Abstract
Objectives
To assess the prevalence of and risk factors for refractive error (RE) in Han and Mongolian adults aged 40–80 years in Inner Mongolia in China and to identify ethnic differences in RE between these populations.
Methods
Our cross-sectional study is part of the China National Health Survey (CNHS). The age-adjusted prevalence of RE in Han and Mongolian adults aged 40–80 in Inner Mongolia were compared. A multivariable logistic regression model was used to identify risk factors.
Results
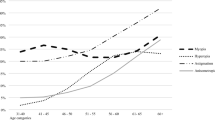
Among 2090 people, the age-adjusted prevalence of myopia (SE < −0.5D), hyperopia (SE > 0.5D), high myopia (SE < −6.0D) and astigmatism (cylinder ≥ 0.5D) were 29.4% (95% confidence interval (CI), 27.4–31.3%), 28.4% (95% CI, 26.4–30.5%), 3.6% (95% CI, 2.8–4.4%) and 65.9% (95% CI, 63.9–67.9%), respectively. The age-adjusted prevalence of myopia in the Han population was higher than that in the Mongolian population (31.8% vs. 23.0%, p < 0.001), but the prevalence of hyperopia was lower (25.8% vs. 35.3%, p = 0.002). In the multivariable logistic regression, ethnicity was associated with myopia (p = 0.001) and hyperopia (p = 0.001). Myopia was also associated with age, time spent in rural areas (p < 0.001) and middle/high school and undergraduate/graduate education levels (p = 0.027 and p < 0.001, respectively, compared with lower education levels). Additionally, age, height (p = 0.015) and pterygium (p = 0.014) were associated with hyperopia.
Conclusions
Ethnicity is closely related to RE in Inner Mongolia in mainland China. Our study investigates differences in prevalence of and risk factors for RE between the Han and Mongolian populations, which could not be explained by differences in the risk factors investigated in this study.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Naidoo KS, Leasher J, Bourne RR, Flaxman SR, Jonas JB, Keeffe J, et al. Global vision impairment and blindness due to uncorrected refractive error, 1990–2010. Optom Vis Sci. 2016;93:227–34.
Vitale S, Cotch MF, Sperduto RD. Prevalence of visual impairment in the United States. JAMA. 2006;295:2158–63.
Pizzarello L, Abiose A, Ffytche T, Duerksen R, Thulasiraj R, Taylor H, et al. VISION 2020: the right to sight: a global initiative to eliminate avoidable blindness. Arch Ophthalmol. 2004;122:615–20.
Lougheed T. Myopia: the evidence for environmental factors. Environ Health Perspect. 2014;122:A12–A19.
Ramamurthy D, Chua SYL, Saw SM. A review of environmental risk factors for myopia during early life, childhood and adolescence. Clin Exp Optom. 2015;98:497–506.
Hornbeak DM, Young TL. Myopia genetics: a review of current research and emerging trends. Curr Opin Ophthalmol. 2009;20:356–62.
Pan CW, Ramamurthy D, Saw SM. Worldwide prevalence and risk factors for myopia. Ophthalmic Physiol Opt. 2012;32:3–16.
Wojciechowski R. Nature and nurture: the complex genetics of myopia and refractive error. Clin Genet. 2011;79:301–20.
Tabulation on the 2010 population census of the People’s Republic of China. http://www.stats.gov.cn/tjsj/pcsj/rkpc/6rp/indexch.htm. 2010.
Bai H, Guo X, Narisu N, Lan T, Wu Q, Xing Y, et al. Whole-genome sequencing of 175 Mongolians uncovers population-specific genetic architecture and gene flow throughout North and East Asia. Nat Genet. 2018;50:1696–704.
Li G, Wang H, Wang K, Wang W, Dong F, Qian Y, et al. Prevalence, awareness, treatment, control and risk factors related to hypertension among urban adults in Inner Mongolia 2014: differences between Mongolian and Han populations. BMC Public Health. 2016;16:294.
Bai Z, Yang X, Han X, Dong P, Liu A. Comparison between coronary plaque 64-slice spiral CT characteristics and risk factors of coronary artery disease patients in Chinese Han population and Mongolian. Pak J Med Sci. 2013;29:933–7.
Li N, Wang H, Yan Z, Yao X, Hong J, Zhou L. Ethnic disparities in the clustering of risk factors for cardiovascular disease among the Kazakh, Uygur, Mongolian and Han populations of Xinjiang: a cross-sectional study. BMC Public Health. 2012;12:499.
Huriletemuer Zhang C, Zhao S, Wang D, Wang Z, Jiang M, et al. An epidemiological study of stroke and its sub-types in the over 55 Mongolian and Han populations in a pastoral area of inner Mongolia. Int J Stroke. 2011;6:468.
Jiang XY, Chang FH, Bai TY, Lv XL, Wang MJ. Susceptibility of lung cancer with polymorphisms of CYP1A1, GSTM1, GSTM3, GSTT1 and GSTP1 genotypes in the population of Inner Mongolia region. Asian Pac J Cancer Prev. 2014;15:5207–14.
