Abstract
Objectives
To investigate risk factors for retinopathy of prematurity (ROP) in a newly established ROP screening and management programme in Rwanda, Africa.
Methods
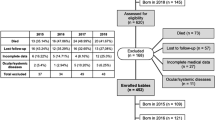
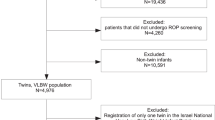
In this multi-centre prospective study 795/2222 (36%) babies fulfilled the inclusion criteria (gestational age (GA) < 35 weeks or birth weight (BW) < 1800 g or unstable clinical course), 424 (53%) of whom were screened for ROP. 270 died before the first screening. ROP and treatment-warranted ROP were classified using the revised International Classification of ROP (2005). Data on maternal and perinatal risk factors were collected from daily neonatal notes.
Results
31 babies (7.3%, CI 5.0–10.2) developed any ROP, 13 of whom (41.9%, CI 24.5–60.9) required treatment. ROP was seen in six neonates with GA > 30 weeks and BW > 1500 g, one of whom required treatment. In univariate analysis the following were associated with any ROP: increasing number of days on supplemental oxygen (OR 2.1, CI 1.5–3.0, P < 0.001), low GA (OR 3.4, CI 1.8–6.4, P < 0.001), low BW (OR 2.3, CI 1.5–3.4, P < 0.001), at least one episode of hyperglycaemia ≥ 150 mg/dl (OR 6.6, CI 2.0–21.5, P < 0.001), blood transfusion (OR 3.5, CI 1.6–7.4, P < 0.001) or sepsis (OR 3.2, CI 1.2–8.6, P = 0.01). In multivariate analysis longer exposure to supplemental oxygen (OR 2.1, CI 1.2–3.6, P = 0.01) and hyperglycaemia (OR 3.5, CI 1.0–12.4, P = 0.05) remained significant.
Conclusions
ROP has become an emerging health problem in Rwanda, requiring programmes for screening and treatment. ROP screening is indicated beyond the 2013 American Academy guidelines. Improved quality of neonatal care, particularly oxygen delivery and monitoring is needed.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
Change history
04 September 2019
A Correction to this paper has been published: https://doi.org/10.1038/s41433-019-0561-5
References
Chan-Ling T, Gole GA, Quinn GE, Adamson SJ, Darlow BA. Pathophysiology, screening and treatment of ROP: a multi-disciplinary perspective. Prog Retin Eye Res. 2018;62:77–119.
Gilbert C, Rahi J, Eckstein M, O’Sullivan J, Foster A. Retinopathy of prematurity in middle-income countries. Lancet. 1997;350:12–4.
Blencowe H, Lawn JE, Vazquez T, Fielder A, Gilbert C. Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pedia Res. 2013;74(Suppl 1):35–49.
Quinn G, Gilbert C, Darlow B, Zin A. Retinopathy of prematurity: an epidemic in the making. Chin Med J. 2010;123:2929–37.
Gilbert C, Fielder A, Gordillo L, Guinn G, Semiglia R, Zin A, et al. Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate and high levels of development: implications for screening programs. Pediatrics. 2005;115:e518–e25.
Gilbert CE. Screening for retinopathy of prematurity: does one size fit all? Arch Dis Child Fetal Neonatal Ed. 2016;101:F280–1.
Delport S, Swanepoel J, Odendaal P, Roux P. Incidence of retinopathy of prematurity in very low birth weight infants born at Kalafong Hospital, Pretoria. S Afr Med J. 2002;92:986–90.
Kirsten G, Van Zyl J, Le Grange M, Ancker E, Van Zyl F. The outcome at 12 months of very-low-birth-weight infants ventilated at Tygerberg Hospital. S Afr Med J. 1995;85:649–54.
Keraan Q, Tinley C, Horn A, Pollock T, Steffen J, Joolay Y. Retinopathy of prematurity in a cohort of neonates at Groote Schuur Hospital, Cape Town, South Africa. S Afr Med J. 2016;107:64–9.
Van der Merwe SK, Freeman N, Bekker A, Harvey J, Smith J. Prevalence of and risk factors for retinopathy of prematurity in a cohort of preterm infants treated exclusively with non-invasive ventilation in the first week after birth. S Afr Med J. 2013;103:96–100.
Fajolu IB, Rotimi-Samuel A, Aribaba OT, Musa KO, Akinsola FB, Ezeaka VC, et al. Retinopathy of prematurity and associated factors in Lagos, Nigeria. Paediatr Int Child Health. 2015;35:324–8.
Mora JS, Waite C, Gilbert CE, Breidenstein B, Sloper JJ. A worldwide survey of retinopathy of prematurity screening. Br J Ophthalmol. 2018;102:9–13.
Ntigurirwa P, Mellor K, Langer D, Evans M, Robertson E, Tuyisenge L, et al. A health partnership to reduce neonatal mortality in four hospitals in Rwanda. Glob Health. 2017;13:28.
