis Sci. 2011;52:5215–9.
Messmer EM, Torres Suarez E, Mackert MI, et al. In vivo confocal microscopy in blepharitis. Klin Monbl Augenheikd. 2005;222:894–900.
Randon M, Liang H, El Hamdaoui M, et al. In vivo confocal microscopy as a novel and reliable tool for the diagnosis of Demodex eyelid infestation. Br J Ophthalmol. 2015;99:336–41.
Villani E, Canton V, Magnani F, et al. The aging meibomian gland: an in vivo confocal study. Invest Ophthalmol Vis Sci. 2013;54:4735–40.
Matsumoto Y, Sato EA, Ibrahim OM, et al. The application of in vivo laser confocal microscopy to the diagnosis and evaluation of meibomian gland dysfunction. Mol Vis. 2008;14:1263–71.
Finis D, Ackermann P, Pischel N, et al. Evaluation of meibomian gland dysfunction and local distribution of meibomian gland atrophy by non-contact infrared meibography. Curr Eye Res. 2015;40:982–9.
Gerling G, Tauber J, Baudouin C, et al. The international Workshop on Meibomian Gland Dysfunction: report of the subcommittee on management and treatment of MGD. Invest Ophthalmol Vis Sci. 2011;52:2050–64.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Randon, M., Aragno, V., Abbas, R. et al. In vivo confocal microscopy classification in the diagnosis of meibomian gland dysfunction. Eye 33, 754–760 (2019). https://doi.org/10.1038/s41433-018-0307-9
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-018-0307-9
This article is cited by
-
In Vivo Confocal Microscopy for Automated Detection of Meibomian Gland Dysfunction: A Study Based on Deep Convolutional Neural Networks
Journal of Imaging Informatics in Medicine (2025)
-
Loose suture-related ocular surface inflammation and activation of conjunctiva-associated lymphoid tissue in patients after keratoplasty
Scientific Reports (2024)
-
Dry Eye Disease Associated with Meibomian Gland Dysfunction: Focus on Tear Film Characteristics and the Therapeutic Landscape
Ophthalmology and Therapy (2023)
-
Meibomian Gland Dysfunction Clinical Practice Guidelines
Japanese Journal of Ophthalmology (2023)
-
Imaging of meibomian glands: from bench to bedside and back
Eye (2019)