Bai H, Liu H, Suyalatu S, Guo X, Chu S, Chen Y, et al. Association analysis of genetic variants with type 2 diabetes in a Mongolian population in China. J Diabetes Res. 2015;2015:613236.
Qin L, Zhao P, Liu Z, Chang P. Associations SELE gene haplotype variant and hypertension in Mongolian and Han populations. Intern Med. 2015;54:287–93.
Komatsu F, Kagawa Y, Kawabata T, Kaneko Y, Purvee B, Otgon J, et al. Dietary habits of Mongolian people, and their influence on lifestyle-related diseases and early aging. Curr Aging Sci. 2008;1:84–100.
Wickremasinghe S, Foster PJ, Uranchimeg D, Lee PS, Devereux JG, Alsbirk PH, et al. Ocular biometry and refraction in Mongolian adults. Invest Ophthalmol Vis Sci. 2004;45:776–83.
Zhao HX, Zhang L, Guan WY. Difference in normal corneal thickness and curvature between Mongolian and Han nationalities. Int J Ophthalmol. 2015;8:399–402.
He H, Pan L, Pa L, Cui Z, Ren X, Wang D et al. Data resource profile: the china national health survey (CNHS). Int J Epidemiol. 2018. https://doi.org/10.1093/ije/dyy1151.
Huang CY, Hou CH, Lin KK, Lee JS, Yang ML. Relationship of lifestyle and body stature growth with the development of myopia and axial length elongation in Taiwanese elementary school children. Indian J Ophthalmol. 2014;62:865–9.
Northstone K, Guggenheim JA, Howe LD, Tilling K, Paternoster L, Kemp JP, et al. Body stature growth trajectories during childhood and the development of myopia. Ophthalmology. 2013;120:1064–73.
Guo Y, Liu LJ, Xu L, Lv YY, Tang P, Feng Y, et al. Outdoor activity and myopia among primary students in rural and urban regions of Beijing. Ophthalmology. 2013;120:277–83.
Tan CS, Chan YH, Wong TY, Gazzard G, Niti M, Ng TP, et al. Prevalence and risk factors for refractive errors and ocular biometry parameters in an elderly Asian population: the Singapore Longitudinal Aging Study (SLAS). Eye. 2011;25:1294–301.
Saw SM, Chua WH, Hong CY, Wu HM, Chia KS, Stone RA, et al. Height and its relationship to refraction and biometry parameters in Singapore Chinese children. Invest Ophthalmol Vis Sci. 2002;43:1408–13.
Saw SM, Chia KS, Lindstrom JM, Tan DT, Stone RA. Childhood myopia and parental smoking. Br J Ophthalmol. 2004;88:934–7.
Stone RA, Wilson LB, Ying GS, Liu C, Criss JS, Orlow J, et al. Associations between childhood refraction and parental smoking. Invest Ophthalmol Vis Sci. 2006;47:4277–87.
Rahi JS, Cumberland PM, Peckham CS. Myopia over the lifecourse: prevalence and early life influences in the 1958 British birth cohort. Ophthalmology. 2011;118:797–804.
Pan CW, Zheng YF, Anuar AR, Chew M, Gazzard G, Aung T, et al. Prevalence of refractive errors in a multiethnic Asian population: the Singapore epidemiology of eye disease study. Invest Ophthalmol Vis Sci. 2013;54:2590–8.
Bai H, Guo X, Zhang D, Narisu N, Bu J, Jirimutu J, et al. The genome of a Mongolian individual reveals the genetic imprints of Mongolians on modern human populations. Genome Biol Evol. 2014;6:3122–36.
Hu W, Tong WJ, Liu YB, Teng GX, Zhang YH. Correlation between alcohol intake and smoking and hypertension in Mongolian people. Chin J Public Health. 2006;22:2.
Muge K, Xi W, Degang Z, Shangli S. Rangeland nomadic culture of the Mongolian nationality (I)-origin, language and religion of the Mongolian nationality. Grassl Turf. 2013;33:80–4.
Jiliang X. The research on fertility intention national differences and its influencing factors: from the comparison between the Han nationality and the Mongolian nationality. Popul J. 2015;37:25–35.
Zhang Y, Zhang Z, Zhang J, He S, Liu Y, Zhang Y, et al. A cohort study on the relationship between different hip circumference levels and the events of cerebrovascular diseases and deaths in Mongolian peasants and herdsmen. Chin J Dis Control Prev. 2014;18:290–5.
Lin Z, Buren B, Jin X, Hasen G, Xiao J. Developments of height and weight in Mongolian students aged 6 to 18 years. Chin J Public Health. 2012;28:102–4.
Zheng L, Han Z, Lu S, Li Y, Shuyuan L. Morphological traits in peoples of Mongolian nationality of the Hulunbuir league, Inner Mongolia, China. Anthropol Anz. 2002;60:175–85.
Papadopoulos PA, Papadopoulos AP. Current management of presbyopia. Middle East Afr J Ophthalmol. 2014;21:10–7.
Wong TY, Foster PJ, Hee J, Ng TP, Tielsch JM, Chew SJ, et al. Prevalence and risk factors for refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41:2486–94.