International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity revisited. Arch Ophthalmol. 2005;123:991–9.
Section on Ophthalmology, American Academy of Pediatrics, American Academy of Ophthalmology, American Association for Pediatric Ophthalmology, Strabismus. Screening examination of premature infants for retinopathy of prematurity. Important changes from 2006 criteria are noted including new recommendations for selective earlier screening, treatment, and follow-up after discharge from the NICU. Pediatrics. 2013;131:189–95.
O’Sullivan J, Gilbert C, Foster A. The causes of childhood blindness in South Africa. S Afr Med J. 1997;87:1691–5.
Baiyeroju-Agbeja AMOS. Screening for retinopathy of prematurity in Ibadan. Niger J Ophthalmol. 1998;6:23–5.
Jacoby MR, Du Toit L. Screening for retinopathy of prematurity in a provincial hospital in Port Elizabeth, South Africa. S Afr Med J. 2016;106:598–601.
Visser Kift E, Freeman N, Cook C, Myer L. Retinopathy of prematurity screening criteria and workload implications at Tygerberg Children’s Hospital, South Africa: a cross-sectional study. S Afr Med J. 2016;106:602–6.
Adio AO, Ugwu RO, Nwokocha CG, Eneh AU. Retinopathy of prematurity in Port Harcourt, Nigeria. ISRN Ophthalmol. 2014:1–6.
Howson CP, Kinney MV, McDougall L, Lawn JE. Born too soon: preterm birth matters. Reprod Health. 2013;10(Suppl 1):S1.
Goncalves E, Nasser LS, Martelli DR, Alkmim IR, Mourao TV, Caldeira AP, et al. Incidence and risk factors for retinopathy of prematurity in a Brazilian reference service. Sao Paulo Med J. 2014;132:85–91.
Rao KA, Purkayastha J, Hazarika M, Chaitra R, Adith KM. Analysis of prenatal and postnatal risk factors of retinopathy of prematurity in a tertiary care hospital in South India. Indian J Ophthalmol. 2013;61:640–4.
Vinekar A, Jayadev C, Kumar S, Mangalesh S, Dogra MR, Bauer NJ, et al. Impact of improved neonatal care on the profile of retinopathy of prematurity in rural neonatal centers in India over a 4-year period. Eye Brain. 2016;8:45–53.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European Consensus Guidelines on the management of respiratory distress syndrome—2016 update. Neonatology. 2017;111:107–25.
Askie LM, Darlow BA, Finer N, Schmidt B, Stenson B, Tarnow-Mordi W, et al. Association between oxygen saturation targeting and death or disability in extremely preterm infants in the Neonatal Oxygenation Prospective Meta-analysis Collaboration. JAMA. 2018;319:2190–201.
Liegl R, Hellstrom A, Smith LE. Retinopathy of prematurity: the need for prevention. Eye Brain. 2016;8:91–102.
Arima M, Tsukamoto S, Fujiwara K, Murayama M, Fujikawa K, Sonoda KH. Late-onset circulatory collapse and continuous positive airway pressure are useful predictors of treatment-requiring retinopathy of prematurity: a 9-year retrospective analysis. Sci Rep. 2017;7:3904.
Binenbaum G, Bell EF, Donohue P, Quinn G, Shaffer J, Tomlinson LA, et al. Development of modified screening criteria for retinopathy of prematurity: primary results from the Postnatal Growth and Retinopathy of Prematurity Study. JAMA Ophthalmol. 2018;136:1034–40.
Sood BG, Madan A, Saha S, Schendel D, Thorsen P, Skogstrand K, et al. Perinatal systemic inflammatory response syndrome and retinopathy of prematurity. Pedia Res. 2010;67:394–400.
Silveira RC, Fortes Filho JB, Procianoy RS. Assessment of the contribution of cytokine plasma levels to detect retinopathy of prematurity in very low birth weight infants. Invest Ophthalmol Vis Sci. 2011;52:1297–301.
Landre-Peigne C, Ka AS, Peigne V, Bougere J, Seye MN, Imbert P. Efficacy of an infection control programme in reducing nosocomial bloodstream infections in a Senegalese neonatal unit. J Hosp Infect. 2011;79:161–5.
Dogra MR, Katoch D, Dogra M. An update on Retinopathy of Prematurity (ROP). Indian J Pediatr. 2017;84:930–6.
Oluleye TS, Rotimi-Samuel A, Adenekan A. Mobile phones for retinopathy of prematurity screening in Lagos, Nigeria, sub-Saharan Africa. Eur J Ophthalmol. 2016;26:92–4.
Aprahamian AD, Coats DK, Paysse EA, Brady-Mccreery K. Compliance with outpatient follow-up recommendations for infants at risk for retinopathy of prematurity. J aapos. 2000;4:282–6.
Barry GP, Tauber K, Emmanuel G, Horgan MJ, Simon JW. The effectiveness of policy changes designed to increase the attendance rate for outpatient retinopathy of prematurity (ROP) screening examinations. J AAPOS. 2013;17:296–300.
