Abstract
Background/Objectives
To analyze the surgical and sensory outcomes of intermittent exotropia according to refractive errors and the factors associated with surgical success.
Subjects/Methods
A total of 326 children were divided into three groups according to preoperative refractive error; hyperopic eyes with SE ≥+2D (hyperopic group), eyes with SE between −1D and +2D (emmetropic group), and myopic eyes with SE ≤−1D (myopic group). The surgical outcomes and the sensory outcomes measured by near and distant stereoacuity were compared among the three groups.
Results
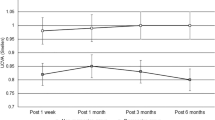
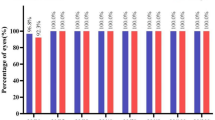
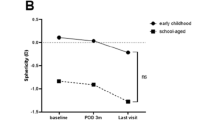
The surgical success rate in hyperopic group was significantly lower compared to myopic group at last follow-up (P = 0.012). Preoperative near stereopsis was not different among three groups, however, the distance stereopsis was significantly deteriorated in the hyperopic group compared to the other two groups (Titmus; P = 0.168, FD2; P < 0.001, DR; P = 0.048). There was postoperative improvement in both near and distant stereopsis in all three groups (Titmus; P = 0.009, FD2; P = 0.021, DR; P = 0.036) and no significant difference was found in the postoperative distant stereopsis among the three groups.
Conclusions
Preoperative refractive error is a prognostic factor of surgical success in patients with intermittent exotropia. Patients with hyperopia achieved less favorable surgical outcome compared to myopic patients. The preoperative distant stereoacuity was decreased in hyperopic patients compared to myopic patients, which eventually improved after surgery and showed no significant difference at postoperative measurements.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Rutstein RP, Corliss DA. The clinical course of intermittent exotropia. Optom Vis Sci. 2003;80:644–9.
Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG. Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J AAPOS. 2009;13:4–7.
Hardesty HH, Boynton JR, Keenan JP. Treatment of intermittent exotropia. Arch Ophthalmol. 1978;96:268–74.
Richard JM, Parks MM. Intermittent exotropia. Surgical results in different age groups. Ophthalmology. 1983;90:1172–7.
Clarke WN, Noel LP. Surgical results in intermittent exotropia. Can J Ophthalmol. 1981;16:66–9.
Tang SM, Chan RY, Bin Lin S, Rong SS, Lau HH, Lau WW, et al. Refractive errors and concomitant strabismus: a systematic review and meta-analysis. Sci Rep. 2016;6:35177.
Zhu H, Yu JJ, Yu RB, Ding H, Bai J, Chen J, Liu H. Association between childhood strabismus and refractive error in Chinese preschool children. PLoS ONE. 2015;10:e0120720.
Wen G, Tarczy-Hornoch K, McKean-Cowdin R, Cotter SA, Borchert M, Lin J, et al. Prevalence of myopia, hyperopia, and astigmatism in non-Hispanic white and Asian children: multi-ethnic pediatric eye disease study. Ophthalmology. 2013;120:2109–16.
BURIAN HM, SPIVEY BE. The surgical management of exodeviations. Trans Am Ophthalmol Soc. 1964;62:276–306.
Gezer A, Sezen F, Nasri N, Gözüm N. Factors influencing the outcome of strabismus surgery in patients with exotropia. J AAPOS. 2004;8:56–60.
Oh JY, Hwang JM. Survival analysis of 365 patients with exotropia after surgery. Eye (Lond). 2006;20:1268–72.
Chia A, Seenyen L, Long QB. Surgical experiences with two-muscle surgery for the treatment of intermittent exotropia. J AAPOS. 2006;10:206–11.
Stoller SH, Simon JW, Lininger LL. Bilateral lateral rectus recession for exotropia: a survival analysis. J Pediatr Ophthalmol Strabismus. 1994;31:89–92.
Kulp MT, Ying GS, Huang J, Maguire M, Quinn G, Ciner EB, et al. Associations between hyperopia and other vision and refractive error characteristics. Optom Vis Sci. 2014;91:383–9.
Colburn JD, Morrison DG, Estes RL, Li C, Lu P, Donahue SP. Longitudinal follow-up of hypermetropic children identified during preschool vision screening. J AAPOS. 2010;14:211–5.
Yang M, Chen J, Shen T, Kang Y, Deng D, Lin X, et al. Clinical characteristics and surgical outcomes in patients with intermittent exotropia: a large sample study in South China. Medicine (Baltimore). 2016;95:e2590.
Lim SH, Hwang BS, Kim MM. Prognostic factors for recurrence after bilateral rectus recession procedure in patients with intermittent exotropia. Eye (Lond). 2012;26:846–52.
Kim MK, Kim US, Cho MJ, Baek SH. Hyperopic refractive errors as a prognostic factor in intermittent exotropia surgery. Eye (Lond). 2015;29:1555–60.
Zou D, Casafina C, Whiteman A, Jain S. Predictors of surgical success in patients with intermittent exotropia. J AAPOS. 2017;21:15–8.
Scattergood KD, Brown MH, Guyton DL. Artifacts introduced by spectacle lenses in the measurement of strabismic deviations. Am J Ophthalmol. 1983;96:439–48.
Von Noorden GK, Campos EC. Binocular vision and ocular motility: theory and management of strabismus. 6th ed. St. Louis: Mosby; 2002.
Iacobucci IL, Archer SM, Giles CL. Children with exotropia responsive to spectacle correction of hyperopia. Am J Ophthalmol. 1993;116:79–83.
Chung SA, Kim IS, Kim WK, Lee JB. Changes in exodeviation following hyperopic correction in patients with intermittent exotropia. J Pediatr Ophthalmol Strabismus. 2011;48:278–84.
Adams WE, Leske DA, Hatt SR, Mohney BG, Birch EE, Weakley DR Jr, et al. Improvement in distance stereoacuity following surgery for intermittent exotropia. J AAPOS. 2008;12:141–4.
Holmes JM, Leske DA, Hatt SR, Brodsky MC, Mohney BG. Stability of near stereoacuity in childhood intermittent exotropia. J AAPOS. 2011;15:462–7.
Stathacopoulos RA, Rosenbaum AL, Zanoni D, Stager DR, McCall LC, Ziffer AJ, et al. Distance stereoacuity. Assessing control in intermittent exotropia. Ophthalmology. 1993;100:495–500.
O’Neal TD, Rosenbaum AL, Stathacopoulos RA. Distance stereo acuity improvement in intermittent exotropic patients following strabismus surgery. J Pediatr Ophthalmol Strabismus. 1995;32:353–7. discussion 8
Yildirim C, Mutlu FM, Chen Y, Altinsoy HI. Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol. 1999;128:222–30.
Holmes JM, Birch EE, Leske DA, Fu VL, Mohney BG. New tests of distance stereoacuity and their role in evaluating intermittent exotropia. Ophthalmology. 2007;114:1215–20.
Simons K. Stereoacuity norms in young children. Arch Ophthalmol. 1981;99:439–45.
Fox R, Patterson R, Francis EL. Stereoacuity in young children. Invest Ophthalmol Vis Sci. 1986;27:598–600.
Acknowledgements
We thank all the patients for participating in this study. All authors have completed and submitted the ICMJE form for disclosure of potential conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ahn, Y.J., Park, Y.Y., Chung, Y.W. et al. Surgical and sensory outcomes in patients with intermittent exotropia according to preoperative refractive error. Eye 33, 1314–1320 (2019). https://doi.org/10.1038/s41433-019-0419-x
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0419-x