Saw SM, Chan YH, Wong WL, Shankar A, Sandar M, Aung T, et al. Prevalence and risk factors for refractive errors in the Singapore Malay Eye Survey. Ophthalmology. 2008;115:1713–9.
Sawada A, Tomidokoro A, Araie M, Iwase A, Yamamoto T, Tajimi Study Group. Refractive errors in an elderly Japanese population: the Tajimi study. Ophthalmology. 2008;115:363–70.
Ip JM, Rose KA, Morgan IG, Burlutsky G, Mitchell P. Myopia and the urban environment: findings in a sample of 12-year-old Australian school children. Invest Ophthalmol Vis Sci. 2008;49:3858–63.
Morgan IG, Ohno-Matsui K, Saw SM. Myopia. Lancet. 2012;379:1739–48.
Verhoeven VJ, Buitendijk GH, Rivadeneira F, Uitterlinden AG, Vingerling JR.Consortium for Refractive Error and Myopia (CREAM) et al. Education influences the role of genetics in myopia. Eur J Epidemiol. 2013;28:973–80.
Dirani M, Shekar SN, Baird PN. The role of educational attainment in refraction: the Genes in Myopia (GEM) twin study. Invest Ophthalmol Vis Sci. 2008;49:534–8.
Jin JX, Hua WJ, Jiang X, Wu XY, Yang JW, Gao GP, et al. Effect of outdoor activity on myopia onset and progression in school-aged children in northeast China: the Sujiatun Eye Care Study. BMC Ophthalmol. 2015;15:73.
Sherwin JC, Hewitt AW, Coroneo MT, Kearns LS, Griffiths LR, Mackey DA. The association between time spent outdoors and myopia using a novel biomarker of outdoor light exposure. Invest Ophthalmol Vis Sci. 2012;53:4363–70.
McCarthy CS, Megaw P, Devadas M, Morgan IG. Dopaminergic agents affect the ability of brief periods of normal vision to prevent form-deprivation myopia. Exp Eye Res. 2007;84:100–7.
He M, Huang W, Li Y, Zheng Y, Yin Q, Foster PJ. Refractive error and biometry in older Chinese adults: the Liwan eye study. Invest Ophthalmol Vis Sci. 2009;50:5130–6.
American Academy of Ophthalmology. Clinical optics, 2016–7. American Academy of Ophthalmology: San Francisco; 2016.
Shiroma H, Higa A, Sawaguchi S, Iwase A, Tomidokoro A, Amano S, et al. Prevalence and risk factors of pterygium in a southwestern island of Japan: the Kumejima Study. Am J Ophthalmol. 2009;148:766–71.
Lim CY, Kim SH, Chuck RS, Lee JK, Park CY. Risk factors for pterygium in Korea: the Korean National Health and Nutrition Examination Survey V, 2010–2012. Medicine. 2015;94:e1258.
Linke SJ, Steinberg J, Eddy MT, Richard G, Katz T. Relationship between minimum corneal thickness and refractive state, keratometry, age, sex, and left or right eye in refractive surgery candidates. J Cataract Refract Surg. 2011;37:2175–80.
Jonas JB, Xu L. Histological changes of high axial myopia. Eye. 2014;28:113–7.
Mimura T, Usui T, Yamagami S, Funatsu H, Noma H, Toyono T, et al. Relationship between conjunctivochalasis and refractive error. Eye Contact Lens. 2011;37:71–8.
Chen T, Ding L, Shan G, Ke L, Ma J, Zhong Y. Prevalence and racial differences in pterygium: a cross-sectional study in Han and Uygur adults in Xinjiang, China. Invest Ophthalmol Vis Sci. 2015;56:1109–17.
Acknowledgements
We thank Guoju Li, Ke Wang, Fen Dong, Haiying Gong, Guodong Xu, Yanlong Li, Bin Wang, and Guangjin Zhu for their assistance in data collection. This study was supported by the National Science and Technology Pillar Program during the Twelfth Five-Year Plan Period sponsored by the Ministry of Science and Technology of China (Grant 2012BAI37B02). The authors alone are responsible for the content of the paper.
Funding
National Science and Technology Pillar Program during the Twelfth Five-Year Plan Period sponsored by the Ministry of Science and Technology of China (Grant 2012BAI37B02)
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, M., Ma, J., Pan, L. et al. Prevalence of and risk factors for refractive error: a cross-sectional study in Han and Mongolian adults aged 40–80 years in Inner Mongolia, China. Eye 33, 1722–1732 (2019). https://doi.org/10.1038/s41433-019-0469-0
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0469-0
This article is cited by
-
High prevalence of refractive errors in an elderly population; a public health issue
BMC Ophthalmology (2023)
-
Corneal characteristics of Mongolian population with type 2 diabetic peripheral neuropathy in inner Mongolia, China: an assessment using corneal confocal microscopy
BMC Ophthalmology (2023)
-
Prevalence and risk factors of refractive error in Qinghai, China: a cross-sectional study in Han and Tibetan adults in Xining and surrounding areas
BMC Ophthalmology (2021)