Vinekar A, Jayadev C, Dogra M, Shetty B. Improving follow-up of infants during retinopathy of prematurity screening in rural areas. Indian Pediatr. 2016;53(Suppl 2):S151–s4.
Campbell JP, Ryan MC, Lore E, Tian P, Ostmo S, Jonas K, et al. Diagnostic discrepancies in retinopathy of prematurity classification. Ophthalmology. 2016;123:1795–801.
Acknowledgements
The authors would like to acknowledge the members of the Rwanda Retinopathy of Prematurity (ROP) Study Group for their valuable contribution to this study (alphabetical order): Cannoodt Luk, PhD, Health Policy Analyst, KU Leuven (Belgium), NGO Umubano-Impore; Casteels Ingele, MD, PhD, Paediatric Ophthalmologist, KU Leuven, Belgium; Conard Craig, MD, MPH, Paediatrician CHUB; De Smedt Stefan, MD, PhD, ophthalmologist/epidemiologist, AZ St Maarten, Mechelen, Belgium; Devlieger Hugo, MD, PhD, neonatologist, KU Leuven, Belgium; Fonteyne Yannick, MD; Gilbert Clare, MD, PhD, International Centre for Eye Health, London School of Hygiene and Tropical Medicine, London, UK; Gisagara Egide, MD, ophthalmologist ; Kumwami Muzungu, MD, paediatrician CHUK; Mudereva Godelieve, MD, ophthalmologist CHUK; Muhizi Charles, MD, ophthalmologist CHUB; Mulindwa Karemazi Gustave, MD, paediatrician CHUB; Musiime Stephenson, MD, FCPaeds(SA), paediatrician KFH; Mutangana Francis, MD, ophthalmologist KFH; Mutsinzi Edison, MD, ophthalmologist Kabgayi Eye Unit; Ngambe Tharcisse, MD, paediatrician KFH; Noë Piet, MD, ophthalmologist Kabgayi Eye Unit, Rwanda Charity Eye Hospital; Nsabimana Hovaire, MD, paediatrician CHUB; Nyemazi Alex, MD, ophthalmologist KFH; Sebuseruka Sonia, MD, ophthalmologist; Tuyisabe Theophile, MD, ophthalmologist Kabgayi Eye Unit; Tuyisenge Lisine, MD, paediatrician CHUK; Uwurukundo Marie Claude, MD, paediatrician KFH; Van Kerschaver Erwin, MD PhD.
Funding
Hoffknecht Van Vuure Stichting (The Netherlands), Vision for All (Switzerland), Rotary Club Overijse Zonienwoud (Belgium), Lions Club Heerlijkheid Mechelen (Belgium), Lumos University Hospitals Leuven (Belgium), Théa Pharma, NGO Umubano- Impore (Rwanda). The funding organizations had no role in the design or conduct of this research.
Rwanda Retinopathy of Prematurity (ROP) Study Group
Luk Cannoodt11, Ingele Casteels9, Craig Conard7, Stefan De Smedt10, Hugo Devlieger12, Yannick Fonteyne8, Clare Gilbert13, Egide Gisagara3, Muzungu Kumwami6, Godelieve Mudereva3, Charles Muhizi2, Gustave Mulindwa Karemazi7, Stephenson Musiime5, Francis Mutangana1, Edison Mutsinzi14, Tharcisse Ngambe5, Piet Noë15, Hovaire Nsabimana7, Alex Nyemazi1, Sonia Sebuseruka16, Theophile Tuyisabe14, Lisine Tuyisenge6, Marie Claude Uwurukundo5, Erwin Van Kerschaver
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Meeting presentation: The work has been accepted and presented as Poster Presentation (Poster 186-B0340, abstract #2906642) for the 2018 ARVO Annual Meeting in Honolulu.
Supplementary information
Rights and permissions
About this article
Cite this article
Mutangana, F., Muhizi, C., Mudereva, G. et al. Retinopathy of prematurity in Rwanda: a prospective multi-centre study following introduction of screening and treatment services. Eye 34, 847–856 (2020). https://doi.org/10.1038/s41433-019-0529-5
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41433-019-0529-5
This article is cited by
-
Prevalence and associated factors of retinopathy of prematurity in sub‑Saharan Africa: a systematic review and meta‑analysis
BMC Ophthalmology (2025)
-
Prevalence and pattern of retinopathy of prematurity at two national referral hospitals in Uganda: a cross-sectional study
BMC Ophthalmology (2023)
-
Long use of continuous positive airway pressure protects against the development of treatment-requiring retinopathy of prematurity
Scientific Reports (2022)
-
Oxygen management among infants in neonatal units in sub-Saharan Africa: a cross-sectional survey
Journal of Perinatology (2021)
-
Association between neonatal hyperglycemia and retinopathy of prematurity: a meta-analysis
European Journal of Pediatrics (2021)